- *Corresponding Author:
- A. R. Kamuhabwa
Unit of Pharmacology and Therapeutics, School of Pharmacy, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania
E-mail: enali2012@gmail.com
| Date of Submission | 14 August 2014 |
| Date of Revision | 30 January 2015 |
| Date of Acceptance | 13 September 2015 |
| Indian J Pharm Sci 2015;77(5):542-549 |
This is an open access article distributed under the terms of the Creative Commons Attribution?NonCommercial?ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non?commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
A descriptive cross-sectional study was conducted to assess quality of dispensing and knowledge of dispensers in 206 private retail pharmacies. The study was conducted in Dar es Salaam, Tanzania between September 2011 and April 2012. Patient simulation (mystery shopper) approach was used to assess dispensing skills of drug dispensers for prescription only medicines. In assessing dispensing skills, a 7-days course of metronidazole tablets was bought from each pharmacy. The knowledge of drug dispenser's regarding dispensing of prescription only medicines was assessed through focus group discussions and interviews. Majority (70.4%) of drug dispensers were not trained pharmaceutical personnel. The level of dispensing skills ranged from low (25.7%) to medium (70.4%). Majority of drug dispensers had low (11.4%) to medium (83.2%) levels of knowledge about dispensing of 'prescription only' medicines. From these findings, it is recommended that the national Pharmacy Council should ensure that prescription only medicines are dispensed by trained pharmaceutical personnel. On job training and continuing professional development should also be emphasized to build capacity of drug dispensers.
Keywords
Dispensing, knowledge, prescription only medicines, drug dispensers, pharmacy
Use of drugs in developing countries has been described as ‘irrational’ by many authors; the prescribing and dispensing of ineffective, unsuitable, sub-optimal or unsafe pharmaceutical products has been widely documented [1,2]. A wide range of contributing factors include difficulties in ensuring the continuous availability of essential drugs, limited finance for health care and shortages of trained personnel. Other challenges include, lack of enforcement of regulations, high prevalence of counterfeit products, access to objective drug information, costs to individuals for purchasing drugs, and health beliefs and cultural traditions regarding their use. The weakness or the absence of national drug policies is also an important obstacle for implementing interventions to improve drug use. However, drug policies can only be effective if mechanisms of implementation are in place, such as monitoring of national drug regulation, a good distribution system, regular supervision and adequate storage facilities.
The World Health Organization (WHO) defines rational drug use as “patients receiving medications appropriate to their clinical needs, in doses that meet their own individual requirements, for an adequate period of time, and at the lowest cost to them and the community” [3]. Rational drug use also means using drugs which are safe and effective, given at adequate dose and for optimal duration of treatment [1]. The Tanzanian ministry of health was one of the few ministries in the world that adapted the Essential Drugs Program (EDP) when it was introduced in early 1990’s by the WHO. This was to ensure that drugs are prescribed and dispensed rationally. Subsequently, rational drug use in Tanzania has been promoted by formulating the National Drug Policy [4].
Currently, there are about 700 pharmacists, 550 pharmaceutical technicians and 600 pharmaceutical assistants registered in Tanzania. There are more than 6,000 public and private pharmaceutical outlets countrywide [5]. This indicates a poor ratio between trained pharmaceutical personnel and pharmaceutical outlets. The government oversees running of the public health facilities such as hospitals, health centers and dispensaries. Usually, a pharmacy department in the hospital is operated under the supervision of pharmacists who are assisted by pharmaceutical technicians, pharmaceutical assistants and other drug dispensers.
In the private sector (which includes for-profit companies, non-governmental organizations and religious organizations), independent pharmacies and hospital-based pharmacies are required to be staffed the same way as in the public sector. In the private sector, pharmaceutical services are graded as either Part I or Part II pharmacies. A part I pharmacy is a fully fledged pharmacy unit operating under the direct supervision of a pharmacist. In these premises, a pharmacist is assisted by a pharmaceutical technician, pharmaceutical assistant and other drug dispensers. On the other hand, a part II pharmacy is a drug store that sells drugs that appear in the schedule of part two poisons list of the Tanzania Food and Drug Authority Act of 2003 [6]. Any person who can read and write and is mentally well usually may supervise these outlets.
Ideally, pharmacists should be available for dispensing of medications, especially prescription only medicines in part I community pharmacies. However, this has not been the case in most developing countries [7,8]. Several studies have reported that most of the dispensers are not trained pharmaceutical personnel of any kind [9,10]. As a result, few pharmacists are onsite in community pharmacies and the dispensing is undertaken by untrained personnel [11]. Effects of allowing control of medicines by untrained dispensers promotes irrational dispensing and failure in the facilitation of patient’s adherence to treatment [12,13]. The major consequences of these effects are the emergence of multiple drug resistance, fatalities caused by toxicity, unforeseen drug’s adverse effects and interaction, treatment failures due to lack of patient adherence to treatment caused by improper information given to patients, and increased treatment costs to individuals and communities. The extent, to which this problem exists in Tanzania, is not documented.
Due to mushrooming of drug outlets and shortage of drug dispensing personnel in Tanzania, it can be assumed that untrained staff called `dispensers` run and supervise these drug outlets. While this improves accessibility to medicines for many people, it compromises heavily on quality, efficacy and safety of drugs, which are the fundamentals of pharmaceutical care [14]. This justifies the need for regulation of pharmaceutical services including provision of training to drug dispensers. This study aimed at assessing the knowledge and skills of drug dispensers for dispensing prescription only medicines in the retail private community pharmacies in the urban area of Tanzania.
Materials and Methods
This descriptive cross-sectional study was conducted between September 2011 and April 2012 in the retail private community pharmacies in all the three municipalities (Ilala, Kinondoni and Temeke) of Dar as Salaam, Tanzania. Patient simulation (mystery shopper) using a checklist was used to assess skills of drug dispensers. Direct interviews using structured questionnaires and Focus Group Discussions (FGDs) were employed for assessing the knowledge of the drug dispensers.
Study setting and sampling techniques
A list of registered retail community pharmacies obtained from Tanzania Food and Drugs Authority (TFDA) indicated that by September 2011 there were 305 part I retail pharmacies in Dar es Salaam. Dar es Salaam is divided into three municipalities (Kinondoni, Ilala and Temeke). It is the largest commercial city in Tanzania with a population of about 4 million people. The city has the highest number of pharmaceutical outlets compared to other regions in Tanzania.
For the purpose of this study, 206 pharmacies were visited by a mystery shopper and later on interviews were conducted with drug dispensing personnel. Pharmacies were selected using stratification method in the three municipalities (19 pharmacies in Temeke, 95 in Ilala and 92 in Kinondoni). Within each municipality, sampling was based on whether the pharmacy was located in the city centre or in the outskirts of the city. With regard to data collection using questionnaires, a total of 185 drug dispensers were directly interviewed in the pharmacies.
Data collection
Information from each dispenser from the respective pharmacy was obtained using simulated client through a checklist [15]. Mystery shoppers (two intern pharmacists) visited the pharmacies with prescriptions of artemether-lumefantrine, amoxycillin and metronidazole. A single 7-days course of metronidazole was bought from each pharmacy for the purpose of assessing dispensing skills. More information was collected through direct interviews of drug dispensers in the community pharmacies using structured questionnaires as well as FGDs for the purpose of assessing dispenser’s knowledge [16].
Tracer drugs
Malaria and microbial infections are very common and greatly affect most developing countries, including Tanzania. Therefore antimalarial and antimicrobial drugs are the most commonly dispensed prescription only medicines in the private retail community pharmacies. In Tanzania, artemether-lumefantrine is used as a first line drug for treatment of uncomplicated malaria and is available in the private community pharmacies as Coartem®. Amoxycillin and metronidazole are commonly used for respiratory and gastrointestinal tract infections, respectively. In this study, these three drugs were used as tracer drugs in assessing the dispensers` knowledge and skills.
Assessment of dispensing skills
Mystery shoppers visited the pharmacies with prescriptions containing the three tracer drugs. At the pharmacy, they enquired about the doses, frequencies, side effects, drug-drug interactions and other relevant information when using these drugs. They then requested to buy a 7-days course of metronidazole as prescribed. After leaving the pharmacy, they filled in a form containing a check list of items that were designed to assess the dispensing process and dispensing skills of the dispensers, including interpretation of the prescribed medicines, instructions given after dispensing of drugs, packing and labeling of the dispensed drugs. An initial average competency score was calculated based on the score from the checklist. After data analysis, the drug dispensers` skills was then graded as low (0-1), medium (2-3) and high (4-5).
Assessment of knowledge of drug dispensers
For the purpose of assessing dispensing knowledge, permission was sought from pharmacy owners to have interviews with drug dispensers. The intern pharmacists conducted interviews in the pharmacies by using questionnaires. Questions were based on the importance of a prescription for dispensing prescription only medicines, drug-drug and drug-food interactions, drug side effects and adverse reactions. A knowledge scale was prepared in which one point was awarded for each correct answer/information given, and a zero point for the wrong answer or failure to provide the expected response. After data analysis, the drug dispenser`s knowledge was then graded as low (0-1), medium (2-3) and high (4-5).
A qualitative approach using FGDs was also used to generate an in-depth understanding of drug dispensers` knowledge about drug-drug interactions, drug resistance to bacteria and malarial parasites, adverse drug reactions, importance of communication, and interpretation of prescriptions when dispensing prescription only medicines. The FGDs were held with 30 dispensers from the pharmacies. Three FGDs, each comprising of 10 dispensers were conducted. Drug dispensers who were selected for FGDs included pharmaceutical personnel and non-pharmaceutical personnel who were dispensing medicines in the private retail community pharmacies. FDGs were conducted at Muhimbili University of Health and Allied Sciences. A social scientist supervised FGDs using a guided format containing probes based on the objectives of the study. Guided discussions were conducted and tape recorded. The main focus of the FGDs was to identify gaps in the dispensing practice of prescription only medicines and to propose strategies for intervention.
Data analysis
Data were analyzed by using the Statistical Package for Social Sciences (SPSS) version 16.0 computer software. Descriptive analysis was undertaken and chi-square test was used to test significant differences in proportions between the different variables for the study. We considered a p-value of less than 0.05 to be statistically significant.
Ethical issues
The study received ethical clearance from Muhimbili University of Health and Allied Sciences Research and Publications Committee. Permission to conduct the study in the selected retail community pharmacies was obtained from TFDA, Pharmacy Council and pharmacy owners. In assessing the knowledge of drug dispensers using mystery shoppers, drug dispensers were not informed in advance and were not asked for consent to participate in the study. For interviews and FGDs, drugs dispensers were provided with written consent requests and relevant information regarding the purpose of the study. All the information obtained was recorded in the checklist or questionnaires, and data were entered into the computer using study code numbers.
Results
Using simulated clients, a total of 206 drug dispensers were assessed for dispensing skills in the retail private community pharmacies in Dar es Salaam. Among them, 61(29.6%) were trained pharmaceutical personnel (21 pharmacists, 31 pharmaceutical technicians and 9 pharmaceutical assistants). Hundred and forty five (70.4%) were non-pharmaceutical personnel, including 9 clinical officers, 113 nurses and 23 sales persons with no formal pharmaceutical or medical training.
The main variables determined were dispensing of prescription only medicines with prescriptions, adequate packaging of dispensed medicines, labeling and instructing the patient about the correct use of medicines. Other variables included instructions given by the dispenser about storage of medicines at home and counseling patients about drug-drug interaction, drug adverse reactions and adherence to medications. In most cases, levels of dispensing skills ranged from low to medium and the differences observed between pharmaceutical and non-pharmaceutical personnel were statistically significant (P=0.000013). Of the 206 dispensing personnel assessed, 53 (25.7%) of them had low dispensing practice skills, 145 (70.4%) had medium skills and only 8 (3.9%) had high dispensing skills (Table 1).
| Qualification of drug dispensers | Dispensing skills (%) | ||
|---|---|---|---|
| Low | Medium | High | |
| Pharmaceutical personnel | |||
| Pharmacists | 0 (0.0) | 15 (10.3) | 6 (75.0) |
| Pharmaceutical technicians | 0 (0.0) | 31 (21.4) | 0 (0.0) |
| Pharmaceutical assistants | 4 (7.5) | 5 (3.4) | 0 (0.0) |
| None?pharmaceutical personnel | |||
| Clinical officers | 0 (0.0) | 9 (6.2) | 0 (0.0) |
| Nurses | 32 (60.4) | 79 (54.5) | 2 (25.0) |
| Others | 17 (32.1) | 6 (4.1) | 0 (0.0) |
| Total | 53 (25.7) | 145 (70.4) | 8 (3.9) |
Table 1: Levels of dispensing skills of drug dispensers (n=206)
No significant differences were observed in dispensing skills with respect to location of pharmacy (P=0.31), size of the pharmacy in terms of the volume of sales, number of drug dispensers working in the pharmacy (P=0.58), and the municipality within which the pharmacies are situated (P=0.12). Almost all (99.5%) drug dispensers failed to give information about proper storage conditions of the medicines at home. With regard to packaging and labeling of the dispensed metronidazole tablets, 205 (99.5%) dispensers indicated the frequency of drug usage as ``2×3`` instead of ``two tablets after every eight hours``. Only 26.2% of drug dispensers indicated on the package the duration (7 days) of use of the drug. About 40% of drug dispensers failed to indicate the strength of metronidazole tablets on the medication package.
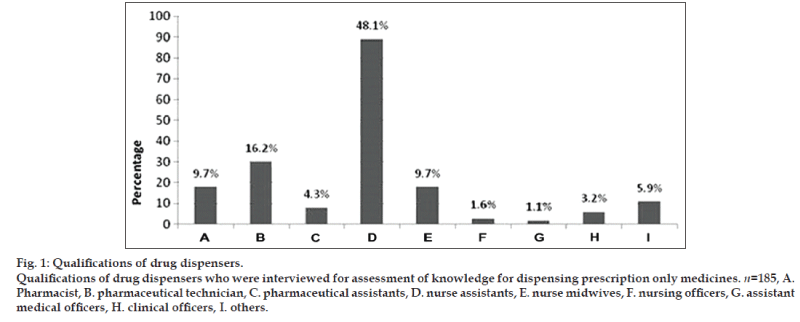
Using questionnaires, 185 drug dispensers were interviewed for the purpose of assessing their dispensing knowledge for prescription only medicines. Among them, 56 (30.2%) were trained pharmaceutical personnel (18 pharmacists, 30 pharmaceutical technicians and 8 pharmaceutical assistants) and 129 (69.7%) were non-pharmaceutical personnel. The different categories of these drug dispensers are shown in fig. 1.
In assessing drug dispensers` knowledge about prescription only medicines, questions were designed to find out if drug dispensers knew why it was important for patients to have been assessed by medical practitioners before they can be dispensed with amoxycillin, artemether-lumefathrine or metronidazole. Particular emphasis was on the consequences of under-dosing, over-dosing and resistance of microorganisms to antimicrobial agents. With regard to knowledge of the drug dispensers on dispensing prescription only medicines, majority (94.6%) of them had low to medium knowledge and only 10 (5.4%) dispensers had high level of knowledge (Table 2). The observed differences in knowledge between pharmaceutical and non-pharmaceutical personnel was statistically significant (P=0.000001). All drug dispensers with high knowledge for dispensing prescription only medicines were pharmacists (6) and pharmaceutical technicians (4).
| Qualification of drug dispensers | Knowledge on prescription only medicines (%) | ||
|---|---|---|---|
| Low | Medium | High | |
| Pharmaceutical personnel | |||
| Pharmacists | 0 (0.0) | 12 (66.7) | 6 (33.3) |
| Pharmaceutical technicians | 1 (3.3) | 25 (83.3) | 4 (13.3) |
| Pharmaceutical assistants | 1 (12.5) | 7 (87.5) | 0 (0.0) |
| Non?pharmaceutical personnel | |||
| Auxiliary nurses | 14 (15.7) | 75 (84.3) | 0 (0.0) |
| Nurse midwives | 2 (11.1) | 16 (88.9) | 0 (0.0) |
| Nurse officers | 0 (0.0) | 3 (100) | 0 (0.0) |
| Clinical officers | 0 (0.0) | 6 (100) | (0.0) |
| Assistant medical officers | 0 (0.0) | 2 (100) | 0 (0.0) |
| Others | 3 (27.3) | 8 (72.7) | 0 (0.0) |
| Total | 21 (11.4) | 154 (83.2) | 10 (5.4) |
Table 2: Knowledge levels of drug dispensing personnel regarding dispensing of prescription only medicines (n=185)
Drug dispensers were asked to mention the common side effects and adverse drug reactions of the tracer medicines. About two thirds (69.4%) of the drug dispensers were aware of some side effects and adverse reactions of the tracer medicines. The most mentioned adverse effect for amoxycillin was allergic reaction, while abdominal discomfort was the most mentioned side effect for oral metronidazole.
Knowledge on concomitant use of drugs with other drugs, food or alcohol was also assessed. With regard to drug-food interactions, the aim was to assess if drug dispensers are aware of the importance of fatty meals when a patient is dispensed with artemether-lumefantrine. Over all, the knowledge levels of drug dispensing personnel about drug-drug and drug-food interactions ranged from medium (62.2%) to high (37.8%, Table 3). Only 70 (37.8%) respondents were aware of the importance of fatty meals when a patient is given artemether-lumefantrine. Another area of concern for drug-drug and drug-beverage interaction was the concomitant use of metronidazole and alcohol.
| Qualification of drug dispensers | Knowledge on drug?drugand drug?foodinteractions (%) | |
|---|---|---|
| Medium | High | |
| Pharmaceutical personnel | ||
| Pharmacists | 3 (14.3) | 16 (88.9) |
| Pharmaceutical technicians | 4 (13.3) | 26 (86.7) |
| Pharmaceutical assistants | 6 (75.0) | 2 (25.0) |
| Non-pharmaceutical | ||
| Auxiliary nurses | 76 (85.4) | 13 (14.6) |
| Nurse midwives | 11 (61.1) | 7 (38.9) |
| Nurse officers | 3 (100) | 0 (0.0) |
| Clinical officers | 1 (16.7) | 5 (83.3) |
| Assistant medical officers | 2 (100) | 0 (0.0) |
| Others | 9 (90.0) | 1 (10.0) |
| Total | 115 (62.2) | 70 (37.8) |
Table 3: Knowledge levels of drug dispensing personnel about drug?drug and drug?food interactions (n=185)
Eighty seven (42.2%) drug dispensers did not counsel the patients about the need to avoid alcohol when taking metronidazole. In general there was a correlation (P=0.001) between the level of knowledge and the professional category of the dispensing personnel. Majority (79.7%) of drug dispensers with medium knowledge about drug-food interaction were non-pharmaceutical personnel. On the other hand, 44 (78.6%) drug dispensing personnel with high knowledge about drug-food interactions were pharmacists and pharmaceutical technicians (Table 3).
The results of qualitative part of this study were obtained from the FGDs. During these discussions it was clear that there are challenges faced by drug dispensers. Many patients visiting these pharmacies to buy medicines have no health insurance and may therefore be unable to buy a full dose of the prescribed medication. As a result, some patients ask to buy half a dose and promise to come back for prescription refill before completion of the dispensed drugs. Participants in the FGDs mentioned that some patients do not come back, and therefore do not complete the prescribed doses. Drug dispensers commented that this is the main reason for irrational dispensing and use of medicines including antibiotics.
Many drug dispensers also said that many pharmacies do not have rooms for counseling patients and clients, which affects confidentiality. Drug dispensers commented that pharmacy owners do not provide resources and time for the dispensers to attend short courses and other training avenues for continuing education and professional development. Limitation on accessing new information on drugs and diseases was also mentioned as an impediment for upgrading knowledge of drug dispensers.
Other challenges facing drug dispensers included unreadable prescriptions from prescribers and the lack of easy communication between prescribers and dispensers. In case there is an obvious prescription error, some drug dispensers decide to correct the prescriptions, while others return the patients to their prescribers for clarification or correction of medication errors. This creates inconveniences to patients as they spend more time waiting for prescribers to correct the prescriptions or provide clarification to the dispensers.
Discussion
The findings of this study have shown that majority of drug dispensers in the retail community private pharmacies have insufficient skills and knowledge in providing patients with accurate information regarding dosage, interactions, side effects, adherence and storage of medications. Dispensing of prescription only medicines by such personnel results in irrational dispensing and increases the likelihood of patient’s non-adherence to treatment [12,13]. This is likely to result in the emergence of multiple drug resistance, fatalities caused by drug toxicities, unforeseen drug’s adverse effects, interactions, treatment failures and increased treatment costs to individuals and communities [17].
The observed lack of skills and knowledge among drug dispensers for dispensing prescription only medicines can be partly due to the fact that the majority of the drug dispensers are non-pharmaceutical personnel with no formal training as drug dispensers. As per regulation, medicines should be dispensed under the supervision of a qualified and registered pharmacist. From the findings of this study it seems that this regulation is not enforced and therefore pharmacies are not properly supervised.
It was also revealed that most of the drug dispensers have low to medium skills in dispensing prescription only medicines. Skills of dispensers are also limited with regard to proper packaging of medicines, labeling, instructing patients about the correct uses and storage of medicines at home. Moreover, patient counseling about drug and food interactions, adverse drug reactions and adherence strategies were among the shortcomings of drug dispensers. These findings are similar to that of a previous study which showed that dispensers in private pharmacies in Dar as salaam have poor knowledge in providing accurate information to patients on dosage and adverse reactions for antimalarial drugs [8].
Of major concern was the instructions given by drug dispensers for the daily doses of metronidazole. Drug dispensers instructed patients to take two tablets in the morning, afternoon and in the evening. As such, the daily dose is taken over the period of 12 h instead of 24 h. Obviously this is likely the major reason on why antimicrobial agents are showing increasing incidences of resistance to antibiotics [18,19]. In addition, drug dispensers are still unaware of the importance of advising patients to take artemether-lumefantrine with fatty meals. Food, especially dietary fat enhances the bioavailability of lumefantrine [20]. This is particularly relevant in view of the low food intake by many patients during the acute phase of malaria. It is known that in patients with uncomplicated malaria, the extent and variability of lumefantrine absorption improves with clinical recovery as normal food intake is resumed [21]. In the present study, majority of drug dispensers in the community pharmacies did not advise patients about the importance of food and fatty meals when using artemether-lumefantrine.
Due to frequent shortage of antimalarial and other drugs in the public health facilities in Tanzania, private community pharmacies are the main sources of drugs. These premises are readily available and accessible by the majority of general public. It is in these premises where most people obtain their medicines, information about medication and counseling on medical care. However, large client volumes to these premises have been associated with low quality of pharmaceutical services [22,23]. It is therefore of importance that dispensers involved in dispensing medicines in these premises are capable of counseling the patients in all matters related to medicines. In order to achieve this responsibility, these personnel need to be trained and have adequate skills and knowledge regarding good dispensing practice and rational use of medicines.
The knowledge and skills of most of the dispensers in the retail pharmacies depend on the level of supervision and training provided in a particular facility. Since pharmaceutical personnel, in particular pharmacists are few and do not have enough time to provide supervisory trainings, most dispensers are left to train themselves and what they acquire depends much on personal efforts. This therefore justifies the need for provision of training to these dispensers. In addition, most drug dispensers are not supported by the pharmacy owners for continuing education and professional development. As such, they are not up to date with new drug information, technological changes, emerging and re-emerging diseases. Knowing that science and technology is always and rapidly changing, it is necessary that drug dispensers should have access to up to date reading materials and computers with internet connection in the pharmacies for accessing relevant drug and diseases information.
The results of this study show that the levels of knowledge and skills of drug dispensers with regard to dispensing prescription only medicines are not adequate, especially among the non-pharmaceutical personnel who are the majority of dispensers. Due to increasing treatment of malaria outside government facilities, strategies to control irrational dispensing and use of antimalarial drugs is necessary. Since the majority of the dispensing personnel were trained pharmaceutical personnel, the Pharmacy Council of Tanzania should ensure that only trained non-pharmaceutical personnel are allowed to dispense medicines in the pharmacies. The Pharmacy Council should also devise mechanisms to enforce on job training and professional development among drug dispensing personnel in order to build their capability with changing technology, emerging diseases and new drug information and treatment guidelines.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- le Grand A, Hogerzeil HV, Haaijer-Ruskamp FM. Intervention research in rational use of drugs: A review. Health Policy Plan 1999;14:89-102.
- Smith F. Community pharmacy in Ghana: Enhancing the contribution to primary health care. Health Policy Plan 2004;19:234-41.
- World Health Organization. The Selection and Use of Essential Medicines. Report of the WHO Expert Committee, 2002 (Including the 12th Model List of Essential Medicines).Technical Report Series No. 914. Geneva: WHO; 2003.
- Tanzania Ministry of Health. National Health Policy. Dar es Salaam: Tanzania Ministry of Health; 1990.
- Tanzania Food and Drug Authority. Annual Report. Dar es Salaam: TFDA; 2004.
- The United Republic of Tanzania. The Tanzania Food, Drugs and Cosmetics Act. Dar es, Salaam: TFDA; 2003.
- Cederlof C, Tomson G. Private pharmacies and the health sector reform in developing countries – Professionals and commercial highlights. J SocAdm Pharm 1995;3:101-11.
- Minzi OM, Haule AF. Poor knowledge on new malaria treatment guidelines among drug dispensers in private pharmacies in Tanzania: The need for involving the private sector in policy preparations and implementation. East Afr J Public Health 2008;5:117-21.
- Kamat VR, Nichter M. Pharmacies, self-medication, and pharmaceutical marketing in Bombay. Indian SocSci Med 1998;47:779-94.
- Tumwikirize WA, Ekwaru PJ, Mohammed K, Ogwal-Okeng JW, Aupont O. Management of acute respiratory infections in drug shops and private pharmacies in Uganda: A study of counter attendants’ knowledge and reported behaviour. East Afr Med J 2004;Suppl:33-40.
- Basak SC, Prasad GS, Arunkumar A, Senthilkumar S. An attempt to develop community pharmacy practice: Results of two surveys and two workshops conducted in Tamil Nadu. Indian J Pharm Sci 2005;67:362-67.
- Awad AI, Ball DE, Eltayeb IB. Improving rational drug use in Africa: The example of Sudan. East Mediterr Health J 2007;13:1202-11.
- Waako PJ, Odoi-adome R, Obua C, Owino E, Tumwikirize W, Ogwal-Okeng J, et al.Existing capacity to manage pharmaceuticals and related commodities in East Africa: An assessment with specific reference to antiretroviral therapy. Hum Resour Health 2009;7:21.
- Matowe L, Waako P, Adome RO, Kibwage I, Minzi O, Bienvenu E. A strategy to improve skills in pharmaceutical supply management in East Africa: The regional technical resource collaboration for pharmaceutical management. Hum Resour Health 2008;6:30.
- Kamuhabwa A, Ramji K. Antimalarial drugs for pediatrics: Prescribing and dispensing practices in Tanzanian City. Trop J Pharm Res 2011;10:611-8.
- Caamaño F, Ruano A, Figueiras A, Gestal-Otero JJ. Data collection methods for analyzing the quality of the dispensing in pharmacies. Pharm World Sci 2002;24:217-23.
- Hardon A, Le Grand A. Pharmaceuticals in Communities: Practices, Public Health Consequences and Intervention Strategies. Amsterdam: Royal Tropical Institute, Primary Health Care Department; 1993.p. 40.
- Erb A, Stürmer T, Marre R, Brenner H. Prevalence of antibiotic resistance in Escherichia coli: Overview of geographical, temporal, and methodological variations. Eur J ClinMicrobiol Infect Dis 2007;26:83-90.
- Macgowan AP; BSAC Working Parties on Resistance Surveillance. Clinical implications of antimicrobial resistance for therapy. J AntimicrobChemother 2008;62Suppl 2:ii105-14.
- Ezzet F, van Vugt M, Nosten F, Looareesuwan S, White NJ. Pharmacokinetics and pharmacodynamics of lumefantrine (benflumetol) in acute falciparum malaria.Antimicrob Agents Chemother2000;44:697-704.
- Ezzet F, Mull R, Karbwang J. Population pharmacokinetics and therapeutic response of CGP 56697 (artemether + benflumetol) in malaria patients. Br J ClinPharmacol 1998;46:553-61.
- Stenson B, Syhakhang L, Eriksson B, Tomson G. Real world pharmacy: Assessing the quality of private pharmacy practice in the Lao People’s Democratic Republic.SocSci Med 2001;52:393-404.
- Kroeger A, Ochoa H, Arana B, Diaz A, Rizzo N, Flores W. Inadequate drug advice in the pharmacies of Guatemala and Mexico: The scale of the problem and explanatory factors. Ann Trop Med Parasitol 2001;95:605-16.