- Corresponding Author:
- Nusrat Shafiq
Department of Pharmacology, Pt. B. D. Sharma Postgraduate Institute of Medical Sciences (PGIMS), Rohtak-124 001
E-mail: nusrat_shafiq@hotmail.com
| Date of Submission | 28 September 2013 |
| Date of Revision | 01 June 2014 |
| Date of Acceptance | 10 June 2014 |
| Indian J Pharm Sci 2014; 76(4): 308-314 |
Abstract
Drug therapy accounts for a major portion of health expenditure. A useful strategy for achieving cost efficient healthcare is drug utilisation research as it forms the basis for making amendments in drug policies and helps in rational drug use. The present observational study was conducted to generate data on drug utilization in inpatients of our tertiary care hospital to identify potential targets for improving drug prescribing patterns. Data was collected retrospectively from randomly selected 231 medical records of patients admitted in various wards of the hospital. WHO Anatomical Therapeutic Chemical/Defined Daily Dose methodology was used to assess drug utilisation data and drug prescriptions were analysed by WHO core drug indicators. Antibiotics were prescribed most frequently and also accounted for majority of drug costs. The prescribed daily dose for most of the antibiotics corresponded to defined daily dose reflecting adherence to international recommendations. Brand name prescribing and polypharmacy was very common.78% of the total drugs prescribed were from the National List of Essential Medicines 2003. Restricting the use of newer and costlier antibiotics, branded drugs and number of drugs per prescription could be considered as targets to cut down the cost of drug therapysignificantly.
Keywords
Drug utilisation, Defined daily dose, Prescribed daily dose, Polypharmacy, Essential medicines
Drug utilisation research holds a crucial place in clinical practice as it forms the basis for making amendments in the drug dispensing policies at local and national levels. The ultimate goal of such research is to facilitate rational drug use. Also, since it helps in developing strategies to utilize health resources in the most efficient manner, it is particularly needed in a developing economy like India where 72% of all health care burden is borne by the patients [1].
The reference standard for drug utilisation is WHO ATC/DDD (Anatomical Therapeutic Chemical/Defined daily dose)methodology [2]. Foreach drug and route of administration, defined daily dose (DDD) is defined by the WHO Collaborating Centre for Drug Statistics andMethodology as the assumed averagemaintenance adult dose per day for its main indication. The DDD therefore is an international unit serving for international or regional comparisons. However, DDD does not necessarily reflect the recommendedor prescribed daily dose (PDD). In fact, several studies have reported discrepancies between DDD and PDD for different groups of drugs [3-6].
A number of studies have reported drug usage patterns in different health care sectors in India [7-16]. The aim of the present study was to generate data on drug utilisation in patients admitted in various wards ofour hospital with a focus to analyse drug prescriptions for WHO core indicators and comparison of average PDD with WHO DDD. The study results would be taken as basis for identifying potential targets to make improvements in prescribing patterns and drug dispensing policies of the hospital.
Materials and Methods
This inpatient drug utilisation study was conducted at the Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh. Ours is a tertiary care referral centre. In a calendar year about 2 lakh and about 18 thousand patients in a month are admitted in various wards of the hospital. Drug prescriptions are written by the treating physicians while the drugs are procured by the patients themselves.
Data was collected by evaluating treatment charts of inpatients stored at the medical records department of the hospital. 231 treatment charts from the month of July 2008 were randomly selected. The data was extracted by two investigators independently. Data collection was done using a predesigned proforma which included patient characteristics such as age, gender, diagnosis, duration of hospitalisation and prescription characteristics such as name of the drug, strength and dosage form, number of units dispensed, whether prescribed in generic name or not. We also evaluated the WHO core drug prescribing indicators including (a) average number of drugs per encounter, (b) percentage of drugs prescribed by generic names, (c) percentage of encounters with an antibiotic, (d) percentage of encounters with an injection, and (e) percentage of drugs prescribed from the essential drugs list or formulary.
All drugs were coded as per the WHO Anatomical Therapeutic and Chemical Classification (ATC) coding system. National List of Essential Medicines 2003 of India [17] was used for assessing the number of drugs prescribed from the essential list. From the prescription data of commonly prescribed groups of drugs, the amounts of drugs consumed were converted into the number of DDD as per the 2010 version of ATC/DDD index. DDD was calculated as items issued × amount of drug per item/WHO DDD measure. The number of DDDs per 100 bed days was calculated. Finally, for anti-infectives, estimated PDD was calculated in grams by multiplying DDD with the ratio of number of DDDs to the number of treatment days.
Statistical analysis
Data was expressed as mean±SD, median (IQR), numbers and percentages. All data was entered into Microsoft Access 2007 version database and subsequently statistically analyzed using the same. No statistical hypothesis was tested.
Results and Discussion
A total of 231 treatment charts were reviewed during the study period. The patients included were admitted for various diagnosis most common being sepsis, multiple organ failure and for surgical procedures. The distribution of various inpatients was similar for males (50.2%) and females (48.9%). The mean±SD age of the patients was 40.5±17.6 years. The median duration of hospital stay was 6 days (range 1-28 days).
Antiinfective agents followed by drugs acting on gastrointestinal system, nutritional supplements and antiinflammatory agents were the most common class of drugs prescribed to the inpatients (Table 1). Eighty percent prescriptions included injectables, most commonly antibiotics. Insulin (11%), H2 blockers (3%) and inotropes (1.5%) were other frequently used injectables.
| Major group | Classes of drugs | Number prescribed (%)* |
|---|---|---|
| Antiinfectives | 167 (72.3) | |
| β-lactams | 68 (29.4) | |
| Quinolones | 39 (16.9) | |
| Aminoglycosides | 37 (16) | |
| Antiprotozoal and | 35 (15) | |
| antihelminthic drugs | ||
| Antifungals | 11 (0.05) | |
| Antitubercular drugs | 10 (0.04) | |
| Macrolides | 9 (0.04) | |
| Others | 8 (0.03) | |
| Tetracyclines | 5 (0.02) | |
| Antivirals | 1 (0.004) | |
| Drugs acting on gastrointestinal system |
151 (65.4) | |
| Proton pump inhibitors | 68 (29.4) | |
| Antiemetics | 46 (19.9) | |
| Laxatives | 33 (14.3) | |
| H2 blockers | 28 (12.1) | |
| Others | 2 (0.008) | |
| Nutritional supplements | 120 (51.9) | |
| Antiinflammatory | 104 (45) | |
| Nonsteroidal | 72 (31.2) | |
| antiinflammatory drugs | ||
| Corticosteroids | 30 (13) | |
| Immunosuppressants | 8 (0.03) | |
| Cardiovascular drugs | 96 (41.6) | |
| Beta blockers | 36 (15.6) | |
| Diuretics | 35 (15) | |
| Calcium channel blockers | 31 (13.4) | |
| ACE inhibitors | 29 (12.5) | |
| Vasodilators | 15 (0.06) | |
| Inotropes | 13 (0.05) | |
| Alpha blockers | 1 (0.04) | |
| Drugs acting on central nervous system |
45 (19.5) | |
| Opioid analgesics | 31 (13.4) | |
| Sedatives and hypnotics | 25 (10.8) | |
| Antiepileptics | 17 (0.07) | |
| Antipsychotics | 3 (0.01) | |
| Antidepressants | 3 (0.01) | |
| Hypolipidemic drugs | 35 (15) | |
| Antiplatelet drugs | 31 (13.4) | |
| Aspirin | 28 (12.1) | |
| Clopidogrel | 18 (0.08) | |
| Hormonal agents | 30 (13) | |
| Insulin | 20 (0.08) | |
| Thyroid hormones | 8 (0.03) | |
| Growth hormone | 1 (0.004) | |
| Erythropoetin | 1 (0.004) | |
| Drugs acting on respiratory system |
19 (0.08) | |
| Bronchodilators | 15 (0.06) | |
| Antihistamines | 4 (0.02) | |
| Anticoagulant drugs | 16 (6.9) | |
| Heparin | 15 (0.06) | |
| Warfarin | 1 (0.004) | |
| Oral hypoglycaemic agents | 12 (0.05) | |
| Total no of prescriptions | 826 | |
*Number (percent) of patients prescribed a particular drug (total number of patients=231)
Table 1: Various Classes Of Drugs Prescribed
The mean±SD [median (range)] number of drugs prescribed per prescription was 3.6±1.6 [3 (2-12)]. The percentage of prescriptions with ≥3, ≥5 and ≥10 drugs prescribed were 78, 53.6 and 16.5 percent, respectively. Antibiotics were prescribed in more than 60% prescriptions (154/231). Of these, 70 (45.7%) were single antibiotic prescriptions, while 56 (36.3%) and 28 (18%) had two and three or more antibiotics prescribed respectively.
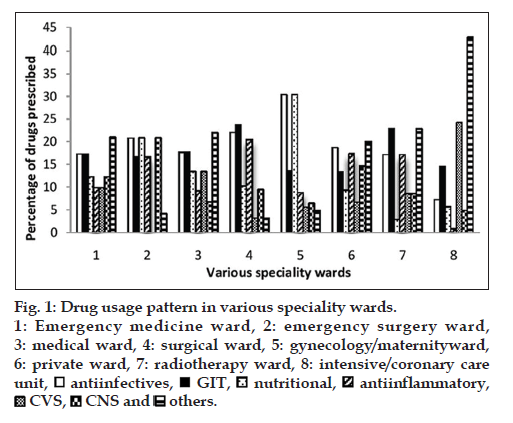
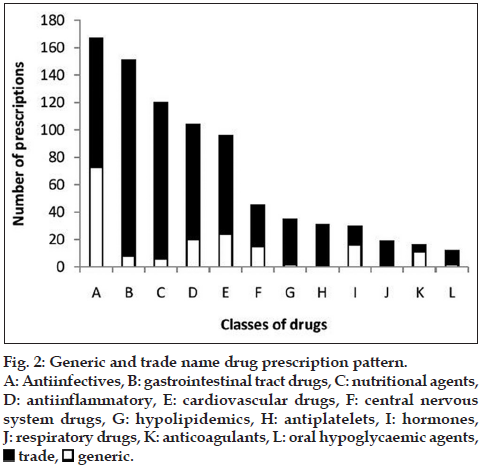
The major classes of drugs prescribed in various speciality wards are shown in fig. 1. The percentage of drugs prescribed from different classes varied in different wards due to variable patient profiles and indications. More than three-fourth prescriptions were by trade names [648/826 (78.45%)] (fig. 2).
Figure 1: Drug usage pattern in various speciality wards.
1: Emergency medicine ward, 2: emergency surgery ward,
3: medical ward, 4: surgical ward, 5: gynecology/maternityward,
6: private ward, 7: radiotherapy ward, 8: intensive/coronary care
unit, antiinfectives,
antiinfectives,  GIT,
GIT,  nutritional,
nutritional,  antiinflammatory,
antiinflammatory,
 CVS,
CVS,  CNS and
CNS and  others.
others.
Figure 2: Generic and trade name drug prescription pattern.
A: Antiinfectives, B: gastrointestinal tract drugs, C: nutritional agents,
D: antiinflammatory, E: cardiovascular drugs, F: central nervous system drugs, G: hypolipidemics, H: antiplatelets, I: hormones,
J: respiratory drugs, K: anticoagulants, L: oral hypoglycaemic agents, trade,
trade,  generic.
generic.
The drug prescriptions were analysed for WHO core indicators (Table 2). Overall, 78% of the total drugs prescribed were from the National List of Essential Medicines 2003. Adherence to the list was most commonly seen with nutritional agents (iron, folic acid, vitamin and calcium preparations) (82%) and least with gastrointestinal drugs (40%).
| WHO core indicators | N (%) |
|---|---|
| Encounters with injectables* | 185 (80.1) |
| Encounters with antibiotics* | 154 (66.7) |
| No. of prescriptions with drugs from EML | 648/826 (78.4) |
| Average number of drugs per prescription | 3.6 |
| No. of prescriptions with generic drugs | 178/826 (21.5%) |
*Number (percent) of patients having encounters with injectables and antibiotics. (EML: Essential medicine list)
Table 2: Who Core Indicators Assessing Drug Prescription
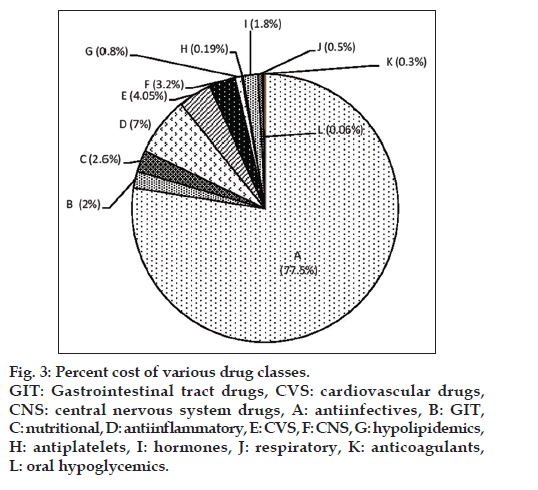
The percentage cost of various groups of drugs is shown in fig. 3. Antiinfective agents comprised the major cost of all prescribed drugs (77.5%). Among these, newer agents like piperacillin-tazobactam, vancomycin and amoxicillin-clavulanic acid accounted for majority of the cost. The median (IQR) cost per prescription in various speciality wards is shown in Table 3.
Figure 3: Percent cost of various drug classes.
GIT: Gastrointestinal tract drugs, CVS: cardiovascular drugs,
CNS: central nervous system drugs, A: antiinfectives, B: GIT,
C: nutritional, D: antiinflammatory, E: CVS, F: CNS, G: hypolipidemics,
H: antiplatelets, I: hormones, J: respiratory, K: anticoagulants,
L: oral hypoglycemics.
| Ward | Median (IQR) Cost (in INR) |
|---|---|
| Female medical ward | 108 (74-225) |
| Radiotherapy ward | 146 (126-455) |
| Gynaecology ward | 299 (165-1863) |
| Maternity ward | 1065 (128-1320.5) |
| Cardiothoracic ward | 1413 (333-3212) |
| Female surgical ward | 1938 (1587.5-3494) |
| Male surgical ward | 1982.5 (1554-2431.5) |
| Emergency ward | 2110 (1707-7600) |
| Male medical ward | 2373.5 (1488-9263) |
| Private ward | 3758.5 (1087?4805.5) |
INR: Indian National Rupee
Table 3: Median (Iqr) Cost Per Prescription In Various Wards
The total number of DDDs consumed were maximum for antibacterials followed by proton pump inhibitors, ACE inhibitors and diuretics while the number of DDDs per 100 bed days was higher for sedatives and hypnotics and ACE inhibitors (Table 4). The comparison of number of PDDs and DDDs of various antibacterials is shown in Table 5.
| Major group | Class | ATC code |
Number of DDDs |
Number
of bed days |
DDDs per 100 bed days |
|---|---|---|---|---|---|
| Antibacterials | |||||
| Beta lactams | J01C | 1506.34 | 661 | 228 | |
| Aminoglycosides | J01G | 153.11 | 208 | 73 | |
| Macrolides | J01F | 34.5 | 33 | 104 | |
| Quinolones | J01M | 315.3 | 222 | 142 | |
| Total | 2009.25 | 1124 | 547 | ||
| Drugs acting on gastrointestinal system |
|||||
| Proton pump inhibitors |
A02BC | 836.33 | 651 | 128 | |
| H2 blockers | A02BA | 74.23 | 121 | 61 | |
| Total | 910.56 | 772 | 189 | ||
| Non steroidal | M01A | 195.3 | 171 | 114 | |
| antiinflammatory | |||||
| drugs | |||||
| Cardiovascular | |||||
| drugs | |||||
| Beta-blockers | C07A | 89.58 | 185 | 48 | |
| Diuretics | C03 | 439.9 | 152 | 289 | |
| Calcium | C08 | 415.25 | 211 | 197 | |
| channel | |||||
| blockers | |||||
| ACE inhibitors | C09 | 449.5 | 141 | 318 | |
| Total | 1394.23 | 689 | 852 | ||
| Central nervous system drugs |
|||||
| Opioid analgesics |
N02A | 48.7 | 104 | 47 | |
| Sedatives and hypnotics |
N05C | 272.33 | 36 | 756 | |
| Antiepileptics | N03A | 146.11 | 174 | 84 | |
| Total | 467.14 | 314 | 887 |
DDDS: Defined daily doses, ATC: anatomical therapeutic and chemical classification, ACE: angiotensin-converting enzyme
Table 4: Comparison Of The Number Of Defined Daily Doses Per 100 Bed Days Of Major Groups Of Drugs Prescribed
| Class | Individual drugs | ATC code | Number of DDDs | Number of bed days | DDDs per 100 bed days | WHO DDD | PDD |
|---|---|---|---|---|---|---|---|
| Beta lactams | |||||||
| Ceftriaxone | J01DD04 | 520.5 | 153 | 340 | 2 | 6.8 | |
| Imipenem | J01DH51 | 16 | 16 | 100 | 2 | 2 | |
| Piperacillin-tazobactam | J01CR05 | 139.87 | 173 | 81 | 14 | 11.34 | |
| Ampicillin | J01CA01 | 83.75 | 93 | 90 | 2 | 1.8 | |
| Amoxicillin | J01CA04 | 109 | 74 | 147 | 1 | 1.47 | |
| Cefixime | J01DD08 | 352.25 | 57 | 618 | 0.4 | 2.47 | |
| Ceftizoxime | J01DD07 | 7.75 | 10 | 77 | 4 | 3.08 | |
| Cefuroxime | J01DC02 | ||||||
| Oral | 22.33 | 16 | 139 | 0.5 | 0.69 | ||
| Injectable | 11 | 6 | 183 | 3 | 5.49 | ||
| Amoxicillin-clavulanate | J01CR02 | ||||||
| Oral | 42.23 | 38 | 111 | 1 | 1.11 | ||
| Injectable | 74.5 | 46 | 162 | 3 | 4.86 | ||
| Cefazolin | J01DB04 | 1.75 | 3 | 58 | 3 | 1.74 | |
| Cefepime | J01DE01 | 22 | 11 | 200 | 2 | 4 | |
| Cloxacillin | J01CF02 | 25 | 16 | 156 | 2 | 3.12 | |
| Ceftazidime | J01DD02 | 3 | 3 | 100 | 4 | 4 | |
| Meropenem | J01DH02 | 12 | 8 | 150 | 2 | 3 | |
| Cefoperazone | J01DD12 | 13.75 | 12 | 114 | 4 | 4.56 | |
| Cefadroxil | J01DB05 | 4.5 | 2 | 225 | 2 | 4.5 | |
| Aminoglycosides | |||||||
| Amikacin | J01GB06 | 82.09 | 96 | 85 | 1 | 0.85 | |
| Streptomycin | J01GA01 | 5.11 | 6 | 85 | 1 | 0.85 | |
| Kanamycin | J01GB04 | 7.28 | 8 | 91 | 1 | 0.91 | |
| Gentamicin | J01GB03 | 53.2 | 68 | 78 | 0.24 | 0.18 | |
| Macrolides | |||||||
| Azithromycin | J01FA10 | 22.9 | 22 | 104 | 0.5 | 0.52 | |
| Clindamycin | J01FF01 | ||||||
| Oral | 4.85 | 4 | 121 | 1.2 | 1.45 | ||
| Injectable | 6.75 | 7 | 96 | 1.8 | 1.73 | ||
| Quinolones | |||||||
| Ciprofloxacin | J01MA02 | ||||||
| Oral | 145.2 | 115 | 126 | 1 | 1.26 | ||
| Injectable | 118.7 | 67 | 177 | 0.5 | 0.88 | ||
| Ofloxacin | J01MA01 | 23.5 | 19 | 123 | 0.4 | 0.49 | |
| Levofloxacin | J01MA12 | 30.8 | 24 | 128 | 0.5 | 0.64 |
DDD: Defined daily doses, PDD: prescribed daily doses, WHO: World Health Organization, ATC: anatomical therapeutic and chemical classification.
Table 5: Comparison Of Estimated Prescribed Daily Doses And Defined Daily Doses Of Various Anti-Bacterials
Our study reports the drug usage pattern among inpatients at a tertiary care level in India. Antibiotics were the most commonly prescribed class of drugs, a finding similar to a previous study conducted in emergency medicine department of our hospital [18]. Among these, β-lactams comprised maximum number of defined daily doses consumed followed by quinolones and aminoglycosides. Piperacillin-tazobactam was the commonly prescribed penicillin-enzyme inhibitor, in contrast to amoxicillin-clavulanate acid reported previously [19], which might be due to its broader spectrum of action and changing resistance patterns and prescription habits.
For β-lactams, the average PDD was similar to or higher than DDD while for aminoglycosides, PDD was lower than DDD, which might be due to different safety profiles of these two groups. Overall, correspondence was observed between PDD and DDD for most antibiotics reflecting adherence to international recommendations in contrast to findings in few other studies demonstrating marked deviations between PDD and DDD for most antibiotics [4,20].
Antibiotics also comprised the highest percentage costs (77.5%) of all groups of drugs similar to a studyin the emergency unit of our hospital in which antibiotics accounted for more than 50% of drug cost expenditure [14]. Agents like piperacillintazobactam, amoxicillin-clavulanate and vancomycin mainly accounted for such high costs. Inappropriate use of antibiotics is also responsible for rising incidence of microbial resistance [21]. Such a scenario demands changes in the hospital antibiotic policy to limit the frequent and inappropriate prescription of antibiotics particularly the newer and costlier agents. An important step in this direction could be implementation of antibiotic restriction program. As per this program, hospital needs to develop a list of restricted antibiotics depending on prevailing resistance patterns and costs, dispensing and initiating course of whom necessitates prior approval from a member of the Infectious diseases team, which would be a multidisciplinary team of staff physicians and clinical/staff pharmacists. In this way, this strategy might prove useful in combating high health care costs and emergence of resistance to newer susceptible agents. The success of this program in decreasing antibiotic utilisation has been demonstrated previously [22]. Another proven useful strategy might be improvement in prescribing practices by making practice guidelines accessible to physicians while they are making clinical decisions [23]. Also, the indiscriminate use of prophylactic antibiotics needs to be curtailed. The use of biomarkers like procalcitonin (PCT) also might help to reduce antibiotic misuse. PCT has been identified as a surrogate marker for estimating the likelihood of a bacterial infection (PCT levels >0.5 µg/l: very likely chances of bacterial infection and levels <0.1 µg/l: very unlikely chances of bacterial infection) [24]. The use of PCT-guided antibiotic management has been shown to markedly reduce the overuse of antibiotic therapy without an apparent negative impact on patient outcome in 11 randomized controlled trials including over 3500 patients from different European countries [25].
Drugs acting on gastrointestinal system and nutritional agents were among the other commonly prescribed agents. However, whether the use of these supplements was actually medically indicated needs a closer scrutiny.
In spite of various benefits like low cost of drug therapy, increased patient adherence [26,27] and equivalent therapeutic benefits as brand name alternatives [28], generic prescribing is not a common practice in India. In our study, more than 75 percent prescriptions were by brand names. Pharmaceutical step-therapy approach, whereby use of a first line agent, a generic alternative, is required prior to coverage of a second line agent, usually a branded product, can be a useful strategy in increasing drug cost savings [29].
Approximately 80 percent of prescriptions had a drug prescribed as an injectable, mostly antibiotics. The high percentage of injectables was quite explainable since this was an inpatient study with patients mostly having acute illnesses. Injectable drugs are associated with problems of administration and medication errors [30]. Hence, the need to switch over to other routes of administration as soon as possible needs to be emphasised.
Seventy eight percent of drugs prescribed were from the Indian National List of Essential Medicines, 2003 [17] which is modelled on the WHO Essential Drugs List [31]. The understanding of concept of essential medicines and their availability to different sections of society needs to be tested. One step in this direction in India was the ?Delhi model? for developing a comprehensive drug policy which aimed to improve the accessibility of essential medicines to all [32]. This model implemented a pooled procurement system of medicines, whereby government obtained medicines from manufacturers in bulk at much lower price than the market price which led to an estimated saving of nearly 30% in the annual drugs bill for the government of Delhi [32].
The average number of drugs per prescription was 3.6. Similar trend has been observed in previous studies [13,33]. Polypharmacy has a number of drawbacks like high health care costs and poor patient compliance, higher incidence of adverse events [34,35] and drug-drug interactions [18]. Hence, there is a continous need to identify predictors of polypharmacy and bring amendments in prescribing practices.
The median (range) cost per prescription in various wards ranged from INR 108 (74-225) in female medical ward to INR 3758.5 (1087?4805.5) in private ward. This amounts to a substantial burden on patient?s finances in a country like India where majority of population bears health expenses themselves.
Hence, there is a need to bring changes in the prescribing practices with particular emphasis on generic drug prescribing and restricting polypharmacy. Also, some amendments need to be incorporated in the hospital antibiotic policy. Besides, establishment of a system for provision of medicines at a subsidised rate to patients might prove a useful step towards decreasing costs of health care burden.
References
- Ministry of Health and Family welfare: National Health Accounts, India New Delhi: Government of India; 2006.
- WHO Collaborating Centre for Drug Statistics Methodology (2009) Guidelines for ATC classification and DDD assignment 2010. Available from: http://www.whocc.no/filearchive/publications/2010guidelines.pdf. [Last accessed on 2013 Jan 05].
- Koristkova B, Grundmann M, Brozmanova H. Differences between prescribed daily doses and defined daily doses of antiepileptics-therapeutic drug monitoring as a marker of the quality of the treatment. Int J Clin Pharmacol Ther2006;44:438-42.
- Muller A, Monnet DL, Talon D, Hénon T, Bertrand X. Discrepancies between prescribed daily doses and WHO defined daily doses of antibacterials at a university hospital. Br J Clin Pharmacol 2006;61:585-91.
- Duarte-Ramos F, Cabrita J. Using a pharmaco-epidemiological approach to estimate diabetes type 2 prevalence in Portugal. Pharmacoepidemiol Drug Saf 2006;15:269-74.
- Grimmsmann T, Himmel W. Discrepancies between prescribed and defined daily doses: A matter of patients or drug classes? Eur J Clin Pharmacol 2011;67:847-54.
- Ghosh BN, Mitra J, Das KK. Prescription habits of physicians in an urban locality. Indian J Public Health 1987;31:120-8.
- Ahmad SR, Bhutta ZA. A survey of paediatric prescribing and dispensing in Karachi. J Pak Med Assoc 1990;40:126-30.
- Phadke AR. The quality of prescribing in an Indian district. Natl Med J India 1996;9:60-5.
- Gupta N, Sharma D, Garg SK, Bhargava VK. Auditing of prescriptions to study utilization of antimicrobials in a tertiary hospital. Indian J Pharmacol 1997;29:411-5.
- Ansari KU, Singh S, Pandey RC. Evaluation of prescribing pattern of doctors for rational drug therapy. Indian J Pharmacal 1998;30:43-6.
- Shewade DG, Pradhan SC. Auditing of prescriptions in a government teaching hospital and four retail medical stores in Pondicherry. Indian J Pharmacol 1998;30:408-10.
- Hazra A, Tripathi SK, Alam MS. Prescribing and dispensing activities at the health facilities of a non-governmental organization. Natl Med J India 2000;13:177-82.
- Biswal S, Mishra P, Malhotra S, Puri GD, Pandhi P. Drug utilization pattern in intensive care unit of a tertiary care hospital. J Clin Pharmacol 2006;46:945-51.
- Gupta M, Malhotra S, Chandra KK, Sharma N, Pandhi, P. Utilization of parenteral antiinfective agents in the medical emergency unit of a tertiary care hospital: An observational study. Pharmacoepidemiol Drug Saf 2004;13:653-7.
- Singh I, Mittal R, Shafiq N, Bharati B, Nigah RK, Pandhi P, et al. A drug utilization study to provide background data for bringing amendments in the drug dispensing policy of a pediatric referral center. Pharmacoepidemiol Drug Saf 2010;19:393-9.
- National List of Essential Medicine 2003. Available from: http://www. cdsco.nic.in/nedl.pdf. [Last accessed on 2011 Jan 01].
- Dhamija P, Bansal D, Srinivasan A, Bhalla A, Hota D, Chakrabarti A. Patterns of prescription drug use and incidence of drug-drug interactions in patients reporting to medical emergency. Fundam Clin Pharmacol 2013;27:231-7.
- Bansal V, Medhi B, Jose V, Pandhi P. Changing trend in the use of antimicrobials over ten years in a tertiary care hospital. Indian J Pharmacol 2011;43:365-7.
- Flemming B, Mabeck CE. Use of Antibiotics in General Practice in Denmark. Scand J Prim Health Care 1986;4:101-4.
- Gyssens IC. Quality measures of antimicrobial drug use. Int J Antimicrob Agents 2001;17:9-19.
- Mansouri MD, Cadle RM, Agbahiwe SO, Musher DM. Impact of an antibiotic restriction program on antibiotic utilization in the treatment of community-acquired pneumonia in a Veterans Affairs Medical Center. Infection 2011;39:53-8.
- Westphal JF, Jehl F, Javelot H, Nonnenmacher C. Enhanced physician adherence to antibiotic use guidelines through increased availability of guidelines at the time of drug ordering in hospital setting. Pharmacoepidemiol Drug Saf 2011;20:162-8.
- Schuetz P, Christ-Crain M, Wolbers M, Schild U, Thomann R, Falconnier C, et al. Procalcitonin guided antibiotic therapy and hospitalization in patients with lower respiratory tract infections: A prospective, multicenter, randomized controlled trial. BMC Health Serv Res 2007;7:102.
- Reinhart K, Hartog CS. Biomarkers as a guide for antimicrobial therapy. Int J Antimicrob Agents 2010;36 Suppl 2:S17-21.
- Haas JS, Phillips KA, Gerstenberger EP, Seger AC. Potential savings from substituting generic drugs for brand-name drugs: Medical expenditure panel survey, 1997-2000. Ann Intern Med 2005;142:891-7.
- Shrank WH, Hoang T, Ettner SL, Glassman PA, Nair K, DeLapp D, et al. The implications of choice: Prescribing generic or preferredpharmaceuticals improves medication adherence for chronic conditions. Arch Intern Med 2006;166:332-7.
- Nightingale SL. From the Food and Drug Administration. Promotional Practices of Pharmacy Benefits Management Companies. JAMA 1998;279:645.
- Motheral BR. Pharmaceutical Step-Therapy Interventions: A Critical Review of the Literature. J Manag Care Pharm 2011;17:143-55.
- Taxis K, Barber N. Ethnographic study of incidence and severity of intravenous drug errors. BMJ 2003;326:684.
- WHO Essential medicine list. Available from: http://www.who.int/medicines/publications/08_ENGLISH_indexFINAL_EML15.pdf [Last accessed on 2013 Jan 01].
- Chaudhury RR, Parameswar R, Gupta U, Sharma S, Tekur U, Bapna JS. Quality medicines for the poor: Experience of the Delhi programme on rational use of drugs. Health Policy Plan 2005;20:124-36.
- Junius-Walker U, Theile G, Pradier EH. Prevalence and predictors of polypharmacy among older primary care patients in Germany. Fam Pract 2007;24:14-9.
- Kojima T, Akishita M, Nakamura T, Nomura K, Ogawa S, Iijima K, et al. Association of polypharmacy with fall risk among geriatricoutpatients. Geriatr Gerontol Int 2011;11:438-44.
- Lai SW, Liao KF, Liao CC, Muo CH, Liu CS, Sung FC. Polypharmacy correlates with increased risk for hip fracture in the elderly: A population-based study. Medicine (Baltimore) 2010;89:295-9.