- *Corresponding Author:
- Monika Agarwa
Department of Psychiatry, Maulana Azad Medical College and Associated Hospital, New Delhi-110 002, India
E-mail: monika_anuj@yahoo.com
| Date of Submission | 29 July 2016 |
| Date of Revision | 22 March 2017 |
| Date of Acceptance | 19 September 2017 |
| Indian J Pharm Sci 2017;79(6): 1008-1013 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Availability and utilization of a wide variety of psychotropic drugs is associated with a wide spectrum of adverse drug reactions. To ensure the rational use of psychotropic drugs, it is imperative to monitor their pattern of use. The present study mainly focuses on the pattern of utilization of psychotropic drugs among psychiatric outpatients in a tertiary care hospital. A hospital based cross sectional study was carried out in the psychiatry outpatient department from January to December 2012. A total of 600 cases were studied. Demographic and drug related information was collected. With respect to the psychotropic drug utilization, sedative-hypnotics (42.9 %) were the most commonly prescribed group of psychotropic drugs followed by antidepressants (31.8 %), antipsychotics (19.6 %) and mood stabilizers (5.6 %). Among the sedative hypnotics, clonazepam (51.1 %) and amongst antidepressants, sertraline (28.9 %) and fluoxetine (17.3 %) were the most frequently utilized. The prescription of atypical antipsychotics like risperidone (41 %) and olanzapine (39.8 %) was predominant (95.4 %) over the typical ones. Valproate (54.7 %) was observed to have surpassed the use of lithium (32 %) as a mood stabilizer in bipolar disorders. A substantial increase in the use of anticonvulsants as mood stabilizers was observed. The use of the psychotropic drugs for different indications was in accordance to the current recommendations and guidelines. Newer drugs were being prescribed more often as compared to the conventional medications owing to their better safety and tolerability profiles. The psychotropic drug use in the health facility was a combination of rational and effective practice.
Keywords
Drug utilization, psychotropic drugs, rationality, WHO drug use indicators
Mental and behavioral disorders are prevalent worldwide. These conditions account for 12 % of the global burden of disease. It is estimated that by 2020, they will account for the loss of 15 % of the disability-adjusted life-years (DALYs) [1]. Globally, these illnesses have a point prevalence of about 10 % for adults [2]. Various epidemiological studies in India suggest the morbidity rate is of about 18-20 per thousand [2]. Pharmacotherapy, psychotherapy and psychosocial rehabilitation are the three components in the management of these disorders. Pharmacotherapy forms a significant part of the comprehensive treatment of these illnesses [1]. Antipsychotics, antidepressants, mood stabilizers and sedative-hypnotics are the main psychotropic drugs targeting the symptoms of the mental and behavioral disorders [3]. The pattern of their usage in psychiatric practice has undergone a dramatic change in the recent years [4]. This can be attributed to the development of newer agents and a broader range of indications [1]. There is very minimal data on drug utilization of psychotropic medicines particularly in Indian context. Knowledge of pattern of utilization of drugs in the general population can be achieved through conduct of drug utilization studies (DUS) [5].
For rational use of medicines, it is essential that the patients receive medication in appropriate doses for an adequate period of time, in accordance to their clinical needs. The cost of the medication should be affordable to both the patient and the community [6]. The overuse, underuse or misuse of medicines results in the wastage of resources and widespread health hazards. Hence, monitoring of drug utilization patterns helps to increase the therapeutic efficacy, provide feedback to the prescriber to ensure rational use of medicines and decrease the adverse drug reactions (ADRs).
The present study has therefore been conducted with a view to observe the pattern of drug use in psychiatry outpatient department in a tertiary care hospital. A cross sectional study was conducted in the Department of Pharmacology, Maulana Azad Medical College (MAMC) and Department of Psychiatry, GB Pant Hospital during a period from January to December 2012.
The study was approved by the Departmental Scientific Review Board and the Institutional Human Ethics Committee of MAMC. A written informed consent was then taken from the patient or their attendant before enrollment in the study. Six hundred patients of either sex, of any age and diagnosis of psychiatric illness were included in the study. A minimum of 50 prescriptions were taken once a month on a randomly chosen date for a period of 12 mo from the psychiatry outpatient department.
The date for data collection every month was chosen using a table of random numbers obtained from the departmental statistical software. Patient related and drug-related information were recorded on a structured proforma. World Health Organization (WHO) drug use indicators were determined. These indicators were prescribing indicator, patient care indicators and facility indicators as per the guidelines by WHO [7]. Based on the drug information collected, the other parameters calculated were indications for which psychotropic drugs were used in the study population, percentage utilization of major groups of psychotropic drugs, indication wise utilization of the major groups of psychotropic drugs, percentage utilization of the subgroups of the major groups of psychotropic drugs and percentage utilization of the individual drugs among the subgroups of the psychotropic drugs.
A total number of 600 patients were included from January to December 2012. Demographic profile is shown in Table 1. WHO Core Drug Indicators are shown in Table 2. It was observed that total of 1615 drugs were prescribed to these 600 patients. Depressive 177 (29.4 %) and psychotic disorders 173 (28.9 %) accounted for the major indications respectively, followed by anxiety disorders 84 (14 %), bipolar disorders 78 (13 %), other diagnoses 61 (10.2 %) and somatoform disorders 27 (4.5 %). Sedatives and hypnotics 693 (42.9 %) were the most commonly prescribed group of psychotropic drugs followed by antidepressants 513 (31.8 %, Figure 1). The maximum use of sedative hypnotics was seen in depressive disorders 220 (31.7 %) followed by psychotic illnesses 175 (25.3 %, Table 3). Among these sedative-hypnotics, benzodiazepines 558 (80.5 %) were used more frequently as compared to the non-benzodiazepines 135 (19.5 %). Clonazepam (51.1 %) and lorazepam (27.6 %) were the most commonly prescribed benzodiazepines while zolpidem (19.2 %) was the nonbenzodiazepine prescribed to the study population.
| Demographic parameter | Number (%) |
|---|---|
| Age (y) 0-19 20-39 40-59 >60 |
47 (7.8) 339 (56.5) 168 (28) 46 (7.6) |
| Sex Male Female |
309 (51.5) 291 (48.5) |
| Education Illiterate Literate |
126 (21) 474 (79) |
| Marital status Married Unmarried Widowed/ divorced |
415 (69.1) 164 (27.5) 21 (3.5) |
| Employment Employed Unemployed |
280 (46.7) 320 (53.3) |
| Family structure Nuclear Joint |
330 (55) 270 (45) |
Table 1: Demographic Profile
| Prescribing indicator | ||
|---|---|---|
| S. No | Description | Value |
| 1 | Average number of drugs per encounter | 2.69±0.86 |
| 2 | Percentage of drugs prescribed by generic name | 25.37 |
| 3 | Percentage of encounters with an antibiotic prescribed | 0.00 |
| 4 | Percentage of encounters with an injection prescribed | 0.56 |
| 5 | Percentage of drugs prescribed from essential medicine list | 87.00 |
| Patient care indicator | ||
| 1 | Average consultation time (min) | 8.25±1.5 |
| 2 | Average dispensing time (s) | 49.5±0.87 |
| 3 | Percentage of drugs actually dispensed (%) | 83.16 |
| 4 | Percentage of Patients’ knowledge of correct dosage (%) | 46.00 |
| Health facility indicator | ||
| 1 | Availability of copy of essential medicine list | Yes |
| 2 | Availability of key drugs (% of medicines available in the essential medicine list) | 94.00 |
Table 2: Who Core Drug Indicators
| Psychiatric illness | Sedatives and hypnotics N (%) |
Antipsychotic drugs N (%) |
Antidepressants N (%) | Mood stabilizers N (%) |
|---|---|---|---|---|
| Psychotic disorder | 175(25.3) | 227(71.8) | 49 (9.6) | Nil |
| Depressive disorders | 220 (31.7) | 18 (5.8) | 236 (46) | Nil |
| Bipolar disorders | 91 (13.2) | 61 (19.5) | 24 (4.7) | 90 (97.3) |
| Anxiety disorders | 110 (15.9) | 4 (1.2) | 100 (19.5) | Nil |
| Others | 97 (14) | 5 (1.6) | 104 (20.2) | 3 (2.7) |
Table 3: Use of Psychotropic Drugs in Various Psychiatric Illness
Table 1: Demographic Profile
Antidepressants were majorly used in depressive disorders 236 (46.0 %, Table 3). The percentage use of different groups of antidepressants which was observed was selective serotonin reuptake inhibitors (SSRIs) 352 (68.7 %), tricyclic antidepressants (TCAs) 125 (24.3 %), atypical antidepressants 21 (4.0 %) and serotonin-norepinephrine reuptake inhibitors (SNRIs) 15 (3 %), respectively. Sertraline (28.9 %) was the most commonly used antidepressant followed by fluoxetine (17.3 %), amitryptiline (14.0 %), escitalopram (12.3 %), paroxetine (9.2 %), dosulepin (4.5 %), imipramine (4.3 %), mirtazapine (3.8 %), desvenlafaxine (1.7 %), venlafaxine (1.0 %), duloxetine (1.0 %), doxepin (0.7 %), clomipramine (1.0 %) and milnacipran (0.5 %), respectively.
Antipsychotics were used most commonly in psychotic disorders 227 (71.8 %) followed by bipolar disorders 61 (19.5 %, Table 3). Among these antipsychotics, atypical agents 301 (95.4 %) were prescribed more frequently as compared to the typical antipsychotics 15 (4.6 %). Ten different antipsychotic drugs were used, which included six atypical agents namely risperidone (41 %), olanzapine (39.9 %), amisulpiride (6.5 %), quetiapine (4.9 %), clozapine (2.3 %), and aripiprazole (0.8 %). The four typical antipsychotics used were fluphenazine (1.5 %), trifluperazine (1.2 %), pimozide (1.2 %) and haloperidol (0.8 %).
Amongst the mood stabilizers, sodium valproate 51 (54.7 %) was the most commonly used drug followed by lithium 30 (32 %), carbamazepine 7 (8 %) and lamotrigine 5 (5.3 %), respectively, which were used for the treatment of bipolar disorders 90 (97.3 %). Valproate was also used for the treatment of other conditions like migraine and chronic daily headache (2.7 %).
Majority of the patients in our study were in the age group of 20-39 y 339 (56.5 %) followed by 40-59 y 168 (28.0 %, Table 1). This is in tune with a study of psychotropic drug utilization among the psychiatry outpatients in a tertiary hospital in Rajkot by Piparva et al. [8]. The third most common age group of patients was below 20 y of age (7.8 %). The prevalence of psychiatric illnesses in this age group is due to a transition from childhood and adolescence to adulthood, increasing the susceptibility for mental illnesses [1]. Patients over 60 y of age comprised 7.6 % of the study population. It is observed that psychiatric disorders may go undetected in this age group and these get confused with natural process as a part of the ageing [1]. Males (51.5 %) were observed to be only marginally exceeding the females (48.5 %) our study population. Similar findings were observed in the study by Piparva et al. [8].
The health seeking behaviour is observed more in the literate population [9]. The findings in our study corroborate with this statement as most of the patients 474 (79 %) were literate. In our study population, 415 (69.1 %) of the individuals were married while 164 (27.3 %) were unmarried and 21 (3.5 %) were widowed and divorced. Three hundred twenty (53.3 %) of the population was unemployed (Table 1). The demographic characteristics such as unemployment, marital distress have been found to have an association with the occurrence of psychiatric illnesses [9]. In the present study, about 330 (55 %) of the patients lived in a nuclear family. The stable family structure has a bearing on recovery from all illnesses and particularly more from psychiatric diseases [9].
In the outpatient department of our hospital, on an average 2.69 drugs were prescribed per encounter. This number is much lesser than that observed in a study conducted by Jhanjee et al. in patients with psychotic disorders. In this study this number was 6.24 [10]. Higher number of drugs per encounter increases the risk of drug interactions, dispensing error, patient not knowing correct dosage schedule, patient noncompliance and increased cost.
In the study, 410 (25.37 %) of the total drugs were prescribed by their generic names which is similar to that obtained (25.12 %) in a study to assess prescribing trends among the outpatients at two tertiary hospitals in Delhi by Biswas et al. [11]. Prescribing by generic names decreases the cost of treatment which is pertinent for a country like India which faces cost restraints due to low socioeconomic status of most of our patients. There were no encounters with antimicrobial agents in addition there was no prescription of fixed dose combination. Such results seem to depict the judicious use of medicines.
The percentage of encounters with an injectable prescribed was as low as 9 (0.67 %). It is a step forward in reducing irrational use of injections, blood borne infections, cost and discomfort to the patients affecting their compliance to treatment [6]. Though maximum drugs 1405 (87 %) were prescribed from essential medicine list (EML) in our study, still there is considerable scope for improving this number.
The consultation time in our study was estimated to be 8.25 min on an average. Review of literature shows that such consultation time has not been recorded in any other study. Psychiatric illnesses are unique as the assessment of the illness and wellbeing of the patient is largely based on communication between the doctor and the patient much more than any other illness. However, due to constraints of resources, manpower and patient overload, consultation time with the prescriber is largely compromised. On an average, the pharmacist took 49.5 s to dispense drugs to a patient. This duration is greater than those observed in Bangladesh (23 s) and Nigeria (13 s) [12]. The findings in our study suggest that in comparison with other studies the pharmacists in the present study gave more time to the patients. In our study, 83.16 % of the drugs were dispensed from the hospital pharmacy. This finding signifies the presence of a robust EML.
The patient’s knowledge of right dose of their medication was lacking. Only 276 (46 %) of the patients had enough knowledge of the amount of drug to be taken and at what time intervals. This finding is however, low as compared to that observed (67 %) in a study by Tekur et al. to monitor the impact of an interventional program on drug utilization in a tertiary care hospital in Delhi [13]. This can be improved by increasing the awareness of the pharmacist to communicate effectively to the patient about the right dose, duration and frequency of drug administration. However, the patient overload and scarcity of manpower are the impediments to the above practice in the present setting.
A copy of the EML of the hospital was available at the hospital pharmacy. About 94 % of the medicines present in the EML were available in the hospital pharmacy. This leads to decrease cost of treatment to the patient as well as increase in compliance to treatment [6].
Sedative and hypnotics (42.9 %) were the most commonly prescribed psychotropic drugs in our psychiatric outpatient clinic. Similar finding was observed in a cross sectional psychiatric epidemiological study regarding use of psychotropic drugs in Europe by Alonso et al. [14] and Piparva et al. [8]. Sedatives and hypnotics were found to be widely prescribed amongst the different illnesses like insomnia, anxiety and agitation. In our study, the maximum utilization of these medications was observed in depressive disorders (31.7 %). Although antidepressants are effective for both core symptoms of depression and coexisting anxiety but they have a lag period and take time to set in. As a result, benzodiazepines may be prescribed for immediate relief [15]. SSRIs and SNRIs are considered to be the firstchoice drugs for the treatment of anxiety disorders [16]. However, sedative and hypnotics are still commonly used for the treatment of anxiety disorders because of their rapid onset of action, good efficacy and a favorable side effect profile [16]. Benzodiazepines (80.5 %) were used more frequently in comparison to the non-benzodiazepines (19.5 %) in our study as reported in other studies from India [8,17]. Clonazepam (51.1 %) was the single most commonly prescribed drug in our study. It was also observed in a drug utilization study of psychotropic drugs in Nagpur by Deshmukh and Ismail [18] possibly because of its potential to act as a psychotherapeutic adjunct in different psychiatric conditions.
Antidepressants were the second most commonly prescribed group of psychotropic medications (31.76 %) in our study with the maximum utilization for depressive disorders followed by anxiety disorders. These medications are considered to be the first line agents for the treatment of depression (46.0 %) and anxiety disorders (19.5 %) [19]. Moreover, they are considered to be among the most effective anxiolytic agents available. Use of antidepressants is however, associated with switching into mania or rapid cycling phase in bipolar disorders. Despite the lack of evidence of any benefit in bipolar depression as well as their nonapproval for use by US Food and Drug Administration (FDA) in this particular condition, antidepressants are being used [9,19].
In this study, the use of SSRIs (68.7 %) predominated over other group which is in tune with a study of dispensing of psychotropic drugs in Australia from 2000 to 2011 by Stephenson et al. [20]. Relatively lower needs for dose titration as well as lower incidence of ADRs are the main reasons for the preferred use of SSRIs over other antidepressants [21]. The high prevalence of utilization of TCAs (24.3 %) in our study is because of the use of their lower doses for the treatment of somatic symptoms like headache as well as due to the fact that TCAs were continued to be used in patients who were already receiving these drugs and were adequately responding to them.
Sertraline (28.9 %) was the most common anti depressant prescribed similar to the study of drug utilization of psychotropics in Australia [20]. Sertraline is the preferred antidepressant over other SSRIs due to fewer drug interactions as compared to others [19]. Antipsychotics were the third most commonly prescribed psychotropic drugs mainly for the treatment of schizophrenia and other psychotic disorder (71.8 %) in the study. The treatment of manic phase of bipolar disorders with lithium or valproate along with antipsychotics is associated with greater efficacy as compared to treatment with single agent alone [22].
Their use in other psychiatric conditions is for the treatment of comorbid psychotic symptoms. Among the antipsychotics, the use of atypical antipsychotics (95.4 %) far exceeded that of the typical ones (4.6 %). This may be explained by their role in the treatment of negative symptoms as well as drug resistant cases of schizophrenia and lesser association with extrapyramidal side effects [23]. Risperidone (41 %) and olanzapine (39.8 %) were the most preferred antipsychotics. Similar finding was also seen in a pharmacoepidemiological study of drug use in Manipal by Raut et al. [17]. The preference maybe attributed to fact that atypical antipsychotics are available since a long time in the market hence the wide knowledge about their indications and dose ranges in the literature may make psychiatrists more comfortable in prescribing these drugs [24].
Amongst the mood stabilizers, valproate (54.7 %) was more frequently prescribed as compared to lithium (32 %), carbamazepine (8 %) and lamotrigine (5.3 %). Bipolar disorders were the indication for the use of mood stabilizers. There has been a substantial increase in the use of anticonvulsants as mood stabilizers. This was reflected in the study of prescription pattern in bipolar disorders in US by Baldessarini et al. [25].
In this drug utilization study, the use of the psychotropic drugs for different indications was in accordance to the current recommendations and guidelines. Newer drugs were being prescribed more owing to their better safety and tolerability profiles. Despite the low prevalence of generic prescribing, utilization of medications was in accordance to the concept of essential medicines. The consultation and dispensing time were largely compromised owing to the patient overload and crunch of resources.
The database regarding the drug utilization of the psychotropic drugs needs to be strengthened further by the conduct of similar studies on larger study population.
Conflict of interest
The authors declare that they have no conflict of interest.
Financial support and sponsorship
Nil.
References
- http://www.who.int/whr/2001/en/whr01_en.pdf.
- Park K. Mental Health. In: Park’s Textbook of Preventive and Social Medicine. 20th ed. Jabalpur: BanarsidasBhanot Publishers; 2009. p.734-41.
- http://apps.who.int/iris/bitstream/10665/70640/1/a95053_eng.pdf.
- Pincus HA, Tanielian TL, Marcus SC, Olfson M, Zarin DA, Thompson J, et al. Prescribing trends in psychotropic medications: primary care, psychiatry, and other medical specialities. JAMA 1998;279:526-31.
- http://apps.who.int/medicinedocs/pdf/s4876e/s4876e.pdf.
- http://apps.who.int/medicinedocs/pdf/whozip23e/whozip23e.pdf.
- http://apps.who.int/medicinedocs/pdf/s2289e/s2289e.pdf.
- Piparva KG, Parmar DM, Singh AP, Gajera MV, Trivedi HR. Drug utilization study of psychotropic drugs in outdoor patients in a teaching hospital. Indian J Psychol Med 2011;33:54-8.
- Kessler RC. Sociology and Psychiatry. In: Benjamin SJ, Sadock VA editors. Kaplan &Sadock’s Comprehensive Textbook of Psychiatry. Philadelphia: Lippincott Williams and Wilkins; 2009. p. 708-16.
- Jhanjee A, Bhatia MS, Oberoi A, Srivastava S. Medication errors in psychiatric practice - A Cross sectional Study. Delhi Psychiatry J 2012;15:5-13
- Biswas NR, Biswas RS, Pal PS, Jain SK, Malhotra SP, Gupta A, et al. Patterns of prescriptions and drug use in two tertiary hospitals in Delhi. Indian J Physiol Pharmacol 2000;44:109-12.
- Hogerzell HV, Bimo, Ros-Degnan D, Laing RO, Ofori-Adjel D, Santoso B, et al. Field tests for rational drug use in twelve developing countries. Lancet 1993;342:1408-10.
- Tekur U, Kalra BS. Monitoring an interventional programme of drug utilization in a health facility of Delhi. Indian J Med Res 2012;135:675-7.
- Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, et al. Psychotropic drug utilization in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. ActaPsychiatrScandSuppl 2004;109:55-64.
- Cloos JM, Ferreira V. Current use of benzodiazepines in anxiety disorders. CurrOpin Psychiatry 2009;22:90-5.
- Ursano RJ, Bell C, Eth S, Friedman M, Norwood A, Pfefferbaum B, et al. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Am J Psychiatry 2004;161:3-31.
- Raut P, Adiga S, Mohan L, Maheshwari B, Dhirhe T. Pharmacoepidemiology of drugs utilized in psychiatry department of Kasturba Hospital, Manipal, Karnataka. Int J Pharm Sci Rev Res 2011;7:89-92.
- Deshmukh SA, Shaikh Ismail TSE. Evaluation of psychotropic drugs use pattern among outpatients attending psychiatry department at Government Medical College and Hospital, Nagpur: a cross sectional study. Int J Pharm Bio Sci 2012;3:428-36.
- De Battista C. Antidepressant Agents. In: Katzung BG, Masters SB, Trevor AJ, editors. Basic & Clinical Pharmacology. New York: The McGraw-Hill Companies; 2012. p. 521-42.
- Stephenson CP, Karanges E, McGregor IS. Trends in the utilisation of psychotropic medications in Australia from 2000 to 2011. Aust N Z J Psychiatry 2013;47:74-87.
- Bech P, Ciadella P, Haugh MC, Birkett MA, Hours A, Boissel JP, et al. Meta-analysis of randomized controlled trials of fluoxetine v. of major depression placebo and tricyclic antidepressants in the short-term treatment. Br J Psychiatry 2000;176:421-8.
- Cookson J. Atypical antipsychotics in bipolar disorder: the treatment of mania. AdvPsychiatr Treat 2008;14:330-8.
- Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM, et al. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet 2009;373:31-41.
- Apiquian R, Fresán A, de la Fuente-Sandoval C, Ulloa RE, Nicolini H. Survey on schizophrenia treatment in Mexico: perception and antipsychotic prescription patterns. BMC Psychiatry 2004;4:12.
- Baldessarini RJ, Leahy L, Arcona S, Gause D, Zhang W, Hennen J. Patterns of psychotropic drug prescription for U.S. patients with diagnoses of bipolar disorders. PsychiatrServ 2007;58:85-91.
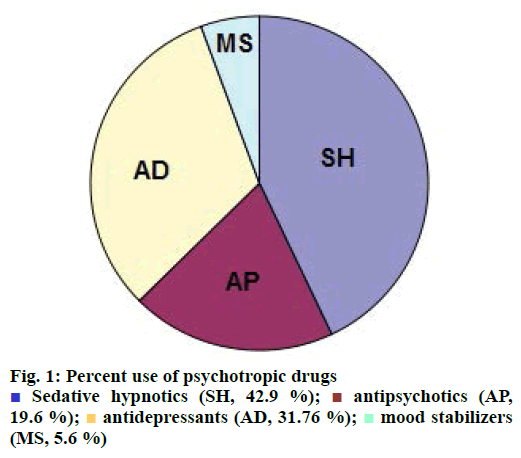
 Sedative hypnotics (SH, 42.9 %);
Sedative hypnotics (SH, 42.9 %);  antipsychotics (AP, 19.6 %);
antipsychotics (AP, 19.6 %);  antidepressants (AD, 31.76 %);
antidepressants (AD, 31.76 %);  mood stabilizers (MS, 5.6 %)
mood stabilizers (MS, 5.6 %)