- *Corresponding Author:
- D. Padmini Devi
Department of Pharmacology, 1Department of General Surgery, St. John’s Medical College, Bengaluru-560 034, India
E-mail: p_nidhin@hotmail.com
| Date of Submission | 22 July 2016 |
| Date of Revision | 18 February 2017 |
| Date of Acceptance | 27 July 2017 |
| Indian J Pharm Sci 2017;79(5):778-784 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Polypharmacy is the use of 5 or more medications per day and high level polypharmacy is the use of 10 medications or more per day by a patient. Perioperative patients form a significantly large population who are prescribed additional drugs for pain relief and infection prophylaxis. This study is aimed to estimate the prevalence of polypharmacy among perioperative elderly patients and to determine the predictors and outcomes of polypharmacy. This was a prospective observational study conducted among elderly patients aged 60 years or more who were admitted to the surgical wards for elective or emergency surgical procedures at a tertiary care teaching hospital from May 2014 to April 2015. Data were collected using a structured case report format. Descriptive statistics were used to summarise demographic characteristics, prescription patterns and outcomes. Predictors were evaluated using univariate analysis followed by regression analysis. About 135 patients were screened and 117 patients were included in the study. Prevalence of polypharmacy was 84.6% and prevalence of high level polypharmacy was 11.1%. The most common drugs related to surgery being used were pantoprazole (87.2%), pethidine (64.1%) and ondansetron (46.2%). Whereas, the most common surgery unrelated drugs prescribed were short acting human insulin (36.8%), amlodipine (29.1%) and metformin (22.2%). The number of adverse drug reactions encountered in our study was 7 and none was life threatening. The duration of hospital stay (adjusted odds ratio; 95% confidence intervals: 2.505; 1.239, 5.064) and number of co-morbidities (adjusted odds ratio; 95% confidence intervals: 1.927; 1.057, 3.514) were the significant predictors of polypharmacy. In conclusion, polypharmacy was high among elderly perioperative patients in our setting. Comorbidities and prolonged duration of hospital stay were important predictors of polypharmacy in elderly surgical patients.
Keywords
Elderly, geriatrics, perioperative, polypharmacy, prescriptions, surgical unit
The term ‘elderly’ or ‘geriatrics’ refers to a population with a chronological age of more than 65 y in most of the developed nations while this does not adapt very well to the underdeveloped or developing nations [1]. The United Nations thus recommends no standard numerical criterion but agreed a cut-off of more than 60 y as elderly population [1]. In January 1999, the Government of India adopted the “National Policy on Older Persons” by which ‘senior citizen’ or ‘elderly’ is defined as persons who are of the chronological age of 60 y or above [2]. Based on the 2011 census, the number of elderly living in India is 103.8 million (10.38 crores), which corresponds to 8.6% of the total population [2].
Polypharmacy as such has no standard definition but is generally referred as taking multiple medications together usually 5 or more per day and/or administration of more medications than that are clinically warranted indicating unnecessary or unwanted drug use [3]. High level of polypharmacy is defined as intake of 10 or more drugs [3]. In United States of America (USA), approximately one-third of all prescription drugs are consumed by the elderly who contribute a mere 13% of the population [4]. The scenario is not much different among the elderly in India. A study done in Tamilnadu revealed that 58.23% of all prescriptions to the elderly had therapeutic polypharmacy [5]. The major concern with polypharmacy is its propensity to cause adverse drug reactions (ADRs). ADRs are more so in the elderly due to certain metabolic changes and reduced drug clearance associated with ageing combined with increasing number of medications [6]. Off late surgical procedures have become an integral part of the global health care with an estimated 234 million major surgical procedures performed annually worldwide [7]. An urban study in Delhi, the capital city of India, reports that approximately 12% of the entire population has undergone at least one form of a major surgical procedure in their life time [8].
Pharmacotherapy in surgical patients includes analgesics to tackle pain and antibiotics to prevent surgical site infections. However, studies done in the past have shown that up to 44% of surgical patients may be taking medications unrelated to surgery at the time of admission irrespective of the nature and complexity of the surgery [9]. However, nearly one-fourth of patients undergoing major surgery are already on long term medications which is more so among the elderly and thereby increasing the propensity of polypharmacy [10]. Previous Indian studies have not addressed the problem of polypharmacy among elderly perioperative patients to the best of our knowledge and hence in this study we propose to ascertain the prevalence of polypharmacy among elderly perioperative patients in a tertiary teaching care hospital and to assess the predictors and outcomes of polypharmacy in the same population.
Materials and Methods
This is a prospective observational study conducted in the Department of General Surgery, St. John’s Medical College Hospital, a tertiary care teaching hospital. This hospital is a 1200 bedded facility performing an average of 150 surgeries per month under general surgery department. The duration of the study was one year from May 2014 to April 2015. All consenting elderly patients above the age of 60 y admitted to the Department of General Surgery irrespective of whether elective or emergency surgery were included in the study. Day care surgical patients and critically ill patients who were unable to answer were excluded from the study.
Assuming the prevalence of polypharmacy among elderly patients to be around 58% (p) based on a previous study done among elderly patients in Tamilnadu state [5], the sample size calculated with an absolute precision (d) of 10% using the formula 4p(100-p)/d2 [11] was 98. Accounting for non-responders, it was decided to increase the sample size to 110 elderly patients. Ethics approval was obtained from the Institutional Ethics Committee of our hospital (reference number: 26/2014).
Consecutive sampling was done wherein all eligible elderly patients who fulfilled the eligibility criteria were considered. A participant information sheet describing the benefits and risks of the study was distributed to the patient and a written informed consent was obtained using a language of patient’s own understanding. A semi structured standardized questionnaire was used to collect demographic details, clinical diagnosis and medication history from admission until discharge from the daily treatment chart and discharge summary. When necessary, patients were interviewed for any clarification. Data entry was done in Epi Info™ Version 7 (CDC, USA) and analysis was performed with SPSS Version 20.0 (IBM Corp., USA). Patterns and outcomes of polypharmacy were summarised using descriptive statistics and predictors were analysed using univariate analysis followed by regression analysis. A P value of <0.05 was considered significant for all statistical tests.
Results and Discussion
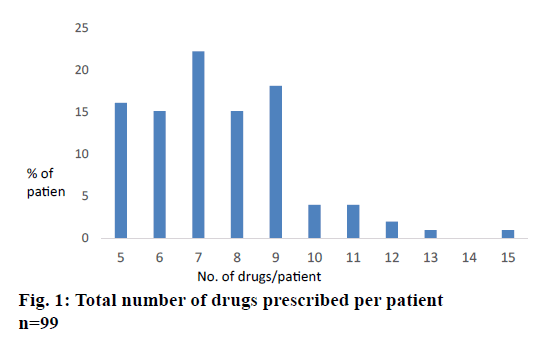
A total of 135 elderly patients were screened for eligibility and only 117 were included in the study as 6 patients were critically ill unable to answer and 12 patients did not give consent. The mean (SD) age of the patients included was 67.4 (7.07) y. The mean (SD) of duration of hospital stay was 10.00 (6.52), the minimum being 2 d and maximum being 38 d. Majority of our study participants were from urban population (59%) and were men (72.6%) with at least half the patients suffering from diabetes (56.4%) and hypertension (51.3%) as shown in Table 1. The number of co-morbidities per each patient is depicted in Table 2. Out of 117 patients, 45.3% underwent a major surgical procedure, while 35.9% and 18.8% underwent an intermediate and minor surgical procedure, respectively. Major surgeries include those like exploratory laparotomy, hernioplasty, cholecystectomy, gastrectomy and likewise. While intermediate procedures include appendectomy, debridement under anaesthesia, split thickness skin grafting, sphincterotomy, fistulectomy, below-knee amputation, exploration under anaesthesia and minor procedures include simple excision, incision and drainage and secondary suturing (Table 3). Prevalence of polypharmacy (≥5 drugs) was 84.6% with prevalence of high level polypharmacy (≥10 drugs) at 11.1%. Figure 1 depicts the entire spectrum of number of drugs per individual patient with polypharmacy. Table 4 describes the patterns of surgery-related and non-surgery related drugs prescribed in our study population. Surgery related drugs are those which were given to patients during perioperative period solely as a result of surgery like analgesic, antibiotics and likewise which are expected to be stopped as the patient returns back to normal life. Surgery unrelated drugs were defined as those the patient had already been taking as a result of his/her chronic medical condition like antidiabetic or antihypertensive medications [9]. The most common drugs related to surgery being used were pantoprazole (87.2%), pethidine (64.1%) and ondansetron (46.2%), whereas the most common surgery unrelated drugs prescribed being fast acting human insulin (36.8%), amlodipine (29.1%) and metformin (22.2%). The maximum number of antibiotics prescribed to a single patient at a time was 3. Three patients (2.6%) received 3 antibiotics simultaneously namely amikacin, metronidazole and one of the cephalosporins. About 48 (41%) patients received 2 antibiotics, 41 (35%) received one antibiotic and 25 (21.4%) patients received no antibiotic prophylaxis. The number of ADRs encountered in our study patients was 7 of which 6 of them were encountered in patients who had therapeutic polypharmacy (Table 5). None of the ADRs reported were life-threatening that had the potential to cause symptoms, which if not treated would put the patient at risk of death. Table 3 lists the various ADRs encountered in the study in descending order based in their occurrence. Factors like age, sex, duration of hospital stay, number of comorbidities and complexity of surgeries (independent variables) were analysed initially using univariate analysis and those that had a significance value of ≤0.2 were subjected to logistic regression analysis (Table 6). The dependant variable considered was a dichotomous variable–presence or absence of polypharmacy. The duration of hospital stay (adjusted odds ratio (aOR); 95% confidence intervals (95% CI): P value: 2.505; 1.239, 5.064: 0.048) and number of co-morbidities (aOR; 95% CI: 1.927; 1.057, 3.514: 0.019) were statistically significant. Complexity of the procedure was not statistically significant (P=0.633).
| Variable | All patients | Patients with polypharmacy | |
|---|---|---|---|
| Frequency* (%) | Frequency# (%) | ||
| Age | 60-74 y | 92 (78.6) | 78 (78.8) |
| ≥75 y | 25 (21.4) | 21 (21.2) | |
| Gender | Male | 85 (72.6) | 72 (72.7) |
| Female | 32 (27.4) | 27 (27.3) | |
| Residence | Urban | 69 (59.0) | 58 (58.6) |
| Rural | 48 (41.0) | 41 (41.4) | |
| Comorbidities | Diabetes | 66 (56.4) | 60 (60.6) |
| Hypertension | 60 (51.3) | 58 (58.6) | |
| Lung disorders | 12 (10.2) | 11 (11.1) | |
| Ischaemic heart disease | 8 (6.8) | 6 (6.1) | |
| Chronic kidney disease | 5 (4.3) | 4 (4.0) | |
| Type of surgery | Major | 53 (45.3) | 42 (42.4) |
| Intermediate | 42 (35.9) | 37 (37.4) | |
| Minor | 22 (18.8) | 20 (20.2) | |
| Duration of hospital stay | ≤7 days | 51 (43.6) | 42 (42.4) |
| 8–14 days | 41 (35.0) | 35 (35.4) | |
| >14 days | 25 (21.4) | 22 (22.2) | |
*Total number of patients (n)=117. #Total number of patients with polypharmacy (n)=99
Table 1: Demographic characteristics of the study population
| Number of comorbidities | All patients | Patients with polypharmacy |
|---|---|---|
| Frequency* (%) | Frequency# (%) | |
| 0 | 20 (17.1) | 10 (10.10) |
| 1 | 42 (35.9) | 36 (36.36) |
| 2 | 35 (29.9) | 33 (33.33) |
| 3 | 16 (13.7) | 16 (16.16) |
| 4 | 4 (3.4) | 4 (4.04) |
*Total number of patients (n)=117. #Total number of patients with polypharmacy (n)=99
Table 2: Number of comorbidities in a patient
| Types of surgery | All patients | Patients with polypharmacy |
|---|---|---|
| Frequency* (%) | Frequency# (%) | |
| Major surgeries | ||
| Hernia repair | 16 (13.68) | 10 (10.10) |
| Laproscopic abdominal procedures | 16 (13.68) | 12 (12.12) |
| Laparotomy | 10 (8.5) | 10 (10.10) |
| Open cholecystectomy | 5 (4.27) | 4 (4.04) |
| Gastrectomy | 4 (2.56) | 4 (4.04 |
| Nephrectomy | 1 (0.85) | 1 (1.01) |
| Mastectomy | 1 (0.85) | 1 (1.01) |
| Intermediate surgeries | ||
| Amputation | 16 (13.68) | 13 (13.13) |
| Debridement | 11 (9.40) | 10 (10.10) |
| Split thickness skin grafting | 9 (7.69) | 8 (8.08) |
| Haemorrhoidectomy | 2 (1.71) | 2 (2.02) |
| Trendelberg’s procedure | 2 (1.71) | 2 (2.02) |
| Jabolays procedure/hydrocoelectomy | 2 (1.71) | 2 (2.02) |
| Minor surgeries | ||
| Incision and drainage | 12 (10.26) | 12 (12.12) |
| Simple excision | 7 (5.98) | 6 (6.06) |
| Secondary suturing | 2 (1.71) | 2 (2.02) |
| Incisional biopsy | 1 (0.85) | 0 (0) |
Table 3: Frequency of specific types of surgery
| Drug | Frequency* (%) |
|---|---|
| Surgery related drugs | |
| Pantoprazole | 102 (87.2) |
| Pethidine | 75 (64.1) |
| Ondansetron | 54 (46.2) |
| Paracetamol | 47(40.2) |
| Tramadol | 37 (31.6) |
| Metronidazole | 24 (20.5) |
| Ciprofloxacin | 24 (20.5) |
| Surgery unrelated drugs | |
| Human insulin (fast acting) | 43 (36.8) |
| Amlodipine | 34 (29.1) |
| Metformin | 26 (22.2) |
| Human insulin (Intermediate/long acting) | 17 (14.5) |
| Dalteparin | 14 (12) |
*Total number of patients (n)=117
Table 4: Prescription pattern during perioperative period in elderly
| ADR | Frequency | Causality (WHO) |
|---|---|---|
| Thiazide-induced hyponatremi | 3 | Possible |
| Amikacin-induced nephrotoxicity | 2 | Probable |
| Ceftriaxone-induced rash | 1 | Probable |
| Enoxaparin-induced ecchymosis | 1 | Probable |
Total number of ADRs=7
Table 5: List of adrs in descedning order of occurrence
| Variable | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| Unadjusted OR | P-value | Adjusted OR (95% CI) | P-value | |
| Increasing age | 0.991 | 0.797 | Not included | - |
| Male sex | 1.026 | 0.965 | Not included | - |
| Duration of hospital stay | 2.305 | 0.071 | 2.505 (1.239, 5.064) | 0.048 |
| Comorbidities | 1.380 | 0.011 | 1.927 (1.057, 3.514) | 0.019 |
| Complex surgery | 1.707 | 0.158 | 1.213 (0.549, 2.680) | 0.633 |
OR: odds ratio; CI: confidence interval
Table 6: Predictors of polypharmacy
The problems faced by the elderly are unique as they are physiologically and psychologically very different from their younger counterparts and the function of various organ systems declines with ageing thereby producing a different constellation of diseases warranting multiple medications. Thus, therapeutic polypharmacy and resulting adverse reactions or drugdrug interactions among elderly patients is common [12]. Further to this, perioperative patients constitute a unique population. There is increased body fat and decreased total body water and muscle mass leading to many of the pharmacokinetic changes and there is increased sensitivity to certain drugs. Hepatic and renal function changes alter the drug metabolism and elimination during the perioperative period and gastrointestinal absorption of oral medications may be impaired due to changes in splanchnic blood flow [13]. All of these may lead to an increase in unwanted drug effects or side effects.
Prevalence of polypharmacy in our study population was 84.6%, which is very high when compared to that reported by Gopinath et al. [5]. This is because our study was performed among perioperative elderly patients as against the latter which included mostly non-surgical elderly patients. However, this high prevalence is comparable to the other similar studies. A study done in Chidambaram, Tamilnadu reported that 88.26% of all prescriptions to elderly had polypharmacy [14]. In the last decade, data from the west suggest that 20% of elderly people above the age of 70 y consume 5 or more drugs to combat a myriad of chronic diseases [15]. Thus it is quite evident that the problem of polypharmacy and its ill effects among elderly is quite prevalent globally and more so during the perioperative period. This problem is more severe in smaller set-ups where there are no senior physicians with expertise in dealing with geriatric patients who would be better able to tackle polypharmacy but at the same time prescribe rationally [5].
Polypharmacy is an established risk factor for ADRs and there is evidence that increasing number of drugs causes increased incidence of ADRs [16]. ADRs due to drug-drug interactions are a common cause of admission to the hospital and are an important cause of mortality and morbidity. Studies done after 1985 have shown that the ADR rate in European and American geriatric settings are greater by at least 20% when compared to the general medicine setting [17]. Another 4-y prospective study done among geriatric residents of nursing homes from USA has reported that the mean number of drugs per patient in the ADR group was 7.8 while the mean number of drugs in the remaining geriatric population was a mere 3.3 [18]. Having said that the number of ADRs reported in our study was less in number (7 ADRs) and they were non-life threatening. This is possibly because our institution is a tertiary care referral centre, having in-house round the clock experienced surgeons and physician to analyse the risk situations for an ADR and appropriately prescribed medications thereby mitigating an ADR. There have been studies, which show that a good communication between the patient and his doctor would do good in avoiding ADR be it in the hospital or community [19]. A good doctor patient communication is achieved by the mere availability of doctors like in our setting.
In the perioperative period, there is less patient participation in one’s own medical care due to various reasons like anxiety, pain and medication including anaesthesia effect. Therefore, there are more chances of ADRs getting missed due to non-reporting. In a study comprising 2557 doses of medications administered in hospital wards, 456 errors were found by direct observation, 34 by chart review and only 1 error by self-report. Thus perioperative ADRs are usually underreported [20]. Therefore, it is important that drugs with a well-known safety profile are being used in this most crucial period [21]. Our study pointed out that the most common surgery related drugs that were used belonged to the classes of analgesics, antibiotics, antiemetics and gastroprotectants. It was by protocol that most of our patients in the surgical units receive a proton pump inhibitor unless otherwise contraindicated to tide away non-steroidal antiinflammatory drug (NSAID)- induced gastritis and the most commonly available intravenous preparation is pantoprazole. As expected, various classes of analgesics including both opiates and NSAIDs were used based on the patient characteristics, intensity of pain and individual surgeon’s preferences. Some of the common analgesics being used were paracetamol, pethidine and tramadol. Some of the more sedative drugs like morphine or fentanyl are avoided in elderly according to the department protocol due to risk of fall in elderly. Drug-induced nausea is mostly treated with ondansetron than any other class of antiemetic and thus favouring increased usage perioperatively. On the other hand, the drugs unrelated to surgery were those that are used to treat various noncommunicable diseases like diabetes, hypertension, dyslipidemia and ischaemic heart diseases. Since the prevalence of diabetes mellitus is quite high among the elderly and it is a protocol to use human insulin during the perioperative period rather than oral hypoglycemic drugs, human insulin has come out as the most common surgery unrelated drug that is being used followed by the antihypertensive amlodipine, which is a calcium channel blocker.
With regards to antibiotic usage, our study revealed that an equal number of patients received either one or two antibiotics depending on the type of surgery and surgical site. The choice of antibiotic greatly depends on the surgeon’s preference and the patient’s affordability. However, those with infected wounds were initially treated empirically with 3 antibiotics that cover Gram-positive, Gram-negative and anaerobic bacteria. However, the definitive treatment was always based on the microbial culture testing and antibiotic susceptibility testing. About a quarter of our patients did not receive a continuous dose of antibiotics but for a single dose as they underwent a minor clean surgery.
Studies done in the past have shown various factors to be predictors of polypharmacy. Some of them include comorbidities, low subjective health, over the counter drug usage [22-24]. In our study, we considered the following factors namely age, sex, duration of hospital stay, number of comorbidities and complexity of the procedure. They were subjected to univariate analysis and then a binary logistic regression model was used. It was found that the odds of polypharmacy increase approximately two and half times with an increase of one day in the total duration of hospital admission. The second predictor, which was significant, was the total number of comorbidities. As the number of comorbidities increase, the odds of polypharmacy approximately double. The third important factor, which we considered was the complexity of the procedure whether major, intermediate or minor surgery. Our results revealed that there was a 20% chance of increased risk of polypharmacy if the procedure was a major one but it did not reach statistical significance. Similarly, the other factors like increasing age and sex were also not significantly associated with polypharmacy. These could be explained probably due to the smaller sample size.
In conclusion, prevalence of polypharmacy was high (85%) in perioperative elderly patients in our setting as it was mostly unavoidable due to the multiplicity of comorbidities. However, prevalence of high level polypharmacy was quite small (11%) ADRs were very less and mostly clinically insignificant due. The duration of hospital stay (aOR: 2.505, P: 0.048) and number of co-morbidities (aOR: 1.927, P: 0.019) were the statistically significant predictors for polypharmacy in our perioperative elderly population. Since it is a challenge to avoid polypharmacy in elderly due to a high probability of multiple comorbidities, we recommend a strictly conservative and rational prescription of clinically safer drugs during the perioperative period with an aim to minimise ADRs.
Financial assistance
None.
Conflicts Of Interest
The authors declare no conflicts of interest.
References
- http://www.who.int/healthinfo/survey/ageingdefnolder/en/.
- http://mospi.nic.in/mospi_new/upload/elderly_in_india.pdf.
- Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother 2007;5(4):345-51.
- Bushardt RL, Massey EB, Simpson TW, Ariail JC, Simpson KN. Polypharmacy: misleading, but manageable. Clin Interv Aging 2008;3(2):383-9.
- Gopinath S, Rajalingam B, Sriram S, Vijayakumar S. An individual Based Study of the Geriatric Population : a Polypharmacy. Int J Pharm Pharm Sci 2011;3(4):63-6.
- Dagli RJ, Sharma A. Polypharmacy: a global risk factor for elderly people. J Int Oral Health 2014;6(6):1-2.
- Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet 2008;372:139-44.
- Bhasin SK, Roy R, Agrawal S, Sharma R. An epidemiological study of major surgical procedures in an urban population of East Delhi. Indian J Surg 2011;73(2):131-5.
- Kennedy JM, van Rij AM, Spears GF, Pettigrew RA, Tucker IG. Polypharmacy in a general surgical unit and consequences of drug withdrawal. Br J Clin Pharmacol 2000;49(4):353-62.
- Pass SE, Simpson RW. Discontinuation and reinstitution of medications during the perioperative period. Am J Health Syst Pharm 2004;61(9):899-912.
- Gogate N. Principles of sample size calculation. Indian J Ophthalmol 2010; 58:517-8.
- John NN, Kumar NA. A study on polypharmacy in senior Indian population. Int J Pharm Chem Biol Sci 2013;3(1):168-71.
- Rivera R, Antognini JF. Perioperative drug therapy in elderly patients. Anesthesiology 2009;110(5):1176-81.
- VP Maheshkumar, CK Dhanapal. Prevalence of polypharmacy in geriatric patients in rural teaching hospital. Am J Phytomed Clin Ther 2014;2:413-9.
- Rollason V, Vogt N. Reduction of polypharmacy in the elderly: a systematic review of the role of the pharmacist. Drugs Aging 2003;20(11):817-32.
- Nguyen JK, Fouts MM, Kotabe SE, Lo E. Polypharmacy as a risk factor for adverse drug reactions in geriatric nursing home residents. Am J Geriatr Pharmacother 2006;4(1):36-41.
- Routledge PA, O’Mahony MS, Woodhouse KW. Adverse drug reactions in elderly patients. Br J Clin Pharmacol 2004;57(2):121-6.
- Cooper JW. Probable adverse drug reactions in a rural geriatric nursing home population: a four-year study. J Am Geriatr Soc 1996;44(2):194-7.
- Atkin PA, Veitch PC, Veitch EM, Ogle SJ. The epidemiology of serious adverse drug reactions among the elderly. Drugs Aging 1999;14(2):141-52.
- Flynn EA, Barker KN, Pepper GA, Bates DW, Mikeal RL. Comparison of methods for detecting medication errors in 36 hospitals and skilled-nursing facilities. Am J Health Syst Pharm 2002;59(5):436-46.
- Nanji KC, Patel A, Shaikh S, Seger DL, Bates DW. Evaluation of perioperative medication errors and adverse drug events. Anesthesiology 2016;124(1):25-34.
- Ballentine NH. Polypharmacy in the elderly: maximizing benefit, minimizing harm. Crit Care Nurs Q 2008;31(1):40-5.
- Junius-Walker U, Theile G, Hummers-Pradier E. Prevalence and predictors of polypharmacy among older primary care patients in Germany. Fam Pract 2007;24(1):14-9.
- Wawruch M, Zikavska M, Wsolova L, Kuzelova M, Tisonova J, Gajdosik J, et al. Polypharmacy in elderly hospitalised patients in Slovakia. Pharm World Sci 2008;30(3):235-42.