- *Corresponding Author:
- Geetha Kandasamy
Department of Clinical Pharmacy
College of Pharmacy, King Khalid University
Abha, Kingdom of Saudi Arabia
E-mail: geethpharma@gmail.com
| Date of Received | 10 August 2020 |
| Date of Revised | 05 February 2021 |
| Date of Acceptance | 20 March 2021 |
| Indian J Pharm Sci 2021;83(2):278-283 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Analgesics, including nonsteroidal anti-inflammatory drugs, are a commonly prescribed group of drugs in clinical practice for the management of pain and inflammation. This study was carried out to evaluate the prescribing pattern for nonsteroidal anti-inflammatory drugs in the tertiary care teaching hospital. A prospective cross sectional study was conducted in the orthopaedic department of a tertiary care teaching hospital from February to December 2017. The institutional ethical committee approved the study. Patients of both genders were included in the study. Patients treated with at least one nonsteroidal anti-inflammatory drug in the outpatient department of orthopaedics were included. The prescription was compared with World Health Organization drug prescribing indicators to compare selective and nonselective nonsteroidal anti-inflammatory drugs associated with the treatment also concurrent prescription of gastro protective agents. The data collected was analysed by descriptive statistics. Chi-Square test was used to compare the difference between the two groups. A p value of <0.05 was considered significant. Out of 500 prescriptions included in the study, the total number of drugs prescribed was 1098, of which were nonsteroidal anti-inflammatory drugs. Based on the World Health Organization’s drug use indicators, the average number of drugs per encounter was 2.19 % and the average number of nonsteroidal antiinflammatory drugs per encounter was 1.38 %. Out of all the nonsteroidal anti-inflammatory drugs prescribed, 428 (62.20 %) were from National List of Essential Medicine India 2015 and 678 (98.5 %) nonsteroidal anti-inflammatory drugs were prescribed by generic name. Among the study population, only 40 % of patients were prescribed Proton Pump Inhibitors along with nonsteroidal anti-inflammatory drugs. Proton Pump Inhibitors are effective in ulcer prophylaxis in their standard dose. The present study concluded that among cyclooxygenase-1 inhibitors, Diclofenac was the most commonly prescribed nonsteroidal anti-inflammatory drugs from the national list of essential medicine. The most frequently prescribed cyclooxygenase-2 inhibitor in this study was Etoricoxib. The percentage of analgesic prescribed by generic name was excellent. However, the average number of drugs per prescription deviated from the World Health Organization’s rational drug use indicator. The use of gastro protective agents needs to be rationalised with nonsteroidal anti-inflammatory drugsy
Keywords
Non-steroidal anti-inflammatory drugs, prescription, world health organisation, indicators.
Over the past two decades, non-steroidal antiinflammatory drugs (NSAIDs) have played a central role in the treatment of pain and inflammation. NSAIDs are the largest single group of drugs used globally, constituting more than 20 % of all prescriptions [1]. It is found that more than thirty million individuals consume NSAIDs daily. Around 400 formulations of NSAIDs are marketed in India, resulting in widespread exposure of patients to this class of drugs and its adverse effects [2]. For all the above reasons, studies evaluating the pattern of prescriptions of NSAIDs are very important.
The cyclooxygenase-2 (COX-2) enzyme helps in controlling gastric mucus production, the water excretion from the kidney. It also induces platelet formation and is involved in producing prostaglandins for inflammatory response. Though there is wide clinical use of traditional NSAIDs as analgesics, anti-pyretic and anti-inflammatory agents, their gastro-intestinal toxicity is a major clinical constraint. Subsequently, selective COX-2 inhibitors have emerged as potentially gastro-friendly NSAIDs and it is believed that sufficient therapeutic benefits are achieved by selective COX-2 inhibition [3,4].
Rational drug prescribing has been the subject of several studies [5]. The World Health Organization (WHO) compiled a set of core drug use indicators that are useful for studying the prescribing patterns of drugs in healthcare settings [6,7]. Prescriptions can be used as authorised documents prescribed by a physician and the dispensing pharmacist are responsible for any misconduct in prescribing or dispensing. NSAIDs, including both traditional nonselective NSAIDs and selective COX-2 inhibitors, are among the most widely used drugs for the management of pain. Both prescription and over-the-counter NSAIDs are widely used for their anti-inflammatory and analgesic effects. NSAIDs are the essential choice in pain management because of the combined role of the COX pathway in inflammation [8].
A previous study conducted in Aden in Yemen revealed that non-selective NSAIDs were the most commonly prescribed, with diclofenac sodium being the most frequently prescribed (26.6 %), followed by meloxicam (12.8 %) and ibuprofen the least common (12 %). A combination of two non-selective NSAIDs was also reported. Selective COX-2 inhibitors were much less commonly used. This class of drug was mainly prescribed for infective conditions (29.3 %), fever (9.3 %), orthopaedic pain (8.1 %) and musculoskeletal pain (7.8 %). In general, the study concluded that there was irrational use of NSAIDs and deviation from the WHO standards regarding NSAIDs, with a high rate of NSAID prescription and low practice of prescribing drugs by generic names [9].
Similarly, an Iranian study found that the most prescribed NSAIDs was diclofenac (49.21 %), followed by ibuprofen (28.6 %) and naproxen (8 %). Prescribing two NSAIDs simultaneously was reported in 7 % of the prescriptions. General Doctors tend to prescribe NSAIDs more frequently than specialists- (67 %) and (33 %) respectively. The study reported irrational prescribing patterns in coadministration of NSAIDs and gastroprotective agents as well as NSAID combinations [10].
Another study conducted in Nigeria showed that the most commonly prescribed medicine is Aspirin (62.2 %) followed by Diclofenac potassium (13.7 %), while Tenoxicam and Piroxicam were the least prescribed (0.1 %). In contrast to the previous study, this study showed compliance with the WHO’s standards regarding prescribing patterns [11].
Rational use of drugs is essential and it has global importance. Rational drug prescribing can be defined as appropriate drugs prescribed in the right dose, at correct time intervals and for a sufficient duration. Irrational drug use is a common problem in many countries of the world. Therefore, periodic evaluation of drug utilisation patterns needs to be done to enable suitable modifications in the prescription of drugs to increase the therapeutic benefit and decrease the adverse effects in accordance with World Health Organization (WHO) drug use indicators [12]. The purpose of a drug utilisation study is to provide feedback to the prescriber and to create awareness about the rational use of medicines [13]. Hence, this study aimed to evaluate the use and prescribing pattern of NSAIDs in tertiary care teaching hospitals.
Materials and Methods
Study design and setting
This study used a prospective cross-sectional design, which was carried out in the orthopaedic out-patient department of a tertiary care teaching hospital, Tamilnadu in India, between the February and December 2017.
Study population
A total of 1695 patients visited the orthopaedic department during the study period. Out of 1695, only 1480 patients were prescribed NASIDs.
Sample size and sampling technique
The sample size was based on the number of patients visiting the out-patient orthopaedic department (1695) and determined by using a Raosoft sample size calculator (http://www.raosof.com/samplesize. html) with a predetermined margin of error of 5 % and a confidence level of 95 % [14]. In order to minimise erroneous findings and to increase study reliability, the target sample size was set at 314 participants. The number was increased to 500 patients. The institutional ethical committee approved the study. A non-random sampling procedure–i.e. a convenience sampling–was followed, as selecting a truly random sample was not possible due to the unfeasibility of constructing a sampling frame.
Population criteria
After obtaining their informed consent, patients of both genders who were prescribed at least one NSAID during the study period. Patients with severe psychiatric disorders, terminal illness and inpatients of any department were excluded from the study.
Patient data collection
Patient data were collected through data collection forms which consisted of details including the following: age, sex and drug therapy. Additional information was collected from patients’ medical records after a direct interview with the patients. The collected data was evaluated for the WHO’s prescribing indicators, indication for prescribing NSAIDs and comparison of selective and non-selective NSAIDs.
Evaluation of data
The prescription was assessed according to the WHO’s prescribing indicators [15]. ‘Average number of drugs per encounter, Percentage of encounters with NSAIDs prescribed, Percentage of encounters with an injection of NSAID prescribed, Percentage of encounters with nonselective NSAID prescribed, Percentage of encounters with COX-2 selective NSAID prescribed, Percentage of NSAIDs prescribed by generic names, Percentage of encounter with NSAIDs prescribed from National List of Essential Medicine, India (NLEM- 2015) [16], Percentage of encounter with fixed-dose combination (FDC) of NSAIDs prescribed, Percentage of encounters with NSAIDs and gastroprotective agent prescribed’.
Statistical analysis
The collected data were cleared, entered and analysed using the Statistical Package for Social Sciences (SPSS) version 24.0 for the windows. Chi-Square test was used to compare the difference between the two groups. A p value of <0.05 was considered significant. Results were described in terms of frequencies. Collected data was analysed by descriptive statistics.
Results and Discussion
This study set out with the aim of assessing the use and prescribing pattern of NSAIDs in a tertiary care teaching hospital. Out of 1695 who visited the orthopaedic department during the study period, 1480 patients were prescribed NASIDs and 500 patients were enrolled for this study. Out of 500 prescriptions included in the study, the total number of drugs prescribed was 1098, among them 688 NSAIDs. Among the 500 patients, 234 (46.8 %) were male and 266 (53.2 %) were female. The age and gender distribution of the pattern of NSAIDs prescribing is presented in Table 1. About 8.8 % (44) and 4.8 % (24) the patients were smokers and drank alcohol, respectively. The youngest age for which Diclofenac and Ibuprofen was prescribed was 17 y old and this was 22 y for Aspirin. Results showed significant differences (p<0.0001) in the frequency of NSAID prescribing according to age groups utilising the Chi-Square test. Diclofenac 148 (21.51 %) and Aceclofenac 104 (15.11%) were prescribed mostly for the adult age group, Aspirin was prescribed only to the adult age group, while Ibuprofen derivatives were prescribed mainly for adults 48 (6.97 %) and to a much lesser extent to children less than 18 y of age (2.32 %). There were no differences (p=0.193) in the pattern of prescriptions according to gender.
| NSAID | Gender | <18 y | 18-49 y | 50 or more y | Total |
|---|---|---|---|---|---|
| Aspirin | Male | 0 | 2 | 4 | 6 |
| Female | 0 | 2 | 2 | 4 | |
| Total | 0 | 4 | 6 | 10 (1.45 %) | |
| Ibuprofen | Male | 2 | 9 | 7 | 18 |
| Female | 3 | 19 | 8 | 30 | |
| Total | 5 | 28 | 15 | 48 (6.97 %) | |
| Diclofenac | Male | 3 | 43 | 24 | 70 |
| Female | 0 | 44 | 34 | 78 | |
| Total | 3 | 87 | 58 | 148 (21.51 %) | |
| Aceclofenac | Male | 0 | 22 | 33 | 55 |
| Female | 0 | 28 | 21 | 49 | |
| Total | 0 | 50 | 54 | 104 (15.11 %) | |
| Paracetamol | Male | 4 | 33 | 28 | 65 |
| Female | 2 | 29 | 24 | 53 | |
| Total | 6 | 62 | 50 | 118 (17.15 %) | |
| Etoricoxib | Male | 0 | 60 | 32 | 92 |
| Female | 1 | 65 | 40 | 106 | |
| Total | 1 | 125 | 72 | 198 (28.77 %) | |
| Etodolac | Male | 1 | 13 | 11 | 25 |
| Female | 0 | 14 | 15 | 29 | |
| Total | 1 | 27 | 26 | 54 (7.84 %) | |
| Piroxicam | Male | 0 | 3 | 2 | 5 |
| Female | 0 | 2 | 1 | 3 | |
| Total | 0 | 5 | 3 | 8 (1.16 %) |
NSAID=Non-steroidal Anti-inflammatory drug; Pearson Chi-Square statistic=122.5, p value=0.0001, for NSAID prescription in relation to age; Pearson Chi-Square statistic=9.7, p value=0.193, for NSAID prescription in relation to gender
Table 1: Prescribing Frequencies Of Non-Steroidal Inflammatory Drugs According to the Age Group and Sex of the Patients
Similar to what was observed in previous research conducted in the United Arab Emirates [16], the current study shows that the average number of drugs per encounter is 2.19 % and the average number of NSAIDs per encounter is 1.38 %. This is considered high, as the standard value recommended by the WHO for the average number of drugs per encounter is 1.6-1.8 [15]. Out of all the NSAIDs prescribed, 428 (62.20 %) were from NLEM India 2015 and 678 (98.5 %) NSAIDs were prescribed by generic name (Table 2 and Table 3). Mirroring the findings observed in a previous study conducted in India [17], the percentage of NSAIDs prescribed from the national essential drug list in the current study is suboptimal (WHO standard value is 100 %) [15]. However, the percentage of NSAIDs prescribed by generic name was satisfactory in the current study. This finding is contrary to the study by Agrawal et al. (2016), where 47.26 % of NSAIDs were prescribed by generic name [17].
| WHO core prescribing Indicators | Percentage |
|---|---|
| Average number of drugs per encounter | 2.19 |
| Average number of NSAIDs per encounter | 1.38 |
| Percentage of encounters with NSAIDs prescribed | 100 |
| Percentage of encounters with an injection of NSAID prescribed | 0 |
| Percentage of encounters with nonselective NSAIDs Prescribed | 71 |
| Percentage of encounters with selective COX-2 NSAIDs prescribed | 29 |
| Percentage of NSAIDs prescribed by generic names | 98.5 |
| Percentage of NSAIDs prescribed from NLEM | 62.2 |
| Percentage of encounters with a fixed dose combination of NSAIDs prescribed | 25.58 |
| Percentage of encounters with NSAIDs and gastroprotective agent co-prescribed | 40 |
WHO-World Health Organisation; NSAIDs-Non steroidal anti-inflammatory drugs; NLEM-National list of essential medicine
Table 2: Who Core Prescribing Indicators
| Prescribed NSAIDs, which are listed in NLEM-2015 | Number of encounters (%) | Prescribed NSAIDs, which are not listed in NLEM-2015 | Number of encounters (%) |
|---|---|---|---|
| Aceclofenac | 104 (15.11) | Etoricoxib | 198 (28.8) |
| Diclofenac | 148 (21.5) | Etodolac | 54 (7.8) |
| Paracetamol | 118 (17.1) | Piroxicam | 8 (1.2) |
| Ibuprofen | 48 (6.9) | ||
| Aspirin | 10 (1.5) |
NSAIDs-Non steroidal anti-inflammatory drugs; NLEM-National list of essential medicine
Table 3: Prescribed Nonsteroidal Anti-Inflammatory Drugs Listed and not Listed In National List of Essential Medicine 2015 [13]
The route of administration was dominated by the oral route in 360 patients (72 %), followed by oral with topical route of administration in 90 (18 %) patients and topical route in 50 patients (10 %). Thus, the oral route of administration was the most frequently prescribed.
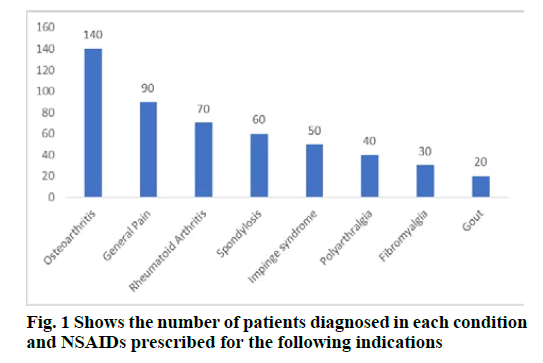
Out of 500 patients, Osteoarthritis 140 (28 %) was the most common condition for which NSAID was prescribed, followed by general pain 90 (18 %), such as post-operative pain, leg pain and joint pain, then rheumatoid arthritis 70 (14 %), impinge syndrome 50 (10 %), spondylosis 60 (12 %), post-viral polyarthralgia 40 (8 %), fibromyalgia 30 (6 %) and gout 20 (4 %) (fig.1). The present study shows osteoarthritis was the most common condition, followed by general pain, rheumatoid arthritis, soft tissue injury, spondylosis, etc.
Consistent with results observed in earlier studies, the current study revealed that the most commonly prescribed NSAID was non-selective COX 1 inhibitors [9,10,18,19,20] i.e. Diclofenac 148 (21.5 %), followed by Paracetamol 118 (17.1 %), Aceclofenac 104 (15.1 %), Ibuprofen 48 (6.9 %), Piroxicam 8 (1.2 %). The most commonly prescribed COX-2 inhibitor was Etoricoxib 198 (28.8 %), followed by Etodolac 54 (7.8 %) and Aspirin 10 (1.5 %). A previous drug utilisation study revealed that 22 % of prescriptions contain paracetamol and diclofenac. However, Aceclofenac accounted for only 1 % of NSAIDs prescription [21].
Monotherapy was given to 324 (65 %) patients, whereas a fixed dose combination of two NSAIDs was given to 176 (35 %) (Table 4 and Table 5). Among the most commonly prescribed monotherapy was Etoricoxib 148 (29.6 %), followed by Diclofenac 102 (20.4 %). However, the most commonly prescribed drug among fixed dose combinations was Aceclofenac+Paracetamol followed by Aceclofenac+Paracetamol+Rabeprazole. Fixed dose combination contributes to improved patient adherence due to the reduction in the number of pills taken by the patient [22].
| Number of encounters (%) | |
|---|---|
| Monotherapy | (n=500) |
| Diclofenac | 102(20.4) |
| Paracetamol | 12 (2.4 %) |
| Etodolac | 50 (10 %) |
| Etoricoxib | 148 (29.6 %) |
| Ibuprofen | 12 (2.4 %) |
Table 4: Monotherapy Prescribed among the Study Population
| Fixed Dose combinations of NSAIDs | Number of encounters (%) |
|---|---|
| (n=500) | |
| Aceclofenac + Paracetamol | 56 (11.2 %) |
| Aceclofenac + Paracetamol + Rabeprazole | 48(9.6 %) |
| Diclofenac &Ibuprofen | 34 (6.8 %) |
| Etoricoxib & Diclofenac | 22 (4.4 %) |
| Etoricoxib & Ibuprofen | 2 (0.4 %) |
| Etoricoxib & Aspirin | 8 (1.6 %) |
| Etoricoxib &Piroxicam | 6(1.2 %) |
| Total | 176 (35.2 %) |
Table 5: Fixed Dose Combinations of Nsaids
Among the study sample, only 40 % of patients were prescribed proton pump inhibitors (PPIs- Pantoprazole 22 %, Rabeprazole 14 %, Omeprazole 4 %) along with NSAIDs, whereas the remaining 60 % of patients were not prescribed any gastro-protective agent. Out of these 60 %, 28 % of the patients were prescribed COX- 2 inhibitors. Thus, 32 % of patients were prescribed COX-1 inhibitors without any gastro-protective agent (Table 6). Consequently, the chances of developing gastro-intestinal complications in these patients is high [23]. Inappropriate prescribing of NSAIDs in diabetes mellitus patients led to significant gastrointestinal and cardio vascular adverse events [24]. Hence, rational use and safe prescription of NSAIDs with other drugs is necessary in order to prevent or minimise the adverse effects.
| Co-prescribed Drugs | Number of patients (%) |
|---|---|
| (n=500) | |
| Pantoprazole | 110 (22 %) |
| Rabeprazole | 70 (14 %) |
| Omeprazole | 20 (4 %) |
Table 6: Gastro Protective Agents Co-Prescribed With Nsaids
The current study concludes that, among COX-1 inhibitors, Diclofenac was the most commonly prescribed NSAIDs from NLEM, and Etoricoxib was found to be the most commonly prescribed among COX- 2 inhibitors. The percentage of analgesics prescribed by generic name was appropriate, but the average number of drugs per prescription deviated from the WHO’s rational drug use indicator. The use of gastro protective agents along with NSAIDs needs to be rationalised.
A limitation of this study is that the sample was selected using a non-random sampling method, and this may have resulted in a biased sample as the intended population did not have equal sampling probability. Therefore, the study finding cannot be extrapolated to all patients prescribed NSAIDs.
Funding
This work is supported by the Dean of Scientific Research at King Khalid University, Abha, Kingdom of Saudi Arabia for the financial support is greatly appreciated for the general research project under grant number GRP/339/42, awarded to Geetha Kandasamy.
Acknowledgement
We would like to thank all the staff members of the orthopaedic department of the tertiary care teaching hospital for their support throughout the study. The authors thank the Deanship of Scientific Research at King Khalid University for providing adequate support.
Conflict of Interest
The authors declare no conflict of interest.
References
- Pincus T, Searingen C. Preference for Nonsteroidal Antiinflammatory Drugs versus Acetaminophen and Concomitant Use of Both. J Rheumatol 2000;27:1020-7.
- Paul AD, Chauhan CK. Study of usage pattern of nonsteroidal anti-inflammatory drugs (NSAIDs) among different practice categories in Indian clinical setting. Eur J Clin Pharmacol 2005;60(12):889-92.
- Graumlich JF. Preventing gastrointestinal complications of NSAIDs: risk factors, recent advances and latest strategies. Postgrad Med 2001;109(5):117-28.
- Silverstein FE, Faich G, Goldstein JL, Simon LS, Pincus T, Whelton A, et al. Gastrointestinal toxicity with celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: a randomized controlled trial. JAMA 2000;284(10):1247-55.
- Karande S, Sankhe P, Kulkarni M. Patterns of prescription and drug dispensing. Ind J Paediat 2005;72(2):117-21.
- Quick JD, Hogerzeil HV, Velásquez G, Rägo L. Twenty-five years of essential medicines. Bull World Health Organ 2002;80:913-4.
- Anonymus. Pharmacist, GP blamed for coma. The Guardian 1988:17 March.
- Wehling M. Non-steroidal anti-inflammatory drug use in chronic pain conditions with special emphasis on the elderly and patients with relevant comorbidities: management and mitigation of risks and adverse effects. Eur J Clin Pharmacol 2014;70(10):1159-72.
- Alshakka MA, Badullah WF, Alolayan SO, Mahmoud MA. Prescribing patterns of non-steroidal anti-inflammatory drugs (NSAIDs) at outpatient departments of four hospitals. Biomed Res 2018;29(19).
- Taherzadeh Z, Zeinali M, Tabeshpour J, Maziar S, Zirak M, Sent D, et al. Prescription pattern analysis of nonsteroidal anti-inflammatory drugs in the north-eastern Iranian population. J Res Pharm Pract 2017;6(4):206.
- Awodele O, Fadipe A, Adekoya M, Adeyemi O. Prescribing Pattern of Non-Steroidal Ant?inflammatory Drugs at the Outpatient Pharmacy Department of Lagos University Teaching Hospital, Nigeria. Ghana Medical Journal. 2015;49(1):25.
- Shankar PR, Pai R, Dubey AK, Upadhyay DK. Prescribing patterns in the orthopaedics outpatient department in a teaching hospital in Pokhara, Western Nepal. Kathmandu Univ Med J 2007;5(1):16-21.
- Pradhan SC, Shewade DG, Shashindran CH, Bapna JS. Drug utilization studies. Natl Med J 1988;1(4):185-9.
- www.raosoft.com/samplesize.html
- http://apps.who.int/medicinedocs/en/d/Js2289e/
- Sharif SI, Al-Shaqra M, Hajjar H, Shamout A, Wess L. Patterns of drug prescribing in a hospital in Dubai, United Arab Emirates. Libyan J Med 2008;3(1):10-2.
- Pooja A, Vijender KA. Evaluation of analgesics use in orthopedic department at tertiary care hospital in Bareilly, Uttar Pradesh, India. Int J Basic Clin Pharmacol 2016;5(6):2538-41.
- Dhananjay K, Guruprasad NB, Acharya A. A study of prescription pattern of non-steroidal anti-inflammatory drugs in medicine out-patient clinic of a rural teaching hospital. J Evol Med Dent Sci 2013;2(32):6089-97.
- http://apps.who.int/medicinedocs/en/d/Js2289e/
- Sharma T, Dutta S, Dhasmana DC. Prescribing pattern of NSAIDs in orthopaedic OPD of a tertiary care teaching hospital. J K Science 2006;8(3):160-2.
- Manohar VR, Rashmi BR, Chandrashekar R, Reefa D Souza, Mohandas Rai, Sheethal U. A prospective prescription pattern of non-steroidal anti-inflammatory drugs among general practitioners in Dakshina Kannada District of southern India. Int Res J Pharm 2015;6 (7):420-2.
- Ingle P, Patil PH, Lathi V. Study of rational prescribing and dispensing of prescriptions with non-steroidal ant-inflammatory drugs in orthopedic outpatient department. Asian J Pharm Clin Res 2015;8(4):278-81.
- Tachecí I, Bradna P, Douda T, Baštecká D, Kopá?ová M, Rejchrt S, et al. NSAID-induced enteropathy in rheumatoid arthritis patients with chronic occult gastrointestinal bleeding: a prospective capsule endoscopy study. Gastroenterology research and practice 2013:1-10.
- Mazhar F, Haider N, Sultana J, Akram S, Yousif A. Prospective study of NSAIDs prescribing in Saudi Arabia: Cardiovascular and gastrointestinal risk in patients with diabetes mellitus. Int J Clin Pharmacol Ther 2018;56(2):64.