- *Corresponding Author:
- D. V. Derle
Department of Pharmaceutics, N. D. M. V. P’s College of Pharmacy, Shivaji Nagar, Gangapur Road, Nasik-422 002
E-mail: dvderle@yahoo.com
| Date of Submission | 13 June 2005 |
| Date of Revision | 12 January 2006 |
| Date of Acceptance | 24 June 2006 |
| Indian J Pharm Sci, 2006, 68 (4): 409-414 |
Abstract
The nonsteroidal antiinflammatory drugs are among the most widely prescribed and used drugs in the community for rheumatologic as well as nonrheumatologic conditions, which include acute and chronic pain; biliary, ureteric colic; dysmenorrhoea; fever; and other applications that derive from the suppression of prostaglandin synthesis. Almost all nonsteroidal antiinflammatory drugs irritate gastric mucosa and enhance ulceration by blocking protective action of the prostaglandins on gastric mucosa, causing ulcer formation not only in stomach but also in lower part of oesophagus and in duodenum too. This review focuses on the adverse effects of nonsteroidal antiinflammatory drugs, severity of these adverse effects and attempts made to reduce the side effects through the concomitant use of other drugs.
The nonsteroidal antiinflammatory drugs (NSAIDs) possess antiinflammatory, analgesic and antipyretic activities. The Indian drug industry is always ready to cater to the needs of medical professionals by developing combinations of various kinds of drugs that are capturing substantial market share. In India, a variety of NSAID combinations are available, often as over-thecounter (OTC) products. Marketing these combinations is the easiest way of selling two drugs when one (or even none) may be needed for the patient. These combined pills are marketed with slogans like “ibuprofen for pain and paracetamol for fever” and “ibuprofen for peripheral action and paracetamol for central action.” It is indeed very unfortunate that the medical fraternity in India has fallen prey to such gimmicks. The credulous patient then has to pay for the doctors’ fees in terms of extra cost and extra adverse effects. Some of the widely used drug combinations in India are shown in Table 1.
| Combination | Strength | Dosage form |
|---|---|---|
| Ibuprofen+paracetamol | 400 mg+325 mg | Tablet |
| 400 mg+500 mg | ||
| Ibuprofen+paracetamol | 100 mg+125 mg per 5 ml | Syrup for children |
| 100 mg+162.5 mg per 5 ml | Syrup for children | |
| Ibuprofen+methocarbamol | 400 mg+750 mg | Tablet |
| Indomethacin+paracetamol | 25 mg+325 mg | Tablet |
| 25 mg+500 mg | ||
| Nimesulide+paracetamol | 100 mg+500 mg | Tablet |
| Diclofenac+paracetamol | 50 mg+325 mg | Tablet |
| 50 mg+500 mg | Tablet | |
| Diclofenac+paracetamol+dextroprophoxyphene | 50 mg+250 mg+325 mg | |
| Diclofenac+paracetamol+chlorzoxazone | 50 mg+325 mg+250 mg | Tablet |
| 50 mg+500 mg+500 mg | ||
| Diclofenac+paracetamol+chlormezanon | 50 mg+325 mg+100 mg | Tablet |
| 50 mg+500 mg+100 mg | Tablet |
Table 1: Some Nsaid Combinations Available In India’s Market
Inflammation is the body’s local response to infection or injury. It can be elicited by a variety of injurious agents, which include cold, heat, trauma, microbial invasion, etc. The function of inflammation is to destroy or inactivate the foreign invaders and/or set the stage for tissue repair. Almost all NSAIDs on long-term treatment inhibit the enzyme cyclooxygenase (COX) and production of prostaglandins. Continuous intake of NSAIDs results in gastric erosion. These can cause symptoms of an ulcer and upper gastrointestinal bleed (UGIB), which ultimately leads to death of some people. There are three basic stages of inflammation [1]. Firstly, vasodilatation and increased permeability of blood vessels, followed by phagocytic migration and finally repair.
Pain is a protective mechanism for the body. Pain differs from the other somatosensory modalities wherein emotions like fear, anxiety and feeling of unpleasantness are experienced along with the perceived sensation. The stimuli that give rise to pain result in a sensory experience plus a reaction to it. Analgesia system acts by blocking pain signals at the initial entry point to the spinal cord [2,3]. A chemical called endogenous pyrogen (EP) is released from monocytes and macrophages in the presence of infection or inflammation. EP acts upon the thermoreceptors in the hypothalamus (and perhaps other brain areas). The action of EP is mediated via local release of prostaglandin, which then directly alters central thermoreceptor function. Aspirin, ibuprofen, naproxen and acetaminophen reduce fever by inhibiting synthesis of prostaglandin.
NSAIDs can be classified [4] broadly into two types based on their chemical structure. Most NSAIDs are carboxylic acids; but a few, most noticeably phenylbutazones, are enolic acids. Carboxylic acid containing drugs include salicylate derivatives (e.g., aspirin), carbocyclic and heterocyclic acid derivatives (e.g., indomethacin), fenamic acid derivatives (e.g., mefenamic acid), propionic acid derivatives (e.g., ibuprofen, ketoprofen, fenbufen, flurbiprofen, suprofen and naproxen) and phenyl acetic acid derivatives (e.g., diclofenac, aceclofenac, etc.). Enolic acid containing drugs include oxicam derivatives (e.g., piroxicam, tenoxicam and meloxicam) and pyrazoles (e.g., phenylbutazone and oxyphenbutazone). Non-acidic group compounds include nabumenton. Based on the selectivity to cyclooxygenase (COX), NSAIDs can be classified as non-COX selective drugs, which include aspirin, indomethacin, diclofenac, piroxicam, ibuprofen, naproxen and mefenamic acid; preferential COX-2 inhibitors, which include nimesulide, meloxicam, nabumetone and aceclofenac; and highly selective COX2 inhibitors, which include celecoxib, rofecoxib, valdecoxib, parecoxib, etoricoxib and lumiracoxib.
Most of the NSAIDs have three major types of action: 1) antiinflammatory action for treating several conditions including rheumatoid arthritis, osteoarthritis, musculoskeletal disorders and pericarditis [5]. 2) Analgesia for treating pain of mild-to-moderate intensity. Their maximum therapeutic efficiency is much lower than that of the opioids, but they do not cause dependence [6]. 3) Antipyretic action, which mediates by the release of endogenous pyrogen (EP) from monocytes and macrophages in the presence of infection or inflammation. EP acts on the thermoreceptors in the hypothalamus (and perhaps other brain areas) by altering their rate of firing and their input to the integrating centres. The action of EP is mediated via local release of prostaglandin, which then directly alters central thermoreceptor function [7].
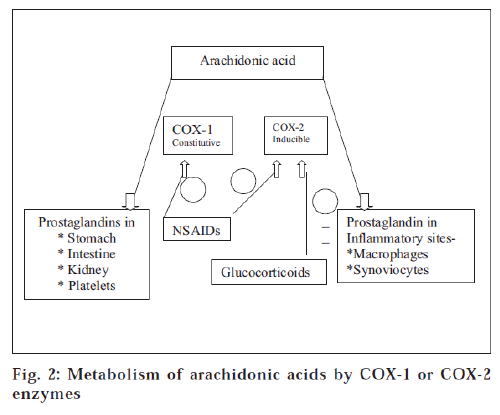
The principal pharmacological effects of NSAIDs are due to their ability to inhibit prostaglandin synthesis by blocking the COX activity of both COX-1 and COX-2. Vane’s hypothesis relates the reduction of inflammation to this inhibition [8]. There are two types of COX enzymes, namely, COX-1 (prostaglandin H1) and COX-2 (prostaglandin H2), which are present in most tissues, including blood platelets and are involved in cell-to-cell signalling and in tissue homeostasis [9].
NSAIDs have been available almost for 100 years since the introduction of aspirin to the market [10]. The earliest NSAID known to modern medicine has been aspirin, produced in 1888, towards the dawn of 20th century by the young research chemist Felix Hoffmann. NSAIDs are the mostly used and abused drugs in the world today (annually about 20,000 tonnes of aspirin is consumed in United States alone). Almost after 117 years of use, the effects of aspirin are well known, but some of the unwanted effects are only now emerging or being defined [11]. For aspirin, these include, in particular, erosions of the upper gastrointestinal tract, ulceration and bleeding, bronchospasm (probably not mediated through prostaglandin) and nasal allergies, liver function abnormalities of obscure reasons, irreversible inhibition of platelet aggregation and enhancement of anticoagulant activity and, perhaps, inhibition of cartilage repair [12].
Acetic acid products include the indoles, which are effective in large-joint arthritis; indomethacin, producing serotonin-like effects in elderly patients. Sulindac is a prodrug and presumably safer for the kidney [14]. Tolmetin sodium is acceptable in children and patients undergoing warfarin anticoagulation [15]. The oxicams are a potent series with long half-lives that hold promise of better efficacy and compliance with risk if given in an appropriate dosage [16]. The mucosal irritation due to acidic nature of most of NSAIDs and inhibition of production of mucosal protective PGE leads to gastric erosion [17].
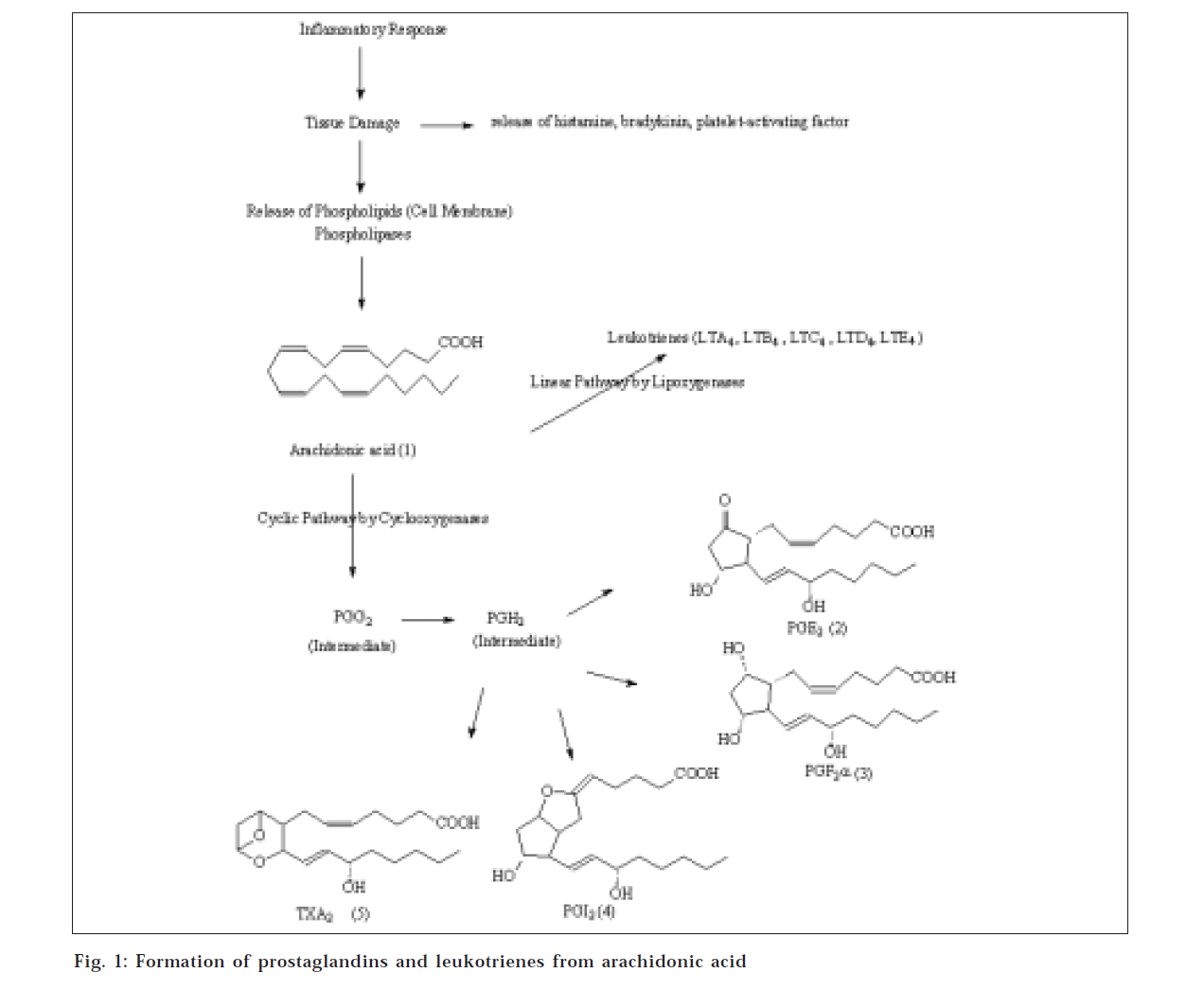
Not all the mechanisms of actions of NSAIDs are completely understood, especially in treatment of inflammatory disorders. The mucosal irritation due to acidic nature of most of NSAIDs and inhibition of production of mucosal protective PGE leads to gastric erosion on long-term treatment. The enzyme COX converts arachidonic acid to endoperoxides (prostaglandins G2 and H2) that are mediators of capillary dilation, which in turn initiates the inflammatory process as shown in fig. 1. The inherent stability of the endoperoxides leads to production of prostaglandins E2 and I2 (prostacyclin), which are prime tissues for the neural transmission of pain. Bradykinin and histamine, which are found in inflammatory sites, serve as initiators of the pain signal. Other end products of prostaglandins from the cyclooxygenase pathway account for the effect of NSAIDs on many of the major features of the complex pathology of arthritis [18]. However, there are other mediator substances that can accomplish the same physiologic effects.
Recently, two isoforms of COX have been discovered, namely, COX-1 and COX-2. COX-1 is responsible for normal physiologic function in platelets, gastrointestinal tract and kidney; whereas COX-2 is induced in inflammatory sites and has limited distribution in brain, kidney and testes. The metabolism of arachidonic acid by constitutive cyclooxygenase (COX-1) or inducible form (COX-2) limited distribution in brain, kidney and testes [19], illustrated in the fig. 2.
Besides prolonging bleeding and causing gastric ulcers, aspirin and other nonsteroidal antiinflammatory drugs can trigger and aggravate an asthmatic attack [20]. In a similar fashion, aspirin can initiate or aggravate urticaria. These effects are most likely not mediated by antibodies but are due to a direct effect of thioether leukotrienes. Many NSAIDs increase the formation of slow-reacting substances after allergen challenge [21]. NSAIDs may not necessarily improve rheumatic disorder. They are often regarded as providing only symptomatic relief. Even, whether these agents cause deterioration of these rheumatic conditions after long-term use is an important question. Certain drugs also increase formation of leukotriene B4 within a close range. The adverse effects of NSAIDs include occult gastrointestinal bleeding with anaemia, gastritis, epigastric pain, dyspepsia, duodenal ulcer with perforation and haemorrhage and ulcerative oesophagitis. NSAIDs may cause water retention in most reported cases has been in terms of cerebral oedema with effect on central nervous system with risk of cardiovascular disorders [22]. Besides the gastrointestinal adverse effects of NSAIDs, the other adverse effects are observed in the renal system [23]. Some of the severe renal toxic effects like renal arteriolar constriction, renal tubular necrosis, congestive cardiac failure, cirrhosis of liver, renovascular disease, renal failure hyperkalaemia, renal papillary necrosis, acute interstitial nephritis and the nephritic syndrome and renal lesions are associated with use of NSAIDs [24].
Ulcer develops in the area of the gastrointestinal tract exposed to acidic gastric juice. Mostly ulcers occur on the lesser curvature of stomach, where they are called gastric ulcers; and if they occur in the pyloric sphincter or first part of duodenum, they are called duodenal ulcers. Rodriguez [25] has discussed the risk of gastrointestinal bleeding and perforation associated with use of NSAIDs. Most peptic ulcers are duodenal. Hirschowitz [26] and Wolfe [27] described the side effects, indications and preventive measures of NSAIDs. It has been reported that lower doses of NSAIDs pose a lower risk of gastrointestinal toxicity. Ulcers can occur not only in the stomach but also in the lower part of the oesophagus and in the duodenum. Indeed, duodenal ulcers are about 10 times more frequent than gastric ulcers [28]. Ulcer formation involves breaking the mucosal barrier and exposing the underlying tissue to the corrosive action of acid and pepsin, which is due to decrease in PEG2release. Many factors may be involved, including genetic susceptibility; drugs, alcohol, bile salts and an excessive secretion of acid and pepsin; these are just some of the contributing factors [29]. According to a study in USA [30] based on NSAID-related gastrointestinal deaths, put into perspective, the rate is higher than that found from cervical cancer, asthma or malignant melanoma. The incidence and prevalence of gastric ulcer are related to many risk factors including Helicobacter pylori infection [31-33] in people taking higher doses of NSAIDs than usual doses of drugs and certain combinations of drugs (e.g., combining of two different NSAIDs) [34,35], smoking, alcohol use, socioeconomic status, loss of sleep, skipping breakfast and stress [36]. Geriatric patients who use NSAIDs face a fivefold increase in the likelihood of serious gastrointestinal events [37]. The average risk of ulcers was found increased when NSAIDs were used for longer time [38] and the risk of developing serious gastrointestinal disorders was higher, as has been reported in a large clinical trial [39]. Age and sex are important determinants of risk when used in a large case-control study. NSAIDs are associated with side effects including gastrointestinal disturbances leading to serious gastrointestinal complications [40]. Further reports indicated that some NSAIDs, especially ketorolac-type, have been considered high-risk antiinflammatory agents [41-43].
All NSAIDs reduce pain and inflammation by inhibiting enzyme COX. Many conventional NSAIDs are available in combination; however, its rationale has not yet been well established in terms of the synergistic effect and it has been pointed out that it may induce synergistic nephrotoxicity [44]. It has been reported that there is no added advantage in the use of paracetamol and ibuprofen (combination) over ibuprofen [45] per se. In 1991, more than 99 million prescription NSAIDs and billions of over-the-counter NSAIDs were sold annually in the US [46]. For majority of individuals, NSAIDs are well tolerated. The Food and Drug Administrations of US reported in 1988 that every year, approximately 200 000 bleeding or perforated NSAID-induced ulcers result in at least 10 000 deaths in United States alone [47]. Deaths due to gastrointestinal causes occur at a frequency that is twice in rheumatoid arthritis patients than in the general population [48]. Tenfold increase in risk was observed in hospitalized patients who were treated with aspirin for myocardial infarction due to gastrointestinal complications [49].
Antiulcer drugs can be broadly divided into three categories: antacids, H2-blockers and proton pump inhibitors and mucosal strengthening agents. Antacids are used to neutralize the intraluminal acid and pepsin; H2-blockers and proton pump inhibitors target acid secretion and strengthen mucosal membrane. None of these drugs alone adequately meet the requirement for successful ulcer therapy [50]. Many steps are taken into consideration to reduce the side effects of NSAIDs [51,52], which are described below.
Use of misoprostol
Replacement of prostaglandin deficiency with misoprostol (at least 200 μg given three times a day) [53] is one such step. Misoprostol, which is a synthetic prostaglandin E1 (PGE1) analogue, acts by replacing mucosal prostaglandin inhibited by NSAIDs therapy. It inhibits gastric acid secretion. Misoprostol does not interfere with antiinflammatory activity of NSAIDs [54,55]. Gastric acid inhibitors are less effective in the treatment of erosions [56]. Misoprostol, among their other gastroprotective properties, reportedly improve the gastric microcirculation [57,58]. Unwanted effects like diarrhoea and abdominal cramps, uterine contractions can also occur.
Use of antacids
Antacids act by neutralizing gastric acid and thus raising the gastric pH. Antacids are proven to heal duodenal ulcers; their use in the treatment of gastric ulcers is not well documented. Antacids may reduce absorption of many concomitant medications, including NSAIDs and resulting drug interactions [59].
Use of proton pump inhibitors
The main agent is a substituted benzimidazole, omeprazole, which is a weak base with value of pKa 3.97. It acts by blocking irreversibly the H+/K+-ATPase (the proton pump), the terminal step in the acid secretory pathway. It markedly inhibits both basal and stimulated gastric acid secretion, but it has some unwanted effects including headache, diarrhoea, rashes, dizziness, mental confusion, impotence, pain in muscles and joints - that limit its usage.
Use of H2-antagonist
The introduction of the H2-receptor antagonists in the mid-1970s by Sir James Black and his colleagues constituted a major breakthrough in drug treatment of peptic ulcer. H2-receptor antagonists competitively inhibit histamine actions at all H2-receptors, but their main clinical use is as inhibitors of gastric acid secretion. The drugs used are cimetidine and ranitidine. Newer H2-receptor antagonists, such as nizatidine and famotidine, are also available. Unwanted effects, including diarrhoea, dizziness, muscle pains, rashes and hypergastrianaemia, have been reported9. Famotidine can effectively prevent aspirin-induced gastric ulcers [62,63]. The recommended uses of some NSAIDs are given in Table 2.
| Indication | Drug |
|---|---|
| Fever and/or pain Inflammation and/or pain and/or fever | paracetamol, mefenamic acid Any NSAIDs; start with one, try for at least a week; if not better, change to another |
| Severe non-inflammatory pain | paracetamol + codeine or opioids alone |
| Dysmenorrhoea | mefenamic acid, diclofenac, ibuprofen |
| Colic, visceral pain Post operative /post partum |
opioids + antispasmodics opioid analgesics |
Table 2: The Recommended Uses Of Some Nsaids
Conclusion
NSAIDs have become a very important weapon in the control of inflammation and pain in joint disease and in other chronic, painful conditions. Their use has been limited by their propensity to cause gut symptoms or actually damage the gut. These drugs exert their antiinflammatory, anticlotting and gut damaging effects through inhibition of COX and decreased prostaglandin production. Anticlotting and untoward effects on the gut are due to the COX-1 form of cyclooxygenase. Employing a few precautions (especially in older females requiring multiple drugs for long periods) can minimize adverse effects. Those COX-2 drugs that remain available should be used only when you and your doctor agree that an NSAID is the best drug for your painful condition. Research supports the use of interventions to reduce and/or avoid NSAID-associated complications, but these strategies are not always applied effectively. This reinforces the need for continued education to improve outcomes of care.
References
- Tortora, J.G., and Grabowski, R.S., Eds., In; Principles of Anatomy and Physiology, 7th Edn., HarperCollins College Publishers, New York, 1993, 695.
- Guyton, C.A. and Hall, E.J., Eds., In; Textbook of Medical Physiology,8thEdn., Prism Books (Pvt) Ltd., Bangalore, 1991, 520.
- Brogden, N.R., Drugs, 1986, 32 (Suppl. 4), 27, 45.
- Paul, B.J., Calicut Med. J., 2004, 2, e8
- Vane, J.R., Amer. J. Med., 1998, 104, 2S.
- Lane, N.E., J. Rheumatol., 1997, 24, 20
- Brooks, P., Amer. J. Med., 1998, 104, 9S
- Koch, M., Arch. Int. Med., 1996, 156, 2321.
- Rang, H.P., Dale, M.M. and Ritter, J.M., Eds., In; Pharmacology, 3rdEdn., International Student Edition, Churchill Livingstone, 1995, 246,390.
- Wallace, J., Gastroenterol, 1997, 112, 1000.
- Ehrlich, G.E. and Machetey, Eds., In; Progress in ClinicalRheumatology, 1st Edn., John Wright PSG, Boston, 1982, 85.
- Buchanan, W.W. and Rooney, P.J., Clin. Rheum. Dis., 1979,499, 539.
- Shen, T.Y., Sem. Arthritis Rheum.,1982, 12, 89.
- Rymer, A.R., Clin. Rheum. Dis., 1979, 5, 533.
- Ehrlich, G.E., Clin. Rheum. Dis., 1979, 5, 481.
- Downie, W.W., Sem. Arthritis Rheum., 1982, 12, 170.
- Foster, R.W., Eds., In; Basic Pharmacology, 4th Edn., Butter worth-Heinemann, Reed Educational and Professional Publishing Limited,1996, 213.
- Simon, L.S., Arthritis Rheum.,1998, 41, 1591.
- Frolich, J.C., Ann. Rheum. Dis., 1995, 54, 942.
- Blower, A.L., Brooks, A. and Fenn, CG.,Aliment Pharmacol.Ther., 1997 11, 283.
- Hawkey, C.J., Cullen, D.J. and Greenwood, D.C., AlimentPharmacol. Ther.,1997, 11, 293.
- MacDonald, T.M., Morant, S.V. and Robinson, G.C., Brit. Med. J.,1997 315, 1333.
- Kalant, H., Walter, H.E. and Roschlan; Eds., In; Principles of MedicalPharmacology, 6th Edn., Oxford University Press, NY, 1998, 420.
- Murray, M.D. and Brater, C.B., Annu. Rev. Pharmacol.Toxicol., 1993, 32, 435, 465.
- Unsworth, J., Sturman, S., Lunec, J. and Blake, D.R., Ann. Rheum.Dis., 1987, 46, 233.
- Rodriguez, L.A.G. and Jick, H., Lancet, 1994, 343, 769.
- Hirschowitz, B.I., Southern Med. J., 1996, 89, 259.
- Wolfe, M.M., Hospital Practice, 1996, 31, 37
- Johnson, D.A., Consultant, 1997, 37, 1329.
- Singh, G., Amer. J. Med., 1998, 105 (1B), 31s.
- Hawkey, C.J., Gut, 2000, 46, 310.
- Cutler, A.F., Int. Med., 1998, 19, 10.
- Rogers, A.I. and Hoel, D., Postgrad. Med., 1997, 102, 158.
- Faigel, D.O., Melnyk, C Brandt, L., Eds., In; Clin. Practice ofGastroenterology, Vol. I, Philadelphia, PA, 1999, 264.
- Wood, D., Digestive Health and Nutrition, 2000, 26, 29.
- Gore, M.J., Digestive Health and Nutrition, 1999, 10.
- Corporate Author, Consultant, 1999, 39, 756, 762.
- Koch, M., Dezi, A., Ferrario, F. and Capurso, L., Arch. Int. Med.,1996, 156, 2321.
- Silverstein, F.E., Graham, D.Y. and Senior, J. R., Ann. Int. Med.,1995, 123, 241.
- Griffin, M., Amer. J. Med., 1998, 104, 23 s.
- Henry, D., Lim, L., Garcia, L. and Rodriguez, Brit. Med. J., 1996,312, 1563.
- Garcia, L.A. and Rodriguez, Arch. Int. Med., 1998, 158, 33.
- MacDonald, T.M., Morant, S.V. and Robinson, G.C., Brit. Med. J.,1997, 315, 1333.
- Howell, D.S., Sapolsky, A.I. and Pita, J.C., Sem. Arthritis Rhem.,1976, 5, 365.
- Derle, D.V. and Gujar, K.N., Indian Drugs, 2001, 38, 371.
- Kendall, B. and Peura, D., Pract. Gastroenterol.,1993, 17,13.
- Smalley, W.E. and Griffin, M.R., Gastroenterology Clinics ofNorth Amer., 1996, 25, 373.
- Fries, J., Millers, Spitz, P., Gastroenterol.,1989, 96, 647.
- Kurata, J. and Abbey, D., J. Clin. Gastroenterol.,1990, 12, 260.
- Gabryelewicz, A., J. Physiol. Pharmacol., 1996, 47, 51.
- Koch, M., Arch. Int. Med., 1996, 156, 2321
- Hawkey, C.J., Karrasch, J.A. and Szczepanki, L., N. Engl. J.Med., 1998, 338, 727.
- Wolfe, M. M., Lichtenstein, D. R. and Singh, G., N. Engl. J. Med.,1999, 340, 1888
- Silverstein, F., Graham, D. and Senior, J., Ann. Intern. Med.,1995, 123, 241.
- Silverstein, E.F., Graham, D.Y. and Senior, J.R., Ann. Intern.Med., 1995, 123, 241.
- Guslandi, M., Sorghi, M., Foppa, A. and Tittobello, A., J. Clin.Gastroenterol., 1993, 17, 201.
- Hai, W.M., Chen, B.W. and Cho, CH., J. GastroenterolHepatol, 1990, 5, 653.
- Maiden, N. and Madhok, R., Brit. Med. J., 1995, 311, 1518.
- Ching, C.K. and Lam, S.K., Drugs., 1994, 47, 305.
- Corporate author, J. Critical Illness, 1999, 14, 73, 77.
- Lanza, F., Internal Medicine, 1999, 20, 45.
- Ekstrom, P., Carling, C. and Watterhans, S., Scand. J.Gastroenterol., 1996, 37, 753.
- Taha, A.S., Hudson, N. and Hawkey, C.J., N. Engl. J. Med., 1996,334, 1435.