- *Corresponding Author:
- A. Kuvalekar
Interactive Research School for Health Affairs, Bharati Vidyapeeth Deemed University, Pune-411 043, India
E-mail: kuaniket@gmail.com
| Date of Submission | 26 September 2015 |
| Date of Revision | 02 February 2015 |
| Date of Acceptance | 20 June 2014 |
| Indian J Pharm Sci 2015;77(5):630-634 |
This is an open access article distributed under the terms of the Creative Commons Attribution‑NonCommercial‑ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non‑commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Dyslipidemia is a significant morbidity associated with diabetes and cardiovascular disorders. The present study was undertaken to assess the lipid profile of type 2 diabetic and age-gender matched healthy subjects and its association, if any, with fasting plasma glucose. Clinically diagnosed diabetic subjects were recruited for the study. The fasting plasma glucose and lipid profiles were analyzed for 99 diabetic and 101 healthy volunteers. The blood samples were analyzed for fasting plasma glucose, total cholesterol, triglycerides, high density lipoprotein-cholesterol, low density lipoprotein-cholesterol and very low density lipoprotein-cholesterol. Correlation analysis of lipid profile with fasting plasma glucose and calculation of risk ratio was done. The levels of high density lipoprotein-cholesterol and low density lipoprotein-cholesterol were found to be significantly low in diabetics and subjects with lower low density lipoprotein-cholesterol were on statins. Inspite of lower lipid values, the risk ratio for diabetics was significantly higher. The correlation analysis indicated significant difference in relationship between fasting plasma glucose, lipid parameters and risk ratios in the two groups. Diabetics with lower high density lipoprotein-cholesterol and higher total cholesterol present with a higher risk ratio pointing to need of non-statin high density lipoprotein-raising medications decreasing their predisposition to cardiovascular disorders. The study highlights the altered pattern of correlation of lipid profile with fasting plasma glucose in diabetics and their increased risk of cardiovascular disorders. The dyslipidemia in the form of triglyceridemia and significantly low high density lipoprotein-cholesterol in diabetics point towards the need of non-statin high density lipoprotein-raising medications.
Keywords
Cardiovascular disorders, diabetes, dyslipidemia, hypercholesterolemia, risk ratio, serum lipids
Type 2 diabetes (T2D) is estimated to affect approximately 439 million individuals by year 2030 worldwide [1]. It is associated with significant morbidity and mortality due to cardiovascular complications [2]. South East Asian countries account highest burden of diabetes, including India which may have up to 33 million cases [3]. Cardiovascular disease (CVD) is more prevalennt in patient with type 2 diabetes than general population [4]. Dyslipidemia is a well known risk factor for CVD, with respect to type 2 diabetes and it affects almost 50% of population [5]. The characteristic features of dyslipidemia are high plasma triglyceride concentration, low high-density lipoprotein (HDL) cholesterol concentration and increased concentration of small dense low-density lipoprotein (LDL) cholesterol particle [6]. The elevated level of LDL is the characteristic marker for CVD [7]. Although there is considerable evidence that abnormalities in serum lipids and lipid metabolism are major risk factors for increased incidence of CVD in type 2 diabetes, the relative role of various lipoprotein abnormalities in determining the risk in diabetic individuals needs to be addressed [8].
In view of the predisposition for the development of atherosclerotic vascular disease in diabetics, attention has been focused on abnormalities of lipid and lipoprotein metabolism in diabetes. The aim of the present work was to study pattern, and severity of lipid disorders among type 2 diabetic patients especially in urban rural region of Pune, Maharashtra, India.
Total of 99 (45 males and 54 females) type 2 diabetic subjects attending the OPD of Bharati Medical Hospital and 101 (43 males and 58 females) controls were included in the study. Subjects with HIV/ HBsAg, bodily injuries, surgical procedures in recent past, underweight (BMI≤18.5) and alcoholics were excluded. The purpose of the study was explained to all potential subjects and only those who gave informed written consent were included in the study. The anthropometric measurements like height, weight, BMI, waist circumference, hip circumference were recorded for all the subjects. Blood pressure was measured using standard mercury sphygmomanometer after patient had rested for at least 10 min. About 8 ml venous blood samples, after at least 8 h fasting, were collected from all subjects by vain puncture, in plain and EDTA vacutainers.
A standard dietary and physical activity questionnaire was delivered to all the subjects. The ongoing prescribed drugs, their dosages and other co-morbidities, if any were recorded for all diabetic subjects. The present study was undertaken after ethical approval from the Institutional Human Ethical Committee (BVDU/MC/2 dated 27th February 2012).
Glucose, total cholesterol (TC), triglycerides (TG), high density lipoprotein cholesterol (HDL-C), low density lipoprotein cholesterol (LDL-C) were estimated using commercial kits (Coral clinical system, Goa, India). Very low density lipoprotein cholesterol (VLDL-C) was estimated by using the formula: triglycerides/5. Risk ratios for all the samples were calculated by dividing TC by HDL-C.
The lipid profiles from the subjects were classified as per the guidelines of National Cholesterol Education Programme (NCEP) Adult Treatment Panel III (ATP III). The NCEP-ATPIII guidelines classify hypercholesterolemia when TC>200 mg/dl, high LDL-C if LDL-C>100 mg/dl, hypertriglyceridemia if TG>150 mg/dl and low HDL-C if the value is <40 mg/dl. The subjects with one or more abnormal lipid concentrations were considered dyslipidemic. Type 2 diabetes mellitus was defined as per the American Diabetes Association (ADA) criteria. The data obtained from the study were analyzed by GraphPad 13.0 (Trial Version). Pearson’s correlation test was performed to examine various correlations. Two tailed unpaired t-test was used to compare means of different parameters. The differences among the means were considered significant if P≤0.05. All the values were represented as mg/dl unless otherwise specified.
The present study included 99 (45 males and 54 females) type 2 diabetic subjects and 101 (43 males and 58 females) healthy controls. The mean age of diabetic and control subjects was 51.82±0.63 and 50.50±0.61 years, respectively.
Table 1 shows lipid profiles of subjects and its classification based on ATPIII for total cholesterol, triacylglycerols, LDL-C and HDL-C levels. The lower HDL-C (97%) and higher TC (15%) was observed in diabetic groups as compared to healthy controls. Table 2 summarizes the FPG, lipid parameters, and risk ratio for the study population.
| Parameters | Healthy (%) | Diabetics (%) |
|---|---|---|
| Total cholesterol (mg/dl) | ||
| <200 | 101 (100) | 84 (84.85) |
| >200 | ‑ | 15 (15.15) |
| Triglycerides (mg/dl) | ||
| <150 | 61 (60.40) | 64 (64.65) |
| >150 | 40 (39.60) | 35 (35.35) |
| HDL‑C (mg/dl) | ||
| <40 | 78 (77.23) | 97 (97.98) |
| >40 | 23 (22.77) | 2 (2.02) |
| LDL‑C (mg/dl) | ||
| <100 | 99 (98.02) | 99 (100) |
| >100 | 2 (1.98) | ‑ |
ATP III: adult Treatment Panel III, HDL‑C: high density lipoprotein cholesterol, LDL‑C: low density lipoprotein cholesterol
Table 1: Frequency Of The Lipid Parameters In Healthy And Diabetic Groups In The Study Population Based On Atp III Guidelines
| Parameters | Mean ± SE | P | |
|---|---|---|---|
| Healthy | Diabetic | ||
| ( n =101) | ( n =99) | ||
| FPG (mg/dl) | 66.16 ± 2.2 | 131.26 ± 6.2 | <0.05 |
| TC | 148.77 ± 2.7 | 162.92 ± 4.8 | ≤0.05 |
| TG | 141.87 ± 6.6 | 137.04 ± 6.2ns | 0.5985 |
| HDL‑C | 31.03 ± 1.1 | 25.38 ± 0.9 | <0.05 |
| LDL‑C | 53.65 ± 1.9 | 43.79 ± 1.5 | <0.05 |
| Risk ratio | 5.39 ± 0.2 | 7.50 ± 0.4 | <0.05 |
nsNot significant. FPG: fasting plasma glucose, SE: standard error, HDL-C: high density lipoprotein cholesterol, LDL-C: low density lipoprotein cholesterol, TC: total cholesterol, TG: triglycerides
Table 2: Fpg, Lipid Parameters And Risk Ratios For Healthy And Diabetic Population In The Present Study
Highly significant differences were observed in the FPG, TC, HDL-C, LDL-C and risk ratios in diabetics as compared to control. The values reported in the present study are contradictory with the earlier reports indicating higher levels of LDL-C in the diabetic population [9]. In the present study, the LDL-C values were significantly lower in the diabetic group owing to the statin treatments. The imbalance in the lipid profiles in the diabetic subjects is shown to be highly dependent upon medicines and glycemic control [10-12]. The lower HDL-C among diabetic people attending primary care is now well-recognized [13]. In the present study, out of the diabetic people with lower than recommended HDL-C levels, about 45.36% had either hypertension, ischemic heart disease or other forms of cardiovascular disorders. The lower than normal HDL-C is reported to be a highly prevalent and potentially modifiable risk factor for CVD prevention in type 2 diabetes [13]. The current guidelines suggest aggressive treatment modalities to reduce LDL cholesterol, blood pressure and glucose levels in diabetic patients, but data concerning the management of low HDL cholesterol levels is still inconclusive [14]. Hypercholesterolemia and low HDL levels observed in the present study in diabetic population are well known risk factors for cardiovascular diseases. It has been reported that normalizing low HDL-C in primary care diabetic patients would decrease the estimated CVD mortality by 42% in women and 23% in men [13].
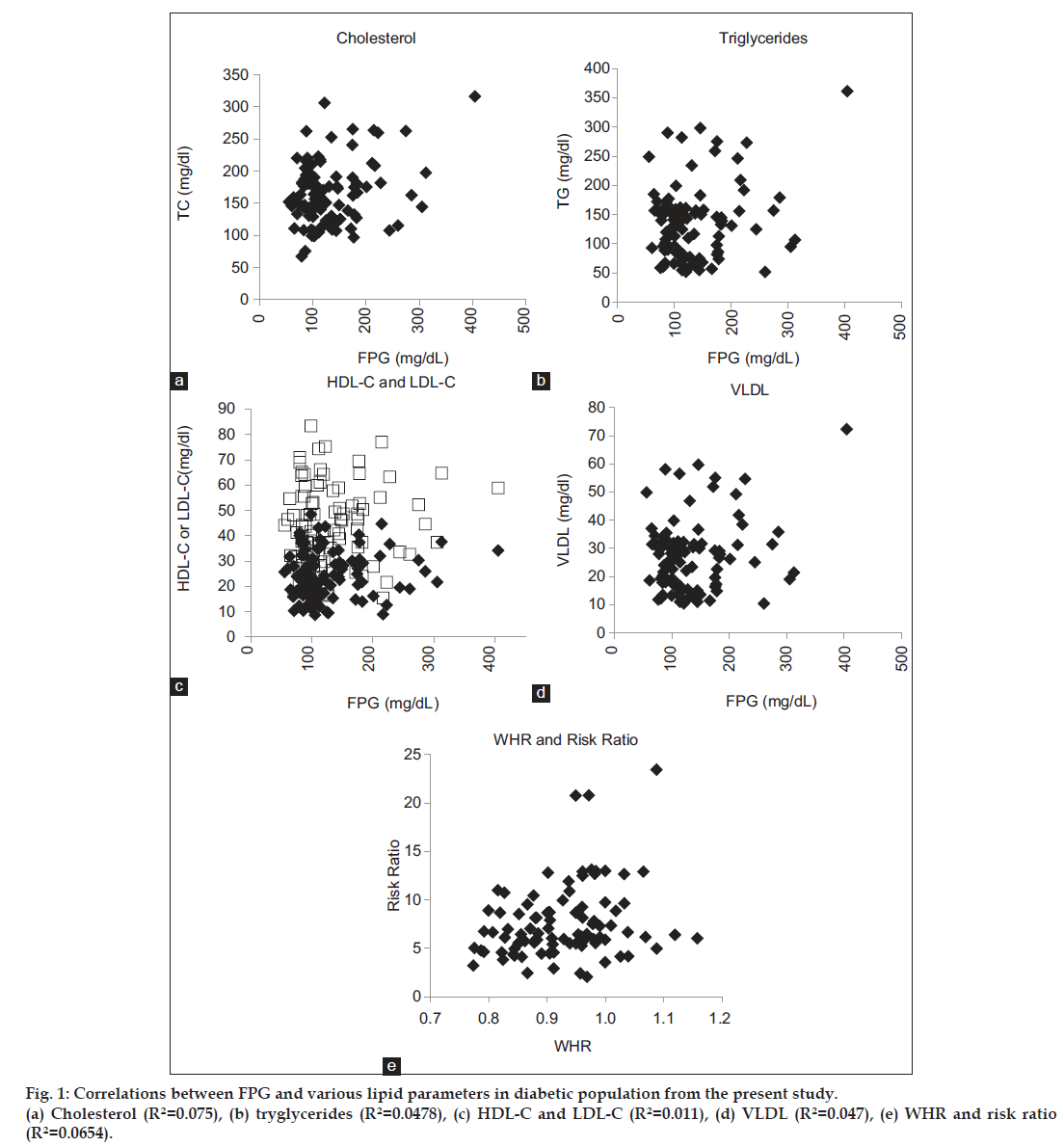
The present study also reported significantly different correlation of FPG with lipid parameters in diabetic subjects as compared to healthy volunteers (Table 3, fig. 1). The relationship among FPG and lipid variables was observed to be different in healthy and diabetic population. The FPG and TG were found to be significantly correlated in diabetic population (P=0.0236). The negatively correlated HDL-C and LDL-C showed a positive and significant correlation with FPG in diabetic subjects (P=0.0443 and P=0.0405, respectively). The positive correlations of FPG with VLDL-C and TC were enhanced in diabetic population with higher probability of FPG modifying the VLDL and TC contents. Also, FPG was found to be the predictor for hypercholesterolemia (R2=0.075), HDL-C and LDL-C contents (R2=0.011) and TG and VLDL (R2=0.047) (P≤0.05 for all regression analyses).
| Correlation between | Healthy | Diabetic | ||
|---|---|---|---|---|
| Correlation coefficient (r) | P | Correlation coefficient (r) | P | |
| FPG and TG | 0.08762ns | 0.3836 | 0.2275 | 0.0236 |
| FPG and HDL‑C | −0.4026 | <0.05 | 0.07825 | 0.0443 |
| FPG and LDL‑C | −0.4001 | <0.05 | 0.08456 | 0.0405 |
| FPG and VLDL‑C | 0.1998 | 0.0452 | 0.2264 | 0.0242 |
| FPG and TC | 0.2428 | 0.0144 | 0.2942 | 0.0031 |
nsNot significant. FPG: fasting plasma glucose, HDL‑C: high density lipoprotein cholesterol, LDL‑C: low density lipoprotein cholesterol, TC: total cholesterol, TG: triglycerides, VLDL‑C: very high density lipoprotein cholesterol
Table 3: Correlation Between Fpg And Various Lipid Parameters In Healthy And Diabetic Individuals
The present study indicates the need for prescribing a non-statin HDL cholesterol–raising medication to diabetic people to decrease their predisposition to CVD. In addition, the altered pattern of correlation of various lipid parameters with FPG and its potential as a predictor of dyslipidemia in diabetics, points to the much stressed necessity of good glycemic control.
Acknowledgements
Authors gratefully acknowledge the financial support from Bharati Vidyapeeth Deemed University.
Financial support and sponsorship
The financial support from Bharati Vidyapeeth Deemed University.
Conflicts of interest
There are no conflicts of interest.
References
- Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res ClinPract 2010;87:4-14.
- U.K. Prospective Diabetes Study 27. Plasma lipids and lipoproteins at diagnosis of NIDDM by age and sex. Diabetes Care 1997;20:1683-7.
- Health Situation in the South East Asia Region 1998-2000. New Delhi: WHO Regional Office for South East Asia; 2002. Available from: http://www.searo.who.int/entity/health_situation_trends/ documents/health_situation_sear_1998-2000.pdf. [Last accessed on 2015 Feb 02].
- Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA 1979;241:2035-8.
- Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA 2004;291:335-42.
- Mooradian AD. Dyslipidemia in type 2 diabetes mellitus. Nat ClinPractEndocrinolMetab 2009;5:150-9.
- Turner RC, Millns H, Neil HA, Stratton IM, Manley SE, Matthews DR, et al.Risk factors for coronary artery disease innon-insulin dependent diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS: 23). BMJ 1998;316:823-8
- Hetal P, Lakhani JD, Dadhania JD, Trivedi JD. The prevalence and pattern of dyslipidemia among type 2 diabetic patients at rural based hospital in Gujarat, India. Indian J ClinPract 2012;22:36-44.
- Samatha P, Venkateswarlu M, Sivaprabodh V. Lipid Profile Levels in Type 2 Diabetes Mellitus from the Tribal Population of Adilabad in Andhra Pradesh, India. J ClinDiagn Res 2012;6:590-2.
- Elam MB, Hunninghake DB, Davis KB, Garg R, Johnson C, Egan D, et al. Effect of niacin on lipid and lipoprotein levels and glycemic control in patients with diabetes and peripheral arterial disease: The ADMIT study: A randomized trial. Arterial Disease Multiple Intervention Trial. JAMA 2000;284:1263-70.
- Mughal MA, Memon MY, Zardari MK, Tanwani RK, Ali M. Effect of acarbose on glycemic control, serum lipids and lipoproteins in type 2 diabetes. J Pak Med Assoc 2000;50:152-6.
- Khan A, Safdar M, Ali Khan MM, Khattak KN, Anderson RA. Cinnamon improves glucose and lipids of people with type 2 diabetes. Diabetes Care 2003;26:3215-8.
- Grant RW, Meigs JB. Prevalence and treatment of low HDL cholesterol among primary care patients with type 2 diabetes: An unmet challenge for cardiovascular risk reduction. Diabetes Care 2007;30:479-84.
- Bitzur R, Cohen H, Kamari Y, Shaish A, Harats D. Triglycerides and HDL cholesterol: Stars or second leads in diabetes? Diabetes Care 2009;32Suppl 2:S373-7.