- *Corresponding Author:
- Fuqiang Tan
Second Department of Orthopedics, Zhongxian People’s Hospital, Chongqing 404300, China
E-mail: fuqiangtan2023@163.com
| Date of Received | 01 July 2022 |
| Date of Revision | 17 May 2023 |
| Date of Acceptance | 04 November 2023 |
| Indian J Pharm Sci 2023;85(6):1738-1745 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Traumatic arthritis is a common joint disease. Salvia miltiorrhiza is a traditional Chinese medicine that has been used for the treatment of cardiovascular diseases and inflammation-related diseases. However, the efficacy and mechanism of Salvia miltiorrhiza extract on traumatic arthritis are still unclear. 60 rats were randomly divided into controls, traumatic arthritis group, and of Salvia miltiorrhiza extract treatment group. Traumatic arthritis model was established in groups B and C, and of Salvia miltiorrhiza extract was administered in group C. The expression levels of arthritis markers and inflammation-related factors were detected. Relative to group B, the relative expression level of serum malondialdehyde in group C was apparently decreased, and that of serum superoxide dismutase was apparently raised. The serum levels of tumor necrosis factor-alpha and nitric oxide in group C were apparently lower as against group B (p<0.05). In addition, the level of serum nuclear factor-kappa B protein in group C was apparently decreased, and the level of inhibitor of nuclear factor-kappa B was apparently raised (p<0.05). Salvia miltiorrhiza extract has a protective outcome on traumatic arthritis and can reduce the inflammatory response. Salvia miltiorrhiza extract can regulate inflammatory signaling pathways, and especially inhibit the expression of tumor necrosis factor-alpha.
Keywords
Salvia miltiorrhiza extract, traumatic arthritis, tumor necrosis factor-alpha, molecular mechanism, malondialdehyde
Traumatic Arthritis (TA) is a common joint disease, and its incidence is increasing year by year, which has brought serious impact on the quality of life and economic burden of patients[1]. Although there are some treatment options available at present, there is still a lack of effective treatment to prevent or reverse the progression of joint destruction. Therefore, the search for new therapeutic strategies and drugs has become a hot topic in the field of arthritis research.
Salvia miltiorrhiza (S. miltiorrhiza) is a Traditional Chinese Medicine (TCM) that has been widely used in cardiovascular diseases and inflammation-related diseases[2]. S. miltiorrhiza and its extracts have a variety of pharmacological activities, such as anti-oxidation, anti-inflammation, anti-fibrinolysis and anti-platelet aggregation[3]. The active ingredients in S. miltiorrhiza Extract (SME) include S. miltiorrhiza ketone, salvianolic acid B, S. miltiorrhiza acid, etc.,[4]. These components have been shown to have biological activities such as anti-inflammatory, anti-oxidation and inhibition of apoptosis[5].
In recent years, more and more studies have been conducted on the role of SME in arthritis. Some experimental studies have shown the protective outcome of SME on TA[6]. SME acts by reducing the inflammatory response, inhibiting the activity of key signaling pathways, and modulating the expression of arthritis markers[7]. In addition, SME are able to reduce joint pathological damage, promote joint repair, and improve joint function[8,9]. These findings suggest a potential clinical application of SME in TA.
In the study of the protective outcome of SME on TA, the exploration of molecular mechanisms is an important direction. Several studies have shown that SME exert their protective outcomes by regulating multiple signaling pathways. Among them, the Nuclear Factor-Kappa B (NF-κB) and Mitochondria-Associated Protein Kinase (MAPK) signaling pathways have been widely studied and considered to be the targets of SME[10,11]. NF-κB and MAPK signaling pathways play a major role in inflammatory response and joint pathological injury, regulating the expression of a variety of inflammatory factors and apoptosis-related factors[12]. By inhibiting the activation of these signaling pathways, SME mitigates the inflammatory response and cellular damage, thereby protecting the joint from further damage[13].
In addition, the inflammatory factor Tumor Necrosis Factor-Alpha (TNF-α) plays an important regulatory role in TA. TNF-α is an early inflammatory factor, and its overexpression is closely related to the occurrence and development of arthritis[14]. Studies have found that SME has a regulatory outcome on TNF-α and can suppress its induced inflammatory response and apoptosis[15]. This finding provides new insights into the mechanism of SME in TA treatment.
Although some progress has been made in terms of the protective outcome of SME on TA and its molecular mechanism, there are still some problems that need to be further solved. First, the active components in SME and their optimal dosage and route of administration in treatment still need to be further studied. In addition, more clinical studies are needed to verify the therapeutic efficacy and safety of SME in different disease stages.
Although there are still some challenges to overcome, the potential of SME as a natural medicine in TA treatment can’t be ignored. It has a variety of pharmacological activities, including anti-inflammatory, anti-oxidation, inhibition of apoptosis, etc., and is able to exert its effects through multiple signaling pathways. In addition, the regulatory effect of SME on TNF-α has also shown its importance in TA. Therefore, further studies on the molecular mechanism and clinical application prospects of SME will provide an important theoretical basis for the treatment of TA and provide new ideas for the development of new therapeutic strategies and drugs.
Materials and Methods
Research materials:
Male Sprague-Dawley (SD) rats weighing (200-250) g, (n=60) were used as subjects, obtained from the Laboratory Animal Center. All animals were adaptively housed for 1 w prior to the experiment to ensure their health status and relatively consistent baseline data. An inclusion criterion includes healthy rats, aged between (8-10) w, with no history of arthritis. Rats with other joint diseases, infections, or immune system abnormalities were excluded.
Reagents:
The main active ingredient of the tanshinone extract used was tanshinone, which was purchased from Xi’an Jinheng Chemical Co., Ltd. Rabbit anti-rat Malondialdehyde (MDA)) antibody and rabbit anti-rat Superoxide Dismutase (SOD) antibody and rabbit anti-rat TNF-α antibody were purchased from Thermo Fisher Scientific (China) Co., Ltd.
Experimental grouping:
60 rats were randomly divided into the following three groups (n=20 each); Controls (A) received normal diet and water. TA group (B): The TA model was established. SME treatment group (C): Based on the establishment of TA model, SME was given by oral gavage, once a day, at a dose of 6 mg/kg. Rats in controls and group B were given the same amount of normal saline by gavage.
Establishment of TA rat model:
Before surgery, the rats were fasted for 12 h but had access to water. The rats were made unconscious using an appropriate dose of an anesthetic, such as isoflurane, and the skin was disinfected adopting a sterile technique. A small incision was made in the right knee joint region of the rat, and then the TA model was established by cutting the joint capsule and stripping the synovium. It was to make sure to avoid rupture of the joint capsule during the procedure. After the TA model was established, the controls received the same surgical procedure without TA induction.
Specimen collection and detection:
7 d later, the rats were sacrificed, and the knee joints were fixed, decalcified, dehydrated, embedded, sectioned, and stained with Hematoxylin and Eosin (HE). The specimens were made into knee joint tissue samples, and the pathological changes of knee joints were observed. Knee tissue samples were adopted separately for the following tests.
Osteoarthritis tissue was scored by Mankin method. Western blot analysis was adopted to detect the protein expression levels of arthritis markers and inflammation-related factors: The protein levels of inhibitor of NF-κB protein (I-κB) and NF-κB in cartilage tissue samples were detected. Knee joint tissue samples were uniformly dissected and Radioimmunoprecipitation Assay (RIPA) lysate was adopted to extract total protein. The proteins were separated and transferred to polyacrylamide gels by Sodium Dodecyl-Sulfate Polyacrylamide Gel Electrophoresis (SDS-PAGE) and protein transfer, followed by immunodetection with specific antibodies, and the gray values of the immunoblot bands were analyzed with a gel imager. The experimental procedures were as follows; first, an appropriate amount of cartilage tissue was taken out, and the corresponding amount of cellular protein was added to extract the test solution, then the cartilage tissue was subjected to an ice bath for 2 h. Then, centrifugation was performed at 4° for 15 min. Then, the supernatant was taken for protein quantification. Then, 1/5th volume of 5× buffer was put under the same protein concentration. It was subjected to denaturation under boiling water, followed by electrophoresis, gel cutting, primary antibody incubation at 4° overnight, image collection and analysis.
Enzyme Linked Immunosorbent Assay (ELISA): The levels of SOD, MDA, Nitric Oxide (NO), and TNF-α in rat cartilage tissue were detected by ELISA kit purchased from Shanghai Jingkang Biological Engineering Co., Ltd. The operation method was strictly carried out according to the instructions.
Statistical methods:
Statistical Package for the Social Science (SPSS) 19.0 statistical software was adopted for data processing, and the mean level of measurement data was expressed as mean±standard deviation (x̄±s). For the comparison of multiple groups of independent measurement data with equal variance in accordance with normal distribution, multivariate analysis of variance was adopted, and t-test was adopted for the comparison of means between groups. The count data were expressed as percentage (%). One-way analysis of variance and Chi-square (χ2) test were adopted, and p<0.05 was considered statistically significant.
Results and Discussion
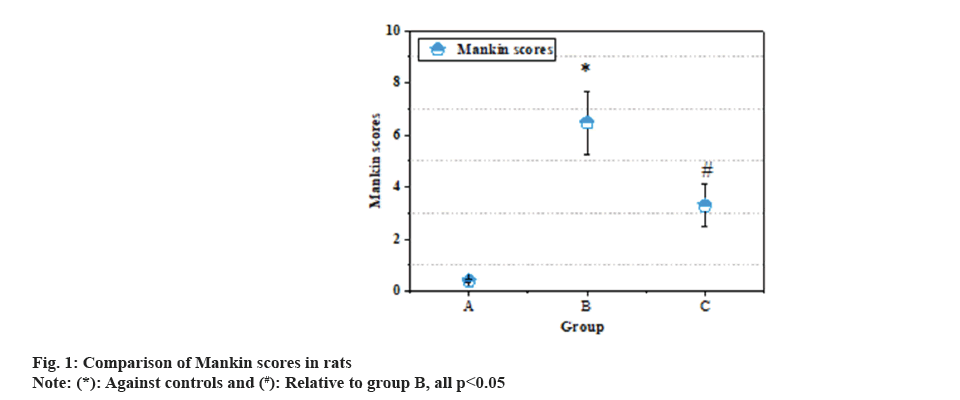
Fig. 1 illustrates the comparison of Mankin scores in rats. The Mankin scores of rats in controls, groups B and C were 0.40±0.05, 6.47±1.21 and 3.29±0.83, respectively. Relative to the rats in controls, the rats in group B had an apparently superior Mankin score of the knee joint, and relative to the group B, the subjects with SME intervention had an apparently inferior Mankin score (p<0.05).
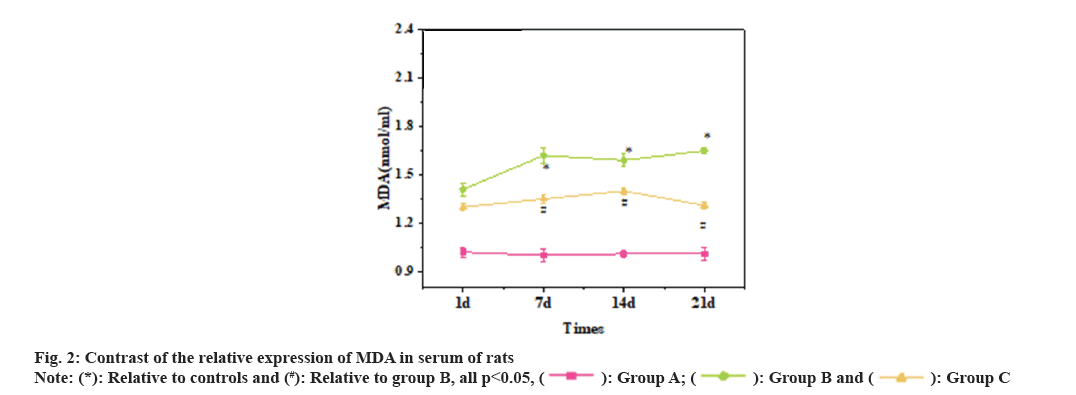
Fig. 2 illustrates the relative expression of MDA in the serum of rats. Relative to the rats in the controls, the relative expression of serum MDA in the groups B and C was apparently raised (p<0.05). Relative to group B, the relative expression of serum MDA in subjects with SME intervention was apparently decreased (p<0.05).
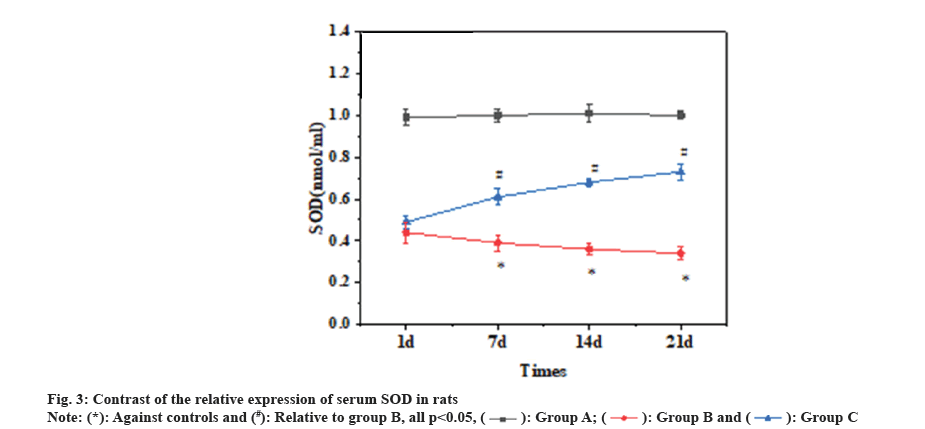
Fig. 3 illustrates the relative expression of serum SOD in rats. Relative to controls, the relative expression of serum SOD in groups B and C was apparently decreased, and as against group B, that was clearly raised in subjects with SME intervention (p<0.05).
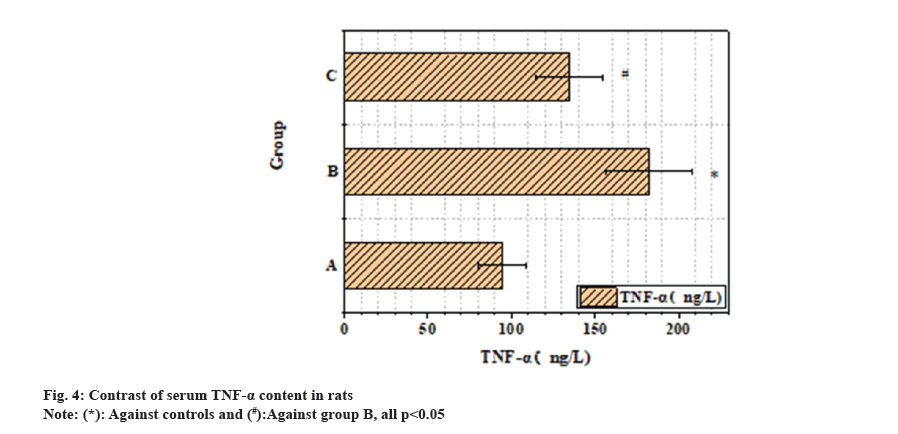
Fig. 4 illustrates the contrast of serum TNF-α content in rats. The serum TNF-α levels of controls, groups B and C were (94.28±14.03) ng/l, (182.39±26.02) ng/l and (134.52±19.89) ng/l, respectively. As against controls, the serum level of TNF-α in groups B and C was clearly raised, and as against group B, that had a clear decrease in subjects with SME intervention (p<0.05).
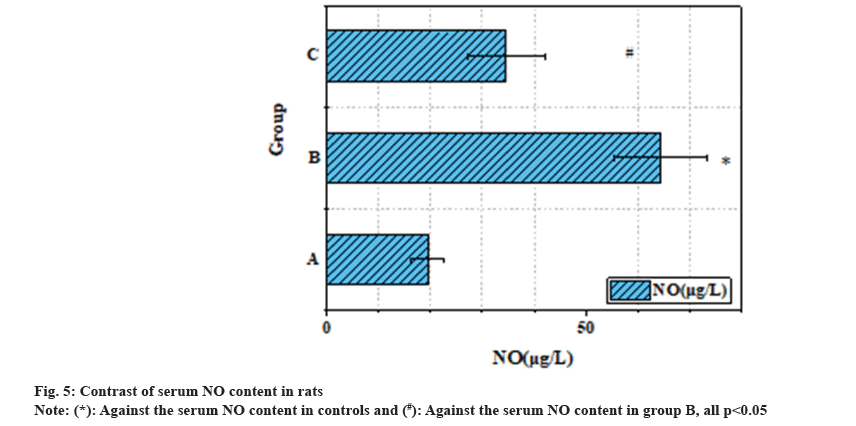
Fig. 5 illustrates the contrast of serum NO content in rats. The serum NO levels of controls, groups B and C were (19.41±3.14) μg/l, (64.27±8.96) μg/l and (34.62±7.35) μg/l, respectively. As against the controls, the serum NO content of the groups B and C had an obvious raise, and as against the group B, that of subjects with SME intervention had an obvious decrease (p<0.05).
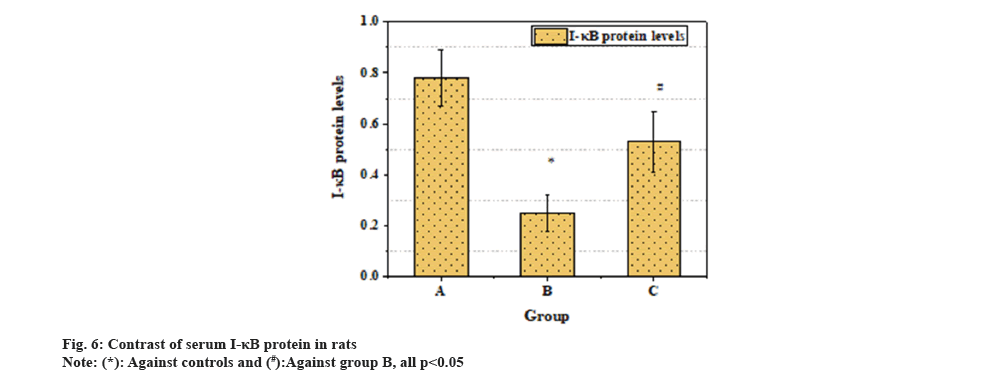
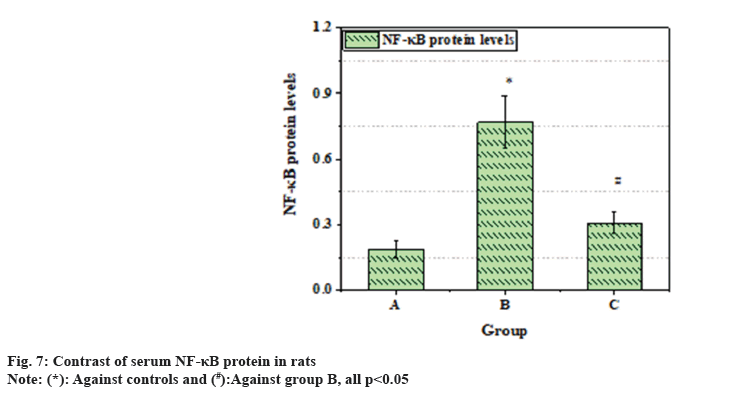
Fig. 6 illustrates the contrast of serum I-κB protein in rats. Fig. 7 illustrates a contrast of serum NF-κB protein in rats. As against controls, the levels of serum I-κB protein had an obvious decrease, and the levels of NF-κB protein had a clear increase in groups B and C (p<0.05). As against group B, the level of serum I-κB protein was clearly raised, and the level of NF-κB protein had an obvious decrease in subjects with SME intervention (p<0.05).
Knee arthritis is a common degenerative joint disease, and its occurrence and development are closely related to oxidative stress, inflammatory response, and activation of NF-κB signaling pathway[16]. As a TCM, SME has shown a wide range of medicinal value in a variety of diseases, especially in antioxidant and anti-inflammatory effects[17,18]. Therefore, this article aimed to evaluate the potential of SME in knee arthritis in rats. The rats were assessed for disease severity (Mankin score), oxidative stress level (relative expression of MDA and SOD in serum), inflammatory response level (serum TNF-α and NO content), and regulation of NF-κB signaling pathway (serum I-κB and NF-κB protein). It was to investigate the outcome of SME on knee arthritis and its possible mechanism.
According to the results of Mankin score, as against the controls, the Mankin score of the group B was clearly raised, while the score of subjects with SME intervention was markedly decreased. It suggested that SME had a therapeutic outcome on knee arthritis and can reduce the severity of the disease.
The results of serum MDA and SOD revealed the relative expression of serum MDA was markedly increased, while that of serum SOD had a marked decrease in group B and subjects with SME intervention. However, as against group B, the relative expression of MDA in serum was decreased, and that of SOD in serum was increased in subjects with SME intervention. It indicated that SME could protect against knee arthritis by reducing oxidative stress and enhancing antioxidant capacity. The serum levels of TNF-α and NO in group B and subjects with SME intervention had a marked increase. As against group B, the serum levels of TNF-α and NO in subjects with SME intervention had a marked decrease. It revealed that SME may improve the symptoms of knee arthritis by suppressing the inflammatory response.
According to the serum I-κB and NF-κB protein, the serum I-κB protein in group B and subjects with SME intervention had a marked decrease, while the NF-κB protein was markedly increased. As against group B, the serum I-κB protein in subjects with SME intervention was obviously raised, and the NF-κB protein was markedly decreased. Therefore, SME may exert therapeutic outcomes on knee arthritis by modulating the NF-κB signaling pathway to suppress inflammatory responses.
In contrast to previous similar studies, this article further clarified the therapeutic potential of SME in knee arthritis. S. miltiorrhiza, as an important medicinal herb, has been widely adopted in clinical practice for the treatment of a variety of diseases. As against other studies, this article more comprehensively evaluated the therapeutic outcomes of SME by comprehensively analyzing multiple indicators. The results showed that SME could markedly improve the symptoms of knee arthritis in rats, reduce the level of oxidative stress and inflammatory response, and play a role by regulating the NF-κB signaling pathway[19].
One study reported the therapeutic effect of SME on arthritis, and it improved the symptoms of arthritis by reducing the inflammatory response and oxidative stress levels[20]. This is consistent with the results of this article and supports the protective role of SME in TA.
In addition, it has been shown that SME has the ability to regulate the NF-κB signaling pathway, thereby suppressing the inflammatory response[21]. NF-κB signaling pathway plays a major role in inflammatory response, and its activation is closely related to the occurrence and development of arthritis[22-24]. Therefore, SME may exert its anti-inflammatory effect by suppressing the NF-κB signaling pathway and reduce the inflammatory symptoms of TA.
However, despite the breakthrough of this article, there are still some limitations. First, this article adopted an animal model, so the application of the results to humans still needs to be further verified. Secondly, the mechanism of SME action is not explored in depth, and more studies are needed to elucidate its detailed molecular mechanisms. In addition, the therapeutic outcomes of SME may vary based on different stages and types of knee arthritis, and further studies are needed to optimize the treatment plan.
In conclusion, it revealed SME had the potential to alleviate the symptoms of knee osteoarthritis, which may act by reducing oxidative stress, suppressing inflammatory response, and regulating NF-κB signaling pathway. Based on the medicinal value of SME in clinical applications, SME have important clinical application prospects in knee arthritis. However, further clinical studies and mechanistic studies are still necessary to further confirm its efficacy and elucidate its mechanism of action to provide more effective drug options for the treatment of knee arthritis.
The results of this article suggested the potential efficacy of SME in knee arthritis. By reducing disease severity, reducing oxidative stress, suppressing inflammatory response, and regulating NF-κB signaling pathway, SME have shown the ability to improve the symptoms of knee osteoarthritis. This is consistent with the medicinal value of SME as a TCM in antioxidant and anti-inflammatory aspects. However, there are some limitations in this article. First, the results from animal models need to be further validated in humans to determine the prospects for clinical application of SME. Secondly, despite the multiple indicators observed in this article, the mechanism of SME action has not been thoroughly studied, and more experiments are needed to elucidate its molecular mechanism. In addition, the efficacy of SME may be different for different types and stages of knee arthritis, and further studies are needed to optimize the treatment plan. In conclusion, SME indicated some therapeutic potential in knee arthritis, with the ability to alleviate symptoms, and may act by reducing oxidative stress, suppressing inflammatory response, and regulating NF-κB signaling pathway.
Conflict of interests:
The authors declared no conflict of interests.
References
- Whittaker JL, Losciale JM, Juhl CB, Thorlund JB, Lundberg M, Truong LK, et al. Risk factors for knee osteoarthritis after traumatic knee injury: A systematic review and meta-analysis of randomised controlled trials and cohort studies for the OPTIKNEE Consensus. Br J Sports Med 2022;56(24):1406-21.
[Crossref] [Google Scholar] [PubMed]
- Zhang L, Han L, Wang X, Wei Y, Zheng J, Zhao L, et al. Exploring the mechanisms underlying the therapeutic effect of Salvia miltiorrhiza in diabetic nephropathy using network pharmacology and molecular docking. Biosci Rep 2021;41(6):BSR20203520.
[Crossref] [Google Scholar] [PubMed]
- Jin GR, Zhang YL, Yap J, Boisvert WA, Lee BH. Hair growth potential of Salvia plebeia extract and its associated mechanisms. Pharm Biol 2020;58(1):400-9.
[Crossref] [Google Scholar] [PubMed]
- Dinel AL, Lucas C, Guillemet D, Layé S, Pallet V, Joffre C. Chronic supplementation with a mix of Salvia officinalis and Salvia lavandulaefolia improves morris water maze learning in normal adult C57Bl/6J mice. Nutrients 2020;12(6):1777.
[Crossref] [Google Scholar] [PubMed]
- Schönknecht K, Surdacka A, Rudenko L. Effectiveness of composed herbal extract in the treatment of gingivitis and oral and pharyngeal mucosa–Review of studies. WiadLek 2021;74(7):1737-49.
[Google Scholar] [PubMed]
- Vázquez‑Leon P, Arenas‑Martínez U, Fregoso‑Aguilar D, Juan E, Miranda‑Paez A. Salvia divinorum increases alcohol intake and tonic immobility whilst decreasing food intake in Wistar rats. Acta Neurobiol Exp 2021;81(1):34-42.
[Crossref] [Google Scholar] [PubMed]
- Veenstra JP, Johnson JJ. Rosemary (Salvia rosmarinus): Health-promoting benefits and food preservative properties. Int J Nutr 2021;6(4):1.
[Google Scholar] [PubMed]
- Raisi A, Dezfoulian O, Davoodi F, Taheri S, Ghahremani SA. Salvia miltiorrhiza hydroalcoholic extract inhibits postoperative peritoneal adhesions in rats. BMC Complement Med Ther 2021;21(1):126.
[Crossref] [Google Scholar] [PubMed]
- Meng H, Wu J, Shen L, Chen G, Jin L, Yan M, et al. Microwave assisted extraction, characterization of a polysaccharide from Salvia miltiorrhiza Bunge and its antioxidant effects via ferroptosis-mediated activation of the Nrf2/HO-1 pathway. Int J Biol Macromol 2022;215:398-412.
[Crossref] [Google Scholar] [PubMed]
- Tlacomulco-Flores LL, Déciga-Campos M, González-Trujano ME, Carballo-Villalobos AI, Pellicer F. Antinociceptive effects of Salvia divinorum and bioactive salvinorins in experimental pain models in mice. J Ethnopharmacol 2020;248:112276.
[Crossref] [Google Scholar] [PubMed]
- Demiroglu M. Functional outcomes of proximal row carpectomy and posterior interosseous neurectomy in degenerative arthritis of the wrist. Acta Med Mediterr 2018;34(3):631-6.
- Zhang K, Liang F, Qaria MA, Wang H, Lin M, Zhang F. Roles of 630 nm red light-emitting diode in inhibition of RhoA signal transduction pathway via reducing PLEKHG5 expression and alleviation of inflammatory response in macrophages. J Biol Regulators Homeostatic Agents 2022;36(5):1419-26.
- Zi J, Wang F, Liu Z, Wang Y, Qiu L, Zhu G, et al. Impact of toll-like receptor 4 expression on inflammatory responses related to premature membrane rupture induced by lipopolysaccharide. Discov Med 2023;35(176):429-35.
[Crossref] [Google Scholar] [PubMed]
- Ying T, Ling C, Xiao F. Effects of probiotics on clinical efficacy, cellular immune function and safety in children with antibiotic-associated diarrhea. Acta Med Mediterr 2023;39:1067.
- Fadwa EO, Amssayef A, Eddouks M. Anti-hyperglycemic and anti-dyslipidemic activities of the aqueous Salvia hispanica extract in diabetic rat. Cardiovasc Hematol Agents Med Chem 2022;20(1):60-6.
[Crossref] [Google Scholar] [PubMed]
- Yuen CW, Murugaiyah V, Najimudin N, Azzam G. Danshen (Salvia miltiorrhiza) water extract shows potential neuroprotective effects in Caenorhabditis elegans. J Ethnopharmacol 2021;266:113418.
[Crossref] [Google Scholar] [PubMed]
- Li JJ, Wang CM, Wang YJ, Yang Q, Cai WY, Li YJ, et al. Network pharmacology analysis and experimental validation to explore the mechanism of Shenlian extract on myocardial ischemia. J Ethnopharmacol 2022;288:114973.
- Abd El-Motelp BA, Ebrahim MT, Mohamed HK. Salvia officinalis extract and 17β-estradiol suppresses ovariectomy induced osteoporosis in female rats. Pak J Biol Sci 2021;24(3):434-44.
[Crossref] [Google Scholar] [PubMed]
- Askari SF, Avan R, Tayarani-Najaran Z, Sahebkar A, Eghbali S. Iranian Salvia species: A phytochemical and pharmacological update. Phytochemistry 2021;183:112619.
[Crossref] [Google Scholar] [PubMed]
- Chammas PE, Hadouiri N, Chammas M, Ramos-Pascual S, Stirling P, Nover L, et al. Proximal row carpectomy generates better mid-to long-term outcomes than four-corner arthrodesis for post-traumatic wrist arthritis: A meta-analysis. Orthop Traumatol Surg Res 2022;108(7):103373.
[Crossref] [Google Scholar] [PubMed]
- Feng JH, Jung JS, Hwang SH, Lee SK, Lee SY, Kwak YG, et al. The mixture of Agrimoniapilosa Ledeb., and Salvia miltiorrhiza Bunge., extract produces analgesic and anti-inflammatory effects in a collagen-induced arthritis mouse model. Anim Cells Syst 2022;26(4):166-73.
[Crossref] [Google Scholar] [PubMed]
- Feng JH, Kim HY, Sim SM, Zuo GL, Jung JS, Hwang SH, et al. The anti-inflammatory and the anti-nociceptive effects of mixed Agrimoniapilosa Ledeb. and Salvia miltiorrhiza Bunge extract. Plants 2021;10(6):1234.
[Crossref] [Google Scholar] [PubMed]
- Zhang L, Jiang S, Guan Z, Huang J, Yin Z, Tan G, et al. Effect of Salvia miltiorrhiza Bunge extracts on improving the efficacy and reducing the toxicity of Tripterygium wilfordii polyglycosides in the treatment of rheumatoid arthritis. J Ethnopharmacol 2023;317:116782.
[Crossref] [Google Scholar] [PubMed]
- Liu S, Zhao XY, Li JF, Lu ZP, Zhang XG. Network meta-analysis of Chinese medicine injections in treatment of rheumatoid arthritis. Zhongguo Zhong Yao Za Zhi 2022;47(20):5627-41.
[Crossref] [Google Scholar] [PubMed]