- *Corresponding Author:
- R. R. Alavala
Shobhaben Pratapbhai Patel School of Pharmacy and Technology Management, Mumbai, Maharashtra 400056, India
E-mail: sekhar7.pharm@gmail.com
| Date of Received | 05 January 2022 |
| Date of Revision | 14 August 2022 |
| Date of Acceptance | 15 May 2023 |
| Indian J Pharm Sci 2023;85(3):644-651 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Cardiac problems are the foremost reason for morbidity and mortality in patients with end-stage renal disease caused by hemodialysis. Many of these patients suffer from increased blood pressure, and acceptable control of blood pressure is a task in these patients because of multifactorial etiology. The present study aims to find out the best possible drug or combination of drugs that can better control blood pressure and improve the quality of life of these patients. It is a multi-centered retrospective study design it was accessed in the patients who visited the Haemodialysis unit of Nephrology unit of Mahatma Gandhi Memorial Hospital, Warangal and Vishwas Super Speciality Hospital, Hanamkonda. The collected data related to demographic characteristics, comorbidities, clinical pathology parameters, current therapy of antihypertensive drugs and blood pressure control (pre-dialysis and post-dialysis) were noted and analysed. 56.60 % of patients on hemodialysis who are suffering from hypertension with the age group of 41-60 y (46.47 %) majority of the population was illiterates with a count of 210 (37.97 %) and business people were of 196 (35.44 %). A combination of amlodipine with metaprolol most frequently prescribed agents (31.82 %), it was significantly (p<0.0001) reducing the systolic blood pressure and diastolic blood pressure in intra (142.80±14.49; 75.13±7.56), post-dialysis (122.29±10.81; 67.91±7.64) respectively compared with pre-dialysis (161.72±14.78; 81.66±.6.99). The mean intradialytic weight gain was 2.65 kg. In post dialysis treatment, the greatest mean (95 % confidence interval) changes in creatinine (p<0.0353), albumin (p<0.0001), Kt/v (p<0.0001 and mean arterial pressure reduced (p<0.0001) in post-dialysis compared to pre-dialysis respectively. The combination of amlodipine with metaprolol frequently prescribed medication provides adequate blood pressure control in all phases of dialysis with the least intra-dialysis complication.
Keywords
Hemodialysis, blood pressure, amlodipine, metoprolol, anti-hypertensives
Hypertension is the most common comorbidity condition in hemodialysis patients and is usually tough to control. Since the high cardiovascular burden in hemodialysis patients, blood pressure control is crucial to recouping the outcomes. Pathophysiology of hypertension in End-Stage Renal Disease (ESRD) is intricate, multifactorial and poses diverse treatment challenges. Adequate control of blood pressure in different stages of dialysis and is difficult with conventional hemodialysis alone but is essential to improve cardiovascular outcomes[1-3]. However, several anti-hypertensive medications are used for patients to manage appropriately.
Pre-Dialysis (PD) hypertension is defined as a creatinine clearance of <15-20 ml/min, the decline in renal function with an expected start of dialysis within 6-12 mo and 1 w Systolic Blood Pressure (SBP) measurements >150 mm of Hg or Diastolic Blood Pressure (DBP) >85 mm of Hg[4-6]. Intradialytic Hypertension (ID-HTN) was defined as the rise in mean arterial pressure >15 mm Hg within or immediately post-dialysis. Post dialysis (PD) is defined after a 44 h intradialytic ambulatory BP of ≥135/85 mm of Hg. Besides, it is common practice to withhold anti-hypertensive before dialysis routinely in patients may worsen intradialytic blood pressure control and increase the prevalence of euvolemic ID-HTN. It may also increase the risk of cardiac arrhythmias and further compromise hemodynamic stability during dialysis[2,5,6]. In such situations, the pre-dialysis administration of antihypertensive is appropriate and necessary, and drug choice should be based on the patient's comorbidities, pharmacokinetics and dialyzability[7]. First-line interventions for blood pressure control should focus on sodium restriction, adequate sodium removal during hemodialysis, and attaining an adequate dry weight. Despite these interventions, adequate blood pressure control with thrice-weekly hemodialysis typically requires the addition of pharmacologic agents.
Some studies revealed the first-line anti-hypertensive agents based on their safety profile and benefit as angiotensin-converting enzyme inhibitors and angiotensin receptor blockers[1]. β-blockers and combined α- and β-blockers should also be used in patients with cardiovascular disease or congestive heart failure and may improve outcomes in these populations. Calcium channel blockers and direct vasodilators are also effective for controlling blood pressure. In patients who are non-compliant with therapy, renally eliminated agents (such as lisinopril and atenolol) can be given thrice weekly the following hemodialysis. Newer antihypertensive agents, such as direct renin inhibitors, may provide alternative options to improve blood pressure but require testing for efficacy and safety in hemodialysis patients [1,4,7].
Materials and Methods
Study design and methodology:
It is a multi-centered retrospective study design, which accessed the patients who visited the Hemodialysis unit of Nephrology unit of Mahatma Gandhi Medical (MGM) Hospital, Warangal, and Vishwas Super Specialty Hospital, Hanamkonda. The study protocol was done by the ideologies of the Declaration of Helsinki and was approved by the Ethics Committee of the VCOP.
Study population:
A total of 596 patients with renal failure patients aged ≥18 y undergoing hemodialysis in the Nephrology Unit of MGM Hospital, Warangal, and Vishwas Super Specialty Hospital, Hanamkonda on a thrice weekly basis for at least 3 mo were included in the present study. Patients were excluded if they were on dialysis for <2 or >8 h, if they received a renal transplant, or if their BP measurement data were unavailable. Informed consent was taken from all the patients. Overall, 553 hemodialysis patients participated in the study based on our inclusion and exclusion criteria of the protocol.
Collection of data:
Demographic characteristics (e.g., age, gender, weight, body mass index, educational status, and occupation type), comorbidities (diabetes, hypertension, diabetic nephropathy, chronic glomerulonephritis, polycystic kidney disease, and toxic nephropathy), sodium, potassium, creatinine, albumin, hemoglobin, Kt/V, body mass index, mean arterial pressure and mean heart rate and a complete list of medication obtained from study centres.
Statistical analysis:
Descriptive statistics was used to generate results. Data was analyzed by Graph Pad Prism version 5 using Paired t-test. The p-value (<0.05) was considered statistically significant.
Results and Discussion
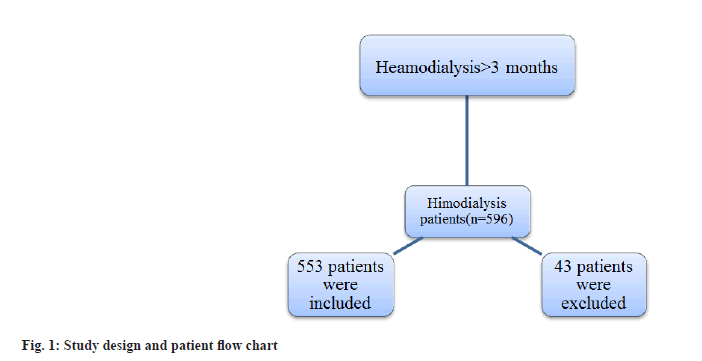
The demographic and clinical characteristics of the participants were shown in Table 1. For this study, 596 patients were recruited. They underwent hemodialysis in the dialysis unit of MGM Hospital. During the treatment, 43 patients were excluded from the study, whichever was due to no sufficient data available or gone the dialysis center when getting only limited dialysis therapy (<1 mo). Overall, 553 hemodialysis patients satisfied our inclusion standards and were included in our statistical analysis (fig. 1).
| Variables | Frequency N (%) | Significance |
|---|---|---|
| Sex | p=0.008 | |
| Male | 353(63.83) | |
| Female | 200(36.16) | |
| Age | ||
| Male | 52.25±12.67 | |
| Female | 42.07±11.56 |
Table 1: Demographic Characteristics Of Participants.
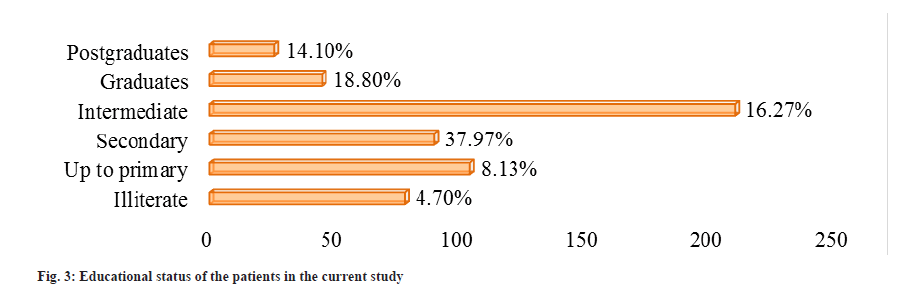
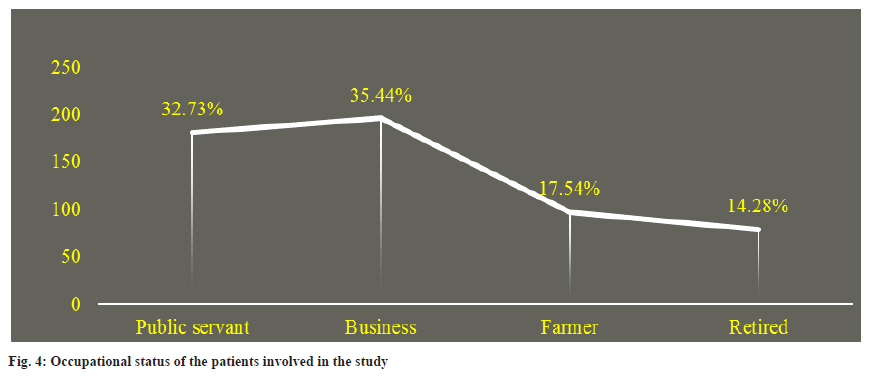
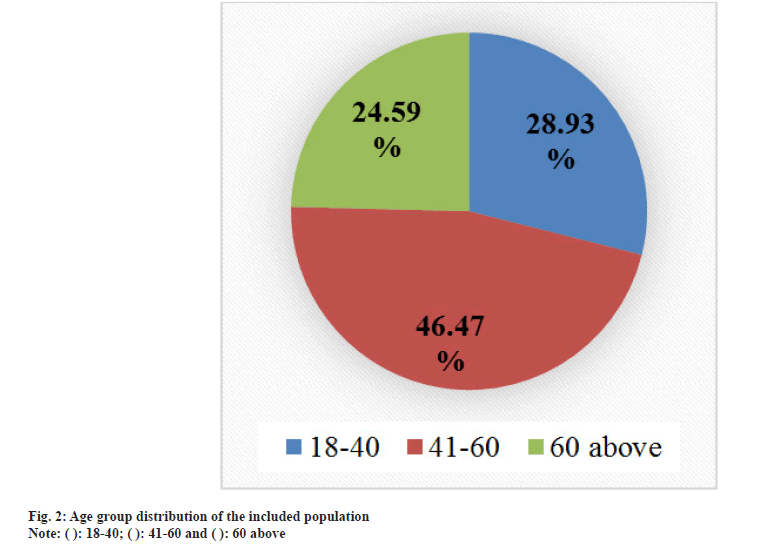
From the selected patients, 353 (63.83 %) were male, and 200 (36.16 %) were female, the greater number of patients from the age group of 41-60 y (46.47 %) followed by the patient age group of 18-40 (28.93 %) and above 60 (24.59 %) were on antihypertensive therapy, they had intermediate 210 (37.97 %) and mainly were business people 196 (35.44 %) (Table 1 and fig. 2-fig. 4).
Comorbidity conditions in patients of ESRD leading to hemodialysis:
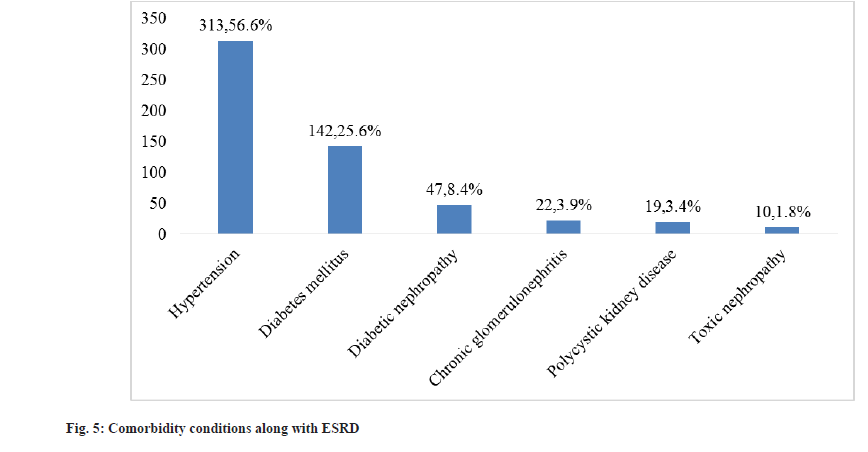
Hypertension is the top comorbidity condition 313 (56.60 %), followed by diabetes mellitus 142 (25.67 %) and diabetic nephropathy 47 (8.49 %) (fig. 5).
Antihypertensive agents prescribed pattern in hemodialysis:
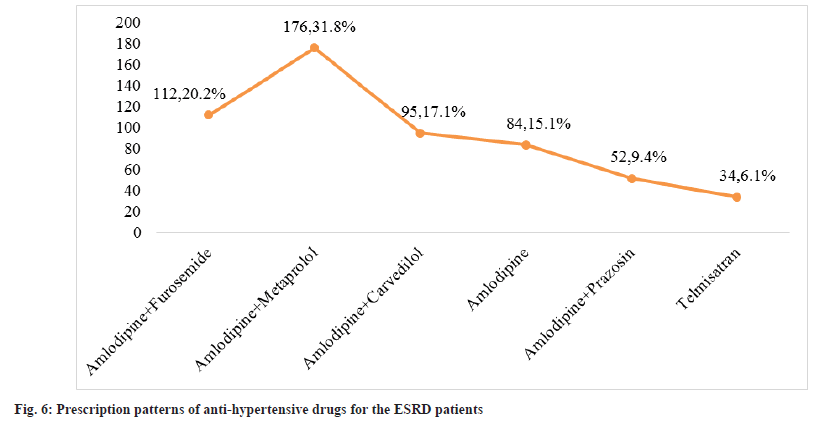
553 patients were included in the work, 313 (56.60 %) were hypertensive and prescribed antihypertensive medicine. A combination of amlodipine with metaprolol most frequently prescribed agents (31.82 %) followed by Amlodipine+Furosemide (20.25 %) and amlodipine+carvedilol (17.17 %) (fig. 6).
Efficacy of different antihypertensive drugs:
The selected patients on dialysis weekly thrice and for the treatment of hypertension combination is provided the average blood pressure control in inter-dialysis and post dialysis. The combination of amlodipine with metaprolol and significantly (p<0.0001) reduce the SBP and DBP in inter (154.20±13.42; 76.25±6.48), post-dialysis (122.29±10.81; 67.91±7.64) respectively compared with pre-dialysis (161.72±14.78; 81.66±.6.99). The amlodipine increases the SBP and DBP significantly in post-dialysis conditions, but amlodipine with prazosin and telmisatran in inter-dialysis blood pressure is not regulated but significantly (p<0.0001) controlled in postdialysis conditions. Efficacy of antihypertensive drugs in regulating post-dialysis blood pressure; Amlodipine + Metoprolol > Amlodipine + Furosemide > Telmisartan > Amlodipine + Carvedilol>Amlodipine respectively (Table 2).
| Treatment | Pre-dialysis BP (mm of Hg) | Intra- dialysis BP (mm of Hg) | Post-dialysis BP (mm of Hg) | p-Value | |||
|---|---|---|---|---|---|---|---|
| SBP | DBP | SBP | DBP | SBP | DBP | ||
| Amd+Fur | 169.86±15.44 | 91.76±7.33 | 168.20±12.04 | 80.42±8.28 | 131.28±12.99¥,δ | 68.66±9.41¥,δ | <0.0001 |
| Amd+Met | 161.72±14.78 | 81.66±.6.99 | 154.60±13.42 | 76.25±6.48 | 122.29±10.81¥,δ | 67.91±7.64¥,δ | <0.0001 |
| Amd+Card | 158.70±13.46 | 76.59±4.95 | 155.66±12.76 | 75.42±5.82 | 135.40±1136¥,δ | 69.82±6.38¥,δ | <0.0001 |
| Amd | 154.55±16.40 | 92.13±5.96 | 153.56±10.52 | 88.62±7.52 | 130.26±10, .31¥,δ | 72.44±4.64¥,δ | <0.0001 |
| Amd+Prz | 158.22±14.82 | 89.43±6.04 | 157.66±10.52 | 85.60±5.16 | 129.55±10.21¥,δ | 65.91±5.92¥,δ | <0.0001 |
| Tlm | 143.24±11.76 | 88.66±5.91 | 141.90±11.47 | 86.34±5.46 | 131.39±9.99¥,δ | 80.89±5.28¥,δ | <0.0001 |
Note: Amd: Amlodipine; Fur: Furosemide; Met: Metoprolol; Card: Carvedilol; Prz: Prazosin; Tlm: Telmisatran; ¥: Pre vs. Post and δ: Intra vs. Post
Table 2: Efficacy Of Different Antihypertensive Drugs.
Clinical and biochemical parameters:
The mean pre and post dialytic body weights were 62.81 and 60.16 kg respectively. The mean interdialytic weight gain was 2.65 kg. In post dialysis treatment the greatest mean (95 % confidence interval) changes in creatinine (17.11 [1.195 to 33.03] μmol/l; p<0.0353), albumin (0.75 [0.680 to 0.819]g/l; p<0.0001), Kt/v (0.40[0.365 to 0.043]; p<0.0001) and mean arterial pressure reduced (18.78 [17.49 to 20.07] mm of Hg; p<0.0001) in post-dialysis compared to pre-dialysis respectively (Table 3).
| Variables | Pre-dialysis | Post-dialysis | p-Value | 95 % confidence intervals |
|---|---|---|---|---|
| Weight gain | 62.81±12.50 | 60.16±11.00 | 0.0001 | 1.299 to 4.001 |
| Sodium (mmol/l) | 116.10±11.19 | 136.21±13.10 | <0.0001 | -21.51 to -18.71 |
| Potassium(mmol/l) | 5.02±0.61 | 5.28±0.68 | <0.0001 | -0.334 to 0.185 |
| Creatinine (µmol/l) | 856.92±134.10 | 839.81±142.52 | 0.0353* | 1.195 to 33.03 |
| Albumin (g/l) | 4.31±0.52 | 3.56±0.67 | <0.0001 | 0.680 to 0.819 |
| Hemoglobin (g/dl) | 8.35±1.32 | 12.74±1.16 | <0.0001 | -4.533 to -4.247 |
| Kt/V | 1.80±0.34 | 1.40±0.25 | <0.0001 | 0.365 to 0.043 |
| Body mass index, kg/m2 | 20.67±4.24 | 21.80±4.01 | <0.0001 | -1.604 to -0.656 |
| Mean arterial pressure (mm Hg) | 121.34±10.78 | 102.56±11.64 | <0.0001 | 17.49 to 20.07 |
| Mean Heart rate (bpm) | 75.00±5.02 | 86.30±6.83 | <0.0001 | -11.99 to -10.61 |
Table 3: In Pre And Post Dialysis Changes With Clinical And Biochemical Parameters
The majority of the patients of ESRD leading to Hemodialysis suffer from hypertension. Hypertension exists in up to 90 % of ESRD patients unrelatedly to the pathogenesis of kidney disease. Hypertension is acknowledged as a significant adaptable cause for advancing Chronic Kidney Disease (CKD) to ESRD and complete cardiovascular morbidity and mortality. Clinical guidelines-derived treatment objectives denote the ethics of evidence-based treatments for dialysis patients[8,9].
The selection of a particular class of medications should be individualized for each patient, a process that involves considering comorbidities, blood pressure response to dialysis, drug clearance with dialysis, and side effect profile. As in the general hypertensive population, compelling indications may warrant the use of specific agents. As in the general hypertensive population, compelling indications may warrant the use of specific agents. Angiotensin Converting Enzyme (ACE) inhibitors, Angiotensin II Receptor Blockers (ARB) and beta blockers likely confer the most cardio protection, given effects on vascular stiffness and cardiac remodelling. Thus, these medications are reasonable first-line anti-hypertensive agents. As cardiac conditions are frequent comorbidities in dialysis patients, the use of these agents is further bolstered. The presence of intradialytic hypotension or hypertension may inform the decision between use of ACE inhibitor or ARB. Calcium Channel Blockers (CCBs) are effective add-on medications[10].
Although BP levels <140/90 mm of Hg are suggested by existing dialysis guidelines[11]. The ideal timing and method of BP measurement have yet to be defined, compared to pre-dialysis or intradialytic or post-dialysis BP measurements, for better mean BP correlates. The present study representing more antihypertensive treatment uses considerably affects blood pressure changes in an advanced CKD with a higher incidence of hypertension. Presently CKD is fluctuating down on the way to the younger age group, which can be owed to alteration of certain insalubrious lifestyle which influences the individuals to initial change of the principal diseases like hypertension and diabetes mellitus owing to initial improvement of CKD as a complication. The mean age of progress of the ESRD and essential renal replacement therapy is much lower in India than in other countries[12,13]. Our study compares the BP medication patterns in hemodialysis patients with dialysis period. CCBs were the most common ones to be used. Usage of RAS blockers was miserable.
In the present study, more males 353 with higher mean age (52.25±12.67), which depicts the propensity for the progress of CKD in older males, and the commonest cause of CKD in patients on keep hemodialysis is hypertension and diabetes mellitus. From many studies, the males through greater mean age, which depicts the propensity, intended for the progress of CKD in adult males and the chief cause of CKD in patients on keep hemodialysis is diabetic nephropathy[14]. Hypertension and diabetes mellitus remained the most common disease that led to CKD and lastly, ESRD was parallel to other Indian studies[15]. Many of the victims of ESRD leads to hemodialysis undergo hypertension. By this increase in blood pressure together with a source and a result of CKD. It predisposes these patients to undergo left ventricular hypertrophy, congestive heart failure, stroke and other cardiac and neurological complications cause high injury and death in these patients[16]. In Pre-dialysis SBP, it is a parameter for medical management in the controlling of hypertension, which remained establish to be related through all the blood pressure changes, confirming its helpfulness as a principal metric for hypertension in hemodialysis patients, it explained by Shafi et al.[17]. The present study results in CCBs being most effective in controlling BP, similar study conducted in previous studies in general population with long-term control in BP[17,18]. The perceived effects of CCBs in monitoring in BP might be owing to their vasodilator effects[19] and long half-life[20], as well as the sustained release of CCBs[21]. Treatment with antihypertensive drugs in ESRD patients was accompanying by amended cardiovascular events and mortality[22]. The present endorsement is to employ CCBs as the first-line agent in patients on HD. Additional anti-hypertensive agents are frequently needed for persistent hypertension, and renin-angiotensinaldosterone system and beta-blockers are some of the next recommended therapies [9].
Prescription of particular medications maybe due to physician’s perceived risk of adverse events, cardiovascular risk factors, availability, and affordability of various drugs. CCBs have been shown to decrease stroke and cardiovascular mortality[23]. They possibly interfere with the process of vascular calcification and attenuate the effect of calcium ions from the dialysate on the vasculature. The effectiveness of CCBs in reducing peripheral vascular resistance and ability to lower blood pressure in volume overload as well and has led to their rampant use in dialysis patients[24]. Once-a-day dosing of most of the CCBs also tilts the balance in their favor. Present study also depicts high usage of CCBs.
ACE inhibitors have been shown to decrease residual renal function loss[25] and mortality[26]. Despite evidence pepping in favor of ACE inhibitors/ARB in ESRD population, the use of these medications was dismal in our study. The β-blockers have a proven role in heart failure and coronary artery disease patients[27]. Since deaths in dialysis patients are predominantly attributed to cardiovascular reasons, β-blockers are usually given priority over other classes of antihypertensive agents. In our study too, they were used in majority of patients (31.8 %) received Amlodipine and metaprolol. In our study, carvedilol was also used in much higher percentage (17.1 %). This could possibly stem from the evidence in their favorable effects in dilated cardiomyopathy[28] and better BP control due to lesser removal during dialysis[29,30].
The α-blockers are used mostly in difficult to control BP in patients on multiple anti-hypertensive agents[10]. In our study, they were used as third/ fourth-line agents and were required in higher doses in later period of dialysis period. Most of the patients through ESRD leading to HD need antihypertensive drugs. While in the present study, a combination of Amlodipine with Prazosin and or furosemide was the most regularly prescribed agents, they remained repeatedly allied with intradialysis difficulties. In contrast, a combination of Amlodipine with metaprolol provided adequate blood pressure control in all phases of dialysis with the least intra-dialysis complication. Volume overload due to insufficient dialysis is the chief source of poor regulator of blood pressure in these patients; consequently, CCBs are stated to be the drug of the first choice in patients with volume overload.
Acknowledgments:
Authors wanted to express their gratitude towards Registrar, KLEF Deemed to be University for their consistent support for the smooth conduction of the research work.
Conflict of interests:
The authors declared no conflict of interests.
References
- Agarwal R, Nissenson AR, Batlle D, Coyne DW, Trout JR, Warnock DG. Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United States. Am J Med 2003;115(4):291-7.
[Crossref] [Google Scholar] [PubMed]
- Agarwal R. Epidemiology of interdialytic ambulatory hypertension and the role of volume excess. Am J Nephrol 2011;34(4):381-90.
[Crossref] [Google Scholar] [PubMed]
- Agarwal R. Blood pressure and mortality among hemodialysis patients. Hypertension 2010;55(3):762-8.
[Crossref] [Google Scholar] [PubMed]
- Agarwal R, Flynn J, Pogue V, Rahman M, Reisin E, Weir MR. Assessment and management of hypertension in patients on dialysis. J Am Soc Nephrol 2014;25(8):1630-46.
[Crossref] [Google Scholar] [PubMed]
- Levin NW, Kotanko P, Eckardt KU, Kasiske BL, Chazot C, Cheung AK, et al. Blood pressure in chronic kidney disease stage 5D—report from a Kidney Disease: Improving global outcomes controversies conference. Kidney Int 2010;77(4):273-84.
[Crossref] [Google Scholar] [PubMed]
- Tandon T, Sinha AD, Agarwal R. Shorter delivered dialysis times associate with a higher and more difficult to treat blood pressure. Nephrol Dial Transplant 2013;28(6):1562-8.
[Crossref] [Google Scholar] [PubMed]
- Agarwal R, Peixoto AJ, Santos SF, Zoccali C. Pre-and postdialysis blood pressures are imprecise estimates of interdialytic ambulatory blood pressure. Clin J Am Soc Nephrol 2006;1(3):389-98.
[Crossref] [Google Scholar] [PubMed]
- Van Buren PN, Inrig JK. Hypertension and hemodialysis: Pathophysiology and outcomes in adult and pediatric populations. Pediatr Nephrol 2012;27:339-50.
[Crossref] [Google Scholar] [PubMed]
- Gorsane I, Mahfoudhi M, Younsi F, Helal I, Abdallah TB. Prevalence and risk factors of hypertension in hemodialysis. Open J Nephrol 2015;5(2):54-60.
[Crossref] [Google Scholar] [PubMed]
- Inrig JK. Antihypertensive agents in hemodialysis patients: A current perspective. Semin Dial 2010;23(3):290-7.
[Crossref] [Google Scholar] [PubMed]
- Alebiosu CO, Ayodele OO, Abbas A, Olutoyin AI. Chronic renal failure at the Olabisi Onabanjo university teaching hospital, Sagamu, Nigeria. Afr Health Sci 2006;6(3):132-8.
[Crossref] [Google Scholar] [PubMed]
- Dash SC, Agarwal SK. Incidence of chronic kidney disease in India. Nephrol Dial Transplant 2006;21(1):232-3.
[Crossref] [Google Scholar] [PubMed]
- Ahmad R, Rehman S, Habib A, Naim F. Efficacy of various antihypertensive drugs in the treatment of hypertension in the patients of end-stage renal disease leading to haemodialysis: A retrospective study. J Nephrol Ther 2016;7(283):2161-0959.
- Gheith O, Farouk N, Nampoory N, Halim MA, Al-Otaibi T. Diabetic kidney disease: World-wide difference of prevalence and risk factors. J Nephropharmacol 2016;5(1):49-56.
[Google Scholar] [PubMed]
- Modi GK, Jha V. The incidence of end-stage renal disease in India: A population-based study. Kidney Int 2006;70(12):2131-3.
[Crossref] [Google Scholar] [PubMed]
- Takeda A, Toda T, Fujii T, Shinohara S, Sasaki S, Matsui N. Discordance of influence of hypertension on mortality and cardiovascular risk in hemodialysis patients. Am J Kidney Dis 2005;45(1):112-8.
[Crossref] [Google Scholar] [PubMed]
- Shafi T, Sozio SM, Bandeen-Roche KJ, Ephraim PL, Luly JR, Peter WL, et al. Predialysis systolic BP variability and outcomes in hemodialysis patients. J Am Soc Nephrol 2014;25(4):799-809.
[Crossref] [Google Scholar] [PubMed]
- Umemoto S, Ogihara T, Matsuzaki M, Rakugi H, Ohashi Y, Saruta T. Effects of calcium channel blocker-based combinations on intra-individual blood pressure variability: Post hoc analysis of the COPE trial. Hypertens Res 2016;39(1):46-53.
[Crossref] [Google Scholar] [PubMed]
- Wang JG, Yan P, Jeffers BW. Effects of amlodipine and other classes of antihypertensive drugs on long-term blood pressure variability: Evidence from randomized controlled trials. J Am Soc Hypertens 2014;8:340-349.
[Crossref] [Google Scholar] [PubMed]
- Yao K, Nagashima K, Miki H. Pharmacological, pharmacokinetic, and clinical properties of benidipine hydrochloride, a novel, long-acting calcium channel blocker. J Pharmacol Sci 2006;100(4):243-61.
[Crossref] [Google Scholar] [PubMed]
- Pico JC, Domínguez G, Negri AL, Caubet JC, Terragno NA. Comparative pharmacokinetics of a single oral dose of two formulations of amlodipine. Arzneimittelforschung 2008;58(7):323-7.
[Crossref] [Google Scholar] [PubMed]
- Zhang Y, Agnoletti D, Safar ME, Blacher J. Effect of antihypertensive agents on blood pressure variability: the Natrilix SR versus candesartan and amlodipine in the reduction of systolic blood pressure in hypertensive patients (X-CELLENT) study. Hypertension 2011;58(2):155-60.
[Crossref] [Google Scholar] [PubMed]
- Agarwal R, Sinha AD. Cardiovascular protection with antihypertensive drugs in dialysis patients: Systematic review and meta-analysis. Hypertension 2009;53(5):860-6.
[Crossref] [Google Scholar] [PubMed]
- Tepel M, Van der Giet M, Park A, Zidek W. Association of calcium channel blockers and mortality in haemodialysis patients. Clin Sci 2002;103(5):511-5.
[Crossref] [Google Scholar] [PubMed]
- London GM, Marchais SJ, Guerin AP, Metivier F, Safar ME, Fabiani F, et al. Salt and water retention and calcium blockade in uremia. Circulation 1990;82(1):105-13.
[Crossref] [Google Scholar] [PubMed]
- Moist LM, Port FK, Orzol SM, Young EW, Ostbye T, Wolfe RA, et al. Predictors of loss of residual renal function among new dialysis patients. J Am Soc Nephrol 2000;11(3):556-64.
[Crossref] [Google Scholar] [PubMed]
- McCullough PA, Sandberg KR, Yee J, Hudson MP. Mortality benefit of angiotensin-converting enzyme inhibitors after cardiac events in patients with end-stage renal disease. J Renin Angiotensin Aldosterone Syst 2002;3(3):188-91.
[Crossref] [Google Scholar] [PubMed]
- Workgroup KD. K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis 2005;45:S1-53.
[Google Scholar] [PubMed]
- Cice G, Ferrara L, D’Andrea A, D’Isa S, Di Benedetto A, Cittadini A, et al. Carvedilol increases two-year survivalin dialysis patients with dilated cardiomyopathy: A prospective, placebo-controlled trial. J Am Coll Cardiol 2003;41(9):1438-44.
[Crossref] [Google Scholar] [PubMed]
- Miki S, Masumura H, Kaifu Y, Yuasa S. Pharmacokinetics and efficacy of carvedilol in chronic hemodialysis patients with hypertension. J Cardiovasc Pharmacol 1991;18:S68.
[Google Scholar] [PubMed]
 ): 18-40; (
): 18-40; ( ): 41-60 and (
): 41-60 and ( ): 60 above
): 60 above