- Corresponding Author:
- U. Aiman
Department of Pharmacology, Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh-202 002, India
E-mail: aimanjnmc@gmail.com
| Date of Submission | 07 April 2014 |
| Date of Revision | 08 September 2014 |
| Date of Acceptance | 13 September 2014 |
| Indian J Pharm Sci 2014;76(6):504-509 |
Abstract
Peripheral arterial disease, being a manifestation of systemic atherosclerosis, carries a high risk of adverse cardiovascular events. Secondary medical prevention therapies of same magnitude as that for coronary artery disease are recommended for peripheral arterial disease patients also. Available evidence indicates that this condition commonly remains underdiagnosed and undertreated. There is lack of any report about management of these patients in India. The objectives of the present study were to characterize the atherosclerotic risk factor profile and pattern of drug prescription for patients of peripheral arterial disease at a tertiary care teaching hospital and to compare this management with standard guidelines. Data were collected from prescriptions of patients attending cardiothoracic and vascular surgery outpatient department with diagnosis of atherosclerotic peripheral arterial disease from July 2012 to Jun 2013. One hundred twenty prescriptions were analysed. The mean age (±SD) of patients was 53±7.18 years and 23.3% were females. History of smoking, either past or present, was present in 91.6% patients. History of ischemic heart disease was present in 25%, while 26.7% patients were diabetic. Mean number of cardiovascular risk factors was 2.6. The percentage of eligible patients who were receiving a particular drug was 100% for aspirin and statins, 48.3% for angiotensin converting enzyme inhibitors, 46.7% for beta blockers and 66.7% for cilostazol. The vascular surgeons of this centre are using antiplatelet agents and statins adequately for peripheral arterial disease. The prescription of angiotensin converting enzyme inhibitors, beta blockers and cilostazol is low. Exercise therapy and smoking cessation need more attention.
Keywords
Cardiovascular disease, atherosclerosis, peripheral arterial disease, smoking cessation
Peripheral arterial disease (PAD) is a common disorder which affects large populations of adults worldwide. It most commonly affects arteries of the lower limband patients mostly present with intermittent claudication. Atherosclerosis is the leading cause of PAD. The prevalence of PAD differs depending upon diagnostic criteria as well as age and risk factors profile of the study population and may range from 3-12% [1]. Prevalence increases further with advancing age and may reach 15-20% in persons >65 years [2,3]. Recently, it was estimated that 54.8 million people were living with PAD in southeast Asia in 2010 (out of 202 million globally) [4].
Due to the common underlying pathologic process (i.e. atherosclerosis), PAD is commonly coexistent with coronary artery disease (CAD) and/or cerebrovascular disease (CVD), which may be diagnosed or undiagnosed. PAD is said to be the third leading cause of atherosclerotic cardiovascular morbidity, following CAD and stroke [4]. Patients of PAD have a 6.6 fold increased risk of death from CAD [5]. Due to this high risk, PAD is considered to be a CAD equivalent condition and requires intensive risk reduction therapy. There is evidence that a large proportion of PAD patients are not treated with atherosclerotic risk reduction therapies (e.g. antiplatelet drugs, statins, angiotensin converting enzyme (ACE) inhibitors) [6-8] despite of evidence that these therapies improve survival in these patients [9,10]. The present study was done to assess the patterns of atherosclerotic risk factors and their management in lower extremity PAD patients at a tertiary teaching hospital of north India.
Materials and Methods
Data acquisition
Data were collected prospectively from prescriptions of patients attending cardiothoracic and vascular surgery OPD with diagnosis of atherosclerotic PAD from July 2012 to Jun 2013. Ethical clearance was obtained from Institutional Ethics Committee of the hospital.
Pattern of risk factors
All prescriptions were analysed for presence of risk factors for atherosclerosis (history of smoking, hypertension, diabetes, dyslipidemia, renal insufficiency, history of ischemic heart disease or cerebrovascular disease), smoking cessation efforts and advice regarding exercise. Ankle brachial index (ABI) was documented if present on prescription.
Pattern of drug prescription
Prescription of drugs for modification of atherosclerotic risk factors (aspirin, ACE inhibitors, beta blockers and lipid lowering drugs) and for intermittent claudication (cilostazol and pentoxyphylline) was recorded. Prescription of drugs for other purposes (e.g. antacids, analgesics or antipyretics, multivitamins) was not recorded.
Assessment of eligibility for drugs
Each prescription was analysed for eligibility for drugs for modification of atherosclerotic risk factors (aspirin, ACE inhibitors, beta blockers and lipid lowering drugs) and for drugs for intermittent claudication (cilostazol and pentoxyphylline). Eligibility was decided based on ACC/AHA and TASC-II guidelines for management of patients of PAD [11,12]. All patients were considered to be eligible for aspirin, ACE inhibitors, lipid lowering drugs and cilostazol. In addition, patients with history of ischemic heart disease (IHD) were considered as eligible for beta blockers. Patients were considered eligible for pentoxiphylline only if cilostazol was contraindicated/not tolerated.
Results and Discussion
A total of 120 prescriptions were analysed. Basal patient characteristics and risk factors for atherosclerosis are presented in Table 1. The mean number of cardiovascular risk factors (smoking, diabetes, hypertension, dyslipidemia) was 2.6, where 29% patients had all 4 risk factors, 35.5% had any 3 risk factors and 65% had any two risk factors.
| Characteristics | Mean ± SD/number (percent) | |
|---|---|---|
| Age (years ± SD) | 53 ± 7.18 | |
| Males | 92 | (76.6) |
| Females | 28 | (23.3) |
| Current smokers | 76 | (63.3) |
| Past smokers | 34 | (28.3) |
| Diabetes | 32 | (26.6) |
| Hypertension (BP >140/90 mm Hg nondiabetics, | 85 | (71.6) |
| >130/80 mm Hg diabetics) | ||
| Abnormal lipid profile (LDL >100 mg/dl) | 86 | (71.6) |
| Renal insufficiency | 7 | (5.8) |
| History of IHD | 30 (25) | |
| Angina | 22 | |
| MI | 8 | |
| Angioplasty/CABG | 6 | |
| History of TIA/CVA | 6 (5) | |
LDL is low density lipoprotein, IHD is ischemic heart disease, MI is myocardial infarction, CABG is coronary artery bypass grafting, TIA is transient ischemic attack, CVA is cerebrovascular accident (N=120)
Table 1: Baseline characteristics of patients
A record of ABI was present on 74 (61.1%) prescriptions. Based on ABI value, mild to moderate PAD (ABI 0.41-0.90) was present in 66 patients while 8 patients had severe PAD (ABI ≤0.40). Advice to quit smoking was offered to all current smokers. Nicotine replacement therapy (patch or gum) was advised to 5 patients. All patients were advised regular walking.
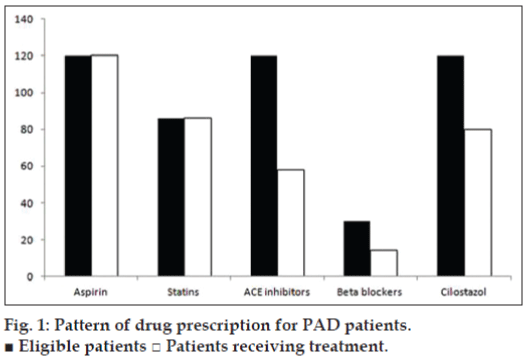
Fig. 1 shows the prescription pattern of drugs for modification of atherosclerotic risk factors (aspirin, statins, ACE inhibitor, beta blocker) or for the treatment of intermittent claudication (cilostazol). All patients were prescribed aspirin. Statin was prescribed to 86 patients while ACE inhibitor (ramipril) was prescribed to 58 patients. Pentoxifylline was prescribed to 72 and cilostazol to 80 patients. Beta blocker was prescribed to 14 patients.
PAD is said to be a global problem of 21st century affecting low and middle income countries worse than high income countries [4]. Evidence exists that there is a lack of awareness of PAD and these patients are usually under diagnosed and under treated [3,6,8,13]. To our knowledge, there is no study reporting pattern of drugs which are being used in India for management of PAD. Therefore, the present study is first to describe pattern of atherosclerosis risk factors and their management in Indian patients of PAD.
ABI is a simple and noninvasive test for establishing a diagnosis of PAD. ABI is the ratio of systolic blood pressure at ankle to that at arm. In normal individuals, ankle systolic pressure is 10-15 mm Hg higher than brachial systolic pressure and thus the normal ABI value is more than 1.00. A value of ABI ≤0.90 is diagnostic of PAD with values between 0.41 and 0.90 reflect mild to moderate PAD and values ≤0.40 reflect severe PAD [11]. In the present study ABI value was available in only 61.1% prescriptions, however in others it was not taken either because of lack of time or because of unawareness of its relevance. ABI has prognostic value not only in predicting wound healing and limb survival but also as an independent predictor of mortality in PAD patients [14]. It becomes even more important in those patients in whom surgical revascularisation planned. Low ABI values have been correlated with high risk of both cardiovascular and cerebrovascular events [15]. Thus, abnormal ABI can serve as a surrogate marker for systemic atherosclerosis.
In the present study, out of 120 patients, history of either current or past smoking was documented in 110 (91.6%) patients. Smoking is a well known risk factor for PAD and appears to be more strongly related with PAD than with CAD [16]. The odds of developing PAD may be as high as 2.3 for former smokers and 4.3 for current smokers. Although evidence also exists for dose response relationship between pack years of smoking and PAD, the number of cigarettes or duration of smoking was not documented in the present study. Smoking may contribute to atherosclerosis, by causing endothelial dysfunction, abnormal lipid profile and altered platelet function.
In the present study, all patients who were smokers were advised to stop smoking; only 5 patients were prescribed nicotine replacement therapy (NRT) in the form of gum (3 patients) and patch (2 patients). Although effective, physician’s advice alone has a low rate of cessation [17]. ACC/AHA guidelines recommend use of any one of the three pharmacotherapies for smoking cessation i.e. nicotine replacement therapy (NRT), bupropion and varenicline. Although the hazards of smoking are well known to medical community, the under use of smoking cessation interventions by medical professionals has been reported [18-20]. Thus, there is an urgent need to enhance training of medical professionals in effective utilisation of smoking cessation interventions. This training should preferably start right from undergraduate period and may be taught to medical students along with subjects of pharmacology, community medicine or general medicine.
All patients in the present study were advised regular walking but there was no specific advice regarding this. Supervised exercise training (SET) programme has been shown to benefit PAD patients, as it increases maximal walking distance by upto 200% [21]. Supervised exercise training is a class I recommendation by ACC/AHA guidelines and should be performed for a minimum of 30 to 45 min in sessions performed at least 3 times per week for a minimum of 12 weeks. In addition, regular exercise programme may be expected to decrease cardiovascular risk in this high risk population. Thus, SET is the only intervention which provides improvements in symptoms and reduces cardiovascular risk both. Despite of these favourable effects, the usefulness of SET remains limited due to the problems of accessibility, travel time and cost. Home based exercise programme is a viable alternative to SET programme when SET is not available or unaffordable. Although less effective than SET, home based exercise programmes can improve walking capacity and quality of life when compared to usual care [22]. Moreover, home based programmes are reported to have higher adherence rates in the long term [23].
History of type 2 diabetes was present in 32 (26.6%) patients. PAD is one of the macrovascular complications of type 2 diabetes and every 1% increase of hemoglobin A1C increases the risk of PAD by 28% [24]. The high prevalence of PAD among diabetic population further emphasizes the importance of measurement of ABI in all diabetics. Ischemic heart disease was present in 30 (25%) patients. Contrary to popular belief, beta blockers are not contraindicated in PAD patients [11] rather they have been shown to decrease incidence of new coronary events by 53% in PAD patients with prior myocardial infarction [25]. Due to their basal cardioprotective effect, beta blockers should be used in all PAD patients who have ischemic heart disease.
Antiplatelet therapy has been shown to reduce adverse cardiovascular events including MI, stroke or vascular death among patients of PAD [26]. Also, low dose aspirin has been shown to reduce the need for peripheral arterial surgery [27]. In the present study all the patients were prescribed aspirin (75-100 mg). The benefits of lowering serum LDL-C with statins in patients of PAD have been reported previously [28]. In addition to prevention of adverse cardiac events, statins have been shown to benefit symptom of intermittent claudication also [29,30]. In the present study, statins (most commonly atorvastatin 20-40 mg) were prescribed to all patients (n=86) who had high LDL (>100 mg/dl). This reflects improved prescription of statins when compared to previous reports about lower statin use by vascular surgeons [31,32]. This improvement in statin use may be due to frequent CME programmes at our hospital which provide opportunity for communication with other specialists e.g. cardiologists. According to ACC/AHA guidelines, LDL goal of <70 mg/dL should be achieved in those PAD patients with very high risk of ischemic events (e.g. diabetes or continued smoking or low HDL cholesterol). If the maximum dose of a single statin fails to achieve this goal then a fibric acid derivative may be combined.
ACE inhibitors are another group of drugs which benefit PAD patients. These agents have been shown to increase resting blood flow as well as blood flow after exercise; they also increase pain free and maximum walking times with improvement in quality of life [33]. In the HOPE study, ramipril was found to reduce major cardiovascular events in both symptomatic as well as asymptomatic PAD [34]. These vasculoprotective effects of ACE-I appear to be independent of their antihypertensive property and may be due to improvement in endothelial function and decreased accumulation of macrophages in intima of arteries, one of the initial steps in the pathogenesis of atherosclerosis. In addition, they also improve insulin resistance and reduce the incidence of type 2 diabetes [35], which is a predisposing factor for PAD. Based on these findings, ACE inhibitor therapy has been suggested as the routine treatment of PAD, regardless of presence or absence of hypertension [36]. In the present study, ACE inhibitors were prescribed to 58 patients only. This underuse of ACE inhibitors in PAD patients has been reported previously also [10,13,37,38].
Cilostazol is a phosphodiesterase 3 inhibitor having antiplatelet and vasodilator properties. It has been shown to improve maximal walking distance by upto 60% after 12-24 weeks of treatment [39]. Apart from these effects, cilostazol has been shown to increase HDL cholesterol and decrease plasma triglyceride levels [40]. However, the clinical relevance of these positive changes in lipid profile remains unknown. It is recommended for all patients of intermittent claudication in the absence of heart failure. While all 120 patients in the present study were eligible for cilostazol, it was prescribed to 80 patients only. Headache, diarrhea and palpitations are common side effects of cilostazol, which may be responsible for underuse of this drug.
Pentoxifylline increases blood flow to the microcirculation and improves oxygenation by reducing blood viscosity and increasing erythrocytic flexibility. The efficacy of pentoxyfylline in PAD has been shown to be inferior to that of cilostazol and in one study, was not significantly different from placebo [41]. It is recommended for those patients of intermittent claudication who do not tolerate cilostazol or have contraindication for it. In the present study, 72 patients were prescribed pentoxyfylline. The reasons for popularity of pentoxifylline seem to be that it was the first drug approved for intermittent claudication and also has better tolerability than cilostazol. One of the reasons for this ambiguity is absence of any national guidelines for management of PAD in India.
PAD is a manifestation of systemic atherosclerosis and patients are at high risk of adverse cardiovascular events. These patients need aggressive risk factor reduction similar to patients of CAD. Medical therapy can substantially improve survival in this group of patients. The utilisation of smoking cessation interventions can help smokers stop smoking and thus reduce the cardiovascular risk. Regular exercise should be promoted by both supervised as well as home based programmes. While antiplatelet agents and statins are being used adequately; use of ACE inhibitors, beta blockers and cilostazol is suboptimal and needs to be increased. Awareness of recognition and optimum management of PAD has to be improved not only among vascular surgeons but all the medical and surgical specialities.
References
- Hiatt WR, Hoag S, Hamman RF. Effect of diagnostic criteria on the prevalence of peripheral arterial disease. The San Luis Valley Diabetes Study. Circulation 1995;91:1472-9.
- Fowkes FG, Housley E, Cawood EH, Macintyre CC, Ruckley CV, Prescott RJ. Edinburgh Artery Study: Prevalence of asymptomatic and symptomatic peripheral arterial disease in the general population. Int J Epidemiol 1991;20:384-92.
- Hirsch AT, Criqui MH, Treat-Jacobson D, Regensteiner JG, Creager MA, Olin JW, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA 2001;286:1317-24.
- Fowkes FG, Rudan D, Rudan I, Aboyans V, Denenberg JO, McDermott MM, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: A systematic review and analysis. Lancet 2013;382:1329-40.
- Criqui MH, Langer RD, Fronek A, Feigelson HS, Klauber MR, McCann TJ, et al. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med 1992;326:381-6.
- Rehring TF, Sandhoff BG, Stolcpart RS, Merenich JA, Hollis HW Jr. Atherosclerotic risk factor control in patients with peripheral arterial disease. J VascSurg 2005;41:816-22.
- Zanati SG, Mouraria GG, Matsubara LS, Giannini M, Matsubara BB. Profile of cardiovascular risk factors and mortality in patients with symptomatic peripheral arterial disease. Clinics (Sao Paulo) 2009;64:323-6.
- Bianchi C, Montalvo V, Ou HW, Bishop V, Abou-Zamzam AM Jr. Pharmacologic risk factor treatment of peripheral arterial disease is lacking and requires vascular surgeon participation. Ann VascSurg 2007;21:163-6.
- Feringa HH, van Waning VH, Bax JJ, Elhendy A, Boersma E, Schouten O, et al. Cardioprotective medication is associated with improved survival in patients with peripheral arterial disease. J Am CollCardiol 2006;47:1182-7.
- Pande RL, Perlstein TS, Beckman JA, Creager MA. Secondary prevention and mortality in peripheral artery disease: National Health and Nutrition Examination Study, 1999 to 2004. Circulation 2011;124:17-23.
- Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): A collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): Endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation 2006;113:e463-654.
- Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J VascSurg 2007;45(Suppl S):S5-67.
- Subherwal S, Patel MR, Kober L, Peterson ED, Jones WS, Gislason GH, et al. Missed opportunities: Despite improvement in use of cardioprotective medications among patients with lower-extremity peripheral artery disease, underuse remains. Circulation 2012;126:1345-54.
- McKenna M, Wolfson S, Kuller L. The ratio of ankle and arm arterial pressure as an independent predictor of mortality. Atherosclerosis 1991;87:119-28.
- Zheng ZJ, Sharrett AR, Chambless LE, Rosamond WD, Nieto FJ, Sheps DS, et al. Associations of ankle-brachial index with clinical coronary heart disease, stroke and preclinical carotid and popliteal atherosclerosis: The Atherosclerosis Risk in Communities (ARIC) Study. Atherosclerosis 1997;131:115-25.
- Lu L, Mackay DF, Pell JP. Meta-analysis of the association between cigarette smoking and peripheral arterial disease. Heart 2014;100:414-23.
- Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev 2013;5:Cd000165.
- Warren GW, Marshall JR, Cummings KM, Toll B, Gritz ER, Hutson A, et al. Practice patterns and perceptions of thoracic oncology providers on tobacco use and cessation in cancer patients. J ThoracOncol 2013;8:543-8.
- Warren GW, Marshall JR, Cummings KM, Toll BA, Gritz ER, Hutson A, et al. Addressing tobacco use in patients with cancer: A survey of american society of clinical oncology members. J OncolPract 2013;9:258-62.
- Weaver KE, Danhauer SC, Tooze JA, Blackstock AW, Spangler J, Thomas L, et al. Smoking cessation counseling beliefs and behaviors of outpatient oncology providers. Oncologist 2012;17:455-62.
- Watson L, Ellis B, Leng GC. Exercise for intermittent claudication. Cochrane Database Syst Rev 2008;7:Cd000990.
- Al-Jundi W, Madbak K, Beard JD, Nawaz S, Tew GA. Systematic Review of Home-based Exercise Programmes for Individuals with Intermittent Claudication. Eur J VascEndovascSurg 2013;46:690-706.
- Ashworth NL, Chad KE, Harrison EL, Reeder BA, Marshall SC. Home versus center based physical activity programs in older adults. Cochrane Database Syst Rev 2005;1:Cd004017.
- Adler AI, Stevens RJ, Neil A, Stratton IM, Boulton AJ, Holman RR. UKPDS 59: Hyperglycemia and other potentially modifiable risk factors for peripheral vascular disease in type 2 diabetes. Diabetes care 2002;25:894-9.
- Aronow WS, Ahn C. Effect of beta blockers on incidence of new coronary events in older persons with prior myocardial infarction and symptomatic peripheral arterial disease. Am J Cardiol 2001;87:1284-6.
- Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002;324:71-86.
- Goldhaber SZ, Manson JE, Stampfer MJ, LaMotte F, Rosner B, Buring JE, et al. Low-dose aspirin and subsequent peripheral arterial surgery in the Physicians’ Health Study. Lancet 1992;340:143-5.
- MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: A randomised placebo-controlled trial. Lancet 2002;360:7-22.
- Aronow WS, Nayak D, Woodworth S, Ahn C. Effect of simvastatin versus placebo on treadmill exercise time until the onset of intermittent claudication in older patients with peripheral arterial disease at six months and at one year after treatment. Am J Cardiol 2003;92:711-2.
- Mohler ER 3rd, Hiatt WR, Creager MA. Cholesterol reduction with atorvastatin improves walking distance in patients with peripheral arterial disease. Circulation 2003;108:1481-6.
- Bhatt DL, Steg PG, Ohman EM, Hirsch AT, Ikeda Y, Mas JL, et al. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. J Am Med Assn 2006;295:180-9.
- Klein-Weigel PF, Gutsche-Petrak B, Wolbergs S, Koning C, Flessenkamper I. Secondary medical prevention in patients with peripheral arterial disease - prescriptions of vascular surgeons and medical doctors (angiologists) in a multidisciplinary vascular centre. Vasa 2010;39:145-52.
- Ahimastos AA, Walker PJ, Askew C, Leicht A, Pappas E, Blombery P, et al. Effect of ramipril on walking times and quality of life among patients with peripheral artery disease and intermittent claudication: A randomized controlled trial. J Am Med Assn 2013;309:453-60.
- Ostergren J, Sleight P, Dagenais G, Danisa K, Bosch J, Qilong Y, et al. Impact of ramipril in patients with evidence of clinical or subclinical peripheral arterial disease. Eur Heart J 2004;25:17-24.
- Geng DF, Jin DM, Wu W, Liang YD, Wang JF. Angiotensin converting enzyme inhibitors for prevention of new-onset type 2 diabetes mellitus: A meta-analysis of 72,128 patients. Int J Cardiol 2013;167:2605-10.
- Hirsch AT, Duprez D. The potential role of angiotensin-converting enzyme inhibition in peripheral arterial disease. Vasc Med 2003;8:273-8.
- Badger SA, Soong CV, Lee B, Swain GR, McGuigan KE. Prescribing practice of general practitioners in Northern Ireland for peripheral arterial disease. Angiology 2008;59:57-63.
- Al-Omran M, Verma S, Lindsay TF. Suboptimal use of risk reduction therapy in peripheral arterial disease patients at a major teaching hospital. Ann Saudi Med 2011;31:371-5.
- Thompson PD, Zimet R, Forbes WP, Zhang P. Meta-analysis of results from eight randomized, placebo-controlled trials on the effect of cilostazol on patients with intermittent claudication. Am J Cardiol 2002;90:1314-9.
- Rizzo M, Corrado E, Patti AM, Rini GB, Mikhailidis DP. Cilostazol and atherogenicdyslipidemia: A clinically relevant effect? Expert OpinPharmacother 2011;12:647-55.
- Dawson DL, Cutler BS, Hiatt WR, Hobson RW 2nd, Martin JD, Bortey EB, et al. A comparison of cilostazol and pentoxifylline for treating intermittent claudication. Am J Med 2000;109:523-30.