- *Corresponding Author:
- B. Y. Kumar
K L College of Pharmacy, Koneru Lakshmaiah, Education Foundation, Guntur-522 502, India
E-mail: yernikumarb@gmail.com
| Date of Received | 15 December 2020 |
| Date of Revision | 17 January 2021 |
| Date of Acceptance | 15 April 2021 |
| Indian J Pharm Sci 2021;83(3):610-613 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Taking right medicine at the right time is vital to ensure safety and speedy recovery of the patient. The aim of this study was to conduct a comprehensive review systematic analysis and outcomes of the medication discrepancies which occur as a result of inappropriate prescribing in a hospital setting. A cross sectional study was performed between July 2018 to April 2019 at Star hospitals, South India. A total of 300 prescriptions were collected from different inpatient departments by two practising clinical pharmacists. We used the standard World Health Organization methodology to achieve the study objectives. A feasible sampling technique was used to collect the prescriptions from various departments. Various clinical drug databases like Medscape, Micromedex, and Pub Med were referred. A total of 300 prescriptions were collected and reviewed which comprised 62 % Documentation discrepancies, 19.6 % of omission errors, 10.3 % of prescriptions exceeding the maximum dose, 0.8 % were of prescriptions contained therapeutic duplications. Drugs prescribed out of the formulary also contributed to medication related errors. Mid-level health care practioners were also involved on this study. The study evidenced the potential of inappropriate prescription occurring in the hospital setting ranging from patient admission to discharge. Several factors such as multiple co-morbidities, ploy pharmacy, hassle at the work environment and poor communication among allied health care professionals were found to be the major causes of potential inappropriate prescribing. Execution of efficient strategies will help in controlling the harmful outcomes as a result of irrational prescribing.
Keywords
Critical care unit, Emergency ward, Clinical Pharmacist, Prescription auditin, Medication reconciliation, rational therapy.
When patients are getting admitted to hospitals suffering from various co-morbidities, it’s important that the correct medication history is collected and recorded. In the process of collecting medication history after patient admission, various pitfalls were noticed and this is considered as a major cause for the occurrence of hospital prescribing errors. Nothing is done deliberate, so is the act of prescribing. Majority of the current patient population tend to have multiple comorbidities which compels to have multiple cross consultations. In most of corporate health care settings, the patient enrols under the primary physician. The emergency doctor in the Emergency (ER) department will jot down the plan of treatment as per the advice of the primary care physician. Within a time period of one to two h the patient will be shifted to ward or to the critical care unit based on the clinical status of the patient. And here arises the problem of ambiguity because the physician’s treating the patient at Cardiac Care Unit (CCU) is different from the physicians at Electronic Medical record (EMR) ward and primary physician. Unintentionally, during cross consultations the same patient might be prescribed with two same drugs in different brands or two different drugs of the same pharmacological class and this type of drug discrepancies are called therapeutic duplication errors. It’s very important that the medication audit is done at every stage of patient transition in the hospital. Clinical Pharmacists (cp’s) under the supervision of a Clinical Pharmacologist can perform the medication review. Intense review is necessary to analyse, report and correct the discrepancies. To perform the medication review, the cp’s must be equipped with sound and comprehensive knowledge of the pharmacological agents. Our aim is to analyse the number and frequency of prescriptions with inappropriateness and omission of drugs ranging from the patient admission to discharge. The second prime importance is to find out the root cause analysis of these medication discrepancies. This cross sectional study was conducted on a cohort of patients admitted in the King George hospital. It is a super speciality hospital serving huge number of patients since 1845. The study was conducted between July 2018 to April 2019. Two clinical pharmacists’ as a part of their research started collecting prescriptions with poly pharmacy. Before starting the actual work, the clinical pharmacists were trained by a trainer who is holding a PhD degree, an expertise in the field of clinical pharmacology. An ideal tool was designed to document the patient’s provisional diagnosis, past medical history, past medication history, the current medication, its dose, frequency, and route of administration. Also, a special emphasis is given to the columns such as drug interactions, contraindications in the documentation tool. Each patient informed consent was taken before collecting their data. Various drug tools like Micromedex, Medscape were used to analyse different medications in the prescriptions particularly in cases of multiple medications. Overwhelming number of prescriptions from multiple departments was randomly collected and they were segregated based on the patient gender, age group and co-morbidities. Following meticulous data collection, the clinical pharmacists were interviewed to cross check to what extent the procedure is followed in a fair manner. Various medical prescriptions of the age group 35-55 y with chronic conditions such as cardiovascular diseases, hyperlipidaemia, and type 2 diabetes mellitus is Inclusion criteria. Prescriptions of the patients falling in the category of paediatric, geriatric care and inaccessible medical records of ER department patients and prescriptions without drugs are considered as exclusion criteria. A literature was done to obtain criteria. Criteria were validated by a tworound Delphi consensus technique. A Prescription of Chronic kidney disease stage-IV is found to have both calcium acetate (PHOCEL) and sevelamer carbonate (SEVANIX). According to the literature, both the drugs are used to decrease the serum phosphate levels, so there is no rationale in giving both the drugs while one drug is enough to counter the phosphate levels clinically[1,2], The frequency of the medication can be increased to reduce the phosphate levels effectively instead of adding another drug to the patient medication list. A deliberate or an unintentional prescription? This was a case of Post-operative left knee replacement with a pre-existing morbidity of benign prostate hyperplasia. The patient was advised to continue Tamsulosin (VELLTAM) by the primary doctor which was his old medication. The next d the assistant doctor advised Silodosin (SILODAL) without referring the previous drug chart. Unfortunately, the nurse who is partially equipped with the drug knowledge administered both the drugs of pharmacological category which eventually led to a medication error (administration error)[3]. As part of prescription audit, the clinical pharmacist identified this therapeutic duplication and notified to the doctor in team, subsequently resolved. A Case of military tuberculosis (TB) admitted in an inpatient ward was initiated with anti-tubercular treatment (ATT) which includes all the four primary drugs. Prescribing Vitamin B6 is essential to compensate its deficiency on prolonged use of Isoniazid. Unfortunately, Vitamin B6 (pyridoxine) was not added to the treatment regimen which made the patient to complain tingling sensation near the legs which is most commonly described as “pins and needles” feeling.Case of Rheumatoid arthritis was prescribed with methotrexate (FOLITRAX) weekly once for 4 w, but the practitioner did not prescribe folic acid supplement to mask the deficiency of folic acid which results with the prolonged use of methotrexate. This resulted in low haemoglobin.A patient was admitted for a gynaecologic procedure hysterectomy. Postoperatively she was prescribed analgesics Ketorolac and Tramadol three d for the pain management, but the practioner hasn’t added either H2 blockers or Proton pump inhibitors[4]. The role of antiulcer drugs is indispensable in this prescription to curb the gastrointestinal side effects of NSAIDs.
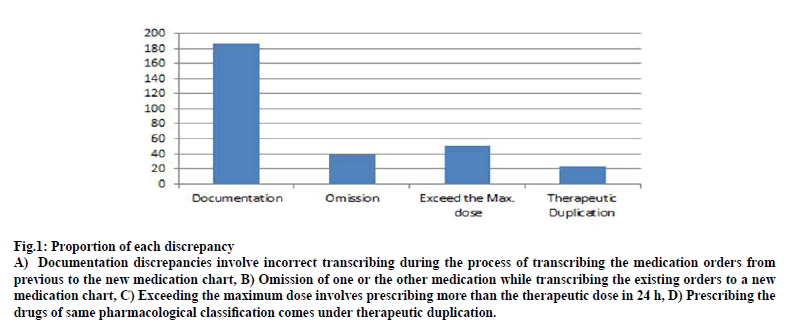
A case of POST coronary artery bypass graft (CABG) re-admitted with chronic cardiac arrhythmias hence treated with amiodarone 150 mg IV bolus there after 900 mg slow/maintenance infusion. The condition of the patient gradually improved, but unfortunately anticoagulant Acenocoumarol was not added in the discharge summary which has a potential to prevent stroke complication in the future because of arrhythmias. Trying to mimic somebody else’s prescription blindly can cause devastating consequences. A case of bilateral pneumonia was prescribed with Moxifloxacin 400 mg twice in a d (BID) by an internal medicine practioner. Assuming that it was the right prescription, a surgical gastroenterologist advised the same drug with same frequency to a different patient which is primarily a prescription error that eventually ended up as an administration error. The rationale prescription would be once a d of Moxifloxacin 400 mg. As a usual practice while majority of the antibiotics prescribed with a frequency BID, a case of complicated respiratory tract infection is also prescribed the same way Levofloxacin 500 mg BID which exceeded the maximal dose for 24 h. The rationale prescription would be once a d of Levofloxacin 750 mg. A microbiological lab report revealed a gram positive infection for which, the patient was prescribed a glycopeptide as Teicoplanin 400 mg BID for 3 d, thereafter 400 mg OD which is a prescription error. Instead, it is correct only when it is prescribed as 400 mg BID for 3 doses thereafter OD as per instructions in the drug leaflet. A case of post-operative orthopaedic procedure was prescribed as Inj. Diclofenac 75 mg TID which is exceeding the maximal dose for 24 h. The maximum dose of Diclofenac sodium for 24 h should not exceed 200 mg. It is a usual practice that we have a couple of registrars in an Intensive care unit. Might be, there is no clear data, but the patient was given intravenous sedatives and anaesthetics in a short period of time by different health care practioners[5],which caused respiratory arrest possibly due to shut down of medulla oblongata. Out of 300 Prescriptions the male patient prescriptions were n=188 (62.6 %) and female were n=112(37.3 %). The Prescriptions were collected, reviewed, compared, and analysed with clinical literature. The distribution of the occurrence of medication discrepancies were described in the fig. 1. Of all the discrepancies found in three hundred prescriptions, incorrect documentation of the medication orders were found to be higher (n=186), the next higher number is omission of the drugs (n=59) while copying the medication orders to the new medication chart. After that, is the prescriptions exceeding the maximum dose (n=31). The lowest number is the prescriptions found with therapeutic duplication (n=24). The number of prescriptions with therapeutic duplication and omission are actually found to be low, but these numbers can remarkably make a big difference in patient recovery. If medications for basic complaints like pain, vitamin supplements are omitted during copying the existing medication orders to the fresh medication chart; it can be acceptable to a certain extent. Whereas even unintentional omission of life saving drug orders is not acceptable as it will not only impede the recovery, in fact sometimes the patient succumbs because he or she will not receive the lifesaving drug. There are multiple reasons for this unintentional omission ranging from distraction to the level of over burden at workplace especially in developing nations and soaring population countries. Well, it takes a lot of effort to bring a drug to the market and the drug development is certainly an arduous process. A drug after crossing through various stages of clinical trials and getting approved by drug regulatory authorities such as food and drug administration (FDA), world health organisation (WHO)[6,7], it will be allowed to be prescribed and dispensed. Ample time and money will be invested in this long process of drug development. In this regard, any medication after making its presence in the pharmaceutical market must be used rationally and never be misutilised. Unfortunately, in the current scenario, drug at the stage of manufacturing or transportation or prescribing or at the stage dispensing it is being misutilised. To ensure that a prescription is rationally and effectively utilised, presence of a clinical pharmacist in a hospital setting, community pharmacist in the community pharmacy setting is really essential and helpful. Clinical Pharmacists monitor the pattern of drug use and if any medication discrepancy is found, they will notify to the Clinical Pharmacologist[8]. With the report in hand, they will take a step forward and guide all the health professionals in a proper way ensuring safe prescribing and correct drug administration procedures. However, efficient training and assessment is necessary to reduce the inappropriateness in the prescriptions. It is clearly understood that corrective and preventive action is imperative for any medication discrepancy which occurs. This way the quality of patient care services can be improved. Another important tool which has to be given great significance is flawless communication among the health care professionals. In patient prescription audit is a prominent strategy which can be executed to curb the number of medication errors and this can be done independently or together as a team of heath care professionals that comprise a physician, clinical pharmacist, a nurse and a dietician. Because of intense pressure in the process of handling many patients and document their clinical status, duty medical officers unintentionally skip the medication orders while transcribing from one sheet to another[9-11]. It is the responsibility of a clinical pharmacist to observe such deviations and notify the resident doctors that it needs be corrected. Another source of medication discrepancy is medication reconciliation. This includes taking appropriate medication history from the patient if he or she is conscious and coherent. Either from the patient attender or an old prescription, the detailed medication history must be taken. In some circumstances such as overflow of patients to the ER ward and patients not bringing the old medication list, the emergency residents fail to document the co-morbidities and correct medication history of the patient and shift the patient to intensive care unit or a ward as such with an incomplete medication order in the drug chart. In this scenario, prescription audit by cp has the potential to ensure that patients also receive the home medications for chronic diseases. A detailed and over all medication review of the patient will be done, this way a pharmacist act as a crucial member of the multidisciplinary team. Incorporating cp’s in the hospitals[12], brings many benefits, so it is high time that medical fraternity gives significance to a clinical pharmacist and physicians try adopting them. Burgeoning number of patients with multiple co-morbidities and rising number of prescriptions are prominent causes for the overburden of health care practioners. Stress, anxiety as a result of working overtime might be another cause for increasing number of medication errors. The figure of people opting the profession of health care services has to rise enormously so that the quality of patient care improves significantly. Clinical Pharmacy is recently incorporated into the Indian healthcare sector where clinical pharmacists need to work with a motto to improve the quality of care through monitoring of medication administration monitoring, resolving the drug related queries, educating the allied health professionals and more importantly through prescription audit.
Figure 1: Proportion of each discrepancy
A) Documentation discrepancies involve incorrect transcribing during the process of transcribing the medication orders from previous to the new medication chart, B) Omission of one or the other medication while transcribing the existing orders to a new medication chart, C) Exceeding the maximum dose involves prescribing more than the therapeutic dose in 24 h, D) Prescribing the drugs of same pharmacological classification comes under therapeutic duplication
References
- Kuyvenhoven MM, De Melker RA, van der Velden K. Prescription of antibiotics and prescribers? characteristics. A study into prescribing antibiotics in upper respiratory tract infections in general practice. Fam Pract 1993;10(4):266-370.
- Prescribing behaviour in clinical practice: patients expectations and doctors perceptions of patients expectations a questionnaire study. BMJ 1997;315(7107):520-3.
- Rognstad S, Brekke M, Fetveit A, Spigset O, Wyller TB, Straand J. The Norwegian General Practice (NORGEP) criteria for assessing potentially inappropriate prescriptions to elderly patients: A modified Delphi study. Scand J Prim Health Care 2009;27(3):153-9.
- Nyborg G, Straand J, Brekke M. Inappropriate prescribing for the elderly-a modern epidemic. Eur J Clin Pharmacol 2012;68(7):1085-94.
- Weng M, Tsai C, Sheu K, Lee Y, Lee H, Tzeng S, et al. The impact of number of drugs prescribed on the risk of potentially inappropriate medication among outpatient older adults with chronic diseases. QJM 2013;106(11):1009-15.
- Motter FR, Fritzen JS, Hilmer SN, Paniz É, Paniz VM. Potentially inappropriate medication in the elderly: a systematic review of validated explicit criteria. Eur J Clin Pharmacol 2018;74(6):679-700.
- Terrell KM, Perkins AJ, Dexter PR, Hui SL, Callahan CM, Miller DK. Computerized decision support to reduce potentially inappropriate prescribing to older emergency department patients: a randomized, controlled trial. J Am Geriatr Soc 2009;57(8):1388-94.
- Loganathan M, Singh S, Franklin BD, Bottle A, Majeed A. Interventions to optimise prescribing in care homes: systematic review. Age Ageing 2011;40(2):150-62.
- Cooper JA, Cadogan CA, Patterson SM, Kerse N, Bradley MC, Ryan C, et al. Interventions to improve the appropriate use of polypharmacy in older people: a Cochrane systematic review. BMJ Open 2015;5:e009235
- Furniss L, Burns A, Craig SK, Scobie S, Cooke J, Faragher B. Effects of a pharmacist's medication review in nursing homes: randomised controlled trial. 2000;176(6):563-7.
- Abramson EL, Bates DW, Jenter C, Volk LA, Barron Y, Quaresimo J, et al. Ambulatory prescribing errors among community-based providers in two states. J Am Med Inform Assoc 2012;19(4):644-8.
- Roberts MS, Stokes JA. Prescriptions, practitioners and pharmacists. Med J Aust 1998;168(7):317-8.