- *Corresponding Author:
- R. C. Doijad
Department Of Pharmaceutics, K.L.E.S’s College of Pharmacy, Belgaum - 590 010, India.
E-mail: rcdoijad1@rediffmail.com
| Date of Submission | 10 March 2006 |
| Date of Decision | 21 September 2006 |
| Date of Acceptance | 22 April 2007 |
| Indian J Pharm Sci, 2007, 69 (2): 323-326 |
Abstract
Influence of processing variables on the solid-state of a model drug, piroxicam in cyclodextrin-based system and its effect on dissolution behavior of the drug was investigated in the present study. Binary systems containing piroxicam and hydroxypropyl-β -cyclodextrin prepared by various processes, were characterized by FTIR, thermal stability, photo stability and dissolution studies. Hydroxypropyl-β -cyclodextrin enhanced the solubility of piroxicam and increased dissolution rates from the binary systems. The complex prepared by co-evaporation method was found to yield better dissolution rate and stability as characterized in present study over those of the complex prepared by other methods.
Various techniques of preparation of cyclodextrin complexes i.e. co-precipitation, slurry, paste and dry mixing methods, have been utilized [1]. During any process of preparation of inclusion complex, the formation of complex depends on various factors like interaction of drug with cyclodextrin and solvents utilized. These would include: the strength of the complex formed (association constant); the extent of interaction between the drug and the cyclodextrin during the process; the use of solvents during the process and their type; the solubility of the drug and the cyclodextrin in the solvent system used; and the duration of processing.
In most cases, the drug would not only exist within the cavity of the cyclodextrin but also between the cyclodextrin rings. In the case of crystalline complexes of β-cyclodextrin, these can be termed as ‘crystal lattice inclusion complexes’ [2]. For amorphous cyclodextrins such as hydroxypropyl-β-cyclodextrin (HP-β-CD), the drug would be dispersed in the cyclodextrin matrix and not necessarily within the cyclodextrin cavity. The drug need not be molecularly dispersed in the carrier and may be present in a crystalline or amorphous form within the matrix. These systems can therefore be appropriately termed as ‘solid dispersions’. The solid-state characteristics of the drug after preparation and during storage will depend on the processing variables characteristics of the system. When the objective of the formulation is to attain faster dissolution rates, presence of amorphous or disordered forms of the drug would be favorable. The higher apparent solubility of the drug and the improved dissolution rate would therefore be a result of presence of amorphous high energy forms of the drug as well as the ability of the cyclodextrin to form a soluble complex with the drug. The performance of the product over the shelf life would depend on the ability of the cyclodextrin to prevent crystallization of the amorphous drug to its stable crystalline form. The method of preparation of these systems would influence the final solid state of the drug and would therefore be a vital determinant of the performance of the system. The primary objective of the study was to investigate and demonstrate the influence of processing variables on the formation of complex of a model drug, piroxicam, in binary systems with HP-β-CD and to correlate it with in vitro dissolution performance and stability.
Piroxicam (PX) is a non-steroidal antiinflammatory drug with poor water solubility [3]. It is a weakly acidic drug possessing very low aqueous solubility. This results in slower dissolution and absorption rates on oral administration and is one of the causes of gastrointestinal side effects. Improvement in drug solubility expected to enhance its bioavailability and reduce local side effects. HP-β-CD has been reported to form a complex with, and improve solubility of PX [4]. PX was therefore chosen as a model drug to study the influence of processing variables on the solid-state characteristics of the drug in HP-β-CD based systems.
PX was obtained as a gift sample from SUN Pharmaceuticals Ltd, Mumbai. Hydroxypropyl-β- cyclodextrin was obtained as a gift sample from Dr.Reddy’s Laboratory, Hyderabad. All other reagents and solvents were of analytical grade and were used as such.
Phase solubility studies were performed by the method of Higuchi and Connors. Briefly, excess amounts of PX (0.05 g) were added to 20 ml of aqueous solutions containing various concentrations of HP-β-CD (1 × 10-2 to 4 × 10-2 M). The suspensions were vigorously shaken at 100 rpm and 25±1o for 3 d. After equilibrium was attained, the samples were filtered through a 0.45 μm Millipore membrane filter and suitably diluted with 0.01 M hydrochloric acid in methanol. PX concentration was determined spectrophotometrically at 242 nm. The apparent 1:1 stability constant, Ks, was calculated from the phase solubility diagrams using the equation, Ks= slope/ So (1 - slope, where So is PX solubility in the absence of HP-β-CD (intercept). The infrared spectra of complexes were recorded on a FTIR Impact-410 Nicolet, USA using KBr pellet method.
Binary system containing PX and HP-β-CD were prepared in a 1:1 molar ratio by various techniques. The codes used for the resulting systems are given in parentheses. A mixture of PX with HP-β-CD equivalent to 500 mg of PX, was kneaded with 1 ml of 50% aqueous ethanol, in a glass mortar. The mass was then dried in a tray dryer at a temperature not exceeding 50o. The dried mass was then stored overnight in a vacuum desiccator.
A mixture of PX with HP-β-CD equivalent to 500 mg of PX was kneaded with a mixture of 1 ml of water and 0.2 ml of 25% ammonia solution. The mass was processed in a manner similar to KNE. PX and HP-β-CD were passed through sieve no-85 and ground thoroughly in a mortar to a homogeneous mixture. The mixture was passed through a sieve no-85 and stored over phosphorous-pentoxide (RH~0%). This system was prepared as a control, to determine the effect of HP-β CD without the aid of any solvent. The improved dissolution behavior of this system was expected to be predominantly by in situ complexation of the drug with HP-β-CD, in the dissolution medium.
Equal molar ratio of HP-β-CD was dissolved in 10 ml water and this solution was added to 10 ml ethanol containing 500 mg PX. The mixture was stirred with heating at a temperature below 50o. The clear solution obtained was further heated below 500 with stirring, till a pasty mass was obtained. The residual solvent was removed under vacuum at room temperature in a Delvac freeze dryer.
Solid dispersions were prepared by this method using two different techniques. Addition of 10 ml of an equal molar ratio aqueous HP-β-CD to 10 ml of 25% ammonia solution in which 500 mg of piroxicam was dissolved to obtain a clear solution. In this method, 0.2 ml of 25% ammonia solution was added to 10 ml of equal molar ratio aqueous HP-β-CD solution in which PX was dispersed. Both the techniques led to formation of clear solutions, which were then treated in a fashion similar to the mixture obtained during the preparation of co-evaporation from aqueous ethanol.
An equimolar ratio mixture (5 g) of HP-β-CD and PX was shaken for 24 h with 40 ml water. Ammonia solution (25% v/v) was added to it drop wise till a clear solution was obtained. The volume was then made up to 50 ml with water. The solution was frozen overnight in Petri dishes at -40o and lyophilized in a Delvac freeze dryer at -40o for 48 h. Secondary drying was carried out at room temperature.
The formulation equivalent to 20 mg of PX was taken for dissolution study in 900 ml of pH 7.2 phosphate buffer in USP XXIII dissolution apparatus (Electrolab, Mumbai), maintained at 50 revolutions per min at 37±2o. Aliquots of the dissolution media were withdrawn at various time intervals and were replaced with equal volume of the same media. The samples were analyzed at 256 nm for the drug contents using spectrophotometrically UV 1201 Shimadzu, Japan.
The samples were stored in sealed containers at various temperature conditions such as room temperature, 37, 45, and 60o for a period of 12 w and the samples were withdrawn at weekly intervals for the estimation of the drug content. The samples were also stored in transparent glass containers and exposed to direct sunlight at the rate of 6 days per week for a period of 12 w and sampling was done similar to that of the thermal stability studies.
The shape of the solubility diagram followed an AL type system (Higuchi and Connors, 1965). Freeze drying of solubilized PX in cyclodextrin solution yielded a solid amorphous product. Further evidence of the complex formation was obtained by FTIR spectroscopy.
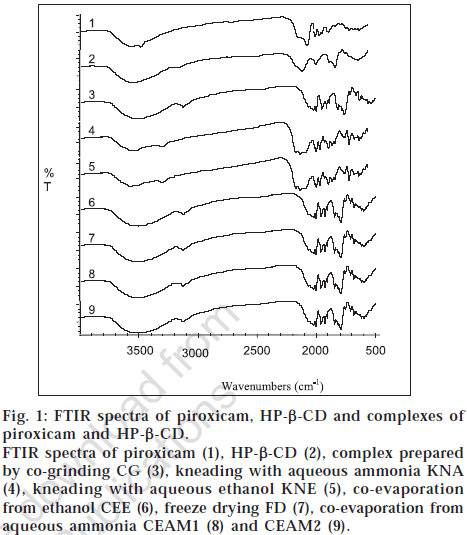
FTIR spectra are presented in fig. 1. PX spectra showed the band at 3330 cm-1. PX exists in two different interconvertable crystal polymorphs [5]. Their IR spectra differ only slightly in the finger print region, but the bands of -NH and -OH stretching lie at 3330 cm-1 in the cubic form. Additional characterization with 1H NMR spectroscopy would be necessary to conclude that hydrogen bonds are formed.
Fig. 1: FTIR spectra of piroxicam, HP-β-CD and complexes of piroxicam and HP-β-CD. FTIR spectra of piroxicam (1), HP-β-CD (2), complex prepared by co-grinding CG (3), kneading with aqueous ammonia KNA (4), kneading with aqueous ethanol KNE (5), co-evaporation from ethanol CEE (6), freeze drying FD (7), co-evaporation from aqueous ammonia CEAM1 (8) and CEAM2 (9).
The dissolution studies Table 1 revealed that all the formulations showed an increased rate of dissolution. The techniques of preparation of the complex prepared were found to have an influence on the dissolution rate. The complex prepared by co-evaporation from aqueous ammonia (CEA) method was found to yield higher rate of dissolution over other methods. The complexes prepared by various techniques were found to exhibit a better stability over the pure drug at all storage conditions as well as when exposed to sunlight, values are shown in the Table 2.
| Time (in min) | Cumulative % drug release | |||||||
|---|---|---|---|---|---|---|---|---|
| Piroxicam pure drug | CG | CEAM2 | CEE | CEAM1 | FD | KNA | KNE | |
| 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 15 | 2.5 | 22 | 85.34 | 18.1 | 90.7 | 85.1 | 74.23 | 66 |
| 30 | 6.2 | 27.1 | 85.99 | 20.36 | 92.8 | 87.2 | 74.99 | 66.89 |
| 45 | 8.6 | 30.7 | 86.89 | 22.17 | 92.8 | 90.7 | 74.7 | 67.81 |
| 60 | 11.1 | 33.9 | 87.7 | 36.2 | 94.2 | 89.3 | 76.99 | 68.23 |
| 75 | 14.8 | 42 | 88 | 41 | 94.2 | 89.3 | 77.23 | 69.11 |
| 90 | 17.8 | 45.6 | 88.69 | 43.44 | 94.9 | 92 | 78.45 | 69.99 |
| 105 | 20 | 50.8 | 90.12 | 50.68 | 96 | 92.8 | 79 | 70.4 |
| 120 | 22.8 | 56.7 | 90.23 | 51.58 | 97 | 93.5 | 80.33 | 71.33 |
| 135 | 25.2 | 58.2 | 90.45 | 52.94 | 97 | 93.5 | 81.67 | 72 |
| 150 | 28 | 58.2 | 91.1 | 53.39 | 97 | 93.91 | 83.03 | 72.48 |
| 165 | 29.5 | 61.8 | 92 | 54.3 | 97.7 | 94.1 | 83.44 | 73.22 |
| 180 | 30.2 | 66.3 | 93.99 | 55.1 | 98.4 | 94.69 | 84 | 73.77 |
| 195 | 33.927 | 68.5 | 94.51 | 56.11 | 99.1 | 94.98 | 85.55 | 74.39 |
| 210 | 35.1 | 73.6 | 95 | 57.0195 | 99.1 | 95.45 | 86.11 | 74.23 |
| 225 | 35.29 | 78.8 | 95.74 | 57.0195 | 99.6 | 95.99 | 86.44 | 74.91 |
Dissolution profile of piroxicam pure drug (-♦-) and cyclodextrin complexes prepared by co-grinding CG (-▇-), co-evaporation from aqueous ammonia CEAM2(-▇-), co-evaporation from ethanol CEE (-×-), CEAM1(-▇-), freeze drying FD(-●-), kneading with aqueous ammonia KNA(-▲-), kneading with aqueous ethanol KNE(-▫-) methods at ph 7.2.
Table 1: Dissolution profiles of Piroxicam and Piroxicam Cyclodextrin complexes
| BatchCode | Room temperature | 37 ±1° | 45 ±1° | 60 ±1° | Direct sunlight exposure |
|---|---|---|---|---|---|
| Pure drug (10-2) | 1.02±0.43 | 1.34±0.42 | 1.52±0.12 | 1.59±0.70 | 4.88±0.70 |
| CG (10-3) | 1.32±0.20 | 1.51±0.46 | 2.10±0.12 | 2.07±0.98 | 6.20±0.93 |
| KNE (10-3) | 0.72±0.10 | 0.86±0.20 | 0.98±0.22 | 1.08±0.34 | 4.24±0.98 |
| CEE (10-3) | 0.69±0.04 | 0.83±0.12 | 0.94±0.24 | 1.12±0.32 | 4.32±0.89 |
| KNA (10-3) | 0.61±0.14 | 0.65±0.10 | 0.74±0.24 | 0.80±0.12 | 3.45±0.65 |
| FD (10-3) | 0.58±0.14 | 0.62±0.12 | 0.69±0.41 | 0.76±0.33 | 3.22±0.87 |
| CEAM2 (10-3) | 0.54±0.12 | 0.60±0.51 | 0.68±0.24 | 0.70±0.55 | 3.15±0.65 |
| CEAM1 (10-3) | 0.53±0.23 | 0.59±0.13 | 0.68±0.11 | 0.69±0.13 | 3.01±0.58 |
Values are mean±SD for n=3, Stability study period is 3 months
Table 2: First Order Degradation Rate Constant (K) of Complexes Prepared by Various Methods Subjected to Stability Studies
References
- Hedges, A.R., Chem. Rev., 1998, 98. 2035. Back to cited text no. 1
- Pitha, J., Szente, L. and Szejtli, J., In; Bruck, S.D., Controlled Drug Delivery, Vol. I. CRC Press, Florida, 1983, 125. Back to cited text no. 2
- Wenz, G., Clin. Drug Invest., 2000, 19, 21. Back to cited text no. 3
- Mario, J., and Mira, B., Eur. J. Pharm. Sci., 2004, 21, 251. Back to cited text no. 4
- Mihalic, M., Hofman, H., Kuftinec, J., Krile, B., Caplar, V., and Kajfez, F., In; Florey, K., Analytical Profiles of Drug Substances, Vol. 15. Harcourt Brace Jovanvich Publishers, 509.