- *Corresponding Author:
- Y. Lin
Department of Neurosurgery,
Jinling Hospital, School of Medicine,
Nanjing University,
Nanjing,
Jiangsu 210002,
China
E-mail: linyixing001@163.com
| This article was originally published in a special issue, “New Advancements in Biomedical and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2022:84(2)Spl Issue “8-15” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the effect of myelotomy on limb function preservation in patients with complete paralysis after cervical spine injury. A total of 80 patients with complete paralysis due to cervical spine injury were selected in our hospital from June 2019 to March 2021. According to the surgical methods, they were divided into two groups. Group A was treated with myelotomy. Group B received dural incision and the treatment results and related indicators of the above two groups were compared. Postoperative drainage volume in group A was significantly lower than that in group B. The visual analogue score and cervical dysfunction index in group B were significantly higher than that in group A and the American Spinal Injury Association sensory and motor function scores and Fugl-Meyer scale scores increased significantly between the two groups 2 w after surgery, 1 y after surgery and the last follow-up. In addition, American Spinal Injury Association sensory and motor function scores and Fugl-Meyer scale scores in group A were significantly higher than those in group B. For patients with complete paralysis of cervical spine injury, myelotomy can achieve better recovery of neurological function and lower pain sensation and can improve the patient’s motor, sensory and limb functions, with less complications and higher safety.
Keywords
Myelotomy, durotomy, cervical spine, paralysis
At present, with the rapid development of construction industry and traffic, cervical trauma and other accidents emerge in an endless stream. There are spinal nerves walking in the human cervical spine and its nerve branches control the sensation and movement of joints and muscles in the whole body, so it also leads to injuries outside the cervical spine that often accompany spinal cord injury. However, spinal cord injury has a high disability rate and the mortality rate is increasing year by year and the medical expenses of patients are extremely high. According to the study results of Rouanet et al., approximately 1.3 million North Americans have suffered spinal cord injury after cervical trauma in general [1]. After spinal cord injury, most cases can appear widely edema of spinal cord and the intramedullary hematoma, enormous influence upon the patient’s vital signs, such as edema, spread to the Cavernous (C4) segment above can lead to respiratory depression, extensive edema further spread of cervical vertebra tube obstruction, cause spinal cord ischemia and necrosis, further lead to damage of spinal cord [2]. At present, many scholars have carried out related studies on the treatment of spinal cord injury. The main purpose of early treatment for cervical spinal cord injury is to decompress and reduce and it is generally believed that early surgical surgery is needed for treatment, and there are a variety of surgical methods. Previous conventional laminar decompression can relieve the epidural pressure to a certain extent, but it cannot relieve the subdural pressure [3]. A number of studies have shown that dural decompression can reduce the pressure in the spinal cord, improve the spinal blood perfusion, reduce secondary injury and promote the recovery of neurological function [4]. Myelotomy has been used in the treatment of spinal cord injury for over a century and a large number of research results have confirmed the effectiveness of the treatment of spinal cord injury [5]. However, there are very few studies on the treatment of spinal cord injury by these two methods in China and there is no relevant study on limb function preservation in patients with complete paralysis. Therefore, the purpose of this study is to explore the effectiveness of the two surgical methods in retaining limb function of injured segments, in order to provide theoretical basis for relevant clinical studies. The results are as follows.
Materials and Methods
General information:
80 patients with complete paralysis due to cervical spine injury admitted to our hospital from June 2019 to March 2021 were selected as the research subjects. According to the surgical methods, they were divided into two groups (40 cases in each group). Group A was the group who underwent myelotomy; group B was the group receiving dural incision, and the treatment results and related indicators of the above two groups were compared to explore the effect of myelotomy on preserving limb function of injured segments in patients with complete paralysis.
Inclusion and exclusion criteria:
Inclusion criteria: Age ≥18 y old; combined with comprehensive symptoms, signs and relevant imaging examinations, the patient was diagnosed as complete paralysis due to cervical spine injury and had surgical indications; all patients had extensive spinal edema or intramedullary hematoma; all patients and their family members gave informed consent to this study and signed informed consent.
Exclusion criteria: Complicated craniocerebral injury and other multiple injuries in the body; patients with heart, liver, kidney and other organ dysfunction or malignant tumor; malignant infection; incomplete clinical data; people with mental disorders, speech disorders and inability to communicate normally.
Surgical methods:
First, patients in the two groups were subjected to general anesthesia, prone lying and disinfected. Neuroelectrophysiological monitor was used to detect the function of the patients near the spinal cord and X-ray machine was used to locate the diseased spinal segment. A longitudinal incision was made with the posterior medial incision to dissect the muscles on both sides of the subperiosteum spinous process to expose the disordered segment. Then dissection and epidural spinal cord dissection were used respectively to give edema in patients with segmental decompression. First of all, A group of patients based on preoperative imaging detection of wiring harness, intramedullary spinal cord lesion segments help determine surgical site location and then in intraoperative spinal cord defects existed in the surface observation and then determine the hematoma parts under the premise of choice without spinal cord blood vessels for longitudinally. The incision length was 5 to 10 mm and the depth reached the site of hematoma or necrotic lesion, then the internal hematoma and necrotic tissue were cleaned with 37° saline. And group B patients is to found the edema of segmental 37° saline soak, then apply surgical microscope to injury and edema segmental range previously opened longitudinally, release the cerebrospinal fluid, observation of patients with respiratory indications, then the subdural hematoma, broken bone, such as to clean up and then disappear for Magnetic Resonance Imaging (MRI) showed high signal of cerebrospinal fluid segmental dentate ligament giving parts cut, until the signal fluctuation returns to normal. After the above two procedures were completed, an artificial dural repair was performed, i.e., dilated dural plasty, with the protection of an antiadhesion membrane and sponge. Then, bone fusion was performed using artificial bone or autogenous bone graft and the tissue was sutured layer by layer after placing a drainage tube, internal fixation and the incision was closed. After the operation, appropriate internal fixation instruments were given, followed by routine application of dehydrating drugs, techniques and gastric mucosal protectant, antibiotics to prevent infection, intensive nursing and placement of bedsores and thrombosis.
Observation indicators:
The general clinical data of the two groups were collected, including age, gender, etiology, etc. The operative clinical indicators, including intraoperative blood loss, operative time and postoperative drainage volume, were collected in the two groups. Visual Analogue Score (VAS) was used to evaluate patients’ pain, mainly to record neck and shoulder pain before surgery, 2 w after surgery, 1 y after surgery and at the last follow-up. VAS score was mainly used to evaluate patients’ pain, with 10 points indicating severe pain, 0 points indicating no pain and 0-10 points indicating different degrees of pain [6]. For patients with preoperative and postoperative 2 w, after 1 y and at the time of the last follow-up in patients with cervical dysfunction index, mainly evaluate cervical dysfunction in patients with neck pain, personal care, lift weights, reading, headache, concentration, work and entertainment, sleep, driving the influence degree of the ten aspects, with 0~5 points, to evaluate from light to heavy. The total score ranges from 0 to 50 and the higher the score, the greater the influence [7]. American Spinal Injury Association (AISA) motor machine sensory function assessment, the preoperative and postoperative patients with 2 w, after 1 y and at the end of the follow-up rate of spinal cord function, including AISA sports scores, which is to examine the patients from top to bottom, tested for 20 muscles on both sides of the body, the strength is divided into 0~5 points, where 0 points is complete paralysis; 1 point is palpable muscle contraction; 2 point can actively move the joint, but it cannot resist gravity; 3 point can resist gravity and carry out full joint active movement; 4 point is anti-resistance full joint active movement and a score of 5 is completely normal. After sensory function score, it is divided into 0 points, that is sensory deficiency; 1 was sensory impairment; 2 is the whole body was divided into 28 detection points to detect acupuncture and light touch [8]. Limb function was evaluated by Fugl-Meyer scale before surgery, 2 w after surgery, 1 y after surgery and the last follow-up of patients in both groups. It mainly observed whether reflex activities could be induced in the upper arm, palm, shoulder and lower limb of patients, divided into upper arm and lower limb, with a total score of 100 and the lower the score, the more serious the movement disorders were [9]. Complications in the two groups were statistically analyzed.
Statistical methods:
Statistical Package for the Social Sciences (SPSS) 20.0 was used for statistical analysis. Comparison of measurement data between the two groups was expressed by mean±standard deviation and t test was used. Counting data between the two groups were compared in terms of number of cases or percentage and the chi-square test was used. p<0.05 was considered to be statistically significant.
Results and Discussion
There was no statistical significance between the two groups in age, gender and cause of disease (p>0.05), and the two groups were comparable as shown in Table 1.
| Gender | Group A (n=40) | Group B (n=40) | Statistics | p value | |
|---|---|---|---|---|---|
| Age | 38.45±12.23 | 39.27±11.19 | 0.314 | 5.314 | |
| Gender | Male | 23 | 24 | 0.119 | 6.137 |
| Female | 17 | 16 | 4.225 | ||
| Causes | Falling | 19 | 22 | 0.428 | |
| Traffic accident | 16 | 11 | |||
| Others | 5 | 7 |
Table 1: Analysis of General Clinical Data
The results showed that there was no significant difference in the amount of intraoperative blood loss and operation time between the two groups (p>0.05). However, postoperative drainage volume in group A was significantly lower than that in group B and the difference was statistically significant (p<0.05), as shown in Table 2.
| Group | Group A (n=40) | Group B (n=40) | T value | p value |
|---|---|---|---|---|
| Intraoperative blood loss | 313.24±52.36 | 328.15±41.32 | 0.546 | 0.527 |
| Postoperative drainage | 371.2±119.6 | 415.3±156.3 | 5.312 | 0.013 |
| Operation time | 3.25±0.85 | 3.46±0.59 | 0.314 | 0.849 |
Table 2: Analysis of Surgical Clinical Indexes
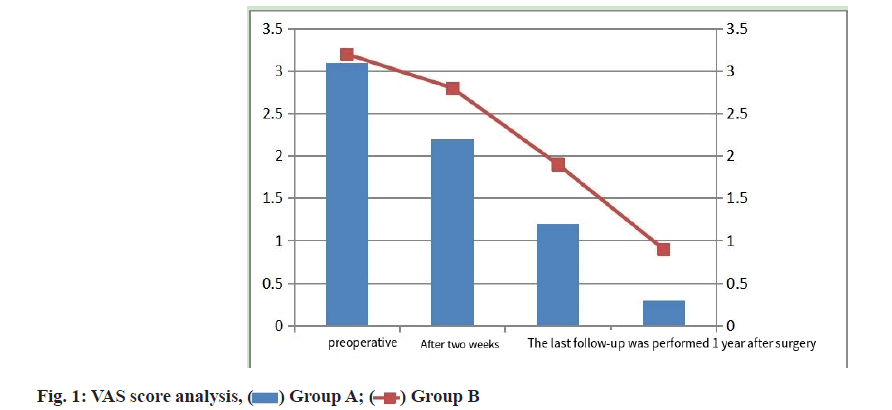
Results showed that there was no statistically significant difference in preoperative pain scores between the two groups (p>0.05), but VAS scores of group B were significantly higher than that of group A at 2 w, 1 y and the last follow-up, the difference was statistically significant (p<0.05), as shown in fig. 1.
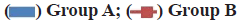
Results two groups of patients with preoperative said there was no statistically significant difference in the cervical dysfunction index (p>0.05), but at the end of 2 w after surgery and 1 y follow-up sessions, two groups of cervical dysfunction index was significantly decreased, and the cervical dysfunction index of group B were significantly higher than that of group A, statistically significant difference (p<0.05), as shown in fig. 2.
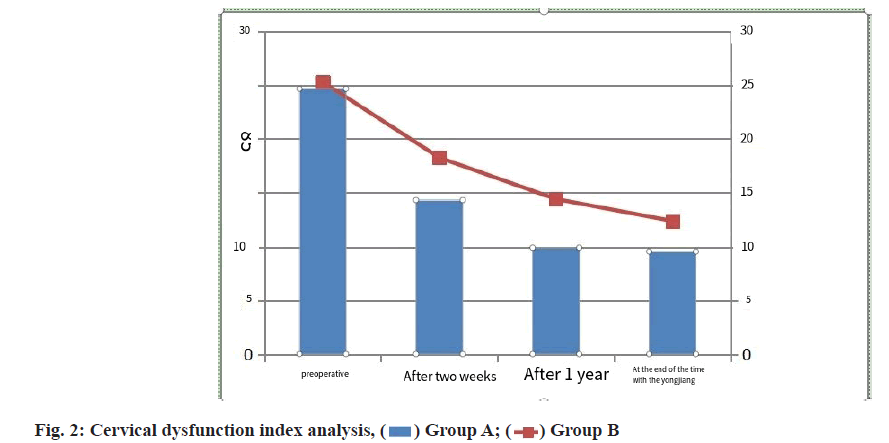
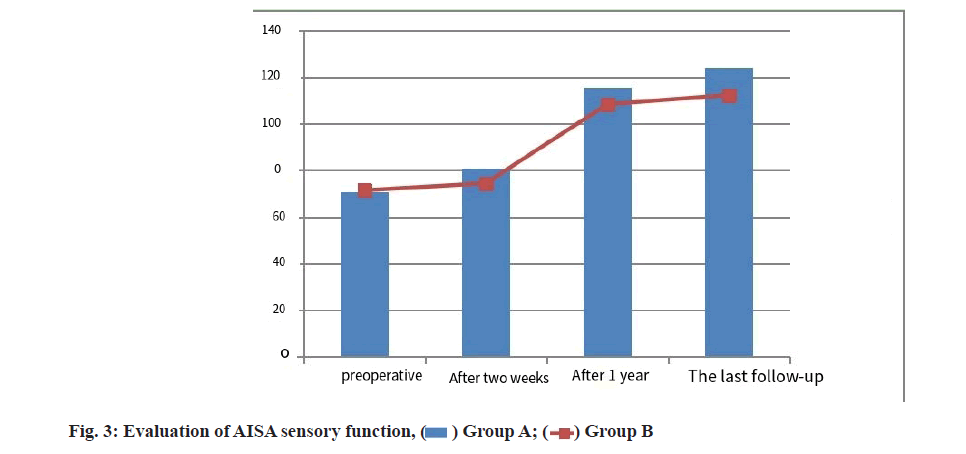
The results showed that there was no statistically significant difference in AISA sensory function scores between the two groups before surgery (p>0.05), but the AISA sensory function scores of the two groups were significantly increased 2 w after surgery, 1 y after surgery and the last follow-up, and the AISA sensory function scores of the group A were significantly higher than that of the group B, the difference was statistically significant (p<0.05). As shown in fig. 3.
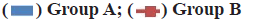
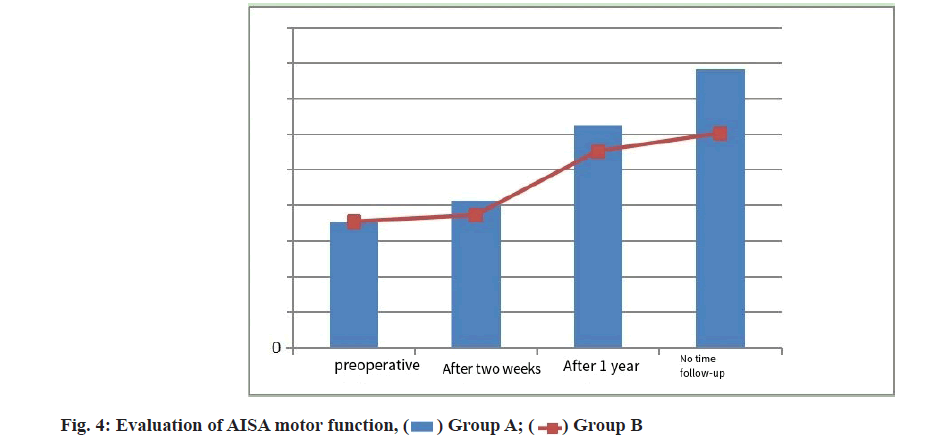
The results showed that there was no statistically significant difference in the AISA motor function score between the two groups before surgery (p>0.05), but the AISA motor function score of the two groups increased significantly 2 w after surgery, 1 y after surgery and the last follow-up and the AISA motor function score of the group A was significantly higher than that of the group B, the difference was statistically significant (p<0.05). As shown in fig. 4.
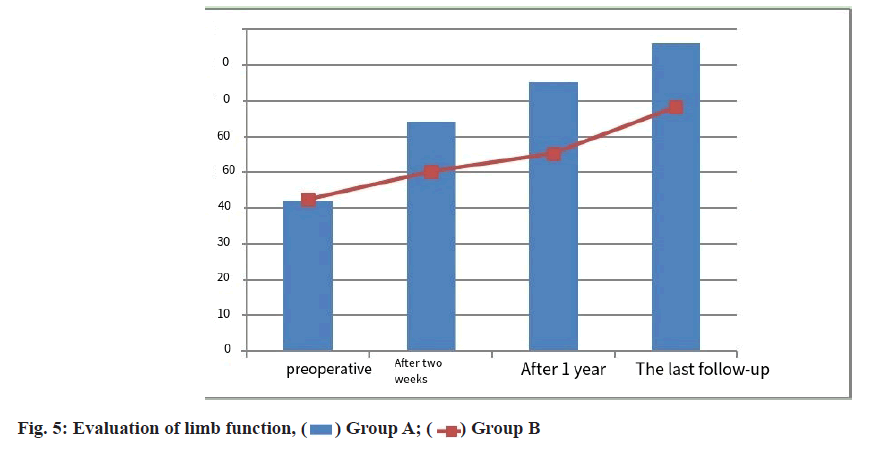
The results showed that there was no statistically significant difference in Fugl-Meyer scale scores between the two groups before surgery (p>0.05), but the Fugl-Meyer scale scores of the two groups increased significantly 2 w after surgery, 1 y after surgery and the last follow-up, and the Fugl-Meyer scale scores of the group A were significantly higher than that of the group B. The difference was statistically significant (p<0.05), as shown in fig. 5.
There was no statistical significance in the incidence of postoperative complications between the two groups (p>0.05), as shown in Table 3
.| Group | Group A (n=40) | Group B (n=40) | χ2 value | p value |
|---|---|---|---|---|
| Lung infection | 15 | 17 | 0.432 | 0.078 |
| Thrombosis of deep vein of lower extremities | 2 | 1 | 0.539 | 0.145 |
| Radicular paralysis | 3 | 2 | 0.112 | 0.267 |
| Incision infection | 2 | 1 | 0.024 | 0.314 |
Table 3: Postoperative Complications Analysis
Clinically, cervical spinal cord injury often occurs in traffic accidents, injuries, high falls and sports injuries, etc. Currently, it has a high incidence and disability rate in the whole world. Traumatic spinal cord injury mainly includes mechanical injury caused by external forces and secondary cell injury caused by the progression of the disease, both of which jointly lead to the destruction of the patient’s nervous tissue [10]. The spinal cord is a part of the human central nervous system, which connects the medulla oblongata in the spinal canal and the two sides of the medulla oblongata connect the limbs. Therefore, it also leads to the occurrence of cervical spinal cord injury, which often leads to complete paralysis [11]. The occurrence of the above mechanical injury is irreversible and the pathologic and molecular cascades caused by it are conducive to the change of secondary injury. Secondary injury is an active regulation process at the cellular and molecular level, which is reversible and controllable. According to relevant research results, the damage caused by secondary injury is much higher than that caused by primary injury, so the removal of necrotic spinal cord tissue is of great significance for the survival of residual spinal cord tissue [12]. In the course of clinical treatment, the choice of surgical methods and surgical timing will have an important impact on the clinical treatment. Studies have shown that surgical treatment given 8 h after injury has a better effect on neurological function recovery or life saving than treatment given 2 d after injury and has been widely recognized in surgery [13]. And the treatment of surgical decompression operation method is more, such as laminectomy, hard membrane dissection and spinal cord dissection, at the same time also exist different opinions on the road way, at present in the relevant domestic research results into the road way is more, the effect of different surgical treatment is less, so the purpose of this study to research, combining the above results are discussed below.
First, the results of this study showed that there were no statistically significant differences in preoperative pain scores and cervical dysfunction index between the two groups. However, at postoperative 2 w, 1 y and the last follow-up, VAS score and cervical dysfunction index in group B were significantly higher than those in group A and the differences were statistically significant. At present, there are no comparative studies on VAS and cervical dysfunction in myelotomy and dural surgery at home and abroad, so the study results cannot be demonstrated. However, the results of this study speculated that the VAS score might be related to the incision exposure and muscle dissection. However, the two surgical methods were consistent in this way and it was speculated that it might be related to the individual patient, sample size and the occurrence of complications. The specific reasons still need to be studied. Cervical dysfunction index may be related to recovery of motor, sensory and limb functions for reasons described below.
Secondly, the results of this study indicated that there were no statistically significant differences between the two groups in preoperative AISA sensory and motor function scores and Fugl-Meyer scale scores. However, at 2 w, 1 y and the last follow-up, AISA sensory and motor function scores and Fugl-Meyer scale scores in the two groups increased significantly and the AISA sensory and motor function scores and Fugl-Meyer scale scores in the group A were significantly higher than those in the group B and the differences were statistically significant. Compared with dural surgery, myelotomy is more effective in repairing limb function, motor function and sensory function in patients with complete paralysis with cervical spine injury. Telemacque et al. [14] reported that epidural surgery is more frequently performed than myelotomy and that epidural surgery may be safer and more effective than myelotomy. In humans, durotomy had a positive effect on neurological function (92.3 %) and in animals (83.3 %). The myelotomy method has been effective in 80 % of animal studies, but only one clinical study of myelotomy has reported positive results for improved movement and sensation in humans, but studies have reported that both dural and myelotomy are not effective for spinal cord injury. Khaing et al. [15] showed that both subdural resection alone and subdural resection combined with myelotomy were effective in alleviating local intracranial hypertension. Histological examination 10 w after surgery showed that the combination of dural resection and myelotomy improved spinal tissue retention by 13.7 % compared to the use of dural resection alone. Myelotomy alone was associated with a 25.9 % improvement, but both types of decompression had a significant beneficial effect on gray matter conservation. Compared with myelotomy alone, epidurotomy and myelotomy improved motor neuron retention by 174.3 % and epidurotomy and myelotomy also significantly improved recovery of hind limb motor function. There are some differences between the results of the above studies and the results of this study, which may be mainly caused by differences in the individual subjects, sample size and surgical methods, but both the above two groups have confirmed the effectiveness of myelotomy and dural resection for decompression treatment of spinal cord injury. However, this study showed that the recovery of motor, sensory and limb functions was higher than that of dural surgery, which may be because dural surgery can relieve the pressure in the spinal canal, thereby reducing the compression on the spinal cord, thereby improving the spinal microcirculation and alleviating a series of subsequent secondary inflammatory reactions. Myelotomy not only relives the compression in the spinal canal, but also removes the epidural fracture fragments, necrotic gray matter and white matter, preserving as much of the surviving nerve tissue as possible. According to relevant research results, after spinal cord injury is given appropriate environmental changes, the injured nerve axons may regenerate and restore spinal cord function [16]. Some researchers have also explored the conditions for spinal cord nerve regeneration and the results show that firstly, a certain amount of neurons must survive to synthesize substances for axon regeneration and secondly, they must grow enough distance to synthesize functional connections with target cells [17]. Some studies also showed that there was no degeneration of nerve fibers and myelinated sheath in paraplegia patients under the plane, which also indicated that there was a high theoretical feasibility for the recovery of spinal cord function in patients. Therefore, the recovery of limb, motor and sensory functions in patients undergoing myelotomy was higher than that undergoing durotomy alone [18].
In conclusion, for patients with complete paralysis caused by cervical spine injury, myelotomy can achieve better recovery of neurological function and lower pain sensation, and can improve patients’ motor, sensory and limb functions, with less complications and higher safety.
Acknowledgement:
This work was supported by the Jinling Hospital, School of Medicine, Nanjing University.
Conflicts of interest:
The authors declared no conflicts of interest.
References
- Rouanet C, Reges D, Rocha E, Gagliardi V, Silva GS. Traumatic spinal cord injury: Current concepts and treatment update. Arq Neuropsiquiatr 2017;75:387-93.
[Crossref] [Google Scholar] [Pub Med]
- Li M, Wang G, Zhu S. Surgical treatment of traumatic cervical spinal cord injury with intramedullary hemorrhage and edema. Chin J Spine Spinal Cord 2001;31(1):31-6.
- Liu A, Mo K, Liao Q. Treatment of thoracolumbar fracture with spinal cord injury by paravertebral muscle approach combined with posterior median laminectomy. J Neck Low Pain 2020;41(2):224-5.
- Jalan D, Saini N, Zaidi M, Pallottie A, Elkabes S, Heary RF. Effects of early surgical decompression on functional and histological outcomes after severe experimental thoracic spinal cord injury. J Neurosurg Spine 2017;26(1):62-75.
[Crossref] [Google Scholar] [Pub Med]
- Meyer C, Bendella H, Rink S, Gensch R, Seitz R, Stein G, et al. The effect of myelotomy following low thoracic spinal cord compression injury in rats. Exp Neurol 2018;306:10-21.
[Crossref] [Google Scholar] [Pub Med]
- Gao S, Liu H, Zhang N. Clinical observation of Qishenhuanwu capsule in the treatment of acute hyperalgesia of cervical spinal cord injury without fracture and dislocation. J Integr Tradit Chin West Med 2001;30(4):360-8.
- Ye Y, Lin Y. Effect of 4D traction combined with Shentong Zhuyu Decoction in the treatment of cervical fracture and dislocation complicated with spinal cord injury. J Integr Tradit Chin West Med 2019;28(28):3114-8.
- Khorasanizadeh M, Yousefifard M, Eskian M, Lu Y, Chalangari M, Harrop JS, et al. Neurological recovery following traumatic spinal cord injury: A systematic review and meta-analysis. J Neurosurg Spine 2019;30(5):683-99.
[Crossref] [Google Scholar] [Pub Med]
- Wang R, Hu X, Zhang T, Fugl‐Meyer KS, Langhammer B. Cross‐cultural adaptation of Life Satisfaction Checklist‐11 among persons with stroke in China: A reliability and validity study. Physiother Res Int 2021;26(2):e1887.
[Crossref] [Google Scholar] [Pub Med]
- Eckert MJ, Martin MJ. Trauma: Spinal Cord Injury. Surg Clin North Am 2017;97(5):1031-45.
[Crossref] [Google Scholar] [Pub Med]
- Mariano R, Flanagan EP, Weinshenker BG, Palace J. A practical approach to the diagnosis of spinal cord lesions. Pract Neurol 2018;18(3):187-200.
[Crossref] [Google Scholar] [Pub Med]
- Fariña MM, de la Barrera SS, Marqués AM, Velasco MF, Vazquez RG. Update on traumatic acute spinal cord injury. Part 2. Med Intensiva 2017;41(5):306-15.
[Crossref] [Google Scholar] [Pub Med]
- Yang D, Li J, Yang M. Neurosurgery 2015(1):147-50.
- Telemacque D, Zhu FZ, Ren ZW, Chen KF, Drepaul D, Yao S, et al. Effects of durotomy versus myelotomy in the repair of spinal cord injury. Neural Regen Res 2020;15(10):1814-20.
- Khaing ZZ, Cates LN, Dewees DM, Hyde JE, Gaing A, Birjandian Z, et al. Effect of durotomy versus myelotomy on tissue sparing and functional outcome after spinal cord injury. J Neurotrauma 2021;38(6):746-55.
[Crossref] [Google Scholar] [Pub Med]
- Yu R, Yin G, Zhao J, Chen H, Meng D, Zhang J, et al. Reducing neuron apoptosis in the pontine micturition center by nerve root transfer for restoration of micturition function after spinal cord injury. BioMed Research International. 2020;2020.
- O’Shea TM, Burda JE, Sofroniew MV. Cell biology of spinal cord injury and repair. J Clin Invest 2017;127(9):3259-70.
[Crossref] [Google Scholar] [Pub Med]
- Hachem LD, Ahuja CS, Fehlings MG. Assessment and management of acute spinal cord injury: From point of injury to rehabilitation. J Spinal Cord Med 2017;40(6):665-75.
[Crossref] [Google Scholar] [Pub Med]