- *Corresponding Author:
- L.Gan
Shanghai Institute of Technology, School of Chemical and Environmental Engineering, Shanghai 200120, China
E-mail: sit2016@vip.sina.com
| Date of Received | 27 November 2022 |
| Date of Revision | 14 June 2023 |
| Date of Acceptance | 08 January 2024 |
| Indian J Pharm Sci 2024;86(1):64-74 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
At present, the drugs used to treat dry eye are mainly ocular topical drugs, with only 5 % of the drugs are absorbed, which on the market have adverse reactions, such as eye pain, eye burns, conjunctival hyperemia and poor patient compliance. In order to reduce irritation and improve bioavailability, a new type of ocular drug delivery system, mixed micelles modified with cationic hyaluronic acid was studied by rotary evaporation method. Vitamin E tocopheryl polyethylene glycol succinate and polyoxyethylene hydrogenated castor oil, two non-ionic surfactants are used for the preparation of cyclosporin micelles. Finally, the micelles were modified with cationic hyaluronic acid to form the final formulation named cationic hyaluronic acid modified cyclosporin A nanomicelle, which was designed with particle size of 17.21 nm, polydispersity index of 0.221, zeta potential of -23.4 mV and osmotic pressure of 299 mOsmol/kg. The release rate of cyclosporin A nanomicelle in vitro reached 88 %, and the preparation showed reduced surface tension (34.46 mN/m) and contact angle (22.8°), which indicated that cyclosporin A nanomicelle had better wetting and spreading properties. Transmission electron microscope showed that the preparation was spherical, homogeneous and no aggregates. After modification with cationic hyaluronic acid, the corneal permeability and apparent permeability increased by about 1.4 times and 1.3 times respectively, indicating that cyclosporin A nanomicelle can improve corneal penetration and improve bioavailability. Draize test of rabbit eye surface showed that cyclosporin A nanomicelle has no ocular irritation. In conclusion, Cationic hyaluronic acid modified cyclosporin A nanomicelle might be a promising ocular drug delivery system for the treatment of dry eye.
h2 class="post-title">KeywordsCationic hyaluronic acid, cyclosporine, micelle, ocular, rotary evaporation
Dry keratitis and conjunctivitis, often called dry eye, is a common ophthalmic disease. Many factors may cause dry eye, and these factors may cause pathophysiological changes on the ocular surface[1]. Dry eye causes burning, foreign body sensation, tingling, pain, photophobia and blurred vision in the eye[2].
Cyclosporine A (CsA) is an immunosuppressive peptide that has been shown to be useful in patients with dry keratitis and conjunctivitis[3]. CsA is a molecule with neutral charge and hydrophobicity[4]. The low water solubility of cyclosporin A poses a challenge for the preparation of safe and effective ophthalmic formulations[5]. In the past two decades, three commercial products of cyclosporin A ocular drug delivery system have been marketed. Restasis® (Allergan, USA), Ikervis® (Santen Pharma, Japan) and Cequa® (Sun Pharma, India).
Restasis®, approved by Food and Drug Administration (FDA) in 2002[6], is an anionic oil-in-water emulsion[7]. The prescription contains CsA, castor oil, glycerin, polysorbate 80 and carbomer type A. Although compared with oil-based CsA solutions, oil-in-water CsA emulsions can reduce related side effects, long-term use of eye drops will cause strong side effects such as eye burns (17 %) and conjunctival hyperemia (5 %)[8]. Poor ocular tolerance, low bioavailability[9], and instability are other major drawbacks reported with Restasis®[10].
Ikervis® was launched in Europe in 2015[11]. It is a cationic emulsion with no preservatives, containing 0.1 % CsA, chain fatty acid triglyceride, cetalkonium chloride, tyloxapol, poloxamer 188 and glycerin[12]. Since the corneal and conjunctival cells are negatively charged at physiological pH, the cationic emulsion interacted with the ocular surface through electrostatic action, which extends the ocular surface retention time and improves the bioavailability of the drug[13]. However, the milky white appearance of Ikervis® causes poor patient compliance such as eye pain (19 %), eye irritation (17.8 %), eye congestion (5.5 %), tears (6.2 %)[14].
Cequa® is a preservative-free nanomicelle solution approved by FDA in 2018[15]. It contains 0.09 % CsA, polyoxyl hydrogenated castor oil, octoxynol-40, polyvinylpyrrolidone, sodium phosphate monobasic dihydrate, sodium phosphate dibasic anhydrous, water for injection and sodium hydroxide or hydrochloric acid to adjust pH[16]. The ophthalmic solution has an osmolality of 160-190 mOsmol/kg and a pH of 6.5 to 7.2[17]. It is a clear aqueous solution. According to the clinical report of Cequa®, the product still has adverse reactions after long-term use, which might be due to its low osmotic pressure. Cequa® has some adverse effects such as (22 %) and conjunctival congestion (6 %)[18,19].
Micelles, composed of amphiphilic molecules, are self-assembled in aqueous medium to form an organized supramolecular structure[20]. It is an attractive carrier, due to its potential to dissolve hydrophobic molecules in aqueous solutions. In addition, it is reported that the small size in the nanometer range and the highly variable surface properties are advantageous in ophthalmic drug delivery[21]. Micelles can promote the penetration of drugs through the conjunctiva and increase the concentration of drugs inside the eyeball and even the back of the eye. It is reported that after a single topical administration of Cequa®, CsA was found to be distributed in the conjunctiva, cornea, vitreous, and retina[22]. The results showed that micelles not only act on the anterior segment of the eye but might also be transmitted to the posterior segment of the eye.
However, long-term use of Cequa® can cause side effects, such as eye pain and conjunctival redness and swelling. The reason for the adverse reaction may be the low osmotic pressure in the preparation and the use of octocynol-40. The osmotic pressure of the eye is 248~371 mOsmol/kg, while the osmotic pressure of Cequa® is 170 mOsmol/kg. Johnson et al.[23] studied the eye irritation test of octoxynols surfactant and concluded that the use of octoxynols products around the eyes should be avoided. Abhirup et al.[24] studied self-assembled multilayer nanomicelles composed of two polymers (polyoxyethylene Hydrogenated Castor Oil (HCO-40) and octoxynol-40). In vitro cytotoxicity studies have shown that octoxynol-40 could decrease the viability of choroid-retinal endothelial RF-6A cells.
In order to reduce eye irritation, increase ocular retention and improve bioavailability, this study used HCO-40 and Vitamin E Tocopheryl Polyethylene Glycol Succinate (TPGS) to prepare micelles and then modified them with cationic hyaluronic acid. HCO-40 is a commonly used surfactant, which is an FDA-approved pharmaceutical excipient for ophthalmology[25]. As a non-ionic surfactant, HCO-40 not only reduces eye irritation but also improves the solubility of the drug.
Moreover, TPGS was used instead of octoxynol-40. TPGS is a water-soluble non-ionic surfactant formed by esterifying vitamin E succinate with polyethylene glycol. As the alkyl chain of TPGS is longer than that of octoxynol-40, the interaction between HCO-40 and TPGS might be stronger than that of octoxynol-40. The critical micelle concentration of mixed micelles and the total surfactant content are expected to be lower than that of Cequa®, which in turn would solve the problem of high ocular irritation.
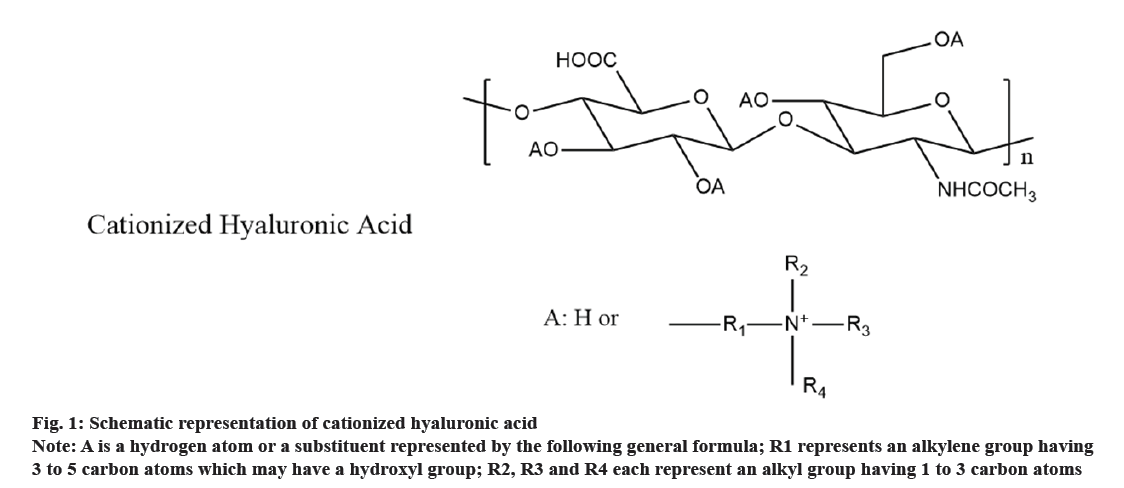
Hyaluronic acid is a natural, non-irritating polysaccharide polymer, which is widely used in ocular delivery systems[26]. In addition to its mucoadhesive properties, sodium hyaluronate exhibits high water-binding capacity, non-irritant, viscosity-increasing, and pseudoplastic behavior. So it is an attractive ophthalmic drug delivery vehicle[27]. Commercially available products include 0.1 % and 0.3 % hyaluronic acid eye drops. Cationic hyaluronic acid is a derivative of hyaluronic acid, as shown in fig. 1, which is characterized in that at least a part of the hydrogen atoms of the hydroxyl group is substituted with a quaternary ammonium cationic group. As part of the groups are cationized, cationic hyaluronic acid can interact with the negatively charged cell surface, prolong the retention, and enhance the moisturizing effect. The cationized hyaluronic acid (HYALOVEILTM-P, Kewpie) has been widely used in all kinds of toiletries, which can keep the skin and hair moisturized for a long time. The schematic of cationized hyaluronic acid can be seen in fig. 1. But it has never been used in medicines. In this study, cationized hyaluronic acid with different degree of cationization was used to modify the micelle system to prolong the ocular residence.
Fig 1: Schematic representation of cationized hyaluronic acid
Note: A is a hydrogen atom or a substituent represented by the following general formula; R1 represents an alkylene group having 3 to 5 carbon atoms which may have a hydroxyl group; R2, R3 and R4 each represent an alkyl group having 1 to 3 carbon atoms
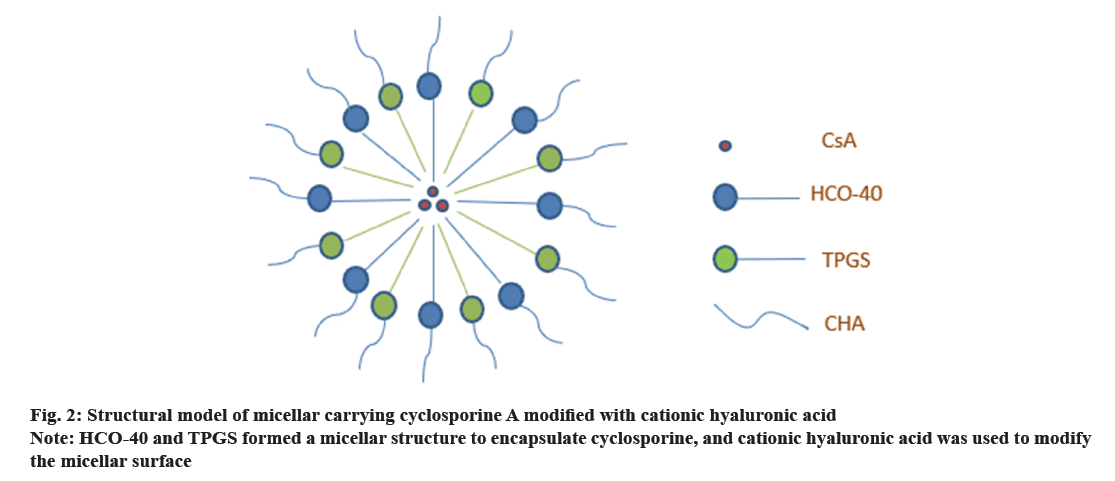
In this paper, HCO-40 and TPGS are combined for the first time to prepare CsA mixed micelles. Then cationized hyaluronic acid was first used to modify the micelle system. The final formulation model was shown in fig. 2. The formulations were characterized by physical and chemical properties, as particle size, zeta value viscosity, surface tension, contact angle, transmission electron microscopy and in vitro release. Ex vivo rabbit corneal penetration experiments were conducted to investigate the effects of CsA's different ophthalmic preparations on corneal penetration. The Draize test method was used to evaluate the ocular irritation of each formulation.
Materials and Methods
Materials:
Experimental animals: Male New Zealand white rabbits, weighing 2-3 kg, were used in experiments. The study was reviewed by the Ethics Committee of Shanghai Institute of Technology.
Experimental reagents: HCO-40 was purchased atomsfrom BASF, Germany. TPGS was purchased from Shanghai Lianlu Industrial Co., Ltd. CsA was purchased from Taizhouhx Co., Ltd, Guangzhou, China. HA1 (HA LQ60, MW 600 KDa), HA2 (HA AML, MW 900 kDa), Cationized Hyaluronic Acid with a cationization degree of 30 %, MW 600 kDa (CHA1), Cationized Hyaluronic Acid with a cationization degree of 40%, MW 200 kDa (CHA2) and Cationized Hyaluronic Acid with a cationization degree of 50%, MW 200 kDa (CHA3) was gifted by Kewpie Co., Ltd, Nakano, Japan. All other reagents were of analytical grade and used as received.
Preparation of formulations:
HCO-40, TPGS, CsA are dissolved in ethanol, and mix these three solutions and then the mixed solution is poured into a round bottom flask. The organic solvent was evaporated on a rotary evaporator to obtain a solid film. The obtained film was hydrated with water for injection and the film was completely dissolved in water to obtain micelles. Adjust the pH of the solution with sodium hydroxide or hydrochloric acid. CHA was weighed and dissolved in isotonic solution to provide CHA solution. To prepare CHA-coated nanomicelle, nanomicelle solution was added dropwise to CHA solution which was under magnetic stirring at 400 rpm. CHA-coated Nano Micelle (CHA-NM) is obtained by stirring the mixture under ambient temperature for 1 h. The preparation of modified cyclosporin micelles of hyaluronic acid is the same as above. The formulation of each preparation can be seen in Table 1.
| Formulation | Formulation name | CsA (W/V) | HCO-40 (W/V) | TPGS (W/V) | Hyaluronic acid (W/V) | Glycerin (W/V) |
|---|---|---|---|---|---|---|
| F1 | CsANM | 0.09 % | 0.40 % | 0.40 % | / | 2.50 % |
| F2 | 0.04 % HA1-CsANM | 0.04 % | ||||
| F3 | 0.03 % HA2-CsANM | 0.03 % | ||||
| F4 | 0.07 % CHA1-CsANM | 0.07 % | ||||
| F5 | 0.8 % CHA2-CsANM | 0.80 % | ||||
| F6 | 0.18 % CHA3-CsANM | 0.18 % |
Note: Prescription details for each preparation: the amount of cyclosporine, HCO-40, TPGS and glycerol was the same and only the amount of hyaluronic acid was different
Table 1: The Formulation of Each Preparation
| Formulation | Formulation of CsANM | Content of HA | Viscosity (mpa/s) |
|---|---|---|---|
| CsANM | - | 1.32±0.05 | |
| 0.04 % HA1-CsANM | 90 mg CsA | HA1:0.04 g | 7.47±0.13 |
| 0.05 % HA1-CsANM | 0.4 g HCO-40 | HA1:0.05 g | 12.07±0.11 |
| 0.03 % HA2-CsANM | 0.4 g TPGS | HA2:0.03 g | 7.90±0.18 |
| 0.05 % HA2-CsANM | 2.5 g Glycerin | HA2:0.05 g | 12.96±0.27 |
| 0.07 % CHA1-CsANM | 100 ml pure water | CHA1:0.07 g | 7.65±0.03 |
| 0.15 % CHA1-CsANM | CHA1:0.15 g | 12.39±0.46 | |
| 0.20 % CHA2-CsANM | CHA2:0.20 g | 2.61±0.18 | |
| 0.80 % CHA2-CsANM | CHA2:0.80 g | 7.23±0.14 | |
| 0.18 % CHA3-CsANM | CHA3:0.18 g | 1.71±0.20 |
Note: Comparison between viscosities of different types and concentrations of hyaluronic acid; Data expressed as mean values±SD, n=3
Table 2: Measurement Results of Viscosity of CSA-Loaded Formulations
Restasis®[28] (0.05 % CsA emulsion, F7), Ikervis®[29] (0.1 % CsA cationic emulsion, F8) and Cequa®[30] (0.09 % CsA micelles, F9) were prepared following the manufacturer’s protocol. For emulsion production, oil and aqueous phases were emulsified at 70°, sheared (10 000 rpm) for 10 min and high pressure homogenized (600 bar/6 cycles). For micelles production, non-ionic surfactant and CsA were dissolved in ethanol, the organic solvent was removed by rotary evaporation and the film was hydrated with water for injection to obtain the final micelle[16].
Characterization of formulations:
Viscosity measurement: Under the condition of SC4-18 rotor and 100 rpm, the viscosity of the preparations was measured with a viscometer (DV3T BROOKFIELD, US), at ambient temperature. All measurements were performed in triplicate.
Size, Polydispersity Index (PDI) and Potential: The mean hydrodynamic diameter, PDI and zeta potential of CsA-NM and CHA-CsANM were determined by Dynamic Laser Scattering (DLS) using a zetasizer (Nano-ZS90, Malvern Instruments, UK) with a detection angle of 90° at 25° temperature. The final result is the average of three measurements of all samples.
Determination of osmotic pressure: Measuring osmotic pressure of prepared formulations by means of a freezing point osmometer (OSMOMAT 3000 basic, Gonotec GmbH, Germany).
Transmission Electron Microscopy (TEM): The ultrastructure of matter can be seen through a TEM. The carbon-coated copper mesh was clamped by forceps and placed on the filter paper. The sample was dropped onto a copper mesh. Then, the copper mesh with the sample was clamped by tweezers, and 2 % phosphotungstic acid was added to the copper mesh for staining. After the sample was stained for 3 min, the staining solution was blotted with filter paper, and the sample was observed and photographed by TEM (F20 Thermo Fisher, US).
Surface tension measurement: By using the ring method, the surface tension of the formulation was measured by a surface tensiometer (K100 KRUSS Germany). All measurements were performed in triplicate.
Contact angle measurement: Measure the contact angle of the prepared formulation with a contact angle meter (DSA, KRUSS. Germany). Approximately 2 μl of the formulation was dropped on a glass slide, and the dropped image was captured and measured by the instrument[31]. All measurements were performed in triplicate.
In vitro drug release:
Using reverse dialysis to investigate the drug release behavior of F1~F9. Take 2 ml of the release medium and place it in a dialysis bag (MWCO14000) with one end open. Place the dialysis bag containing 3 ml of sample and 75 ml of release medium (30 % ethanol artificial tears (7.4)) at a speed of 100 rpm and a temperature of 35±1°[14]. At 30 min, 1 h, 1.5 h, 2 h, 4 h, 6 h, take out 200 μl of the contents in the dialysis bag for testing, and supplement 200 μl of dissolution medium. This volume not only satisfies the sink conditions but also allows the dialysis bag to be suspended in sufficient release medium. The solubility of CsA in 20 % ethanol is 60.61 μg/ml, and the solubility in 50 % ethanol is 167.24 μg/ml[32].
Total drug content:
The mobile phase was prepared with acetonitrile:methanol:water (62 %:5 %:33 % v/v/v), which was set at a flow rate of 1.0 ml/min. Detection wavelength was set at 210 nm. The sample tray temperature was maintained at 70°[14]. A volume of 20 μl was injected onto the High Performance Liquid Chromatography (HPLC) column for analysis.
Studies of corneal permeability:
Carefully fix the fresh cornea between the supply tank and the receiving tank of the diffusion tank, with the epithelial layer of the cornea facing the supply tank. Add 7 ml of Glutathione Bicarbonate Ringer's (GBR) solution containing 30 % ethanol at 37° into the supply pool and the receiving pool[14]. After the system was equilibrated for 10 min, the experimental group removed the solution in the supply tank and replaced it with a sample solution. Control the water circulation to 37°, and slowly blow O2/CO2 (95 %:5 %) mixed gas into the GBR solution. At 30 min, 60 min, 90 min, 120 min, 150 min, 180 min, 240 min and 300 min after the start of the test, 200 μl was sampled from the receiving cell, and an equal volume of 30 % ethanol-GBR solution preheated at 37° was added immediately to keep the volume in the receiving cell constant. Take 20 μl samples and perform HPLC measurement.
Calculate the sample concentration (μg/ml) at each sampling point, and calculate the cumulative permeation Qn (μg) and the apparent permeability coefficient Papp (cm/s) by the following equation (1):
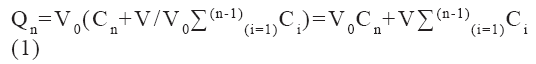
Among them, Cn is the measured concentration of the drug at time t, Ci is the measured concentration before time t, V0 is the volume of the solution in the receiving tank and V is the sampling volume.
The apparent corneal permeability coefficient (Papp) of different formulations was determined from the following equation (2):
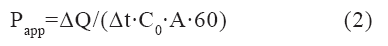
Where ΔQn/Δt (μg/min) is the flux across the corneal tissue, A is the area of diffusion (cm2), C0 (μg/ml) is the initial concentration of drug in donor compartment and 60 is taken as the factor to convert minute into second.
Ocular irritation test:
Using the Draize evaluation method, the rabbit was fixed on the rabbit stand, and 100 μl of the sample was dripped into the conjunctival sac in both eyes, and the eyelids were closed to make the drug distribution uniform.
Acute irritation: The rabbit eyes were given 3 consecutive doses with an interval of 5 min. Check the eye indicators 30 min after the last dose.
Long-term irritation: Rabbit eyes are administered 3 times a day for 7 consecutive d. 2 h after the last administration, check the various indicators of the eye[14].
Statistical analysis:
An Analysis of Variance (ANOVA) by Social Package for Statistical Study Software (SPSS 22®, SPSS Inc., Chicago, IL) was used to test for statistical significance between the prepared formulations and control. p<0.05 was considered as significant.
Results and Discussion
The tear viscosity of human is 0.3~8.3 mPa/s. In order to make the prescription have proper viscosity, the amount of hyaluronic acid was adjusted in this study. The measurement results of viscosity of CsA-loaded formulation can be seen in Table 2.
Table 2 shows that formulations without hyaluronic acid modification have lower viscosity than the other groups. The solubility of CHA3 is low at 1.8 mg/ml, so the viscosity can only reach 1.7 cp in the case of saturated solubility. In order to get the same viscosity value, more cationic hyaluronic acid is used. Moreover, the solubility of cationized Hyaluronic Acid (cationized HA) with a cationization degree of 50 % is so poor that it is far below 7 mPa/s. In the hyaluronic acid modified group, the viscosity of 0.18 % cationized HA with a cationization degree of 50 % was lower than that of the other groups.
The characterization results of the different cyclosporine formulations were shown in Table 3. The particle size of F1 was 10.71 nm, and PDI was 0.124. After modification with hyaluronic acid, the particle size increases. After the micelles modified with hyaluronic acid, the particle size increased from 10.71-21.97 nm, and the PDI increased to 0.228. With the increase in the degree of substitution of the hydroxyl group of hyaluronic acid, the zeta of the hyaluronic acid-modified micellar formulation increased from -33.5 mV to -5 mV. In F4, F5 and F6 formulations, as the degree of cationization of hyaluronic acid increases, the absolute value of its zeta also decreases. PDI is less than 0.3, indicating that the particle size is uniform.
| Formulation | Size (nm) | PDI | Zeta (mV) | Osmolarity (mOsmol/kg) | Viscosity (mpa/s) | Surface tension (γ,mN/m) | Contact angle(θ) |
|---|---|---|---|---|---|---|---|
| F1 | 10.71 | 0.12 | -28.9 | 297 | 1.32 | 34.8 | 29.91 |
| F2 | 18.15 | 0.15 | -33.4 | 298 | 7.47 | 35.51 | 25.18 |
| F3 | 16.37 | 0.2 | -33.5 | 298 | 7.9 | 34.73 | 25.56 |
| F4 | 17.21 | 0.22 | -23.4 | 299 | 7.65 | 34.6 | 22.08 |
| F5 | 21.97 | 0.13 | -17.3 | 318 | 7.23 | 34.56 | 27.84 |
| F6 | 14.48 | 0.23 | -5.31 | 303 | 1.71 | 34.46 | 24.18 |
| F7 | 204.2 | 0.16 | -20.4 | 247 | 7.4 | 39.4 | 22.13 |
| F8 | 186.5 | 0.12 | 31.5 | 259 | 1.49 | 31.61 | 25.16 |
| F9 | 20.12 | 0.15 | -23.9 | 170 | 1.68 | 35.59 | 25.44 |
Note: Results of the physical and chemical properties of different cyclosporine formulations including three CsA commercial products (F7~F9)
Table 3: Characterization Results of Different Cyclosporine Preparations
Table 3 shows that Cequa® (F9) has a particle size of 20.12 nm and Restasis® (F7) and Ikervis® (F8) as emulsions have particle sizes larger than the micelle size. Ikervis® contains cationic surfactants whose final zeta value shows positive charge.
The tear osmolarity is significantly associated with DED, as the increase of tear osmolarity accompanies by the disease, and is the trigger mechanism of DED. Therefore, the preparations of this product are adjusted to be isotonic with physiology.
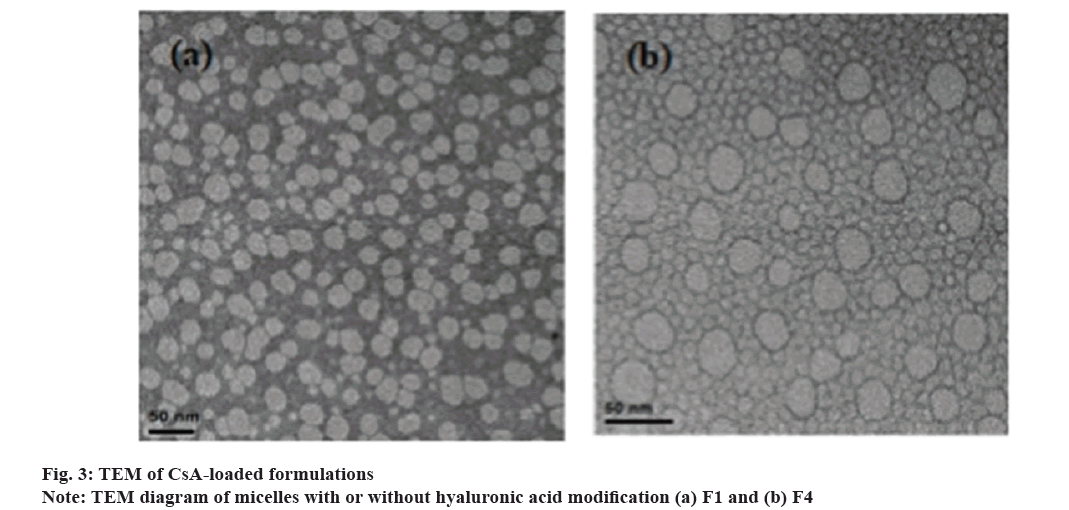
The micellar preparation is clear and transparent. Fig. 3a is a micellar preparation without HA, (b) is a micellar preparation modified with CHA1. What can be clearly seen from the fig. 3b is the micelles without hyaluronic acid have a uniform particle size. It can be seen from (b) that the micelle preparations modified with hyaluronic acid are still spherical and have the same shape without significant changes in particle size.
The lower the surface tension of the preparation, the easier it is to wet the hydrophobic surface of corneal epithelial and lipid layer of the precorneal tear. The surface tension of the Normal Saline (NS) is 70.35±0.06 mN/m. Table 3 shows that the surface tension of F1~F9 is significantly lower than that of NS.
The contact angle shows the degree of wetting of the material. Low values indicate good liquid spreading or wetting ability. If the angle is less than 90°, it means that the liquid wets the solid. Zero contact angles indicates complete wetting. The contact angle of the NS is 31.67±0.87 mN/m. Table 3 shows that the contact angle of the micelles modified with hyaluronic acid is reduced compared with micelles containing no hyaluronic acid, because the spreading effect of the formulation is increased after the modification with hyaluronic acid. And compared with other CsA preparations, the contact angle of CHA1-CsANM is 22.08°, which is the lowest. Compared with the contact angle of CHA1-CsANM, the contact angle of CHA2-CsANM and CHA3-CsANM increased, which may be caused by the difference in molecular weight.
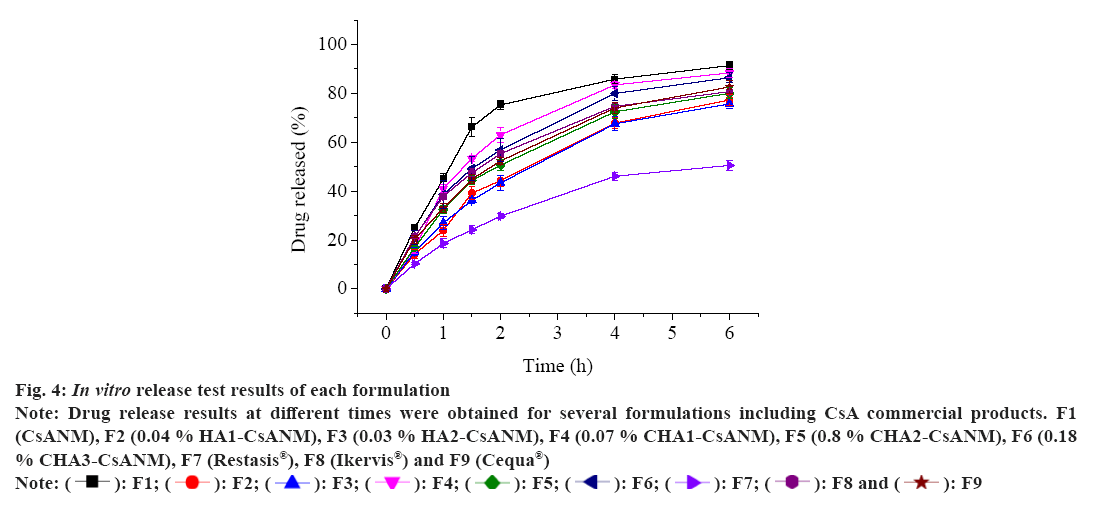
Fig 4: In vitro release test results of each formulation
Note: Drug release results at different times were obtained for several formulations including CsA commercial products. F1 (CsANM), F2 (0.04 % HA1-CsANM), F3 (0.03 % HA2-CsANM), F4 (0.07 % CHA1-CsANM), F5 (0.8 % CHA2-CsANM), F6 (0.18 % CHA3-CsANM), F7 (Restasis®), F8 (Ikervis®) and F9 (Cequa®)
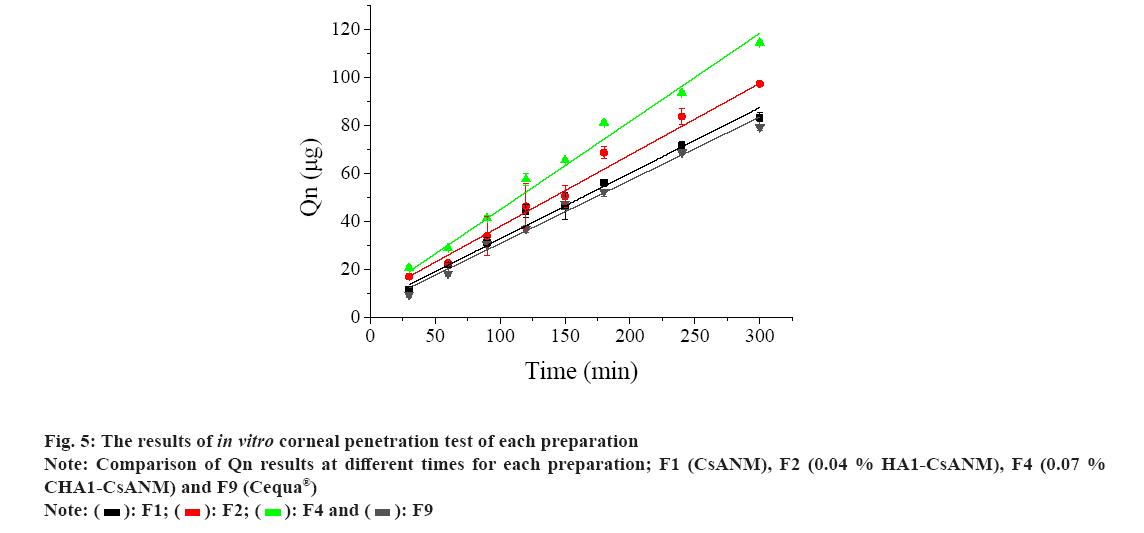
Fig. 5 shows the corneal penetration of the four formulations. The average molecular weight of HA1 and CHA1 are both 600 KDa. Keeping the same average molecular weight of hyaluronic acid is to compare whether cationization will affect the corneal permeability of the preparation. When the modification of hyaluronic acid will affect the corneal permeability of the preparation, the commercially available preparation Cequa® served as the control group. The purpose of choosing CsANM and HA1-CsANM is to compare whether the modification of hyaluronic acid affects corneal permeability.
The results of each formulation in fig. 5 and Table 4 showed that the hyaluronic acid-modified micelles have a better corneal permeability and apparent permeability coefficient compared with micelles with no hyaluronic acid modification. And the cationic hyaluronic acid-modified micelles (CHA1-CsANM) have a best performance. Results of Draize test can be seen in Table 5. Fig.
| Name of each group of preparations | CsA content (μg/ml) | Papp (×10-6 cm/s) |
|---|---|---|
| F1 | 890.50±3.1 | 5.71±2.1 |
| F2 | 889.95±4.6 | 6.27±1.7 |
| F4 | 889.55±2.5 | 6.82±0.8 |
| F9 | 902.85±1.8 | 5.31±1.4 |
Note: Comparison of the apparent permeability coefficients of the four formulations (preparations without hyaluronic acid, preparations containing plain hyaluronic acid, preparations containing cationic hyaluronic acid, and CsA commercial products). There were significant differences between F4 and F9 (p<0.05)
Table 4: Drug Content and Apparent Corneal Permeability Coefficient of Each Preparation
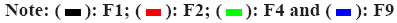
Fig 6 shows the photos taken after 7 d of long-term irritation of rabbit eyes. Normal saline was used as the control group to evaluate F1, F2, F4 and F9 in vivo. In short-term and long-term stimulation evaluation tests, the F1, F2, and F4 scores are all zero, indicating that CsANM, HA1-CsANM and CHA1-CsANM have no stimulating effect even with long-term stimulation. Table 5 shows that F9 has both short-term and long-term secretions, conjunctival hyperemia and slight edema, all showing irritation, which may be related to the surfactant octoxynol-40 contained in F9, or low osmotic pressure (170 mOsmol/kg).
From the comparison of the 0.05 % HA1-CsANM and 0.07 % CHA1-CsANM formulations in Table 2, it can be seen that the viscosity of the cationized formulation will become lower. In the experiment, it was found that compared with 40 % cationized CHA2, the solubility of 50 % cationized CHA3 can only reach 0.18 %, indicating that the degree of cationization is too high, which will significantly reduce the solubility of CHA. The reason for this phenomenon may be that with cationized formulations, the hydrophilicity of hyaluronic acid is reduced, resulting in a decrease in the solubility of hyaluronic acid. The degree of substitution in the hyaluronic acid structure affects solubility. When the solubility is satisfactory, an appropriate amount is required to achieve the desired viscosity.
| Content | Normal saline solution | F1 | F2 | F4 | F9 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| / | A | B | A | B | A | B | A | B | A | B |
| Corneal opacity | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 |
| Corneal injury | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 |
| Iris injury | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 |
| Conjunctival redness | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 1/3 | 1/3 |
| Conjunctival chemosis | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 1/4 | 1/4 |
| Secretions | 0/3 | 0/3 | 0/3 | 0/3 | 1/3 | 0/3 | 0/3 | 0/3 | 1/3 | 1/3 |
| Irritation | non | non | non | non | non | non | non | non | slight | slight |
Note: Draize test is one of the commonly used eye irritation tests to evaluate the irritation of drugs on different ocular surface sites. "A" Acute irritation evaluation result, "B" Long-term irritation evaluation result
Table 5: Results of the Draize Test
The surface tension of F1~F9 is significantly lower than that of NS, which may be due to the addition of surfactants in the CsA formulation, which reduces the surface tension of the formulation. It is shown that the cyclosporine preparation is easier to wet the ocular surface than the isotonic solution.
The micelles not modified with hyaluronic acid had a higher release than the micelles modified by hyaluronic acid. It may be that a layer of hyaluronic acid was modified outside the micelles, which delayed the release of the drug. It shows that the addition of hyaluronic acid affects the release amount. Except for F2, F3 and F5, other micellar formulations have higher release than emulsion F8 (Ikervis®). The lowest release of F7 (Restasis®) may be due to the oily base in the prescription and the larger particle size of the emulsion. The combination of these two factors hinders the release of the drug. The release amount of cationic hyaluronic acid-modified micelles (F4, F5, F6) is higher than that of ordinary hyaluronic acid-modified micelles (F2, F3). F2 and F3 are micelles modified with ordinary hyaluronic acid, and the concentration of hyaluronic acid modification is almost the same. The molecular weight of HA1 is 600 KDa, and the molecular weight of HA2 is 900 KDa. Although there is a difference in molecular weight, there is no significant difference in release profiles, indicating that the molecular weight of hyaluronic acid has little effect on drug release. This indicates that the concentration of hyaluronic acid may affect the release of the preparation. There are also significant differences between the hyaluronic acid-loaded micelles (F4, F5, F6) with different degrees of modification. It can be concluded that as the concentration of cationized hyaluronic acid increases, the release amount gradually decreases.
Cationic hyaluronic acid-modified micelle (CHA1-CsANM) has a best corneal permeability and apparent permeability coefficient performance compared with other formulation, which may be due to hyaluronic acid increases the retention of the preparation in the cornea. The cationized hyaluronic acid modified micellar cornea has a high permeation rate. It may be that hyaluronic acid is cationized, which reduces the electrostatic repulsion with the cornea, so that the preparation increases the residence time in the cornea. Since there is no modification of hyaluronic acid, there is significant difference (p<0.05) in corneal penetration between F4 and F9. The study have shown that human cornea also contains P-gp. This may be TPGS has the effect of inhibiting P-gp efflux, thereby promoting the entry of drugs into the cornea.
In summary, a clear and transparent topical ophthalmic preparation has been prepared. The modified cyclosporine micelles prepared by HCO-40 and TPGS with cationic hyaluronic acid showed lower surface tension and contact angle. CHA-CsANM's nano-micelle preparations use a small amount of surfactant, which can reduce eye irritation. The formulation is relatively small in size, spherical and homogeneous, without aggregates. And CHA1-CsANM has the lowest contact angle, which is good for spreading and wetting in the eye. The micelles modified with CHA1 have high corneal penetration, which is beneficial to improve the bioavailability. Cationic hyaluronic acid modified nanomicelle technology is a promising ophthalmic dosage form for the delivery of cyclosporine drugs for the treatment of dry eye.
Acknowledgements:
The authors greatly appreciate the generous provision of cationic hyaluronic acid by Kewpie Co., Ltd, Nakano, Japan.
Conflict of interest:
The authors declared no conflict of interests.
References
- Rodriguez-Aller M, Guillarme D, El Sanharawi M, Behar-Cohen F, Veuthey JL, Gurny R. In vivo distribution and ex vivo permeation of cyclosporine A prodrug aqueous formulations for ocular application. J Control Release 2013;170(1):153-9.
[Crossref] [Google Scholar] [PubMed]
- Javadi MA, Feizi S. Dry eye syndrome. J Ophthalmic Vis Res 2011;6(3):192-8.
[PubMed]
- Utine CA, Stern M, Akpek EK. Clinical review: Topical ophthalmic use of cyclosporin A. Ocul Immunol Inflamm 2010;18(5):352-61.
[Crossref] [Google Scholar] [PubMed]
- Jurak M, Wiącek AE, Przykaza K, Ładniak A, Woźniak K. Temperature-dependent interactions in the chitosan/cyclosporine A system at liquid–air interface. J Thermal Anal Calorim 2019;138(6):4513-21.
- Lallemand F, Schmitt M, Bourges JL, Gurny R, Benita S, Garrigue JS. Cyclosporine A delivery to the eye: A comprehensive review of academic and industrial efforts. Eur J Pharm Biopharm 2017;117:14-28.
[Crossref] [Google Scholar] [PubMed]
- Tamilvanan S, Kumar BA. Influence of acetazolamide loading on the (in vitro) performances of non-phospholipid-based cationic nanosized emulsion in comparison with phospholipid-based anionic and neutral-charged nanosized emulsions. Drug Dev Ind Pharm 2011;37(9):1003-15.
[Crossref] [Google Scholar] [PubMed]
- Tamilvanan S, Benita S. The potential of lipid emulsion for ocular delivery of lipophilic drugs. Eur J Pharm Biopharm 2004;58(2):357-68.
[Crossref] [Google Scholar] [PubMed]
- Kang H, Cha KH, Cho W, Park J, Park HJ, Sun BK, et al. Cyclosporine Amicellar delivery system for dry eyes. Int J Nanomed 2016:2921-33.
[Crossref] [Google Scholar] [PubMed]
- Karn PR, Kim HD, Kang H, Sun BK, Jin SE, Hwang SJ. Supercritical fluid-mediated liposomes containing cyclosporin A for the treatment of dry eye syndrome in a rabbit model: Comparative study with the conventional cyclosporin A emulsion. Int J Nanomed 2014:3791-800.
[Crossref] [Google Scholar] [PubMed]
- Gupta C, Chauhan A. Ophthalmic delivery of cyclosporine A by punctal plugs. J Control Release 2011;150(1):70-6.
[Crossref] [Google Scholar] [PubMed]
- Garrigue JS, Daull P, Feraille L, Barabino S. Comparative efficacy of cyclosporine eye drop formulations in a mouse model of dry eye. Invest Ophthalmol Vis Sci 2016;57(12):421.
- Dukovski BJ, Juretić M, Bračko D, Randjelović D, Savić S, Moral MC, et al. Functional ibuprofen-loaded cationic nanoemulsion: Development and optimization for dry eye disease treatment. Int J Pharm 2020;576:118979.
- Boboridis KG, Konstas AG. Evaluating the novel application of cyclosporine 0.1% in ocular surface disease. Expert Opin Pharmacother 2018;19(9):1027-39.
[Crossref] [Google Scholar] [PubMed]
- Liu Y, Wang Y, Yang J, Zhang H, Gan L. Cationized hyaluronic acid coated spanlastics for cyclosporine A ocular delivery: Prolonged ocular retention, enhanced corneal permeation and improved tear production. Int J Pharm 2019;565:133-42.
[Crossref] [Google Scholar] [PubMed]
- Jerkins GW, Pattar GR, Kannarr SR. A review of topical cyclosporine A formulations a disease-modifying agent for keratoconjunctivitis sicca. Clin Ophthal 2020:481-9.
[Crossref] [Google Scholar] [PubMed]
- Weiss SL, Mitra AK, McNally EJ, inventors; Sun Pharma Global FZE, assignee. Topical cyclosporine-containing formulations and uses thereof. United States patent US 10,918,694. 2021.
- Mandal A, Gote V, Pal D, Ogundele A, Mitra AK. Ocular pharmacokinetics of a topical ophthalmic nanomicellar solution of cyclosporine (Cequa®) for dry eye disease. Pharm Res 2019;36:1-21.
[Crossref] [Google Scholar] [PubMed]
- de Oliveira RC, Wilson SE. Practical guidance for the use of cyclosporine ophthalmic solutions in the management of dry eye disease. Clin Ophthal 2019:1115-22.
[Crossref] [Google Scholar] [PubMed]
- Bhamra MS, Gondal I, Amarnani A, Betesh S, Zhyvotovska A, Scott W, et al. Ocular manifestations of rheumatoid arthritis: implications of recent clinical trials. Int J Clin Res Trials 2019;4(2):139.
- Trivedi R, Kompella UB. Nanomicellar formulations for sustained drug delivery: Strategies and underlying principles. Nanomedicine 2010;5(3):485-505.
[Crossref] [Google Scholar] [PubMed]
- Komai Y, Ushiki T. The three-dimensional organization of collagen fibrils in the human cornea and sclera. Invest Ophthalmol Vis Sci 1991;32(8):2244-58.
[Google Scholar] [PubMed]
- Vadlapudi AD, Mitra AK. Nanomicelles: An emerging platform for drug delivery to the eye. Ther Deliv 2013;4(1):1-3.
[Crossref] [Google Scholar] [PubMed]
- Johnson Jr W. Final report on the safety assessment of octoxynol-1, octoxynol-3, octoxynol-5, octoxynol-6, octoxynol-7, octoxynol-8, octoxynol-9, octoxynol-10, octoxynol-11, octoxynol-12, octoxynol-13, octoxynol-16, octoxynol-20, octoxynol-25, octoxynol-30, octoxynol-33, octoxynol-40, octoxynol-70, octoxynol-9 carboxylic acid, octoxynol-20 carboxylic acid, potassium octoxynol-12 phosphate, sodium octoxynol-2 ethane sulfonate, sodium octoxynol-2 sulfate, sodium octoxynol-6 sulfate, and sodium octoxynol-9 sulfate. Int J Toxicol 2004;23:59-111.
[Crossref] [Google Scholar] [PubMed]
- Mandal A, Patel P, Pal D, Mitra AK. Multi-layered nanomicelles as self-assembled nanocarrier systems for ocular peptide delivery. AAPS PharmSciTech 2019;20:1-7.
[Crossref] [Google Scholar] [PubMed]
- Cholkar K, Gilger BC, Mitra AK. Topical, aqueous, clear cyclosporine formulation design for anterior and posterior ocular delivery. Transl Vis Sci Technol 2015;4(3):1.
[Crossref] [Google Scholar] [PubMed]
- Maulvi FA, Soni TG, Shah DO. Extended release of hyaluronic acid from hydrogel contact lenses for dry eye syndrome. J Biomater Sci Polym Ed 2015;26(15):1035-50.
[Crossref] [Google Scholar] [PubMed]
- Kaur IP, Smitha R. Penetration enhancers and ocular bioadhesives: Two new avenues for ophthalmic drug delivery. Drug Dev Ind Pharm 2002;28(4):353-69.
[Crossref] [Google Scholar] [PubMed]
- Khan W, Aldouby YH, Avramoff A, Domb AJ. Cyclosporin nanosphere formulation for ophthalmic administration. Int J Pharm 2012;437(1-2):275-6.
[Crossref] [Google Scholar] [PubMed]
- Lallemand F, Daull P, Benita S, Buggage R, Garrigue JS. Successfully improving ocular drug delivery using the cationic nanoemulsion, novasorb. J Drug Deliv 2012;2012:604204.
[Crossref] [Google Scholar] [PubMed]
- Shen Lee B, Kabat AG, Bacharach J, Karpecki P, Luchs J. Managing dry eye disease and facilitating realistic patient expectations: A review and appraisal of current therapies. Clin Ophthalmol 2020:119-26.
[Crossref] [Google Scholar] [PubMed]
- Abdelkader H, Wu Z, Al-Kassas R, Alany RG. Niosomes and discomes for ocular delivery of naltrexone hydrochloride: morphological, rheological, spreading properties and photo-protective effects. Int J Pharm 2012;433(1-2):142-8.
[Crossref] [Google Scholar] [PubMed]
- Guo J, Ping Q, Sun G, Jiao C. Lecithin vesicular carriers for transdermal delivery of cyclosporin A. Int J Pharm 2000;194(2):201-7.
[Crossref] [Google Scholar] [PubMed]