- *Corresponding Author:
- Xinyu Li
Department of Cardiothoracic Oncology, Zhangye People's Hospital Affiliated to Hexi University, Zhangye, Gansu 734000, China
E-mail: 13993642228@163.com
| This article was originally published in a special issue, “Role of Biomedicine in Pharmaceutical Sciences” |
| Indian J Pharm Sci 2023:85(2) Spl Issue “23-31” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the characteristics and influencing factors of electrocardiogram changes in patients with thyroid cancer after operation. This study retrospectively analyzed the case data of 122 patients who underwent thyroid surgery for the first time in the department of breast and thyroid surgery from January 2020 to December 2021. All patients were pathologically confirmed to be papillary thyroid carcinoma. Firstly, the perioperative changes of electrocardiogram indexes were compared in all patients and then the influencing factors (age, sex, blood lipid level, body mass index and surgical method) of perioperative electrocardiogram changes were analyzed by univariate analysis. After operation, the serum thyroid stimulating hormone of all patients was higher and serum free triiodothyronine and free thyroxine were lower than that before operation (p<0.05). After operation, PR interval and QRS duration was shorter than before operation (p<0.05). The perioperative changes of heart rate were statistically significant in different age groups (p=0.043). The age group ≥55 y old had more obvious heart rate changes than the age group <55 y old. There was a difference in heart rate change between groups in different body mass index group (p=0.05). Perioperative free triiodothyronine was positively correlated with heart rate (r=0.476, p=0.004). The change of perioperative free thyroxine was negatively correlated with the change of PR interval duration (r=-0.411, p=0.016). The difference of perioperative corrected QT interval between male and female was statistically significant (p=0.027). There was a negative correlation between perioperative free thyroxine change and p wave change (r=-0.416, p=0.014). Age, gender and body mass index have a certain influence on the changes of perioperative electrocardiogram indicators. Postoperative cardiac function monitoring should be strengthened in elderly and obese patients. The change of thyroid hormone level is correlated with the change of perioperative electrocardiogram index. In the process of long-term thyroid stimulating hormone suppression treatment after operation, it can be tried to establish the sex-age related electrocardiogram standard of stratified thyroid hormone level.
Keywords
Thyroid cancer, electrocardiogram, thyroid hormone, thyroid stimulating hormone
Thyroid cancer is a common malignant tumor of the endocrine system, among which Differentiated Thyroid Cancer (DTC) includes papillary thyroid cancer and follicular thyroid cancer, accounting for more than 90 % of thyroid cancer. In recent years, a large number of domestic and foreign studies have shown that the incidence of thyroid cancer has presented a significant upward trend[1-3]. The treatment of DTC depends on preoperative risk assessment and staging according to tumor location, size, number, local invasion and lymph node status, on which the treatment plan is decided. For patients with DTC, treatments usually include removal of the primary tumor tissue and metastatic lymph nodes; I-131 radiotherapy was selected according to tumor stage; long-term Thyroid Stimulating Hormone (TSH) suppression after surgery or radiotherapy; long-term follow-up was performed to monitor tumor recurrence and metastasis. For DTC, special attention should be paid to balance the advantages and disadvantages of treatment to avoid over-diagnosis and treatment in low-risk patients or patients with benign nodules. Studies have shown that Thyroid Hormones (TH) can not only regulate basal metabolism, but also have some effects on Heart Rate (HR), blood pressure and body temperature. Studies have proved that the greater the degree of TSH inhibition, the greater the risk of cardiovascular diseases, especially atrial fibrillation[4]. Therefore, all patients with thyroid cancer received exogenous intake of levothyroxine (TH) after operation and inhibited TSH level at the same time. In the process of long-term TSH inhibition therapy, the serum Triiodothyronine (T3) level and T3/Thyroxine (T4) value are increased and patients also faced with increased incidence and mortality of cardiovascular diseases and significantly increased risk of osteoporosis while suffering from physical, psychological and quality of life damage[1,5]. As an important auxiliary examination method, Electrocardiogram (ECG) examination is often used to identify cardiac lesions and arrhythmia screening and diagnosis because of its noninvasive, low cost and convenience. At present, there is no study on the changes of ECG in patients with exogenous subclinical hyperthyroidism caused by TSH inhibition after DTC. This study investigated the characteristics and influencing factors of ECG changes in patients with thyroid cancer after operation.
Materials and Methods
General information:
The clinical data of 122 patients who underwent thyroid surgery in the Department of Thyroid Surgery of our hospital from January 2020 to December 2021 were collected. All patients underwent total resection. Total thyroidectomy+isthmus resection+central group lymph node (VI) dissection (80 cases) and total thyroidectomy+isthmus resection+lateral cervical lymph node (II, III, IV) dissection (42 cases). The operation process was smooth and there were no special complications. Papillary thyroid carcinoma was confirmed by postoperative paraffin pathology. Clinical data including gender, height, weight, preoperative Triglyceride (TG), preoperative serum TSH, serum Free Triiodothyronine (FT3), serum Free Thyroxine (FT4) and serum FT4 were collected.
Twelve-lead ECG indicators: HR, PR interval, P wave, QRS wave, QT interval, Corrected QT Interval (QTc) duration, serum TSH, FT3, FT4, ECG indicators on the 3rd d after surgery.
Inclusion criteria: Complete medical records of patients; papillary thyroid carcinoma was confirmed by postoperative pathological paraffin section; first thyroid surgery and sign the informed consent.
Exclusion criteria: Pregnant or lactating women; previous history of head and neck irradiation and thyroid surgery; patients with previous history of tumor or chemotherapy; previous history of thyroid disease; previous history of hypertension, rheumatic heart disease, acute heart failure, coronary atherosclerotic heart disease, congenital heart disease, valvular heart disease, arrhythmia; previous use of amiodarone or alpha (α)/beta (β)-blockers or antagonists and patients with previous diagnosis of mental illness.
Methods:
Thyroid-related hormones: TSH, FT3 and FT4.
Abnormal ECG changes: ECG indicators including HR, P wave, PR interval, QRS duration, QT interval duration and QTc duration.
Measurement methods of the index:
Determination of serum thyroid related hormone levels: TSH, FT3 and FT4 levels were measured by chemiluminescence immunoassay (ADVIA Centaur XP, Siemens, United States of America (USA)). Normal TSH reference range was 0.27-4.2 mU/l; FT3 normal reference range was 3.1-6.8 pmol/l and FT4 normal reference range was 12-22 pmol/l.
Body Mass Index (BMI) calculation: The height (m) and weight (kg) of the patient were measured on admission and the weight (kg) was divided by the square of the height (m) (kg/m2), i.e., BMI=weight (kg)/height (m2).
Twelve-lead ECG tracing and analysis method: The subjects underwent routine 12-lead ECG examination before and on the 3rd d after surgery in a quiet state, with the paper speed set at 25 mm/s and the voltage set at l mV=10 mm. The results were interpreted by manual analysis and automatic instrument report. The indicators included HR, P wave, PQ interval, QRS duration, QT duration and QTc duration. ECG diagnosis refers to clinical electrocardiography.
Methods of research grouping:
Patients were divided into two groups according to age; <55 y and ≥55 y. According to gender, they were divided into two groups; male and female. Patients were divided into normal group and hyperlipidemia group according to their blood lipid levels. According to BMI, they were divided into three groups; normal group (BMI was <22.9 kg/ m2), overweight group (BMI was 22.9-28.5 kg/m2) and obese group (BMI was >28.5 kg/m2). Next, the changes of perioperative ECG indicators and thyroid related hormones in all patients were statistically analyzed, and the correlation between the two was analyzed.
Statistical analysis:
SigmaStat 3.5 statistical software was used for data analysis. Measurement data were expressed as mean±standard deviation (x±s) and t-test was used. Non-normal measurement data were expressed as x±s and F-test was used. Pearson correlation analysis was used for correlation analysis. p<0.05 indicates statistical significance.
Results and Discussion
100 and 22 patients with papillary thyroid cancer were included in the study. There were 42 males and 80 females, with an average age of 45.29±11.39 y. There were 28 cases with hyperlipidemia and 94 cases with normal blood lipids. There were 18 cases of BMI obesity (BMI was >28.5 kg/m2), 72 cases of normal group (BMI was 22.9-28.5 kg/m2) and 32 cases of low group (BMI was <22.9 kg/m2), as shown in Table 1.
| Clinical data | Composition | Number | Composition ratio (%) |
|---|---|---|---|
| Age (year) | <55 | 90 | 73.77 |
| ≥55 | 32 | 26.23 | |
| Gender | Male | 42 | 34.43 |
| Female | 80 | 65.57 | |
| Serum lipid level | Normal | 94 | 77.05 |
| Increase | 28 | 22.95 | |
| BMI (kg/m2) | <22.9 | 32 | 26.23 |
| 22.9-28. 5 | 72 | 59.02 | |
| >28.5 | 18 | 14.75 |
Table 1: Basic Clinical Data of the Patients
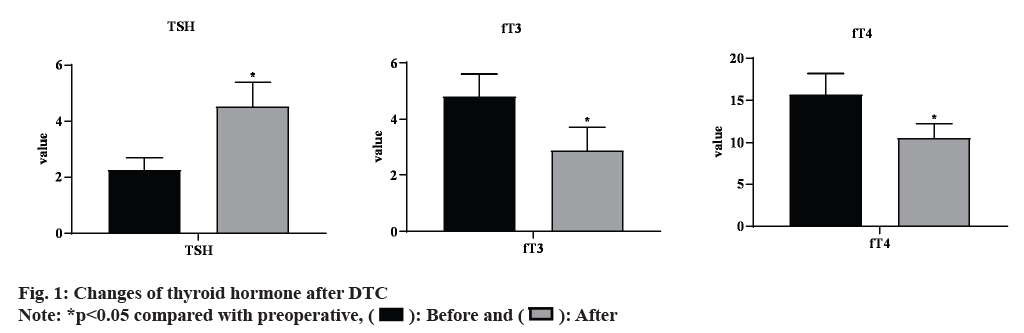
The preoperative and postoperative TSH, FT3 and FT4 values of all patients did not follow normal distribution according to the normality test. The preoperative and postoperative TSH, FT3 and FT4 values of all patients were compared before and after operation and the differences were statistically significant (p<0.05) as shown in fig. 1. Fig. 1 showed that on the 3rd d after operation, the serum levels of FT3 and FT4 of patients in the total resection group were significantly decreased compared with those before operation and the serum TSH level was increased.
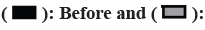
The HR, PR interval, QRS duration, QT duration, QTc duration and P wave of the patients before and after surgery followed normal distribution by normality test and were compared and analyzed before and after surgery, as shown in fig. 2. PR interval was shorter after operation than before operation and the difference was statistically significant (p<0.05). QRS duration was significantly shorter after operation than before operation (p<0.05). The other indexes showed no perioperative changes and the difference was not statistically significant (p>0.05).
There were significant differences in the perioperative HR changes among different age groups (t=2.103, p=0.043) and the HR changes were greater in the ≥55 y old group than in the <55 y old group. The difference of BMI was statistically significant by Analysis of Variance (ANOVA) (F=3.293, p=0.050) and there was no significant difference between the 22.9-28.5 kg/m2 group and the >28.5 kg/m2 group and the <22.9 kg/m2 group. There was no significant difference in perioperative HR between males and females, as shown in Table 2. Correlation analysis was performed between the change values of perioperative TSH, FT3 and FT4 and the change values of perioperative HR. There was a positive correlation between the change values of perioperative FT3 and HR (r=0.476, p=0.004), as shown in Table 3.
| Variety | Group | HR change value | t/F | p |
|---|---|---|---|---|
| Age (year) | <55 | 3.80±9.43 | ||
| ≥55 | -4.56±12.28 | 2.103 | 0.043 | |
| Gender | Male | -0.40±6.47 | ||
| Female | 2.42±12.11 | -0.691 | 0.494 | |
| Serum lipid level | Normal | 0.96±9.69 | ||
| Increase | 4.00±14.79 | 0.661 | 0.513 | |
| BMI (kg/m2) | <22.9 | 0.36±11.61 | ||
| 22.9-28.5 | -0.61±8.05 | |||
| >28.5 | 12.2±13.10 | 3.293 | 0.05 |
Table 2: Comparison of Perioperative HR Changes in Patients with Different General Data Groups
| r | p | |
|---|---|---|
| TSH change value | -0.42 | 0.815 |
| FT3 change value | 0.476 | 0.004 |
| FT4 change value | -0.18 | 0.307 |
Table 3: Correlation Analysis between Perioperative Changes in TSH, FT3, FT4 and Perioperative Changes in HR in Patients
There was no significant difference in the change of PR in different age, gender, blood lipid and BMI groups (p>0.05), as seen in Table 4. According to Table 4, there was no significant difference in the change of PR in ECG during the perioperative period between the two groups. The correlation analysis between the changes of perioperative TSH, FT3, FT4 and the changes of perioperative PR showed that there was a negative correlation with the changes of perioperative FT4 (r=-0.411, p=0.016), as shown in Table 5. There was no significant difference in the change of QRS in patients with different age, gender, blood lipid and BMI (p>0.05), as seen in Table 6. The correlation analysis between the changes of perioperative TSH, FT3, FT4 and the changes of perioperative QRS showed no correlation (p>0.05) as shown in Table 7.
| Variate | Group | PR change value | t/F | p |
|---|---|---|---|---|
| Age (year) | <55 | 0.01±0.01 | ||
| ≥55 | 0.01±0.01 | -1.551 | 0.131 | |
| Gender | Male | 0.01±0.01 | ||
| Female | 0.01±0.01 | -1.433 | 0.162 | |
| Serum lipid level | Normal | 0.01±0.01 | ||
| Increase | 0.01±0.01 | 1.227 | 0.211 | |
| BMI (kg/m2) | <22.9 | 0.01±0.02 | ||
| 22.9-28.5 | 0.01±0.01 | |||
| >28.5 | 0.01±0.01 | 0.783 | 0.466 |
Table 4: Comparison of Perioperative PR Changes in Patients with Different General Data Groups
| r | p | |
|---|---|---|
| TSH change value | 0.145 | 0.412 |
| FT3 change value | 0.072 | 0.685 |
| FT4 change value | -0.411 | 0.016 |
Table 5: Correlation Analysis between Changes in TSH, FT3, FT4 and Changes in PR during Perioperative Period in Patients
| Variate | Group | QRS change value | t/F | p |
|---|---|---|---|---|
| Age (year) | <55 | 0.00 (0.01) | ||
| ≥55 | 0.00 (0.01) | -0.059 | 0.953 | |
| Gender | Male | 0.00 (0.01) | ||
| Female | 0.00 (0.01) | -0.171 | 0.864 | |
| Serum lipid level | Normal | 0.00 (0.01) | ||
| Increase | 0.00 (0.01) | -0.632 | 0.534 | |
| BMI (kg/m2) | <22.9 | 0.00 (0.01) | ||
| 22.9-28.5 | 0.00 (0.01) | |||
| >28.5 | 0.00 (0.02) | 0.217 | 0.897 |
Table 6: Comparison of Perioperative QRS Changes in Patients with Different General Data Groups
| r | p | |
|---|---|---|
| TSH change value | -0.069 | 0.698 |
| FT3 change value | -0.242 | 0.168 |
| FT4 change value | 0.014 | 0.963 |
Table 7: Correlation Analysis of Perioperative TSH, FT3, FT4 Changes and Perioperative QRS Changes in Patients
There was no significant difference in QT change values between different age, gender, blood lipid and BMI groups (p>0.05) as shown in Table 8. There was no correlation between the changes of perioperative TSH, FT3, FT4 and the changes of perioperative QT (p>0.05) as shown in Table 9.
| Variate | Group | QT change value | t/F | p |
|---|---|---|---|---|
| Age (year) | <55 | 0.01 (0.03) | ||
| ≥55 | -0.01 (0.04) | -0.82 | 0.412 | |
| Gender | Male | -0.01 (0.07) | ||
| Female | 0.01 (0.03) | -2.212 | 0.027 | |
| Serum lipid level | Normal | 0.00 (0.04) | ||
| Increase | -0.03 (0.04) | -0.213 | 0.831 | |
| BMI (kg/m2) | <22.9 | 0.01 (0.04) | ||
| 22.9-28.5 | 0.01 (0.03) | |||
| >28.5 | 0.01 (0.05) | 3.821 | 0.148 |
Table 8: Comparison of Perioperative QT Changes in Patients with Different General Data Groups
| r | p | |
|---|---|---|
| TSH change value | 0.177 | 0.316 |
| FT3 change value | -0.025 | 0.887 |
| FT4 change value | -0.291 | 0.095 |
Table 9: Correlation Analysis between Perioperative Changes in TSH, FT3, FT4 and Perioperative Changes in QT in Patients
The changes of perioperative QTc in different age, gender, blood lipid and BMI groups were compared and the changes of perioperative QTc in different gender groups were statistically significant (t=- 2.212, p=0.027) as shown in Table 10. There was no correlation between the changes of perioperative TSH, FT3, FT4 and the changes of perioperative QTc (p>0.05) as shown in Table 11.
| Variate | Group | QTc change value | t/F | p |
|---|---|---|---|---|
| Age (year) | <55 | -0.01 (0.05) | ||
| ≥55 | 0.01 (0.04) | -0.059 | 0.953 | |
| Gender | Male | -0.01 (0.08) | ||
| Female | -0.01 (0.04) | -2.212 | 0.027 | |
| Serum lipid level | Normal | -0.01 (0.04) | ||
| Increase | -0.01 (0.05) | -0.632 | 0.534 | |
| BMI (kg/m2) | <22.9 | 0.00 (0.03) | ||
| 22.9-28.5 | 0.01 (0.04) | |||
| >28.5 | -0.02 (0.07) | 0.217 | 0.897 |
Table 10: Comparison of Perioperative QTC Changes in Patients with Different General Data Groups
| r | p | |
|---|---|---|
| TSH change value | 0.215 | 0.153 |
| FT3 change value | 0.246 | 0.16 |
| FT4 change value | -0.297 | 0.088 |
Table 11: Correlation Analysis between Perioperative Changes in TSH, FT3, FT4 and Perioperative Changes in QT in Patients
Thyroid is an important endocrine organ of the body, which regulates HR, blood pressure, body temperature and basal metabolism by secreting TH[6]. According to existing studies, TH can increase the activities of Sodium (Na+)-Potassium (K+)- Adenosine Triphosphatase (ATP) enzyme and Calcium ion (Ca+)-ATPase enzyme, accelerate the protein synthesis of cardiomyocytes, increase the contractility of cardiomyocytes, exert genomic and non-genomic effects on cardiomyocytes and is essential for normal cardiovascular function[7,8]. Serum TSH can also regulate cardiovascular function and normal structure by regulating the level of TH and other ways. Changes in TH levels in serum or tissues can directly cause changes in cardiovascular function. Many studies have shown that the risk of heart failure is significantly increased and the prognosis is poor when the level of serum TH is low[9,10]. In patients with thyroid cancer, especially after total thyroidectomy, the structure of the normal TH secreting glands is reduced, the compensatory role of the residual glands is limited and the levels of TH in the circulation are significantly reduced. Therefore, levothyroxine L-T4 is usually used for a long time to reduce the risk of recurrence and metastasis of thyroid cancer on the basis of supple mating the physiological requirements of TH and maintaining thyroid function. However, a large number of studies have shown that long-term TSH suppression therapy has corresponding side effects, mainly including heart complications and bone loss (osteoporosis). In this study, the serum FT3 and FT4 levels of all patients were decreased after surgery and the TSH level was increased significantly compared with that before surgery. Studies have shown that there may be a transient increase in TH levels in the circulation on the 1st d after surgery, mainly T4, which may be related to the release of a large amount of TH into the blood by squeezing the thyroid tissue during surgery[11]. With the consumption of TH, serum FT4 was gradually decreased, but the function of residual thyroid tissue in the hemi-resection group was gradually recovered and serum FT4 was gradually increased. Serum TSH is affected by the negative feedback regulation system, especially FT4, which is increased in the early postoperative period.
There were no significant changes in HR, QT interval, QTc duration and P wave before and after surgery, but PR interval and QRS duration were significantly shorter than those before surgery. The effect of TH on myocardial cells is similar to catecholamine, which has a sympathomimetic effect. Increase HR, enhance myocardial contractility and then increases cardiac output and cardiac work[12]. When the level of TH is decreased, the sensitivity of cardiomyocytes to catecholamine’s is decreased, which affects the normal physiological signal transduction of cardiomyocytes and reduces the excitability of sympathetic and parasympathetic nervous systems. P wave represents the atrial depolarization process, which is a commonly used noninvasive ECG indicator to predict paroxysmal atrial fibrillation. In patients with hyperthyroidism, P-wave prolongation has been confirmed to be an independent risk factor related to paroxysmal atrial fibrillation. P wave dispersion (Pdis) is the difference between P wave maximum duration (Pmax) and P wave minimum duration in 12-lead ECG. The increase of Pdis in patients with subclinical hyperthyroidism reflects the inhomogeneity of atrial repolarization, while the prolongation of Pmax indicates the presence of atrial conduction delay and abnormal atrial conduction. QT interval is the total duration of excitation and recovery of myocardial cells, but it mainly represents the repolarization process of myocardium, which is significantly affected by HR. Therefore, the QTc interval obtained by HR correction can better reflect the ventricular depolarization and repolarization process, which is usually calculated by Bazett’s square root formula (QTc=QT/RR1/2)[13]. QRS duration represents the time required for the activation process of ventricular muscle, the occurrence of structural changes and dysfunction of the left heart may be related to the prolonged QRS duration. PR interval was shortened after surgery, but it was in the normal range and no short PR interval was found. The PR interval in the ECG from the origin of the P wave to the origin of the QRS represents the conduction time from the atrium to the ventricular sinus node excitation, also known as the atrioventricular conduction time. The shortening of PR interval is related to the increase of sympathetic nerve tone. Although patients have a certain degree of decrease in TH levels after surgery, the stimulation of surgical procedures often increases the sympathetic nerve tone. Due to the short observation time, the effect of surgery cannot be completely excluded. In addition, some patients have postoperative tachycardia, but the HR returns to the normal range in the follow-up clinical observation, which can be considered as transient tachycardia. For elderly patients, surgery is also one of the reasons for their HR acceleration.
In this study, different age, sex, blood lipid level and BMI of patients, duration of QRS wave, QT interphase, QTc time and P wave duration had no obvious difference. Therefore, there were no significant changes of patients after PTC in ventricular depolarization time, total time of ventricular depolarization and repolarization, ventricular depolarization and repolarization time after HR correction and atrial depolarization time. There was no correlation between the changes of serum TSH, FT3 and FT4 and the changes of QRS, QT interval and QTc duration during the perioperative period, suggesting that the changes of serum TH levels during the perioperative period had relatively little effect on the changes of these electrocardiographic parameters. The perioperative change of FT3 was positively correlated with the perioperative change of HR and the change of FT4 was negatively correlated with the change of P wave duration and PR interval. Atrial fibrillation is the most common arrhythmia and also the most common arrhythmia in patients with hyperthyroidism besides sinus tachycardia. In this study, the effect of BMI on the change of HR was observed, but the changes of other ECG indexes were not observed. Obesity is a disease that may be associated with early abnormalities on ECG or echocardiography. Even without obvious clinical manifestations, obese patients may also present with abnormal T waves on ECG, left ventricular axis deviation and low QRS voltage. Severe obesity can also lead to changes in cardiac morphology, such as left atrial and left ventricular dilatation, left and right ventricular hypertrophy, which is high risk factor for ventricular arrhythmia and sudden death. The cardiac autonomic nervous regulation activity of obese patients is often abnormal, which affects the intra-atrial and atrial conduction time and increases the probability of atrial fibrillation.
Thyroid cancer is the only oncologic disease that includes age as a prognostic factor in the Tumor Size, Nodal and Metastatic (TNM) staging system. In the latest American Joint Committee on Cancer (AJCC) guidelines for thyroid cancer, the age at diagnosis of TNM staging system has been changed from 45 y old to 55 y old, which has better predictive value for mortality than before. In this study, in the process of analyzing the influencing factors of perioperative changes of various ECG indicators, it was found that age was the influencing factor for the difference in HR change and gender had a certain effect on the change of QTc during the perioperative period. However, there was no significant difference in the perioperative changes of other indicators. This may be related to the combined effect of variable factors and TH changes and the small sample size is also an important reason. A variety of reasons can affect surgical patients to have prolonged QTc interval, including advanced age, gender[14,15], abnormal blood electrolytes, antipsychotic drugs and some anesthetic drugs. The prolongation of the QTc interval is associated with the risk of cardiovascular mortality and acute coronary syndrome. Heart Rate Variability (HRV) obtained by holter monitoring can often reflect the individual cardiac autonomic nervous function and regulatory function and is also an important predictor of cardiovascular disease.
In conclusion, age, gender and BMI have a certain impact on the changes of perioperative ECG indicators and postoperative cardiac function monitoring should be strengthened in elderly and obese patients. The changes of TH levels are correlated with the changes of perioperative ECG indicators. In the process of postoperative TSH suppression therapy, it is necessary to establish a sex specific and age specific ECG standard for TH levels stratification, in order to more accurately evaluate the cardiac function of patients with DTC during TSH suppression therapy.
Conflict of interests:
The authors declared no conflict of interests.
References
- Derwahl M, Nicula D. Estrogen and its role in thyroid cancer. Endocr Relat Cancer 2014;21(5):T273-83.
[Crossref] [Google Scholar] [PubMed]
- Aschebrook-Kilfoy B, Grogan RH, Ward MH, Kaplan E, Devesa SS. Follicular thyroid cancer incidence patterns in the United States, 1980–2009. Thyroid 2013;23(8):1015-21.
[Crossref] [Google Scholar] [PubMed]
- Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R. Worldwide increasing incidence of thyroid cancer: Update on epidemiology and risk factors. J Cancer Epidemiol 2013;2013:965212.
[Crossref] [Google Scholar] [PubMed]
- Aschebrook-Kilfoy B, Ward MH, Sabra MM, Devesa SS. Thyroid cancer incidence patterns in the United States by histologic type, 1992–2006. Thyroid 2011;21(2):125-34.
[Crossref] [Google Scholar] [PubMed]
- Kilfoy BA, Zheng T, Holford TR, Han X, Ward MH, Sjodin A, et al. International patterns and trends in thyroid cancer incidence, 1973–2002. Cancer Causes Control 2009;20(5):525-31.
[Crossref] [Google Scholar] [PubMed]
- Simard EP, Ward EM, Siegel R, Jemal A. Cancers with increasing incidence trends in the United States: 1999 through 2008. CA Cancer J Clin 2012;62(2):118-28.
[Crossref] [Google Scholar] [PubMed]
- Moleti M, Sturniolo G, Di Mauro M, Russo M, Vermiglio F. Female reproductive factors and differentiated thyroid cancer. Front Endocrinol 2017;8:111.
- Midgley JE, Toft AD, Larisch R, Dietrich JW, Hoermann R. Time for a reassessment of the treatment of hypothyroidism. BMC Endocr Disord 2019;19(1):1-8.
[Crossref] [Google Scholar] [PubMed]
- FrancisGary L, WaguespackSteven G, BauerAndrew J, CeruttiJanete M, DinauerCatherine A, HayIan D, et al. Management guidelines for children with thyroid nodules and differentiated thyroid cancer. Thyroid 2015;25(7):716-59.
[Crossref] [Google Scholar] [PubMed]
- van der Spoel E, Roelfsema F, van Heemst D. Within-person variation in serum thyrotropin concentrations: Main sources, potential underlying biological mechanisms and clinical implications. Front Endocrinol 2021;12:619568.
[Crossref] [Google Scholar] [PubMed]
- Ward MH, Kilfoy BA, Weyer PJ, Anderson KE, Folsom AR, Cerhan JR. Nitrate intake and the risk of thyroid cancer and thyroid disease. Epidemiology 2010;21(3):389.
[Crossref] [Google Scholar] [PubMed]
- Schonfeld SJ, Ron E, Kitahara CM, Brenner A, Park Y, Sigurdson AJ, et al. Hormonal and reproductive factors and risk of postmenopausal thyroid cancer in the NIH-AARP diet and health study. Cancer Epidemiol 2011;35(6):e85-90.
[Crossref] [Google Scholar] [PubMed]
- Horn-Ross PL, Canchola AJ, Ma H, Reynolds P, Bernstein L. Hormonal factors and the risk of papillary thyroid cancer in the California teachers study cohort. Cancer Epidemiol Biomarkers Prev 2011;20(8):1751-9.
[Crossref] [Google Scholar] [PubMed]
- Braganza MZ, Berrington de González A, Schonfeld SJ, Wentzensen N, Brenner AV, Kitahara CM. Benign breast and gynecologic conditions, reproductive and hormonal factors, and risk of thyroid cancer benign breast and gynecologic conditions and thyroid cancer. Cancer Prev Res 2014;7(4):418-25.
[Crossref] [Google Scholar] [PubMed]
- Zamora-Ros R, Rinaldi S, Biessy C, Tjønneland A, Halkjaer J, Fournier A, et al. Reproductive and menstrual factors and risk of differentiated thyroid carcinoma: The EPIC study. Int J Cancer 2015;136(5):1218-27.
[Crossref] [Google Scholar] [PubMed]
 After
After
 After
After



