- *Corresponding Author:
- Xin Chu
Department of Cardiology, Taizhou people’s hospital, Taizhou, China
E-mail: chuuxinn@126.com
| This article was originally published in a special issue, “Clinical Research in Pharmaceutical and Biomedical Sciences” |
| Indian J Pharm Sci 2021:83(1)spl issue “154-161” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To observe the changes of neutrophil gelatinase associated apolipoprotein (neutrophil gelatinase associated lipocalin), lipoprotein associated phospholipase A2 and inflammatory cytokine hypersensitive C-reactive protein in patients with coronary heart disease and to explore the correlation between serum lipoproteinassociated phospholipase A2, neutrophil gelatinase associated lipocalin, hypersensitive C-reactive protein and the degree of coronary artery disease in patients with coronary heart disease. 200 inpatients in cardiovascular department of our hospital were divided into coronary heart disease group (n=153) and control group (n=47) according to coronary angiography. The serum levels of lipoprotein-associated phospholipase A2, neutrophil gelatinase associated lipocalin and hypersensitive C-reactive protein were measured. According to the Gensini score, the patients in the CHD group were divided into mild, moderate, severe and extremely severe groups. The changes of serum lipoprotein associated phospholipase A2, neutrophil gelatinase associated lipocalin and hypersensitive C-reactive protein was analyzed. At the same time, the relationship between the levels of serum lipoprotein associated phospholipase A2, neutrophil gelatinase associated lipocalin, hypersensitive C-reactive protein and the degree of coronary artery disease was discussed from the three aspects of coronary artery stenosis and Gensini score and the value of combined detection in the diagnosis of coronary heart disease. The serum levels of lipoprotein associated phospholipase A2 lipoprotein associated phospholipase A2 , neutrophil gelatinase-associated lipocalin, hypersensitive C-reactive protein and Gensini score in the coronary heart disease group were significantly higher than those in the control group (p<0.01). The serum levels of lipoprotein-associated phospholipase A2, neutrophil gelatinase associated lipocalin and hypersensitive C-reactive protein in extremely severe coronary artery disease group were significantly higher than those in moderate to severe disease group, mild disease group and control group (p<0.05) and those in severe disease group were significantly higher than those in mild and moderate disease group and control group (p<0.05). The area under the curve of combined detection of lipoprotein-associated phospholipase A2, neutrophil gelatinase associated lipocalin and hypersensitive C-reactive protein in the diagnosis of coronary heart disease reached 0.859. The serum levels of lipoprotein associated phospholipase A2, neutrophil gelatinase associated lipocalin and hypersensitive C-reactive protein are significantly increased in patients with coronary heart disease and are closely related to the severity of coronary artery disease, which can be used to evaluate the severity of coronary artery disease. The diagnostic rate of combined detection of serum lipoprotein associated phospholipase A2, neutrophil gelatinase associated lipocalin and hypersensitive C-reactive protein for coronary heart disease can reach 0.859, which can provide important clinical guidance value.
Keywords
Coronary heart disease, LP-PLA2, NGAL, Hs-CRP, gensini score, coronary artery stenosis.
Coronary atherosclerotic heart disease referred to as coronary heart disease (CHD), is a kind of myocardial dysfunction and/or organic lesion caused by coronary artery stenosis, occlusion, spasm and so on. With environmental pollution, changes in diet and many other reasons, CHD has become the most common type of cardiovascular disease, seriously endangering human health. According to the abstract report of China Cardiovascular Disease report 2016, the mortality rate of CHD has been increasing in recent 10 y, whether in urban areas with good material conditions or rural areas with poor basic conditions. Due to the increasing aging of Chinese residents, the number of deaths from CHD will continue to increase and has become the leading cause of death [1-3]. With the improvement of people’s material and economic living standards, some scholars have shown that the occurrence of CHD is gradually getting younger [4].
As a common cardiovascular disease, the occurrence and development of CHD are related to many factors, including dyslipidemia, hypertension, diabetes, smoking, metabolic syndrome and so on. Atherosclerosis, as the pathological basis of CHD, is affected by many factors. Abnormal lipid metabolism in blood and inflammatory reaction of vascular endothelium play an important role in the occurrence and development of atherosclerosis [5,6]. In recent years, more and more studies have shown that the occurrence of many acute coronary syndrome (ACS) is not only related to the degree of mechanical coronary artery stenosis, but also inflammation occurs in every stage of atherosclerosis and has been unanimously recognized by the academic community [7]. Normal endothelial cells maintain vascular homeostasis through tight junctions and play an anti-inflammatory role through synthesis and secretion. When endothelial cells are injured under the action of various influencing factors, endothelial cells are activated and secrete a large number of adhesion factors, resulting in leukocyte adhesion, resulting in vascular damage. Vascular endothelial inflammatory reaction and injury caused by various factors are not only the initial factors of atherosclerosis, but also play an important role in the development of atherosclerosis. At present, coronary angiography (CAG) is still used as the gold standard for the clinical diagnosis of CHD. This method is intuitive, invasive and costly. Current studies have shown that neovascularization, positive remodeling and severe endothelial dysfunction in atherosclerotic plaques are closely related to the vulnerability of atherosclerotic plaques, which is the result of the comprehensive action of multiple factors. Inflammatory factors have attracted much attention in this process. Nowadays, more and more scholars shift the research focus of early diagnosis of CHD to safer and faster hematological examination indicators.
In this study, the correlation between the levels of lipoprotein-associated phospholipase A2 (LP-PLA2), neutrophil gelatinase-associated lipocalin (NGAL) and hypersensitive C-reactive protein (Hs-CRP) alone and the combined detection of coronary artery disease and diagnosis was analyzed. This paper puts forward the value of combined detection of serum inflammatory markers in the diagnosis of coronary artery disease, and provides a more meaningful theoretical basis for clinic.
Materials and Methods
Subjects
All the subjects were from the Department of Cardiology, Taizhou people’s Hospital. The diagnosis and treatment time was from May 2019 to January 2021, including 153 patients with CHD. Another 47 patients with noncoronary heart disease were used as control.
Inclusion criteria: subjects were selected according to the diagnostic criteria of CHD issued by the American College of Cardiology (ACC) in 2009. The age ranged from 40 to 65 y old and CAG was performed strictly according to the indications of CAG. After successful puncture via femoral artery or radial artery, the catheter was sent to the ostium of coronary artery sinus and CAG was performed. All the imaging results were converted into imaging techniques. The whole operation of the experiment was performed by experienced doctors with cardiac catheterization qualification in the department of cardiology. The degree of coronary artery stenosis was judged by two experienced doctors by visual method, and the degree of coronary artery stenosis was determined according to the percentage of lumen diameter stenosis. Coronary artery stenosis ≥50 % of the left trunk, anterior descending branch, circumflex branch, right coronary artery or its main branches were regarded as diagnostic criteria for coronary heart disease; those who did not receive cardiac interventional therapy within 6 mo before admission; mentally sound persons with independent judgment; voluntarily participated in this study and signed informed consent.
Research exclusion criteria: there are cerebrovascular accidents in clinic, such as cerebral infarction and cerebral hemorrhage; patients with severe systemic immune diseases and impairment of liver and kidney function, patients with severe infection, latent hemorrhage and anemia; history of dementia, depression, Parkinson’s disease and osteoporosis. cardiogenic shock, pump grade III and IV, symptomatic heart failure, malignant arrhythmia, aortic dissection or aneurysm, stroke; malignant tumor, hematological disease; pulmonary heart disease, pulmonary embolism; hyperthyroidism and hypothyroidism, pheochromocytoma and primary aldosteronism; Patients with external thrombotic diseases of coronary artery, myocarditis, cardiomyopathy and other heart diseases.
Control group: Patients with no clinical symptoms of angina pectoris, no ischemic changes in electrocardiogram, normal cardiac function and normal results of coronary angiography.
Detection of serum LP-PLA2, NGAL and Hs-CRP
According to the selection and exclusion criteria, the appropriate subjects for clinical study were selected and the general data such as clinical history, sex, age, height, body mass index (BMI), smoking and hypertension (excluding secondary possibility) were collected. On the 2nd d after admission, fasting routine tests were performed on blood routine, liver, renal function, thyroid function and so on. At the same time, the levels of LP-PLA2, NGAL and Hs-CRP were detected in the morning of the 2nd d after admission. All the examination items were provided by the laboratory of our hospital.
Data processing of coronary arteriography
The results of coronary angiography in patients with CAG were scored by Gensini [8]. Gensini score can objectively and accurately reflect the severity of CHD coronary artery stenosis. Usually, the higher the Gensini score, the more serious the degree of coronary artery stenosis, indicating that CHD is more serious. Specific scoring rules: first, determine the basic score according to the degree of coronary artery stenosis: 1 point for stenosis diameter <25 %, 2 points for 25 % stenosis diameter, 2 points for 50 % stenosis diameter, 4 points for 50 % stenosis diameter, 8 points for 75 % stenosis diameter, 16 points for 90 % stenosis, 32 points for 100 %. Then the corresponding coefficients are determined according to the location of the stenosis (that is, the main branches of the coronary artery), which are: left main coronary artery (LM)×5 of the left trunk. The left anterior descending branch (LAD): proximal segment×2.5, middle segment×1.5, distal segment×1, diagonal branch lesion D1×1~(-1) D2×0.5, left circumflex branch (LCX): proximal segment×2.5, blunt marginal branch×1, distal segment×1, posterior descending branch×1, posterior descending branch×0.5, right coronary artery (RCA) and posterior descending branch×1. The basic score of each coronary artery stenosis is multiplied by the coefficient of the lesion site, that is the score of the diseased vessel and the sum of the score of each diseased vessel is the total score of the degree of coronary artery stenosis of the patient. According to the Gensini score of coronary artery disease, the coronary heart disease group was divided into four groups: mild, moderate, severe and extremely severe (see Table 1).
| Score | Degree of stenosis | Number of cases |
|---|---|---|
| Gensini score<20 points | Mild disease group | 39 |
| 20 points≤Gensini score<40 points | Moderate lesion group | 38 |
| 40 points≤Gensini score<100 points | Severe disease group | 43 |
| Gensini score≥100 points | Extremely severe disease group | 33 |
Table 1: Grouping According to Gensini Score
Statistical analysis
SPSS 26.0 software was used for statistical analysis.
The values of LP-PLA2, NGAL and Hs-CRP in serum were expressed by mean±standard deviation (x±s) and the sampling rate or constituent ratio of counting data was expressed. The average values of LP-PLA2, NGAL and Hs-CRP in each group were compared by t-test, rank sum test was used for data that did not obey normal distribution, chi-square test was used for non-econometric data and correlation analysis of metrological data and degree of coronary artery stenosis were used. All serum inflammatory factor data and combined with multiple data were calculated ROC curve, the use of binary logic regression statistical method to establish a model, through the area under the curve (AUC) to predict the accuracy of coronary heart disease. The difference was statistically significant (p<0.05).
Results and Discussion
There was no difference in age, sex, smoking history and family history of coronary heart disease among the control, mild, moderate, severe and extremely severe groups (p=NS). After admission, there was no significant difference in TG, TC, HDL-C and LDL-C among all groups. The history of hypertension and abnormal blood glucose in the CHD group was higher than that in the control group (paired 0.008, paired 0.021) and there was no difference among the CHD groups (p=NS). There was no significant difference in the proportion of β-blockers, calcium antagonists, nitrates and clopidogrel among the groups within one week before blood sampling (p=NS), (see Table 2).
| Groups | Control group (n=47) | Mild (n=39) | Moderate (n=38) | Heavy weight (n=43) | Extremely heavy (n=33) | p |
|---|---|---|---|---|---|---|
| Age (y) | 59.3±9.7 | 58.6±8.6 | 60.1±10.7 | 58.2±10.2 | 59.1±9.5 | NS |
| Male (%) | 76.2 | 78.1 | 77.9 | 76.9 | 79.1 | NS |
| Smokers (%) | 58.7 | 59.3 | 58.1 | 60.1 | 58.4 | NS |
| Patients with hypertension (%) | 47.4 | 52.1* | 51.6* | 53.2* | 57.7* | 0.008 |
| Abnormal blood glucose (%) | 42.5 | 47.5* | 53.1* | 54.7* | 55.2* | 0.021 |
| Family history of coronary heart disease (%) | 12.1 | 12.9 | 13.6 | 14.1 | 13.7 | NS |
| TG (mmol/1) | 1.52±0.65 | 1.73±1.02 | 1.69±0.87 | 1.79±0.93 | 1.78±0.89 | NS |
| TC (mmol/l) | 4.39±0.72 | 4.62±1.11 | 4.76±1.21 | 4.71±1.29 | 4.77±1.41 | NS |
| HDL-C (mmol/1) | 1.19±0.04 | 1.22±0.06 | 1.27±0.07 | 1.29±0.06 | 1.28±0.05 | NS |
| LDL-C (mmol/I) | 2.73±0.62 | 2.75±0.78 | 2.89±0.96 | 3.05±2.26 | 3.13±2.71 | NS |
| B-receptor blocker (%) | 81.7 | 83.6 | 84.9 | 90.4 | 90.4 | NS |
| Calcium antagonist (%) | 26.8 | 28.5 | 24.2 | 20.7 | 20.7 | NS |
| Clopidogrel (%) | 100 | 100 | 100 | 100 | 100 | NS |
| Nitrate esters (%) | 100 | 100 | 100 | 100 | 100 | NS |
Note: TG: triglyceride, TC: total cholesterol, HDL-C: high density lipoprotein cholesterol, LDL-C: low density lipoprotein cholesterol.
Table 2: Comparison of Clinical Data of Subjects in Each Group.
Comparison of serum LP-PLA2, NGAL, Hs-CRP levels and Gensini scores between the two groups. The serum levels of LP-PLA2, NGAL, Hs-CRP and Gensini score in the CHD group were significantly higher than those in the control group (p<0.01), as shown in Table 3.
| Project | Coronary heart disease group(n=153) | Control group(n=47) | T value |
|---|---|---|---|
| LP-PLA2(ng/L) | 263.19±20.25 | 16.89±2.81 | 14.245 |
| Hs-CRP(mg/L) | 8.95±3.31 | 1.32±1.02 | 15.585 |
| NGAL(pg/ml) | 128.49±9.93 | 43.68±7.32 | 12.362 |
| Gensin integral (points) | 69.69±25.23 | 5.76±3.02 | 13.481 |
Compared with the control group, p<0.01
Table 3: Comparison of Serum LP-PLA2, NGAL, HS-CRP Levels and Gensini Scores Between the Two Groups
Comparison of serum levels of LP-PLA2, NGAL and Hs-CRP in patients with coronary heart disease under different conditions of coronary artery stenosis. The serum levels of LP-PLA2, NGAL and Hs-CRP in the extremely severe coronary artery disease group were significantly higher than those in the moderate to severe disease group and mild disease group, while those in the moderate to severe disease group were significantly higher than those in the mild disease group and the control group (p<0.05) (Table 4).
| Coronary heart disease group (n=153) | ||||||
|---|---|---|---|---|---|---|
| Project | Mild (n=39) | Moderate (n=38) |
Heavy weight (n=43) | Extremely heavy (n=33) | Control group (n=47) |
F value |
| LP-PLA2(ng/L) | 197.65±30.52* | 236.67±36.79*# | 269.62±40.04*#Δ | 297.52±48.54*#Δ□ | 97.89±12.81 | 163.574 |
| Hs-CRP(mg/L) | 5.69±1.53* | 9.71±3.42*# | 10.28±4.07*#Δ | 13.28±5.75*#Δ□ | 2.45±1.04 | 131.260 |
| NGAL(pg/ml) | 64.09±11.19* | 99.51±22.87*# | 131.86±29.08*#Δ | 156.96±34.86*#Δ□ | 32.78±9.74 | 158.440 |
Note:Compared with the control group *p<0.01; with the mild disease group: #p<0.01; with the moderate disease group: p<0.01; with the severe disease group: p<0.01
Table 4: Comparison of Serum Levels of LP-PLA2, NGAL AND HS-CRP in Patients with Coronary Heart Disease Under Different Conditions of Coronary Artery Stenosis
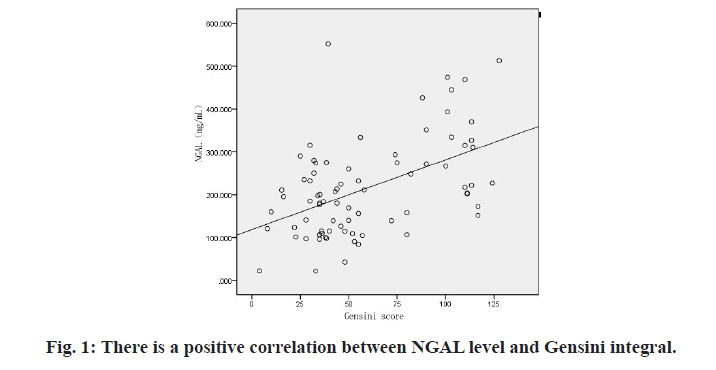
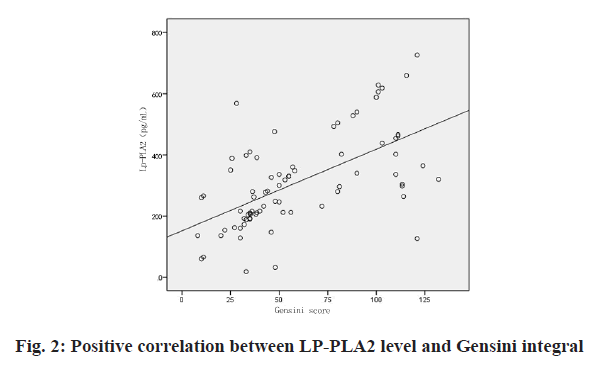
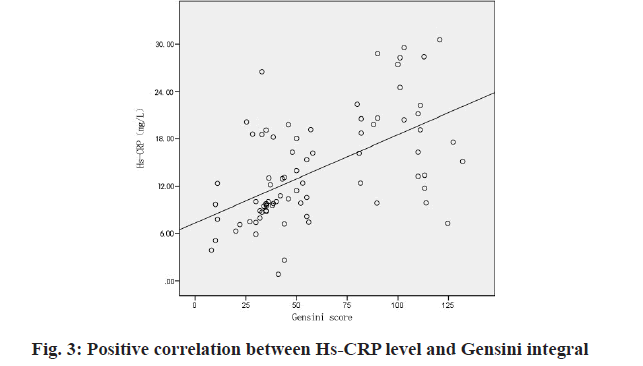
Correlation analysis between serum levels of LP-PLA2, NGAL, Hs-CRP and Gensini score in patients with coronary heart disease. There was a positive correlation between serum LP-PLA2, NGAL, Hs-CR and Gensini score in CHD group (regression coefficient r=0.639, 0.538, 0.559, p<0.01, p<0.01) (Table 5, fig. 1, fig. 2 & fig. 3).
| Project | Gensini score | |
|---|---|---|
| R value | P value | |
| LP-PLA2(ng/L) | 0.639 | <0.01 |
| Hs-CRP(mg/L) | 0.538 | <0.01 |
| NGAL(pg/ml) | 0.559 | <0.01 |
Note: p<0.01.There is a correlation between the index and Gensini
Table 5: Analysis of the Correlation Between Blood LP-PLA2, NGAL, HS-CRP Levels and Gensini Score in Patients with Coronary Heart Disease
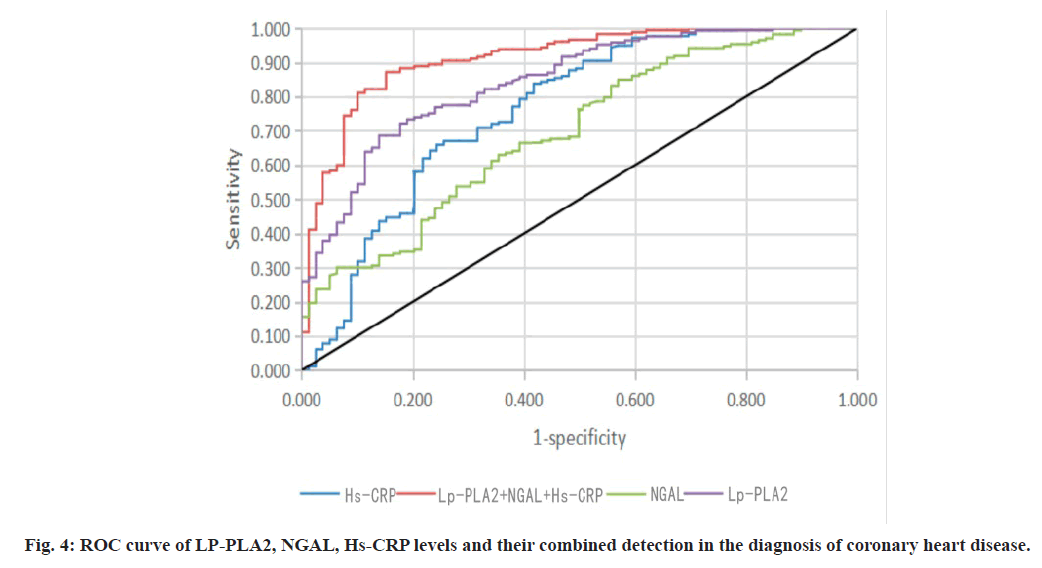
The diagnostic value of each variable in coronary heart disease was calculated by Logistic regression analysis. Univariate binary Logistic regression analysis showed that LP-PLA2, NGAL and Hs-CRP had certain significance in predicting coronary heart disease (see Table 6). All the test indexes were conditionally substituted into the equation for multivariate Logistic regression analysis, which only showed that IL-6 and NGAL had predictive value for coronary heart disease. If three indexes were introduced, the prediction accuracy would change, so we used the statistical method of binary logic regression to establish the model. Through the area under the curve (AUC) to predict the accuracy of coronary heart disease, the combined prediction accuracy of the three indicators is the highest, with an AUC of 0.859 (fig. 4, Table 7).
| Variable | OR | OR 95 % CI | p |
|---|---|---|---|
| LP-PLA2(ng/L) | 1.513 | 1.127-1.893 | 0.005 |
| Hs-CRP(mg/L) | 1.003 | 1.001-1.006 | 0.027 |
| NGAL(pg/ml) | 1.313 | 1.021-1. 696 | 0.023 |
Table 6: The Diagnostic Value of Each Variable Calculated by Logistic Regression Analysis for Coronary Heart Disease
| Project | Sensitivity % | Specificity % | Positive predictive value % | Negative predictive value % | AUC |
|---|---|---|---|---|---|
| LP-PLA2(ng/L) | 83.60 | 85.70 | 86.50 | 81.39 | 0.77 |
| Hs-CRP(mg/L) | 81.36 | 81.75 | 84.41 | 79.85 | 0.63 |
| NGAL(pg/ml) | 78.29 | 84.68 | 85.93 | 80.64 | 0.73 |
| LP-PLA2+Hs-CRP+NGAL | 85.72 | 87.68 | 87.15 | 83.86 | 0.859 |
AUC: Area under curve
Table 7: LP-PLA2, NGAL, HS-CRP Levels and Combined Detection in the Diagnosis of Coronary Heart Disease
Coronary atherosclerotic heart disease is a kind of myocardial dysfunction and/or organic lesion caused by coronary artery stenosis, obstruction, spasm and so on. In recent years, more and more studies have shown that the occurrence of many acute coronary syndrome is not only related to the degree of mechanical coronary artery stenosis. Inflammation occurs in every stage of atherosclerosis and has been unanimously recognized by the academic community [6]. At present, inflammation is considered to be involved in the pathogenesis of many cardiovascular diseases and is one of the important pathogenesis, especially in atherosclerotic diseases and the resulting cardiovascular events [9]. Inflammatory response is mainly through a series of inflammatory cells and inflammatory cytokines, especially monocyte macrophage chemokine (MCP), which promotes mononuclear macrophages from the blood into the arterial wall. When lipids are deposited in the intima of the artery, mononuclear macrophages enter the intima of the artery and phagocytize lipids to form foam cells through the action of their surface receptors, while the extracellular matrix proliferates to form a fibrous cap [10]. Under the action of inflammation, it causes a large number of platelet aggregation and acute thrombosis, which leads to the occurrence of acute coronary syndrome [11]. This study confirmed the relationship between inflammatory factors and coronary artery stenosis.
LP-PLA2 is a vascular specific marker synthesized and secreted by lymphocytes and mature macrophages. It can hydrolyze and oxidize lecithin under arterial intima by binding to low density lipoprotein, thus producing active pro-inflammatory factors, hemolytic lecithin and oxidizing fatty acids. Further enhance the phagocytosis of macrophages to form foam cells, while activated macrophages will produce more LPPLA2 and eventually form a vicious circle [12]. It can cause a large number of hydrolysates in the area where atherosclerosis occurs in blood vessels and then cause monocyte chemotaxis and damage endothelial function. It is a newly discovered inflammatory factor in recent years. It plays an important role in the development of atherosclerosis [13]. The prospective analysis of LPPLA2 by foreign Thompson [14] et al. showed that there was a positive correlation between the concentration of LP-PLA2 in vivo and the risk of coronary heart disease. With the continuous increase of serum LP-PLA2 level, the thickness of fibro lipid plaque fiber cap in patients with coronary heart disease decreased gradually [15]. This study confirmed that the correlation coefficient between LP-PLA2 and coronary artery stenosis was the highest under single factor.
Under normal circumstances, Hs-CRP exists in trace form in the serum of healthy people and the normal range of CRP in healthy adults without infection is generally below 2 mg/L. Therefore, the CRP detected by a highly sensitive method (which can detect the level of <0.3mg/L) is also called hs-CRP. Hs-CRP increased rapidly within 6 to 8 h of inflammatory injury, reached the peak at 48 to 72 h and the plasma half-life was about 19 h. Under the condition of health and stable disease, the plasma level remained basically unchanged. Because hs-CRP has the characteristics of repeatability, relatively stable blood concentration, sensitivity and easy detection, it has become the best index to reflect the inflammatory state in clinic [16-18]. The latest study shows that the expression of hs-CRP in serum of patients with CHD is significantly increased, and the expression of hs-CRP can significantly affect the progression of CHD. The up-regulation of hs-CRP mainly affects the spasm of coronary artery vessels and the deposition of subendothelial adipose tissue. In turn, it affects the stenosis of vascular lumen, leading to cardiomyocyte ischemia and the occurrence of CHD [19- 22]. In the process of increasing the number of coronary artery lesions, the expression of hs-CRP also increased significantly, suggesting that there may be a potential relationship between the expression of hs-CRP and the number of coronary artery lesions, mainly because the change of the expression concentration of hs-CRP can increase the risk of low density lipoprotein and triglyceride deposition, resulting in an increase in the risk of coronary artery branch occlusion in patients [23-25].
As a small molecular substance secreted after renal tubular injury, NGAL has become an important biological marker for prognosis and risk assessment of patients with acute renal injury and chronic nephropathy [26,27]. The widespread expression of NGAL and carotid unstable plaque are strong predictors of death and adverse cardiovascular events in patients with acute myocardial infarction [28]. Current studies have shown that patients with chronic nephropathy are often complicated with vascular calcification due to abnormal calcium and phosphorus metabolism, aggravating myocardial ischemia and promoting the progression of coronary artery disease. And patients with chronic vascular occlusion are often complicated with diabetes and chronic kidney disease. At present, it has been found that there are significant differences in the level of NGAL in patients with different number of diseased coronary arteries. Some studies have found that serum NGAL in patients with CHD is related to the severity of coronary artery disease and is an independent risk factor for complex coronary artery disease [29,30]. This study confirmed that NGAL is associated with coronary artery stenosis.
This study confirmed that the serum levels of LPPLA2, NGAL and Hs-CRP were significantly increased in patients with coronary heart disease and were closely related to the severity of coronary artery disease, which could be used to evaluate the severity of coronary artery disease. The diagnostic rate of combined detection of serum LP-PLA2, NGAL and Hs-CRP for coronary heart disease can reach 0.859, which can provide important clinical guidance value.
Funding
This work is supported by the Scientific Research Foundation of Taizhou People’s Hospital (No. ZL201901).
Conflict of interests
The authors declared no conflicts of interest.
References
- Abd El-Aziz TA, Mohamed RH. Human C-reactive protein gene polymorphism and metabolic syndrome are associated with premature coronary artery disease. Gene 2013;532(2):216-21.
- Allen RA, Lee EM, Roberts DH, Park BK, Pirmohamed M. Polymorphisms in the TNF‐α and TNF‐receptor genes in patients with coronary artery disease. Eur J Clin Invest 2001;31(10):843-51.
- Che J, Li G, Shao Y, Niu H, Shi Y. An analysis of the risk factors for premature coronary artery disease in young and middle-age Chinese patients with hypertension. Exp Clin Cardiol 2013;18(2):89-92.
- Amara A, Mrad M, Sayeh A, Lahideb D, Layouni S, Haggui A, et al. The effect of ACE I/D polymorphisms alone and with concomitant risk factors on coronary artery disease. Clin Appl Thromb 2018;24(1):157-63.
- Balistreri CR, Vasto S, Listi F, Grimaldi MP, Lio D, COLONNA‐ROMANO GI, et al. Association between+1059G/C CRP polymorphism and acute myocardial infarction in a cohort of patients from Sicily: a pilot study. Ann N Y Acad Sci 2006;1067(1):276-81.
- Ben-Hadj-Khalifa S, Ghazouani L, Abboud N, Ben-Khalfallah A, Annabi F, Addad F, et al. Functional interleukin-10 promoter variants in coronary artery disease patients in Tunisia. Eur Cytokine Netw 2010;21(2):136-41.
- Myers GL , Rifai N, Tracy RP, Roberts WL, Alexander RW, Biasucci ML, et al. CDC/AHA Workshop on Markers of Inflammation and Cardiovascular Disease: Application to Clinical and Public Health Practice: Report From the Laboratory Science Discussion Group. Circulation 2004;110(25):e545-9.
- Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J cardiol 1983;51:606-10.
- Grira N, Lahidheb D, Lamine O, Ayoub M, Wassaifi S, Aouni Z, et al. The Association of IL-6, TNFα and CRP Gene Polymorphisms with Coronary Artery Disease in a Tunisian Population: A Case–Control study. Biochem Genet 2021:1-6.
- Brown JC, Gerhardt TE, Kwon E. Risk factors for coronary artery disease. StatPearls 2020.
- Karolczak K, Kamysz W, Karafova A, Drzewoski J, Watala C. Homocysteine is a novel risk factor for suboptimal response of blood platelets to acetylsalicylic acid in coronary artery disease: a randomized multicenter study. Pharmacol Res 2013;74:7-22.
- Naureen A, Munazza B, Shaheen R, Khan SA, Fatima F. Serum homocysteine as a risk factor for coronary heart disease. J Ayub Med Coll Abbottabad 2012;24(1):59-62.
- Zhang YY, Li X, Lin WH, Liu JJ, Jing R, Lu YJ, et al. Relationship between epicardial adipose tissue and clinical prognosis of patients with coronary heart disease after percutaneous coronary intervention. Chin Med J 2018;98(3):208-12.
- Chu H, Yang J, Mi S, Bhuyan SS, Li J, Zhong L, et al. Tumor necrosis factor-alpha G-308 A polymorphism and risk of coronary heart disease and myocardial infarction: a case–control study and meta-analysis. J Cardiovasc Dis Res 2012;3(2):84-90.
- Çoker A, Arman A, Soylu O, Tezel T, Yildirim A. Lack of association between IL‐1 and IL‐6 gene polymorphisms and myocardial infarction in Turkish population. Int J Immunogenet 2011;38(3):201-8.
- Elahi MM, Gilmour A, Matata BM, Mastana SS. A variant of position−308 of the Tumour necrosis factor alpha gene promoter and the risk of coronary heart disease. Heart Lung Circ 2008;17(1):14-8.
- Thompson A, Gao P, Orfei L, Watson S, Di EA, Kaptoge S, et al. Lipoprotein-associated phospholipase A (2) and risk of coronary disease, stroke, and mortality: collaborative analysis of 32 prospective studies. Lancet 2010;375(9725):1536-44.
- Galimudi RK, Spurthi MK, Padala C, Kumar KG, Mudigonda S, Reddy SG, et al. Interleukin 6 (-174G/C) variant and its circulating levels in coronary artery disease patients and their first degree relatives. Inflammation. 2014;37(2):314-21.
- Ghazouani L, Khalifa SB, Abboud N, Hamda KB, Khalfallah AB, Brahim N, et al. TNF-α− 308G> A and IL-6− 174G> C polymorphisms in Tunisian patients with coronary artery disease. Clin Biochem 2010;43(13-14):1085-9.
- Li X, Guo D, Zhou H, Hu Y, Fang X, Chen Y. Pro-inflammatory Mediators and Oxidative Stress: Therapeutic Markers for Recurrent Angina Pectoris after Coronary Artery Stenting in Elderly Patients. Curr Vasc Pharmacol 2021.
- Hernández-Díaz Y, Tovilla-Zárate CA, Juárez-Rojop I, López-Narváez ML, Álvarez-Cámara JF, González-Castro TB. Association between CRP and TNF-α genes variants and cardiovascular heart disease in a Mexican population: protocol for a case-control study. Int J Environ Res Public Health 2016;13(1):103.
- Hua L, Yuan JX, He S, Zhao CH, Jia QW, Zhang J, et al. Analysis on the polymorphisms of site RS4977574, and RS1333045 in region 9p21 and the susceptibility of coronary heart disease in Chinese population. BMC Med Genet 2020;21(1):1-2.
- Latheef K, Rajasekhar D, Vanajakshamma V, Aparna BR, Chaudhury A, Sarma PV. Association of MTHFR, IL-6 and ICAM-1 gene polymorphisms with coronary artery disease in south-Indian ethnic subset: a case-control study. J Cardiovasc Dis Res 2018;9(3):115-22.
- Li CS, Guo BR, Zeng GU, Jing YA, Zheng HF, Wang AL. Association between C-reactive protein gene+1059 G/C polymorphism and the risk of coronary heart disease: a meta-analysis. Chin Med J 2013;126:4780-5
- Phulukdaree A, Khan S, Ramkaran P, Govender R, Moodley D, Chuturgoon AA. The interleukin-6−147 G/C polymorphism is associated with increased risk of coronary artery disease in young south african indian men. Metab Syndr Relat Disord 2013;11(3):205-9.
- Srikanth Babu BMV, Pulla Reddy B, Priya VHS, Munshi A, Surekha Rani H, Suman Latha G, et al. Cytokine gene polymorphisms in the susceptibility to acute coronary syndrome. Genet Test Mol Biomark 2012;16:359-365.
- Bolignano D, Coppolino G, Lacquaniti A, Buemi M. From kidney to cardiovascular diseases: NGAL as a biomarker beyond the confines of nephrology. Eur J Clin Invest 2010;40(3):273-6.
- te Boekhorst BC, Bovens SM, Hellings WE, van der Kraak PH, van de Kolk KW, Vink A, et al. Molecular MRI of murine atherosclerotic plaque targeting NGAL: a protein associated with unstable human plaque characteristics. Cardiovasc Res 2011;89(3):680-8.
- Katagiri M, Takahashi M, Doi K, Myojo M, Kiyosue A, Ando J, et al. Serum neutrophil gelatinase-associated lipocalin concentration reflects severity of coronary artery disease in patients without heart failure and chronic kidney disease. Heart Vessels 2016;31(10):1595-602.
- Zhang P, Wu X, Li G, He Q, Dai H, Ai C, et al. Tumor necrosis factor-alpha gene polymorphisms and susceptibility to ischemic heart disease: A systematic review and meta-analysis. Medicine 2017;96(14):e6569.