- *Corresponding Author:
- Z. K. Li
Department of Ultrasound,
Affiliated Hospital of North Sichuan Medical College,
Nanchong,
Sichuan 637000,
China
E-mail: tsh1234562021@126.com
| This article was originally published in a special issue, “Trending Topics in Biomedical Research and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2022:84(1) Spl Issue “146-155” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the effect and value of thyroid stimulating hormone and thyroglobulin ratio, B-ultrasound and emission computed tomography imaging in the preoperative differentiation of benign and malignant thyroid nodules. 272 patients who underwent thyroid nodule surgery were divided into benign group and malignant group, and the diagnostic performance of a single index in the differentiation of benign and malignant thyroid nodules was analyzed. The levels of thyroid stimulating hormone, thyroglobulin antibody and thyroid imaging reporting and data system in malignant group were higher than those in benign group and the thyroglobulin level in benign group was higher than that in malignant group (p<0.05). Thyroid imaging reporting and data system has a larger area under the receiver operating characteristic curve in the differentiation of benign and malignant thyroid nodules. In thyroglobulin antibody negative group, the thyroid stimulating hormone/thyroglobulin ratio of benign patients was lower than that of malignant patients (p<0.05). Meanwhile, receiver operating characteristic curve reflected that thyroid stimulating hormone/ thyroglobulin ratio had certain diagnostic performance. In the large nodule group, the Y value under the multiple regression models had a larger area under the line and the area under the line of thyroid emission computed tomography imaging was the smallest. In the small nodule group, the Y value was higher than other detection methods, which was 0.794. The accuracy of thyroid stimulating hormone and thyroglobulin ratio, B-ultrasound and emission computed tomography imaging in the differentiation of benign and malignant thyroid nodules was more than 98 %. The combination of thyroid stimulating hormone and thyroglobulin ratio, B-ultrasound and emission computed tomography imaging is effective and has great advantages in the differentiation of benign and malignant thyroid nodules before operation.
Keywords
Thyroid stimulating hormone, thyroglobulin, B-ultrasound, emission computed tomography imaging, thyroid nodules
In recent years, the incidence of thyroid cancer in China is rising and has gradually become the main high-risk tumor endangering people’s health. Thyroid cancer has no specific clinical manifestations, but according to relevant studies, thyroid cancer may be indirectly caused by bad living habits. With China’s economic development and social pressure, people’s psychological tolerance decreases, which further increases the incidence of thyroid cancer[1-3]. In medical practice, it is still considered that early detection and diagnosis is the key to improve the survival rate of malignant tumors. However, in terms of thyroid, it has similar clinical manifestations to benign diseases such as thyroiditis before operation. Thyroid cancer comes from the gradual lesion of thyroid nodules and the preoperative identification of thyroid nodules has become the means for the preliminary diagnosis of thyroid cancer[4-6].
In the identification of benign and malignant thyroid nodules, there are three methods in medical practice, including imaging detection, serum detection and pathological feature detection. In the long-term development of medical technology, imaging has developed rapidly, so it is gradually widely used in the detection of benign and malignant thyroid nodules. However, it is undeniable that the characteristics of benign and malignant thyroid nodules in the image still have fuzzy points, that is, imaging performs well in the display of nodule size, and various indicators need to be relied on for benign and malignant thyroid nodules[7-9]. In order to distinguish benign and malignant thyroid nodules more clearly, Thyroid Stimulating Hormone (TSH) and Thyroglobulin (Tg) ratio, B-ultrasound and Emission Computed Tomography (ECT) imaging were combined in the study. According to the benign and malignant groups of thyroid nodules, the differences of various indicators in the groups were analyzed and the application effect of the combination method in the differentiation was analyzed, so as to improve the ability of distinguishing benign and malignant thyroid nodules in clinic.
Materials and Methods
General information:
272 patients who underwent thyroid nodule surgery in our hospital from June 2018 to January 2020 were selected, including 115 patients with thyroid cancer, all of whom were papillary cancer and 157 patients with benign thyroid nodules. Based on this, the patients were divided into benign group and malignant group (Table 1).
| Index | Benign group | Malignant group | t/c2 | p |
|---|---|---|---|---|
| Age (years) | 51.01±11.23 | 49.87±11.45 | 8.121 | 0.187 |
| Gender | ||||
| Male | 28 | 19 | 0.523 | 0.401 |
| Female | 129 | 96 | ||
| Height (m) | 1.69±0.293 | 1.68±0.296 | 1.231 | 0.579 |
| Weight (kg) | 62.31±8.01 | 62.54±8.07 | 0.564 | 0.611 |
| Degree of education | ||||
| High | 90 | 73 | 12.334 | 0.272 |
| Low | 67 | 42 |
Table 1: General Information of Patients
The inclusion criteria in this study includes patients who underwent thyroid nodule surgery in our hospital and were diagnosed with thyroid cancer and benign thyroid nodule; the clinical data of all patients were perfect; the nutritional status of the patients was good; all patients had no history of alcoholism and smoking; the function of liver and kidney was normal; the patient was over 18 y old. Exclusion criteria include thyroid peroxidase antibody and thyroid stimulating receptor antibody were positive; family history of thyroid diseases; neck trauma; the patient has a history of other tumors and related chronic diseases; the patient had contraindications to Computed Tomography (CT) examination. All patients understood the contents and steps of the experiment and signed the informed consent. The experiment was approved by the ethics committee of our hospital.
Experimental methods and evaluation methods:
Grouping and experimental methods: The patients were divided into benign group and malignant group. The Receiver Operating Characteristic (ROC) curves of TSH, Tg and B-ultrasound grading of the two groups were drawn, and the similarities and differences of each index result between the two groups were compared from the change trend of ROC curve. In addition, the patients were divided into groups according to the negative and positive differences of Thyroglobulin Antibody (TgAb), and the benign and malignant members in the group were analyzed and compared. Using the results obtained, the best diagnostic combination mode is constructed and its ROC curve is drawn to compare the area under the curve and diagnostic performance between the combination mode and the single use mode[10-12].
In the negative results of TgAb, the patients were divided into large nodule group and small nodule group according to the size of thyroid nodules and the benign and malignant patients with thyroid nodules were analyzed. Similarly, the best combination scheme is compared with a single scheme and the area under the curve and diagnostic performance are compared from the drawn ROC curve.
The patient’s thyroid ECT imaging was performed by GE Infinia Hawkeye 4 dual probe Single Photon Emission Computed Tomography (SPECT)/CT instrument in the United States. Technetium (99TcmO4?) was used as the imaging agent for ECT imaging. The imaging agent was injected intravenously during the imaging process and the image was collected 30 min later. The images were read and signed by two doctors independently at the same time.
The thyroid B-ultrasound adopts Philips ie33 color ultrasound detector to classify the nodules according to the Thyroid Imaging Reporting Data System (TIRADS). The image data are independently read by two experienced doctors at the same time for nodule classification and issued at the same time.
Detection and evaluation methods: The grading standard of thyroid nodules under B-ultrasound image is as follows. There is no nodule under the image, the thyroid performance is normal and it is evaluated as class 0; it is suggested that benign lesions, without nodules and calcification are evaluated as class 2; thyroid nodules with clear edges, calcification and uneven echo were evaluated as class 3; the possible malignant lesions were evaluated as 4 categories.
It is highly suggested that the possibility of malignant lesions is more than 95 %, which is evaluated as category 5; 100 % were determined as malignant, that is, thyroid cancer was diagnosed and evaluated as category 6. In order to facilitate the use of indicators, the results of thyroid color Doppler ultrasound were graded according to TI-RADS. The grading standard was: Grade 3 and below, 4a, 4b, 4c and grade 5 were divided into 0~4 points. The index score is based on the diagnostic cut-off value in the ROC curve. If it is greater than the cut-off value, it is recorded as 1 point and if it is less than the cut-off value, it is recorded as 0 point[13-15].
The detection of markers in serum shall be carried out 12 h after fasting. The elbow vein blood of fasting patients shall be taken and the serum sample shall be centrifuged for 10 min under the setting of 3000 revolutions on the centrifuge. The centrifuged serum shall be tested on the computer and the above operations shall be completed within 4 h. At the same time, the patient shall not use drugs before serum testing.
The evaluation method of patient’s nodule size is that TgAb negative patients are divided into large nodules and small nodules according to the size of thyroid nodules. Those with thyroid nodule size of 1 cm or more are rated as large nodules and those less than 1 cm is rated as small nodules.
Observation indicators:
The serum of patients was collected and the levels of TSH, Tg and TgAbs were observed by chemiluminescence method. The normal level range of TSH is 0.15~5.5 mIU/l and the normal level range of Tg is 2.5~7.7 μg/l, the normal range of TgAb level is 0~0.9 IU/ml.
Statistical analysis:
Statistical Package for the Social Sciences (SPSS) 22.0 software is used for statistical analysis of the collected data. The measurement data of normal distribution is represented by mean±Standard Deviation (SD) (x?±s) and the test method is t-test. The measurement data of non-normal distribution is represented by median and the test method is Wilcoxon rank sum test. The counting data were expressed by cases or rates and the comparison between groups was used χ2 inspection, indexes the detection of thyroid nodules was compared by ROC curve and the best critical value in index prediction was determined by Youden index. Multiple logistic regression model was used to calculate the combined detection effect between multiple indicators and Y value was used to represent the combined results. p<0.05 showed that the data difference was statistically significant.
Results and Discussion
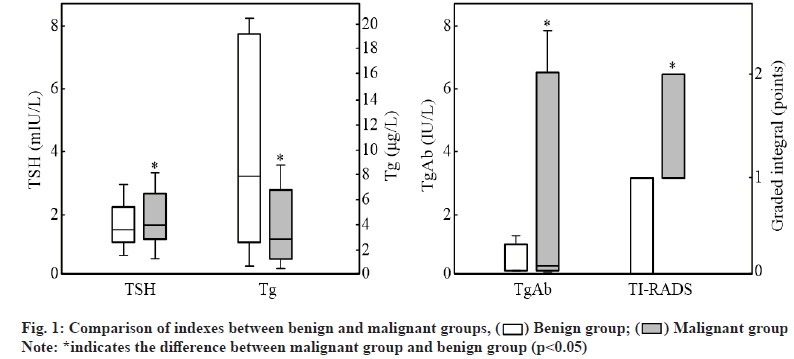
Patients with benign and malignant thyroid nodules were compared. Fig. 1 shows the rank sum test results of various test indexes between benign and malignant patient groups. The figure shows that the TSH and TgAb levels of patients in malignant group and the scores in TI-RADS grading evaluation are higher than the corresponding index levels and scores of benign group, while the Tg level of patients in benign group is higher than that of patients in malignant group. The test shows that the differences are statistically significant (p<0.05).
Fig. 2 shows the ROC curve comparison among various items. Since the area under the curve of Tg in the ROC curve is less than 0.5, the Tg curve does not participate in the comparison. The curve shows that the area under the curve of TSH is the smallest, 0.593, followed by TgAb and the area under the curve is 0.636. The area under the curve of TI-RADS is the largest, reaching Comparison within TgAb negative group is shown here. Fig. 3 shows the comparison of TSH/Tg ratio between benign and malignant thyroid nodules in the TgAb negative group. The figure shows that there are 130 benign patients, the TSH/Tg ratio is 229.40 (54.9, 1671.04) and 86 malignant patients and the TSH/Tg ratio is 388.67 (207.82, 1109.37), there was significant difference in the ratio between benign and malignant patients in the group (Z=-3.624, p<0.05).
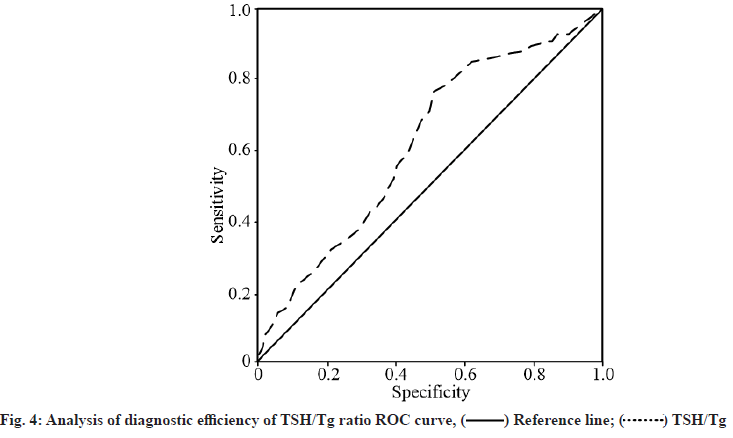
The predicted ROC curve of TSH/Tg ratio for thyroid nodules is shown in fig. 4. The figure shows that the diagnostic cut-off value of TSH/Tg ratio for differentiating benign and malignant thyroid nodules is 178.92 IU/g, and the area under the ROC curve of TSH/ Tg ratio is 0.671.
Fig. 5 shows the ROC curve after the thyroid nodules of patients in the TgAb negative group are divided into large nodule group and small nodule group. In the large nodule group, the combined ROC curve between TSH/ Tg ratio, B-ultrasound score and ECT imaging score and Y value are drawn by using multiple logistic regression model as shown in fig. 5 (a). As can be seen from fig. 5 (a), the largest area under the curve in the thyroid macronodule group is the Y value, which reaches 0.872 and the smallest is the thyroid ECT imaging score, which is 0.547.
In addition, the TSH/Tg ratio and the area under the curve of B-ultrasound integral was 0.657 and 0.721 respectively. The test results showed that (Z=2.094, p<0.05). Fig. 5 (b) shows the drawing of ROC curve of each index in thyroid small nodule group. Similarly, it can be found that the area under the curve of Y value reaches 0.794, followed by B-ultrasound integral, the area under the curve reaches 0.693 and the area under the curve of TSH/Tg ratio is 0.684.
Table 2 shows the comparison results of diagnostic performance evaluation between large nodules and small nodules in TgAb negative group. The table shows that for the benign and malignant diagnosis of patients with large nodules, the sensitivity and specificity of Y value are higher than the other three indicators, and the difference is statistically significant. In addition, the comprehensive diagnostic coincidence rate of Y value reaches 87.26 %, which is significantly higher than the single diagnostic coincidence rate of TSH/Tg ratio, B-ultrasound score and ECT imaging score and the difference is statistically significant. In the small nodule group, for the differentiation of benign and malignant, the highest sensitivity is TSH/Tg ratio, which reaches 96.61 %, followed by B-ultrasound score. However, in the new evaluation of characteristics, TSH/Tg ratio and B-ultrasound score are less than 50 %, the sensitivity of Y value is 81.32 %, and the specificity is 73.97 %. In the comparison of diagnostic coincidence rate, the diagnostic efficiency of Y value reaches 77.11 %. It was significantly higher than the diagnostic coincidence rate of TSH/Tg ratio and B-ultrasound score and the difference was statistically significant.
| Index | Susceptibility (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) | Diagnostic coincidence rate (%) | |
|---|---|---|---|---|---|---|
| Large nodule group | TSH/Tg | 73.01 | 56.39 | 37.96 | 85.29 | 61.05 |
| B-ultrasound integral | 61.52 | 81.64 | 55.18 | 85.61 | 76.21 | |
| ECT imaging integral | 42.18 | 68.42 | 32.54 | 76.42 | 61.33 | |
| Y value | 92.26* | 84.23* | 68.77* | 96.87* | 87.26* | |
| Small nodule group | TSH/Tg | 96.61 | 44.83 | 65.07 | 92.85 | 70.87 |
| B-ultrasound integral | 84.45 | 44.83 | 60.96 | 74.56 | 64.52 | |
| Y value | 81.32 | 73.97* | 75.01 | 80.01 | 77.11* | |
Note: *indicates p<0.05 compared with other indexes
Table 2: Analysis of Diagnostic Performance of Large and Small Nodules In Negative Group
Comparison within TgAb positive group is shown here. Fig. 6 shows the ROC curve drawn after the comparison of diagnostic indexes of benign and malignant patients in the TgAb positive group. From the curve comparison in the figure, the largest area under the curve is the joint detection Y value calculated by multiple regression, which reaches 0.754, followed by the area under the curve of TSH index, which is 0.729 and the smallest is the area under the line of B-ultrasound score, which is only 0.525.
The diagnostic performance of each index is compared and the results are shown in Table 3. Table 3 shows that in the comparison of TSH, B-ultrasound score and Y value, the sensitivity and specificity of TSH score are the lowest. The sensitivity and specificity between B-ultrasound score and Y value are the same, reaching 91.30 % and 55.00 % respectively. The finally calculated diagnostic coincidence rate also reaches 77.82 %.
| Index | Susceptibility (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) | Diagnostic coincidence rate (%) |
|---|---|---|---|---|---|
| TSH/Tg | 70.57 | 35.00 | 64.82 | 41.11 | 56.85 |
| B-ultrasound integral | 91.30 | 55.00 | 76.48 | 77.92 | 77.82 |
| Y value | 91.30 | 55.00 | 76.48 | 77.92 | 77.82 |
Table 3: Analysis of Diagnostic Performance of Benign and Malignant Thyroid Nodules In Positive Group
Effect of combined diagnosis in subsequent experiments is discussed here. Through the analysis of the diagnostic performance of combined diagnosis in the differentiation of benign and malignant thyroid nodules, the thyroid and breast surgical patients in our hospital from May 2020 to September 2020 were identified and 30 patients were randomly selected to draw the graph, as shown in fig. 7. The benign and malignant thyroid nodules were graded and the differential effect of combined Tg, TSH, B-ultrasound and ECT imaging was evaluated according to the judgment of doctors on the benign and malignant thyroid nodules. Fig. 7 shows that there is little difference between the overall results of 30 patients under the combined identification method and the doctor’s diagnosis results. Among them, there is a large difference between the combined identification and the doctor’s diagnosis four times in the first 3 mo, because the preliminary use of combined identification is not skilled. With the increase of use time, there was only a large difference between the identification results of combined use and doctor’s diagnosis in the next 2 mo. In addition, from the results of 5 mo consultation, the overall similarity between combined identification and physician diagnosis reached more than 98 %.
Thyroid cancer is one of the most rapidly rising malignant tumors. It has developed into the most common malignancy in China’s female population after breast cancer. Thyroid cancer has also developed into the eighth largest cancer in China. The occurrence of thyroid cancer comes from the gradual malignant lesions of thyroid nodules. Therefore, in order to reduce the incidence of thyroid cancer, the primary task is to start with the diagnosis and treatment of thyroid nodules. According to relevant investigations, thyroid diagnosis has been determined as a routine physical examination item by more and more health institutions and with the gradual development of B-ultrasound technology, the diagnosis rate of thyroid nodules is also increasing. However, with the increase of the diagnosis rate of thyroid nodules, it leads to the over treatment of thyroid nodules, which is mainly caused by the wrong judgment of benign and malignant thyroid nodules in a large number of diagnoses[16-18]. Preoperative benign and malignant thyroid nodules is the key step to determine the follow-up treatment plan of patients, so accurate judgment of preoperative benign and malignant thyroid nodules can ensure the normal diagnosis and treatment. In a large number of studies and medical practice, it has been repeatedly emphasized that the preoperative identification of benign and malignant thyroid nodules can help doctors make surgical decisions. Therefore, the preoperative identification of thyroid nodules has risen to a very important position[19]. At present, the identification methods of thyroid nodules are mainly divided into imaging methods, pathological methods and serum detection. In terms of detection effect, the single imaging method lacks certain index support and the same pathology and serum detection also lack the support of the current situation of thyroid performance in the image[20]. Therefore, this study will combine TG, TSH, B-ultrasound and ECT imaging for combined detection and analyze the combined effect, so as to provide theoretical support for the clinical diagnosis of benign and malignant thyroid nodules.
The results showed that the levels of TSH, TgAb and TI-RADS in benign patients were lower than those in malignant patients and the level of Tg was higher than that in benign patients. From the above results, it can be preliminarily seen that the benign and malignant thyroid nodules can be reflected in the differences in the grading evaluation of Tg, TSH, TgAb and TIRADS. The effect of each index in the differentiation of benign and malignant thyroid nodules can be further analyzed through ROC curve. The curve results show that TI-RADS classification has the best diagnostic performance, while Tg has the worst single diagnostic performance. From the above results, it can be seen that the benign and malignant thyroid nodules are actually manifested in the differences of Tg, TSH, TgAb and TIRADS grades and can also be diagnosed by a single index in the diagnosis. However, some studies have pointed out that a single index will still make serious mistakes in diagnosis, so relevant joint detection schemes have been proposed[21].
In order to analyze the diagnostic effect of combined detection, TgAb yin and yang were grouped, and the benign and malignant subgroups of patients with thyroid nodules were analyzed. In the TgAb negative group, first analyze the application effect of TSH/Tg ratio. There is a difference in TSH/Tg ratio between benign and malignant patients in the group and the ratio of malignant patients is significantly greater than that of benign patients. The test results show that the difference is statistically significant. Drawing the ROC curve of patients, it is found that the area under the curve of TSH/Tg ratio is significantly better than that under the application of TSH and Tg alone, indicating that the combination of the two has improved the diagnostic performance of benign and malignant thyroid nodules. In addition, according to the nodule size of patients in TgAb negative group, they were divided into large nodule group and small nodule group. The scheme was calculated by multiple logistic regression model. The combined scheme was compared with TSH/Tg ratio, B-ultrasound score and ECT imaging score. The results showed that in the large nodule group, the Y value after combined use had the largest offline area and there was a significant difference with other identification schemes. The test showed that the difference was statistically significant. In the small nodule group, it also showed that the Y value after combined use had the largest offline area. The above results show that the combined detection of the two schemes can significantly improve the accuracy of differentiating benign and malignant thyroid nodules, and show that the diagnostic coincidence rate obtained by the combined method is the highest in both large and small nodules[22]. In the TgAb positive group, the diagnostic effects of combined Y value obtained by multiple logistic regression model and other single indicators were compared. It can be seen from the ROC curve that the area under the curve shown by the Y value is larger than that of other methods.
In terms of the diagnostic coincidence rate of the detection scheme, for large thyroid nodules, the combination of the scheme has the same diagnostic coincidence rate as that of B-ultrasound, which shows that the combination of multiple methods not only improves the diagnostic performance of a single method, but also retains the advantages of B-ultrasound detection. Finally, in order to more clearly understand the application effect of combined Tg, TSH, B-ultrasound and ECT imaging, the follow-up patients in our hospital were empirically analyzed. The results showed that the coincidence rate between the combined method and the final doctor’s diagnosis reached more than 98 %, which shows that the combined Tg, TSH, B-ultrasound and ECT imaging is effective in the identification of benign and malignant thyroid nodules[23].
To sum up, in view of the deficiencies in the identification of benign and malignant thyroid nodules in clinical practice, the proposed combined Tg, TSH, B-ultrasound and ECT imaging is effective in the identification of benign and malignant thyroid nodules before operation.
It can be seen from the results that the diagnostic performance obtained by the combination of Tg, TSH, B-ultrasound and ECT imaging is significantly better than the single use of each diagnostic standard, which is practical in clinical application. However, from the content of the study, the combination mechanism between various evaluation criteria has not been deeply explored. Therefore, the next research scheme is to deeply explore the combination mechanism, so as to put forward a more ideal diagnostic method for the clinical differentiation of benign and malignant thyroid nodules.
Conflict of interests:
The authors declared no conflict of interest.
References
- Zheng Y, Xiao Z, Zhang H, She D, Lin X, Lin Y, et al. Differentiation between benign and malignant palatal tumors using conventional MRI: A retrospective analysis of 130 cases. Oral Surg Oral Med Oral Pathol Oral Radiol 2018;125(4):343-50.
[Crossref] [Google Scholar] [PubMed]
- Li T, Jiang Z, Lu M, Zou S, Wu M, Wei T, et al. Computer-aided diagnosis system of thyroid nodules ultrasonography: Diagnostic performance difference between computer-aided diagnosis and 111 radiologists. Medicine 2020;99(23):e20634.
[Crossref] [Google Scholar] [PubMed]
- Schmeel FC, Luetkens JA, Wagenhäuser PJ, Meier-Schroers M, Kuetting DL, Feißt A, et al. Proton density fat fraction (PDFF) MRI for differentiation of benign and malignant vertebral lesions. Eur Radiol 2018;28(6):2397-405.
[Crossref] [Google Scholar] [PubMed]
- Lu DL, Lu YQ, Mu XY, Qin YY, Zhu ZH, Zhao SS, et al. Differential diagnostic value of 99TcmO4- thyroid scintigraphy and serum TSH in high-risk thyroid nodules revealed by ultrasonography. Int J Radiat Med Nucl Med 2021;45(3):147-54.
- Zhong KX, Zhang JS, Zhang YW, Liu FC, Wu XJ, Ke M, et al. Diagnostic evaluation of thyroid nodules by 99TcmO4- functional imaging combined with color doppler ultra-sound: A comparative analysis with pathological results. J Pract Med 2020;36(1):103-7.
- Tang P, Ren C, Shen L, Zhou Z. Development and validation of a diagnostic nomogram for the preoperative differentiation between follicular thyroid carcinoma and follicular thyroid adenomas. J Comput Assist Tomogr 2021;45(1):128-34.
[Crossref] [Google Scholar] [PubMed]
- Lennartz S, Zopfs D, Abdullayev N, Bratke G, Le Blanc M, Slebocki K, et al. Iodine overlays to improve differentiation between peritoneal carcinomatosis and benign peritoneal lesions. Eur Radiol 2020;30(7):3968-76.
[Crossref] [Google Scholar] [PubMed]
- Galimzianova A, Siebert SM, Kamaya A, Rubin DL, Desser TS. Quantitative framework for risk stratification of thyroid nodules with ultrasound: A step toward automated triage of thyroid cancer. AJR Am J Roentgenol 2020;214(4):885-92.
- Mauri G, Gennaro N, Lee MK, Baek JH. Laser and radiofrequency ablations for benign and malignant thyroid tumors. Int J Hyperthermia 2019;36(2):13-20.
[Crossref] [Google Scholar] [PubMed]
- Tao Q, Zhou YM, He WH. Research progress of thyroid imaging reporting and data system (TIRADS). Chin J Otorhinolaryngol Head Neck Surg 2016;51(5):393-6.
[Crossref] [Google Scholar] [PubMed]
- Girardi FM, Silva LM, Flores CD. A predictive model to distinguish malignant and benign thyroid nodules based on age, gender and ultrasonographic features. Braz J Otorhinolaryngol 2019;85:24-31.
[Crossref] [Google Scholar] [PubMed]
- Yang W, Fananapazir G, LaRoy J, Wilson M, Campbell MJ. Can the American thyroid association, K-Tirads, and Acr-Tirads ultrasound classification systems be used to predict malignancy in bethesda category IV nodules? Endocr Pract 2020;26(9):945-52.
[Crossref] [Google Scholar] [PubMed]
- He JB, Zhang XY, Zhu T, Fan SJ. Ability of asparagine-rich protein to enhance the radiation resistance of Arabidopsis thaliana. Int J Nucl Med Radiat Med 2020;44(4):236-42.
- O'Connell K, Clark A, Hopman W, Lakoff J. Thyroid nodule growth as a predictor of malignancy. Endocr Pract 2019;25(10):1029-34.
[Crossref] [Google Scholar] [PubMed]
- Suster S. Controversies regarding the interpretation of follicular thyroid nodules. Arch Pathol Lab Med 2019;143(12):1472-6.
[Crossref] [Google Scholar] [PubMed]
- Ding Y, Li WL, Li Q, Li D, Zhang FQ, Ding XM, et al. Predictive value of postoperative initial stimulated thyroglobulin level on distant metastasis of differentiated thyroid carcinoma. Int J Nucl Med Radiat Med 2019;43(4):308-13.
- Alexander LF, Patel NJ, Caserta MP, Robbin ML. Thyroid ultrasound: Diffuse and nodular disease. Radiol Clin North Am 2020;58(6):1041-57.
[Crossref] [Google Scholar] [PubMed]
- Lv XF, Wang YH, Sun DL, Sun QY. Ultrasonic characteristics and blood flow analysis of benign and malignant thyroid nodules. J Ultrasound Clin Med 2019;21(6):435-8.
- Wang B, Sun F, Zheng XZ, Sun CY. A novel application of pulmonary transit time to differentiate between benign and malignant pulmonary nodules using myocardial contrast echocardiography. Int J Cardiovasc Imaging 2021;37(4):1215-23.
[Crossref] [Google Scholar] [PubMed]
- Adhami M, Michail P, Rao A, Bhatt CR, Grodski S, Serpell JW, et al. Anti-thyroid antibodies and TSH as potential markers of thyroid carcinoma and aggressive behavior in patients with indeterminate fine-needle aspiration cytology. World J Surg 2020;44(2):363-70.
[Crossref] [Google Scholar] [PubMed]
- Ruanpeng D, Cheungpasitporn W, Thongprayoon C, Hennessey JV, Shrestha RT. Systematic review and meta-analysis of the impact of noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP) on cytological diagnosis and thyroid cancer prevalence. Endocr Pathol 2019;30(3):189-200.
[Crossref] [Google Scholar] [PubMed]
- Tian C, Wang Z, Hou X, Wang C. The diagnostic accuracy of superb microvascular imaging in distinguishing thyroid nodules: A protocol for systematic review and meta-analysis. Medicine 2020;99(40):e22350.
[Crossref] [Google Scholar] [PubMed]
- Kim M, Chung SR, Jeon MJ, Han M, Lee JH, Song DE, et al. Determining whether tumor volume doubling time and growth rate can predict malignancy after delayed diagnostic surgery of follicular neoplasm. Thyroid 2019;29(10):1418-24.
[Crossref] [Google Scholar] [PubMed]
 ) Benign group; (
) Benign group; ( ) Malignant group
) Malignant group 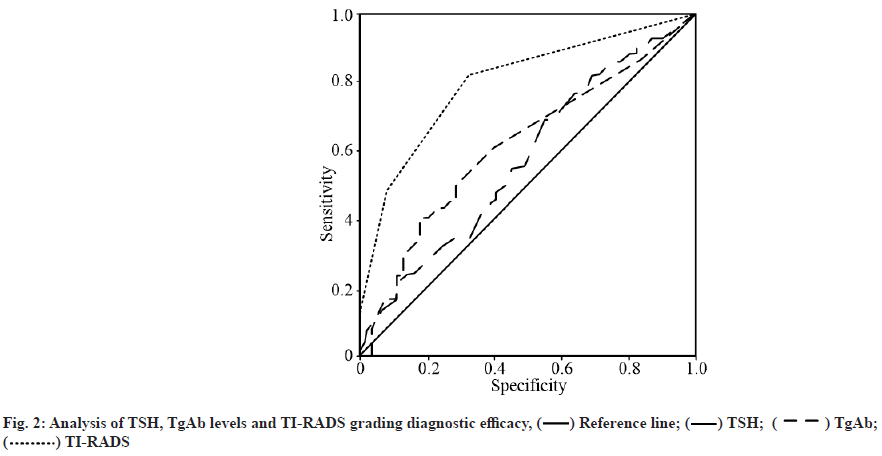
 ) Reference line; (
) Reference line; ( ) TSH; (
) TSH; ( ) TgAb; (
) TgAb; ( ) TI-RADS
) TI-RADS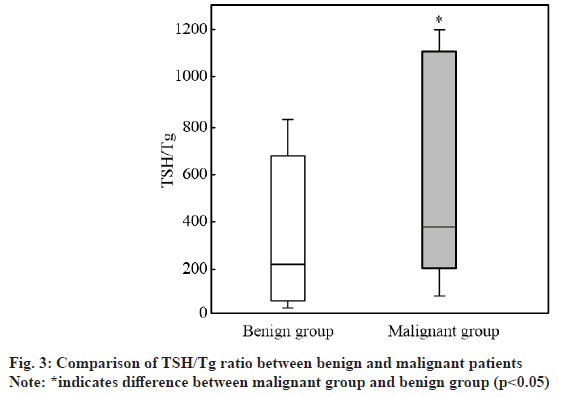
 ) Reference line; (
) Reference line; ( ) TSH/Tg
) TSH/Tg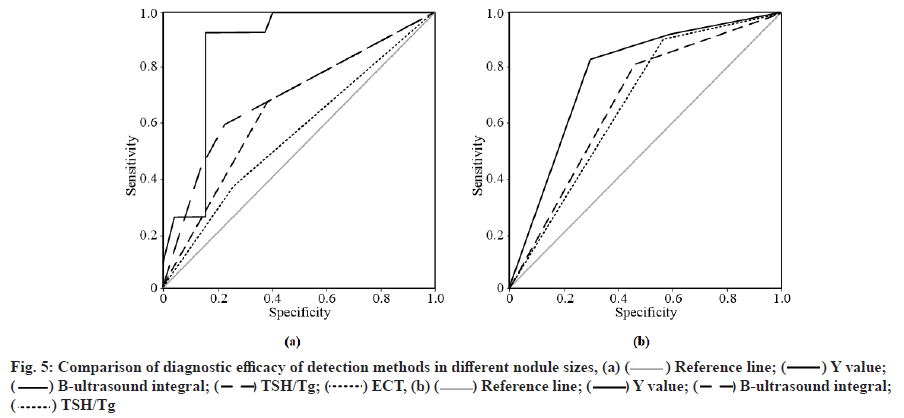
 ) Reference line; (
) Reference line; ( ) Y value; (
) Y value; ( ) B-ultrasound integral; (
) B-ultrasound integral; ( ) TSH/Tg; (
) TSH/Tg; ( ) ECT, (b) (
) ECT, (b) ( ) Reference line; (
) Reference line; ( ) Y value; (
) Y value; ( ) B-ultrasound integral; (
) B-ultrasound integral; ( ) TSH/Tg
) TSH/Tg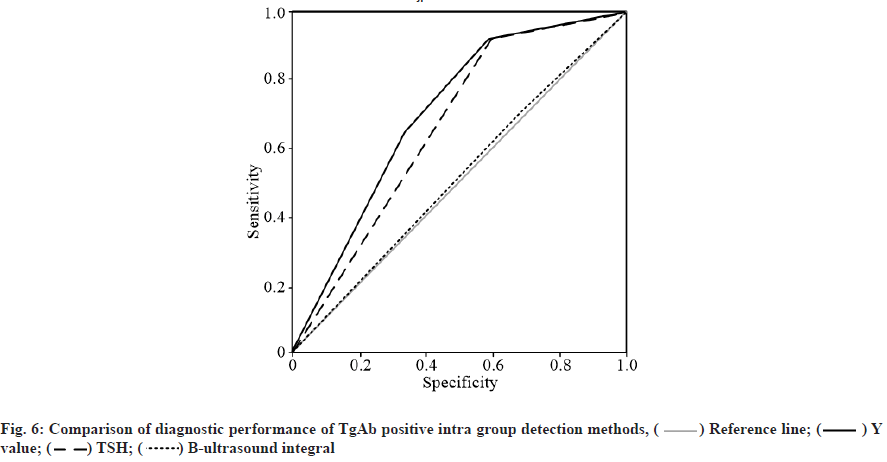
 ) Reference line; (
) Reference line; ( ) Y value; (
) Y value; ( ) TSH; (
) TSH; ( ) B-ultrasound integral
) B-ultrasound integral



