- *Corresponding Author:
- L. Hu
Department of Radiology, Yongchuan Hospital of Chongqing Medical University, Yongchuan, Chongqing 402160, China
E-mail: 700056@hospital.cqmu.edu.cn
| This article was originally published in a special issue, “New Research Outcomes in Drug and Health Sciences” |
| Indian J Pharm Sci 2023:85(6) Spl Issue “210-215” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Evaluating individuals diagnosed with type 2 diabetes mellitus, the research aims to assess the effects of dapagliflozin and metformin combination therapy on myocardial strain using magnetic resonance imaging measurements. A random division was conducted for individuals diagnosed with type 2 diabetes mellitus admitted between January 2019 and January 2021, resulting in the control group (comprising 26 cases) and the observation group (comprising 28 cases). Metformin treatment was given to the control group, whereas the observation group was administrated a combined therapy of dapagliflozin and metformin. The study compared the glycemic and lipid-related indicators, as well as left ventricular myocardial strain parameters between the two groups. Prior to treatment, there were no notable variations in glycemic and lipid-related indicators, as well as left ventricular myocardial strain parameters, between the groups. Following treatment, the observation group showed statistically lower levels of glycated hemoglobin, 2 h postprandial blood glucose, fasting plasma glucose, total cholesterol, triglycerides and low-density lipoprotein compared to the control group (p>0.05). Comparative analysis revealed that the observation group exhibited elevated levels of global longitudinal strain, global circumferential strain and global radial strain when compared to the control group. However, these differences did not yield significant results (p>0.05). Combining dapagliflozin with metformin exhibits positive efficacy in treating type 2 diabetes by effectively controlling blood glucose and lipid levels. Furthermore, the implementation of cardiac magnetic resonance feature tracking technology enables the quantitative evaluation of strain in the left ventricular myocardium, aiding in the detection of subclinical impairment in patients.
Keywords
Type 2 diabetes mellitus, dapagliflozin, metformin, myocardial strain, cardiac magnetic resonance
With its escalating prevalence year by year, Type 2 Diabetes Mellitus (T2DM) is a widely observed clinical condition that results in disturbances in glucose metabolism. The development of T2DM is highly associated with factors such as overweight obesity and lack of physical activity[1]. Metformin is a recommended first-line medication for T2DM treatment, which works by improving insulin sensitivity[2]. However, its efficacy for lowering blood glucose is limited when used as a monotherapy, thus combination therapy has become a routine treatment approach. The glucoselowering effects of dapagliflozin and Sodium- Glucose Co-Transporter-2 (SGLT2) inhibitor, are observed without reliance on insulin. Studies have reported that the combination of dapagliflozin and metformin can more effectively control blood glucose and lipids levels[3], making it a hot topic of research. Abnormal glucose metabolism can lead to cardiac remodeling, which gradually impairs cardiac systolic function and can even result in clinical heart failure in severe cases[4,5]. Myocardial strain provides unique information about left ventricular remodeling and fibrosis, and is widely used to evaluate subclinical myocardial dysfunction[6]. Cardiac Magnetic Resonance- Feature Tracking (CMR-FT) allows for quantitative analysis of myocardial motion changes without the need for special imaging sequences. It provides a reliable indicator to assess cardiac function by obtaining myocardial strain through simple postprocessing. The goal of the study is to figure out the efficacy of dapagliflozin combined with metformin on myocardial strain in individuals with T2DM using CMR-FT assessment.
Materials and Methods
General information:
Between January 2019 and January 2021, a group of 54 individuals who were diagnosed with T2DM were selected from our hospital for this research. The observation group included 28 cases, whereas the control group comprised 26 cases. The control group consisted of 16 males and a total of 10 females among the individuals. They had a disease duration ranging from 1 y to 17 y (mean duration was 9.77±3.29 y) and an age range of 40 y to 67 y (average age was 57.08±6.33 y). The observation group comprised 15 males and 13 females, with a disease duration ranging from 1 y to 18 y (mean duration was 10.15±2.71 y). Within the participant group, age spanned from 42 y to 70 y (average age was 58.67±8.05 y). The groups demonstrated comparable general information (p>0.05), indicating no significant disparities.
Inclusion and exclusion criteria:
Inclusion criteria: Fulfilling the diagnostic criteria specified in the "Chinese Guidelines for the Prevention and Treatment of T2DM (2020 edition)"[7]; age >18 y; not taking other hypoglycemic drugs before enrollment and patient comprehension of the study details, willingness to participate voluntarily and agreement to sign the informed consent document.
Exclusion criteria: Patients with complications of diabetes; pregnant or lactating women; individuals with severe organic diseases; patients with T1DM; be allergic to dapagliflozin and metformin and poor compliance or with cognitive or mental disorders.
Methods:
Drug treatment: The control group was administered oral sustained-release metformin hydrochloride tablets (produced by Zhejiang Dabo Pharmaceutical Co., Ltd., China) at a dose of 0.5 g per time, twice daily, continuously for 3 mo. The observation group received combination therapy with dapagliflozin (produced by AstraZeneca AB, China, Approval number: HJ20170118) and metformin. The metformin dosage was the same as the control group, and dapagliflozin was orally administered at a dose of 10 mg per time, once daily, continuously for 3 mo.
Magnetic Resonance Imaging (MRI) examination: A 3.0T scanner (Magnetom Verio; Siemens, Germany) was utilized for cardiac MRI procedures. Patient positioning during the scanning procedure was supine, prioritizing their comfort. To acquire images of the left ventricle, a balanced steady-state free-precession sequence was utilized in the imaging protocol, focusing on obtaining long-axis and short-axis cine images, including the standard 2-chamber, 3-chamber and 4-chamber views. The imaging parameters consisted of a 39.24 ms repetition time, 1.43 ms echo time, 6.0 mm slice thickness, 340 mm×284 mm field of view, 208×166 matrix size and a flip angle of 51°.
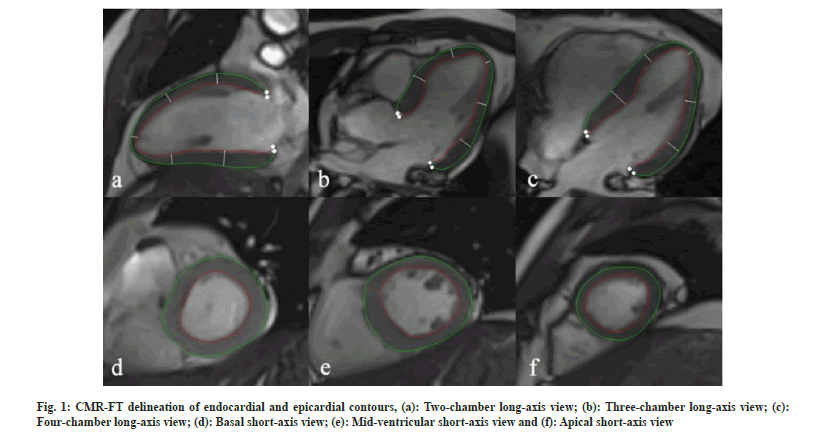
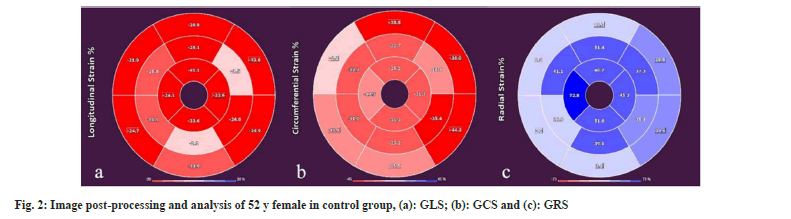
Image post-processing and analysis: CMR-FT software (Medis Suite QStrain 4.0; Netherlands) was utilized for left ventricular strain analysis. Firstly, the left ventricles endocardial and epicardial borders were automatically identified during diastole and systole, and any necessary adjustments were made manually (fig. 1). Left ventricular Global Longitudinal Strain (GLS) was calculated using standard long-axis views, while Global Radial Strain (GRS) and Global Circumferential Strain (GCS) were determined using short-axis views at the basal, mid-ventricular and apical levels as shown in fig. 2.
Observational indicators:
Comparison of glycemic parameters (Hemoglobin A1c (HbA1c), Fasting Plasma Glucose (FPG), 2 h Post-Load Glucose (2hPG)) between the two groups before and after treatment, lipid parameters (Triglyceride (TG), Total Cholesterol (TC), Low- Density Lipoprotein-Cholesterol (LDL-C)), and left ventricular myocardial strain parameters (GLS, GCS and GRS).
Statistical methods:
Statistical Package for the Social Sciences (SPSS) 25.0 will be utilized to perform the statistical analysis in this research. Continuous variables will be reported as means and standard deviations (x±s) and analyzed using t-tests. Categorical variables will be presented as frequencies and percentages (n (%)) and analyzed using Chi-square (χ2) tests. To establish statistical significance, a significance level of p<0.05 will be employed.
Results and Discussion
At baseline, there were no significant disparities in HbA1C, FPG and 2hPG levels between the groups. In response to the treatment, both groups exhibited a decrease in HbA1C, FPG and 2hPG values relative to their respective pre-treatment values. Importantly, the observation group had notably lower HbA1C, FPG and 2hPG values (p<0.05) as shown in Table 1.
| Group | n | Treatment | HbA1c (%) | FPG (mmol/l) | 2hPG (mmol/l) |
|---|---|---|---|---|---|
| Observation | 28 | Before | 11.69±2.41 | 13.39±3.07 | 15.28±5.02 |
| After | 6.84±1.23ab | 7.09±1.66ab | 9.46±2.51ab | ||
| Control | 26 | Before | 11.55±1.32 | 13.26±3.44 | 15.39±4.10 |
| After | 8.78±1.80a | 9.30±2.52a | 11.03±5.19a |
Note: Intra-group comparison prior to treatment, ap<0.05 and comparison between groups post- treatment, bp<0.05
Table 1: Comparison of glucose metabolism indexes Prior to and Post-Treatment (X±S)
At baseline, no significant variations in TG, TC and LDL-C levels were observed between the groups (p>0.05). Post-treatment, both groups showcased a decrease in TC, TG and LDL-C values compared to their respective pre-treatment values. Notably, the observation group showcased statistically lower TG, LDL-C and TC levels than the control group (p<0.05). For further insights, consult as shown in Table 2.
| Group | n | Treatment | TG (mmol/l) | TC (mmol/l) | LDL-C (mmol/l) |
|---|---|---|---|---|---|
| Observation | 28 | Before | 2.10±0.19 | 4.72±0.37 | 2.80±0.42 |
| After | 1.35±0.22ab | 4.21±0.17ab | 2.44±0.46ab | ||
| Control | 26 | Before | 2.16±0.17 | 4.70±0.31 | 2.72±0.41 |
| After | 1.75±0.30a | 4.50±0.19a | 2.50±0.44a |
Note: Intra-group comparison prior to treatment, ap<0.05 and comparison between groups post-treatment, bp<0.05
Table 2: Comparison of blood lipid indexes prior to and Post-Treatment (X±S)
Prior to treatment, no statistically significant differences in GLS, GCS, and GRS levels were detected between the two groups. Subsequently, both groups exhibited an increase in GLS, GCS and GRS values compared to their individual pretreatment levels. Of importance, the observation group displayed significantly higher GLS, GCS and GRS values in contrast to the control (p<0.05) as shown in Table 3.
| Group | n | GLS (%) | GCS (%) | GRS (%) | |
|---|---|---|---|---|---|
| Observation | 28 | Before | -8.00±3.77 | -14.44±3.29 | 19.66±7.39 |
| After | -14.61±3.08ab | -20.20±3.21ab | 26.78±4.58ab | ||
| Control | 26 | Before | -8.06±4.51 | -14.27±3.47 | 19.22±8.03 |
| After | -10.64±3.24a | -16.39±3.35a | 22.10±4.03a |
Note: Intra-group comparison prior to treatment, ap<0.05 and comparison between groups post-treatment, bp<0.05
Table 3: Comparison of Left Ventricular Myocardial Strain Parameters Prior to and Post-Treatment (X±S)
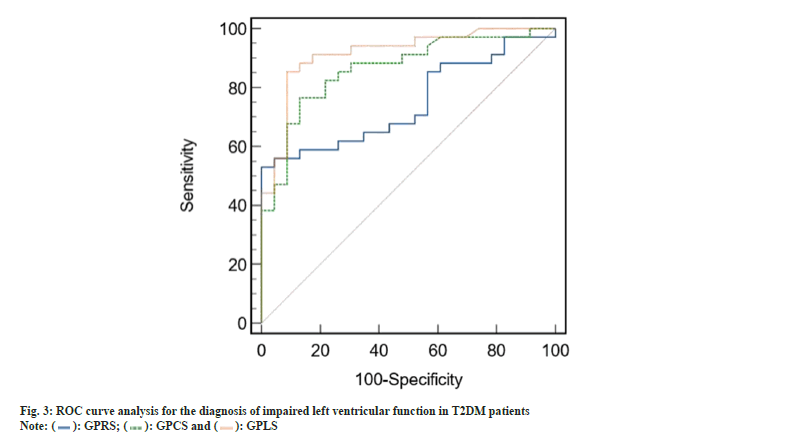
When diagnosing impaired left ventricular function in T2DM patients, the ROC curve analysis indicated that GRS had an optimal cutoff value of 22.01 %. The corresponding sensitivity and specificity were 51.5 % and 98.3 %, respectively, yielding an Area Under the Curve (AUC) of 0.742 (95 % Confidence Interval (CI) 0.620-0.835). Similarly, GCS had an optimal cutoff value of -17.35 %, with a sensitivity of 72.5 %, specificity of 85.0 %, and an AUC of 0.867 (95 % CI 0.723-0.949). For GLS, the optimal cutoff value was -10.10 %, showing a sensitivity of 85.3 %, specificity of 91.3 %, and an AUC of 0.915 (95 % CI 0.810-0.972) as shown in fig. 3.
T2DM is a common endocrine disorder that is influenced by various factors such as environment, genetics and lifestyle. It can lead to multiple severe complications and has a significant disability and mortality rate[8]. The treatment principles for T2DM involve controlling disease progression and maintaining optimal blood sugar levels. Therefore, the rational selection of antidiabetic medications is crucial for managing T2DM. Metformin is a commonly used medication for treating T2DM but has its limitations, with about 1/3rd of patients not achieving ideal blood sugar control when used alone[9,10]. Hence, combination therapy has become a common approach in T2DM treatment. Dapagliflozin, as a non-insulindependent antidiabetic medication, is often used in combination with metformin and has shown good efficacy in T2DM treatment[11].
The study results demonstrate that after treatment, patients receiving combination therapy exhibited significant reductions in HbA1C, FPG and 2hPG levels as opposed to the control group (p<0.05). Combining dapagliflozin with metformin enhanced the efficacy of blood sugar control, consistent with previous research findings[12]. The two medications have complementary advantages and synergistic effects. Metformin primarily increases insulin sensitivity, accelerates glucose metabolism, and relies on insulin secretion to exert its effects. On the other hand, dapagliflozin functions by regulating blood sugar through the kidneys, promoting urinary glucose excretion, without relying on insulin secretion. Additionally, dapagliflozin can improve insulin resistance, making the body more responsive to metformin[13]. Therefore, the combined use of dapagliflozin and metformin leads to better therapeutic outcomes. The observation group exhibited significantly decreased levels of TG, TC and LDL-C in comparison to the control (p<0.05). This mainly reflects dapagliflozin ability to inhibit glucose conversion into fat and promote fat breakdown, thereby improving the patient's lipid profile[14]. The improvement in lipid metabolism combined with the amelioration of lipid parameters also reduces interference with normal glucose metabolism, which further contributes to glycemic control.
Diabetes mellitus contributes to a higher propensity for myocardial injury, an independent risk factor strongly linked to the onset of cardiovascular disease. If not promptly intervened, it may lead to Diabetic Cardiomyopathy (DCM). Myocardial strain, which quantitatively assesses myocardial deformation, is a sensitive marker for subclinical impairment of cardiac function and has higher predictive value than ejection fraction[15,16]. Due to its accuracy and reproducibility, CMR-FT technology has gained significant popularity in recent years for assessing myocardial strain. An analysis of the results revealed noteworthy enhancements in myocardial strain indices, encompassing GLS, GCS and GRS, within the treatment group, in contrast to the control group (p<0.05). This suggests that combining dapagliflozin with metformin has a certain effect in delaying early myocardial damage in individuals with T2DM. Moreover, CMR-FT technology enables accurate quantitative assessment of myocardial strain in T2DM patients, facilitating early detection and intervention for myocardial functional impairment. Based on Receiver Operating Characteristic (ROC) curve analysis, it is evident that GLS, GCS and GRS offer valuable diagnostic insights into impaired left ventricular function in T2DM patients. Remarkably, GLS achieves the highest diagnostic performance and sensitivity, with a cut-off value of -10.10 %.
In conclusion, the combination therapy of dapagliflozin and metformin in treating T2DM has demonstrated definite efficacy in improving glucose metabolism and lipid profile, warranting clinical promotion. Through the use of CMRFT technology, healthcare professionals can accurately assess myocardial strain, enabling the prompt detection of subclinical left ventricular dysfunction in T2DM patients. This imaging approach serves as compelling imaging evidence to guide clinical treatment.
Funding:
This work was supported by 2021 Natural Science Foundation Project of Yongchuan District, Chongqing (No. 2021yc-jckx20032).
Conflict of interests:
The authors declared no conflict of interests.
References
- Shi H, Dang J, He J. Effects of dapagliflozin on blood glucose fluctuation in obese patients with type 2 diabetes mellitus. Chin J Clin Pharmacol 2021;37(21):2867-74.
- Liu D, Xie H, Jiang X. Pharmacological action and clinical application of metformin. J Hubei Med Coll 2022;41(1):95-9.
- Zheng K, Zhang X, Geng J. Effects of lipopeptide and insulin on glucose and lipid metabolism, inflammation, intestinal flora and adiponectin expression in newly diagnosed obese type 2 diabetes mellitus. J Clin Exp Med 2020;19(22):2420-3.
- Larghat AM, Swoboda PP, Biglands JD, Kearney MT, Greenwood JP, Plein S. The microvascular effects of insulin resistance and diabetes on cardiac structure, function and perfusion: A cardiovascular magnetic resonance study. Eur Heart J Cardiovasc Imaging 2014;15(12):1368-76.
[Crossref] [Google Scholar] [PubMed]
- From AM, Scott CG, Chen HH. The development of heart failure in patients with diabetes mellitus and pre-clinical diastolic dysfunction: A population-based study. J Am Coll Cardiol 2010;55(4):300-5.
[Crossref] [Google Scholar] [PubMed]
- Claus P, Omar AM, Pedrizzetti G, Sengupta PP, Nagel E. Tissue tracking technology for assessing cardiac mechanics: Principles, normal values and clinical applications. JACC Cardiovasc Imaging 2015;8(12):1444-60.
[Crossref] [Google Scholar] [PubMed]
- Diabetic Branch of Chinese Medical Association. Chinese Guidelines for the Prevention and Treatment of Type 2 Diabetes (2020 ed). Int J Endocrine Metab 2021;41(5):482-548.
- Liu H, Liu X, He G. Efficacy and microinflammatory and oxidative stress indexes of lialuptide combined with metformin in the treatment of obese diabetes mellitus. Chin J Coal Ind Med 2020;23(2):186-91.
- Zhen S, Huang Y, Stuart R. Analysis of the efficacy of metformin combined with dazepine in the treatment of type 2 diabetes and its effect on islet function. Harbin Med 2022;42(3):56-7.
- Xu Y, Wu P, Wen W. Short-term intensive hypoglycemia with metformin, saglitine and daguergin: A multicenter prospective clinical trial of 54 newly diagnosed type 2 diabetes mellitus. J Southern Med Univ 2019;39(11):1305-11.
- Sun W, Wang F, Yang L. Clinical study of daguerjing in the treatment of type 2 diabetes. Chin General Med 2021;19(8):1303-5.
- Zhou H, Kong Y. Efficacy of aglitine or daguergin combined with metformin in the treatment of type 2 diabetes mellitus. J Clin Pathol 2020;40(5):1169-73.
- Song N, Bu F. Clinical efficacy and related endocrine hormone levels of dagrejing combined with metformin in patients with diabetes mellitus. New World Diabet 2021;24(9):60-2.
- Wang Z, Wang X, Chen T. Observation on the efficacy of Dagelejing combined with metformin in the treatment of type 2 diabetes mellitus. Strait Pharm 2021;33(3):184-5.
- Ambale-Venkatesh B, Yoneyama K, Sharma RK, Ohyama Y, Wu CO, Burke GL, et al. Left ventricular shape predicts different types of cardiovascular events in the general population. Heart 2017;103(7):499-507.
[Crossref] [Google Scholar] [PubMed]
- Yoneyama K, Venkatesh BA, Wu CO, Mewton N, Gjesdal O, Kishi S, et al. Diabetes mellitus and insulin resistance associate with left ventricular shape and torsion by cardiovascular magnetic resonance imaging in asymptomatic individuals from the multi-ethnic study of atherosclerosis. J Cardiovasc Magn Reson 2018;20(1):53.
[Crossref] [Google Scholar] [PubMed]