- *Corresponding Author:
- Weiling Guo
Department of Nursing, Fourth Affiliated Hospital of Nanchang University, Nanchang, Jiangxi 330209, China
E-mail: weigan9660048682@163.com
| This article was originally published in a special issue, “New Research Outcomes in Drug and Health Sciences” |
| Indian J Pharm Sci 2023:85(6) Spl Issue “270-277” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
The overall aim is to research the influence of Baduanjin on cardiopulmonary function in patients suffering from congestive heart failure. 110 patients with congestive heart failure in our infirmary were selected and the duration is from January 2018 to January 2020. The sufferers took part in the research. They were selected and arbitrarily allocated to the conventional group and the study group. The conventional group received conventional treatment, and the study group received Baduanjin exercise after the conventional treatment. After 6 mo of treatment, the comparison of cardiac function, pulmonary function, exercise endurance index, serum index and improvement in quality of life of these two were evaluated. After treatment, the indexes of cardiac function; left ventricular ejection fraction, left ventricular end-systolic volume, left ventricular end-diastolic volume, pulmonary function like peak oxygen uptake, anaerobic threshold, oxygen uptake/minute ventilation, slope, exercise endurance like maximum exercise power, maximum exercise time, 6 min walk test, serum tumor necrosis factor-alpha, interleukin-1, interleukin-6, plasma N-terminal probrain natriuretic peptide level and Minnesota living with heart failure questionnaire score of quality of life in the study group were better than those in the conventional group (p<0.05). Baduanjin can effectively enhance the cardiopulmonary function of patients with congestive heart failure, enhance their exercise endurance and intensity, regulate the expression level of serum indicators, and comprehensively improve the quality of life of patients.
Keywords
Baduanjin, chronic heart failure, cardiac function, pulmonary function, quality of life, exercise state
Chronic Heart Failure (CHF) is the end stage of the progress of various heart diseases. It is a syndrome of cardiac circulation disorder caused by the dysfunction of cardiac systolic function and (or) diastolic function that cannot discharge venous blood from the heart normally, resulting in venous blood stasis and insufficient arterial blood perfusion[1-3]. Although great progress has been made in the treatment of CHF, there is still no radical cure. Patients are still disturbed by symptoms such as decreased exercise tolerance and dyspnea, resulting in a serious decline in their quality of life, and even loss of work and living ability, eventually leading to death[4-6]. Many studies have proved that, conventional standard treatment combined with athletic rehabilitation training can efficiently improve the cardiopulmonary function of CHF patient, improve their exercise tolerance and quality of life, and ultimately prolong the survival time of patients, reduce the readmission rate and mortality[7,8]. Baduanjin is a kind of fitness skill handed down since the Song Dynasty. It has the characteristics of gentle and slow movement, combination of tightness and looseness, perfect integration, combination of movement and stillness, artistic conception and harmony of spirit and form. And as an exercise rehabilitation therapy, Baduanjin has such advantages as no adverse and side effects. At present, Baduanjin has been widely used in patients with respiratory diseases, cardiovascular diseases and so on, which can effectively improve the quality of life and prognosis of cardiac function of Congenital Heart Disease (CHD) patients. This study was carried out to assess the application effect of Baduanjin in CHF patients in an objective way.
Materials and Methods
General data:
110 CHF patients were admitted in our hospital. The study duration proceeded from January 2018 to January 2020. CHF related criteria in 2014 edition of Chinese guidelines for diagnosis and treatment of heart failure[9], Chinese expert consensus on exercise rehabilitation of chronic stable heart failure[10].
Inclusion criteria: Patients who met the above diagnostic criteria for CHF and the requirements of exercise rehabilitation treatment; patients with stable physical signs for more than 3 mo; cardiac function grade II-III in line with New York Heart Association (NYHA); adult patients aged ≥18 y old and voluntary patients who signed informed consent.
Exclusion criteria: Patients with severe arrhythmia; patients with acute myocardial infarction and unstable angina pectoris; patients with uncontrollable hypertension; patients with pre-existing limb disability, skeletal and muscular diseases; patients with pulmonary infection or pre-existing pulmonary diseases; patients with unconsciousness, cognitive impairment, psychiatric diseases and poor compliance; patients in acute stage of infectious diseases, acute cardiovascular and cerebrovascular adverse events, within 14 d after trauma or surgery; patients with contraindications for the treatment methods involved in this study. Some sufferers were randomly allocated to the conventional group, and the rest is the study group, 55 cases in each group. In the conventional group, there were 24 males and 31 females, with a median age of (58.37±9.62) y old ranging from 48 y to 80 y old; NYHA grading: 25 cases of grade II, 30 cases of grade III; classification: 23 cases of non- ischemic cardiomyopathy, 32 cases of ischemic cardiomyopathy; complications: 31 cases of hypertension, 16 cases of diabetes. In the study group, there were 25 males and 30 females, with an average age of (58.64±9.87) y old ranging from 48 y to 82 y old; NYHA grading: 23 cases of grade II, 32 cases of grade III; classification: 22 cases of non-ischemic cardiomyopathy, 33 cases of ischemic cardiomyopathy and complications: 32 cases of hypertension, 15 cases of diabetes. The difference in general data in these two was not statistically significant (p>0.05).
Method:
Conventional group: Conventional anti-heart failure treatment was given, including diuretics, angiotensin converting enzyme inhibitors, beta receptor blockers, aldosterone antagonists, cardio tonics, etc. Moderate exercise and aerobic exercise such as walking was adopted according to the tolerance of patients.
Study group: On account of the above treatment in the conventional-treatment group, the study group did Baduanjin exercise. The pithy formula; holding Tianli Sanjiao in both hands, draw bows left and right resembling shooting eagle, rise one arm to regulate spleen and stomach, look backward to avoid disease and injury, shaking head and tail to release heart-fire, hands rub the back to legs to stabilize kidney, making fist and glaring eyes to enhance strength, shake the back to cure all disease. Give video materials to assist practice. The patients need to gradually improve their exercise proficiency, and improve the continuity and stability of the action. Before the Baduanjin exercise, the regular warm-up should be carried out for 5 min. The warm-up should be carried out in the patient’s favorite way, including aerobic exercise such as walking and gymnastics. After the Baduanjin exercise, stretching exercise should be carried out for 5 min, and the overall exercise time is 30 min each time, 5 d/week for 6 mo. The first 2 mo of the training were carried out in the hospital, and the last 4 mo were carried out outside the hospital. The patients were given Baduanjin demonstration video materials when they were discharged.
The two groups were given real-time monitoring of blood pressure, heart rate, electrocardiogram, as well as blood oxygen saturation while carrying out exercise in the hospital under special monitoring. The exercise was based on the tolerance of the patients, and the principle of gradual progress was observed. After the patients could tolerate the exercise, the exercise time could be appropriately extended or increased by 1 d every week.
Observation index:
The comparison of heart function indexes of the two was made after 6 mo of treatment; Left Ventricular End-Diastolic Volume (LVEDV), Left Ventricular End-Systolic Volume (LVESV), Left Ventricular Ejection Fraction (LVEF), Anaerobic Threshold (VO2AT), Ventilation (VE)/Carbon dioxide output (VCO2) slope, 50 % peak Oxygen Consumption (VO2), MET, exercise endurance index; maximum exercise time, maximum exercise power and 6 Min Walk Test (6MWT), serum index; Tumor Necrosis Factor-Alpha (TNF-α), Interleukin (IL)-1, IL- 6, N-Terminal prohormone of Brain Natriuretic Peptide (NT-proBNP) levels and improvement of quality of life.
Heart function was measured by echocardiography. The pulmonary function indexes were detected by COSMED power bicycle test system, and the symptom limited maximum load exercise was performed according to the sequence of rest, warm-up, incremental exercise and recovery. The relevant information was recorded. After 5 min of rest, the patients were connected with the lead wire of Electrocardiography (ECG), with the blood pressure sensing electrode attached to the strongest position of brachial artery pulsation, the cuff was tied, and the rest, warm-up, incremental exercise and recovery were performed. The data were recorded and analyzed.
Before and after treatment, 3 ml of fasting venous blood samples were obtained from all sufferers in the morning. Plasma and serum were separated by centrifuge and detected by Enzyme-Linked Immunoassay (ELISA). The operation was performed according to the instructions of the kit.
The quality of life was evaluated with the study questionnaire-the Minnesota Living with Heart Failure Questionnaire (MLWHFQ). The higher the score, the more serious the adverse effect of heart failure on the quality of life[11].
Statistical processing:
Statistical Package for the Social Sciences (SPSS) 21.0 software was utilized for statistical processing. By using measuring the data, it was shown in (x͞ ±s) format by t-test, p<0.05.
Results and Discussion
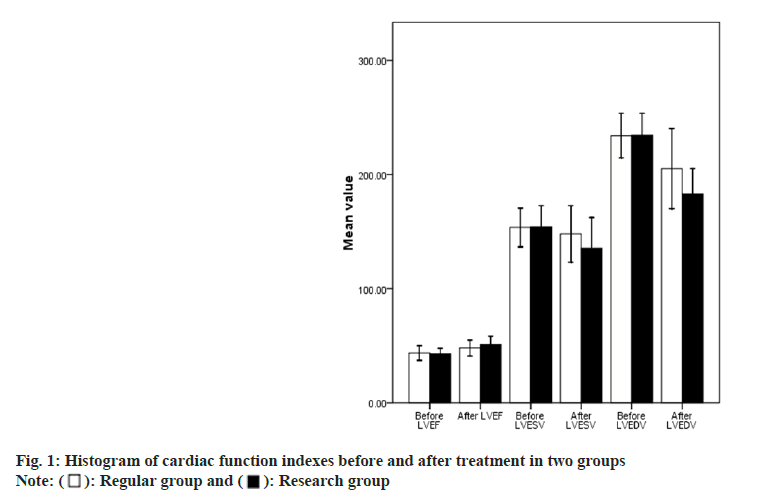
In relation to cardiac function indexes, there was obvious no statistical differences between above two at the pre-treatment, p>0.05. LVEF in the study group was greater than the other one at the post-therapy (p<0.05), LVESV and LVEDV in the study group were lesser, p<0.05; see more details in Table 1 and fig. 1.
| Group | Time | LVEF (%) | LVESV (ml) | LVEDV (ml) |
|---|---|---|---|---|
| Conventional (n=5) | Before treatment | 43.54±6.41 | 153.51±16.94 | 233.91±19.49 |
| After treatment | 47.95±6.98 | 147.87±24.78 | 205.08±35.11 | |
| Study (n=5) | Before treatment | 42.98±4.67 | 154.05±18.56 | 234.45±18.96 |
| After treatment | 51.15±7.19 | 135.50±26.78 | 182.94±22.08 | |
| t | Before treatment | 0.524 | 0.161 | 0.147 |
| After treatment | 0.602 | 0.872 | 0.883 | |
| p | Before treatment | 2.374 | 2.513 | 3.960 |
| After treatment | 0.019 | 0.013 | 0.000 |
Table 1: Comparison of Cardiac Function Indexes between the Two Groups before and after Treatment (x͞ ±s)
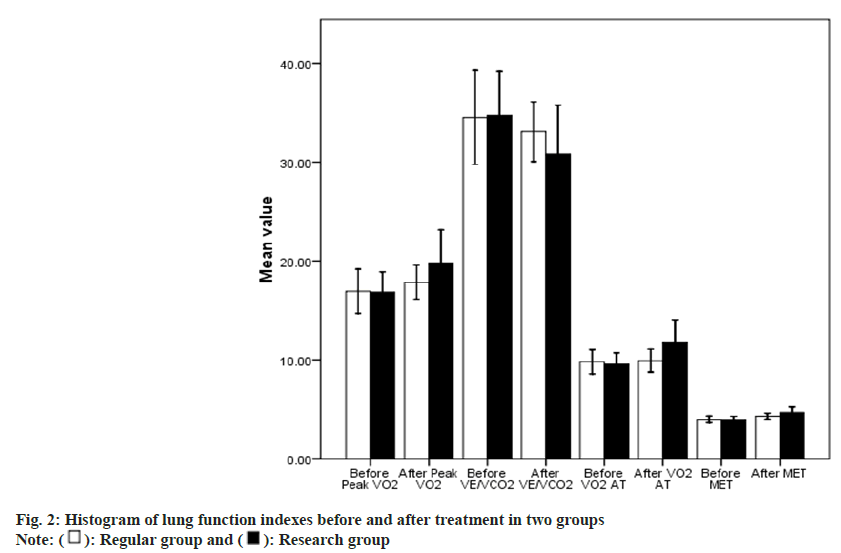
About lung function indexes, the result shows no statistical difference between them at pre- therapy (p>0.05). Peak VO2 and VO2AT in the study group were higher than another one at post-treatment (p<0.05), and VE/VCO2 slope was lower than that in the conventional group (p<0.05) as shown in Table 2 and fig. 2.
| Group | Time | Peak VO2 [ml/(min·kg)] | VE/VCO2 slop | VO2AT [ml/(min·kg)] |
|---|---|---|---|---|
| Conventional (n=5) | Before treatment | 16.93±2.24 | 34.52±4.75 | 9.80±1.23 |
| After treatment | 17.84±1.71 | 33.08±3.02 | 9.92±1.16 | |
| Study group (n=5) | Before treatment | 16.83±2.05 | 34.73±4.43 | 9.55±1.16 |
| After treatment | 19.73±3.41 | 30.81±4.95 | 11.74±2.31 | |
| t | Before treatment | 0.249 | 0.241 | 1.104 |
| After treatment | 0.804 | 0.810 | 0.272 | |
| p | Before treatment | 3.675 | 2.896 | 5.223 |
| After treatment | 0.000 | 0.005 | 0.000 |
Table 2: Comparison of Pulmonary Function Indexes before and after Treatment between the Two Groups (x͞ ±s)
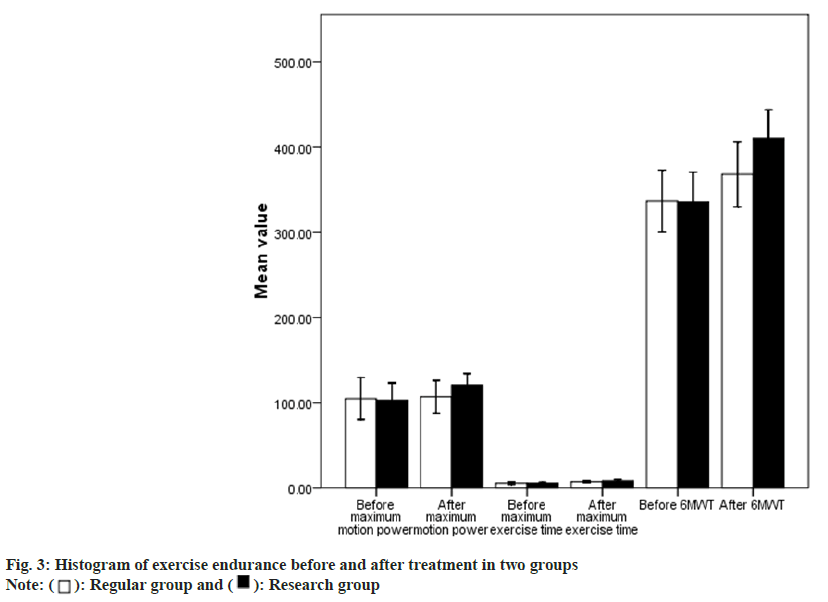
The result presents no statistical difference on all exercise indexes in those two at pre-treatment (p>0.05). The maximum exercise power, maximum exercise time and 6MWT of the study group were pretty greater after the therapy (p<0.05); find more details in Table 3 and fig. 3.
| Group | Time | Maximum exercise power (WI) | Maximum exercise time (min) | 6MWT (m) |
|---|---|---|---|---|
| Conventional (n=5) | Before treatment | 104.89±24.67 | 5.61±1.38 | 336.78±36.37 |
| After treatment | 106.98±19.10 | 7.19±1.07 | 368.26±38.15 | |
| Study (n=5) | Before treatment | 103.08±20.04 | 5.54±1.02 | 335.64±34.84 |
| After treatment | 120.70±13.6 | 8.29±1.26 | 410.20±34.01 | |
| t | Before treatment | 0.422 | 0.335 | 0.168 |
| After treatment | 0.674 | 0.739 | 0.867 | |
| p | Before treatment | 4.339 | 4.925 | 6.084 |
| After treatment | 0.000 | 0.000 | 0.000 |
Table 3: Comparison of Exercise Endurance Indexes between the Two Groups before and after Treatment (x͞ ±s)
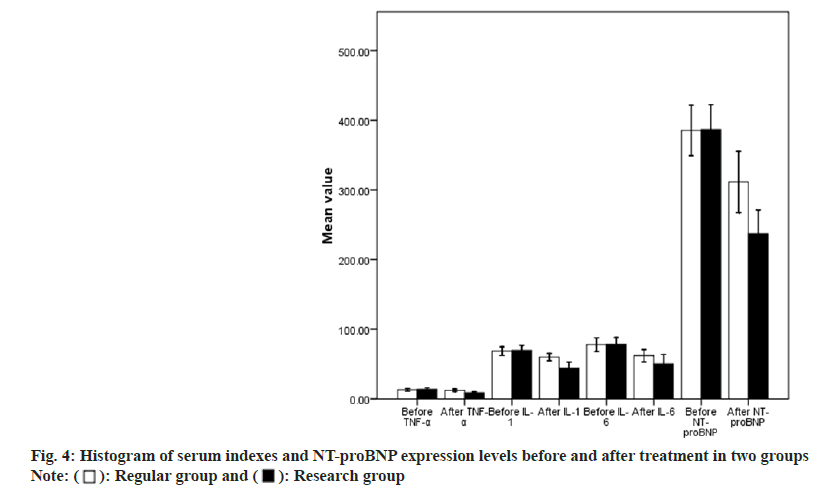
The result presents no statistical difference about serum indexes and NT-proBNP at pretreatment (p>0.05). The levels of TNF-α, IL-1, IL-6, as well as plasma NT-proBNP in the study group were much poorer after the therapy of that sufferers (p<0.05) as shown in Table 4 and fig. 4.
| Group | Time | TNF-α (ng/l) | IL-1 (ng/l) | IL-6 (ng/l) | NT-proBNP (ng/ml) |
|---|---|---|---|---|---|
| Conventional (n=5) | Before treatment | 13.53±1.92 | 68.40±6.35 | 77.72±9.98 | 385.29±36.28 |
| After treatment | 12.26±1.81 | 59.93±5.25 | 61.90±8.97 | 311.35±44.17 | |
| Study (n=5) | Before treatment | 13.84±2.06 | 69.51±7.30 | 78.37±9.61 | 386.60±35.66 |
| After treatment | 8.72±1.45 | 43.85±8.90 | 50.45±13.06 | 237.14±33.94 | |
| t | Before treatment | 0.802 | 0.852 | 0.347 | 0.190 |
| After treatment | 0.424 | 0.396 | 0.730 | 0.850 | |
| p | Before treatment | 11.310 | 11.536 | 5.357 | 9.881 |
| After treatment | 0.000 | 0.000 | 0.000 | 0.000 |
Table 4: Comparison of Serum Indexes and NT-proBNP Levels between the Two Groups before and after Treatment (x͞ ±s)
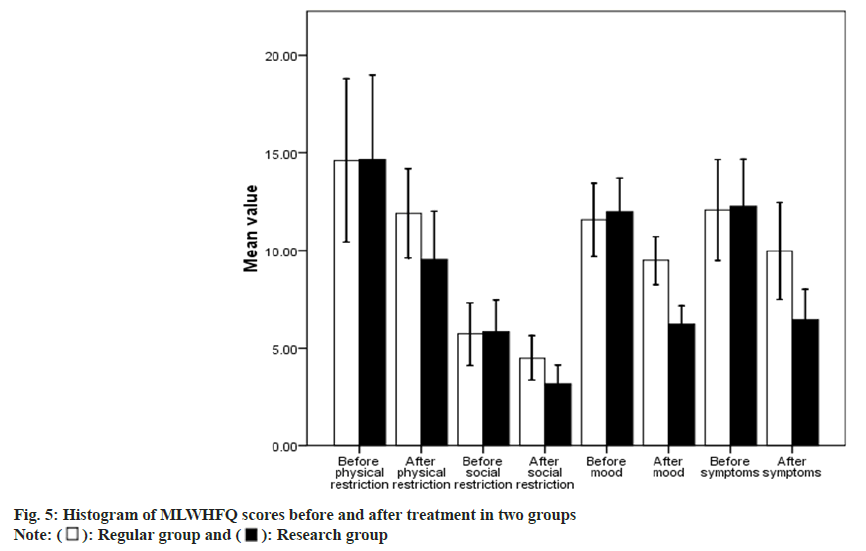
No statistical difference was appeared in MLWHFQ sub item scores in these two before therapy (p>0.05). The scores of physical limitation, social limitation, emotion and symptoms in the Baduanjin-exercise group were much lower (p<0.05) as shown in Table 5 and fig. 5.
| Group | Time | Physical limitation | Social limitation | Emotion | Symptoms |
|---|---|---|---|---|---|
| Conventional (n=5) | Before treatment | 14.61±4.16 | 5.73±1.6 | 11.57±1.89 | 12.06±2.59 |
| After treatment | 11.89±2.29 | 4.49±1.14 | 9.48±1.23 | 9.98±2.47 | |
| Study (n=5) | Before treatment | 14.65±4.31 | 5.83±1.65 | 11.97±1.75 | 12.25±2.42 |
| After treatment | 9.52±2.47 | 3.16±0.99 | 6.21±0.98 | 6.43±1.59 | |
| t | Before treatment | 0.057 | 0.317 | 1.158 | 0.390 |
| After treatment | 0.955 | 0.752 | 0.249 | 0.697 | |
| p | Before treatment | 5.213 | 6.546 | 15.400 | 8.957 |
| After treatment | 0.000 | 0.000 | 0.000 | 0.00 |
Table 5: Comparison of MLWHFQ Scores between the Two Groups before and after Treatment (x͞ ±s, scores)
The mechanism of CHF is relatively complex. At present, it is generally believed that it is related to hemodynamic changes, excessive activation of sympathetic nervous system and renin-angiotensin system, structural changes of myocardial cells mediated by inflammatory factors, myocardial injury caused by myocardial remodeling and other factors[12-14]. According to the theory of traditional Chinese medicine, the heart governs the blood vessels and is the sovereign organ of the human body. If the blood vessels are unobstructed and the Qi function is high, the whole body will be healthy and the five internal organs will be safe. Baduanjin is a way of exercise closely related to the system of traditional Chinese medicine[15,16]. Baduanjin skill harmonizes the movement of human body with breath and regulates the heart, with the characteristics of gentle and smooth movement, harmony and coherence, combination of movement and stillness, combination of looseness and tightness, unity of spirit and form, and artistic conception[17,18]. The whole set of exercises consists of eight specific movements. Each movement is designed according to the direction of the human body’s meridians. It can balance Qi and blood, dredge meridians, relax emotions, dredge blood vessels and regulate viscera and other functions, thus having a clear improvement effect on the human heart and respiratory system. Baduanjin’s movements are basically in line with the principle of bilateral symmetry, less walking, easy to learn and high safety. It can mainly enhance the strength of the core muscles of the limbs and waist, and abdomen, improve the efficiency of muscle pump, strengthen the breathing ability, improve the efficiency of aerobic exercise, and at the same time, the exercise intensity is low, which can help to establish the confidence of patients with CHF. The results showed that before treatment, the cardiopulmonary function, exercise endurance, serum indexes and quality of life of the both groups were at the same baseline level. After treatment, LVEF, LVESV and LVEDV of the Baduanjin-exercise group were greater, suggesting that the heart function of CHF can be effectively improved by practicing Baduanjin for 6 mo. The lung function indexes of the study group; peak VO2, VO2AT, VE/VCO2 slope were better than those of the conventional group; it suggested that Baduanjin could improve the lung and respiratory function of patients with CHF during exercise, and improve the hypoxia of patients. The results indicated that after treatment, the indexes of exercise endurance in the study group; maximum exercise power, maximum exercise time, 6MWT were notably greater; it suggested that insisting on practicing Baduanjin can effectively enhance the activity endurance of CHF, which is of positive significance for improving the psychological state of patients. After treatment, the expression levels of serum TNF-α, IL-1, IL-6 and plasma NT- proBNP in the study group were lower than those in the conventional group, suggesting that Baduanjin exercise can antagonize inflammatory reaction and myocardial tissue injury in patients with CHF by enhancing cardiopulmonary function, improving hypoxia, ischemia and other mechanisms. After treatment, the MLWHFQ sub item scoring of the study group were better than those of the conventional group; this is mainly because the study group realized the enhancement of exercise endurance, improved cardiopulmonary function and alleviated the clinical symptoms of CHF patients by persisting in practicing Baduanjin.
In conclusion, Baduanjin can enhance the cardiopulmonary function of CHF patients, antagonize the inflammatory reaction of patients, reduce myocardial injury, and enhance exercise endurance and intensity of patients, thus comprehensively improving the quality of life of patients. Therefore, Baduanjin can be widely used as a non-drug adjuvant therapy for CHF patients.
Conflict of interests:
The authors declared no conflict of interests.
References
- Dick SA, Epelman S. Chronic heart failure and inflammation: What do we really know? Circ Res 2016;119(1):159-76.
[Crossref] [Google Scholar] [PubMed]
- Li MP, Zhang YJ, Hu XL, Zhou JP, Yang YL, Peng LM, et al. Association of CKIP-1 P21A polymorphism with risk of chronic heart failure in a Chinese population. Oncotarget 2017;8(22):36545.
[Crossref] [Google Scholar] [PubMed]
- Li X, Qi W, Hu X. The effect of comprehensive cardiopulmonary rehabilitation on the cardiopulmonary function of elderly patients with chronic heart failure. Chin Med J 2020;36(5):430-2.
- Lee SH, Kim HS. Exercise interventions for preventing falls among older people in care facilities: A meta-analysis. Worldviews Evid Based Nurs 2017;14(1):74-80.
[Crossref] [Google Scholar] [PubMed]
- Huang R, Zhu R, Luo Y. Baduanjin health qigong therapy for adjuvant treatment of chronic heart failure. Shanxi Med J 2020;49(13):1666-8.
- Qi W, Song LP, Liu ZT, Chen L, Zhang HJ, Zhao W, et al. The effect of Baduanjin on cardiac function and quality of life in patients with chronic heart failure. Beijing Med J 2020;42(3):263-5.
- Liu H. The effect of exercise rehabilitation therapy on the cardiopulmonary function and quality of life of patients with chronic heart failure. J Chronic Dis 2020;21(10):1447-9.
- Li J. Effects of exercise rehabilitation therapy on exercise endurance, cardiopulmonary function and quality of life in patients with chronic stable heart failure. Int Med J 2019;14(5):557-66.
- Chinese society of cardiovascular diseases. Chinese heart failure diagnosis and treatment guidelines 2014. Chin J Cardiovasc Dis 2014;42(2):3-10.
- Cardiovascular disease professional committee of Chinese society of rehabilitation medicine, cardiovascular and cerebrovascular disease professional committee of Chinese society of gerontology. Chinese expert consensus on exercise rehabilitation of chronic stable heart failure. Chin J Cardiovasc Dis 2014(9):714 -20.
- Middel B, Bouma J, de Jongste M. Psychometric properties of the Minnesota Living with Heart Failure Questionnaire (MLHFQ). Clin Rehab Med 2001;15(5):489-500.
- Brake R, Jones ID. Chronic heart failure part 2: Treatment and management. Nurs Stand 2017;31(20):53-63.
[Crossref] [Google Scholar] [PubMed]
- Wan C, Xu X, Chen F. The effect of Shenmu San combined with Baduanjin on cardiac rehabilitation of patients with chronic heart failure. Guangming Tradit Chin Med 2020;35(21):3373-5.
- Li F. Observation on the curative effect of warming yang, nourishing qi, activating blood and distilling water combined with Baduanjin in treating chronic congestive heart failure. Inner Mongolia Tradit Chin Med 2020;39(7):128-9.
- Li X, Zhou R, Gan Y, Jiang X, Wen H. A randomized parallel controlled study of Baduanjin combined with western medicine for chronic ejection fraction retention and chronic heart failure. J Pract Tradit Chin Int Med 2019;33(3):56-9.
- Wang X, Mo X. Research progress in the application of Baduanjin in cardiac rehabilitation. J Integr Tradit Chin Western Med Cardio Cerebrovasc Dis 2019;17(5):703-5.
- Yu D, Jiang Z. The effects of Taijiquan and Baduanjin on exercise tolerance and quality of life in patients with chronic heart failure. New Chin Med 2019;51(3):274-7.
- Zhao D, Hu L, Sun J. The effect of Baduanjin combined with breathing training on the cardiopulmonary function of elderly patients with chronic heart failure. Chin J Geriatr Care Med 2020;18(4):9-11.
 Research group
Research group