- *Corresponding Author:
- Yubao Zhao
Department of Geriatric Medicine, Qujing First People’s Hospital, Qujing, Yunnan Province 655000, China
E-mail: zhaoyubao202312@163.com
| This article was originally published in a special issue, “Role of Biomedicine in Pharmaceutical Sciences” |
| Indian J Pharm Sci 2023:85(2) Spl Issue “41-46” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
A total of 120 chronic heart failure patients admitted to our hospital from June 2020 to October 2022 were randomly separated into observation group (receiving sacubitril/valsartan in combination with metoprolol therapy) and control group (receiving metoprolol treatment), with 60 cases in each group. The cardiac function indexes, myocardial injury indexes, inflammatory cytokines, oxidative stress index, occurrence of adverse reactions, NT-proB-type natriuretic peptide and treatment effects in both groups were assessed. After treatment, left ventricular end-diastolic dimension and left ventricular end-systolic diameter were lower, while left ventricular ejection fraction and stroke volume were higher in the observation group than the control group. Lactate dehydrogenase, creatine kinase-MB, cardiac troponin I, tumor necrosis factor-α, interleukin-6, C-reactive protein, malondialdehyde, NT-proB-type natriuretic peptide levels were declined, while total antioxidant capacity was elevated in the observation group in contrast to the control group. The observation group has lower occurrence rates of adverse reactions and higher total effective rates. To sum up, in the therapy of chronic heart failure, the use of sacubitril/valsartan combined with metoprolol can help to promote the cardiac function of patients, reduce the levels of inflammatory factors and clinical symptoms, and the therapeutic effect is good.
Keywords
Chronic heart failure, metoprolol, sacubitril/valsartan, cardiac function
Chronic Heart Failure (CHF), which has a high incidence in clinic, is a clinical syndrome that is directly related to inflammatory response and activation of the patient’s neuroendocrine system, thus leading to the dysfunction of the patient’s cardiac discharge function and changes in myocardial structure[1]. Through understanding the clinical manifestations of patients, it can be known that the clinical symptoms are mainly dyspnea and fluid retention, which have a high probability of disability and death for patients after the disease, so patients should be admitted to the hospital for treatment in time after the disease[2]. At present, vasodilation, diuresis and heart strength are taken as the key treatment contents in the clinical therapy of CHF, which is helpful to relieve the clinical manifestations of patients after treatment, but the overall prognostic treatment effect is not good[3]. Currently, it is recommended to give the patient drug treatment, among which metoprolol can inactivate the sympathetic nervous system of the patient, significantly promote the ventricular function of the patient, effectively regulate the heart rate, and significantly increase the coronary blood flow[4]. Sacubitril/valsartan has a good antihypertensive effect, with few side effects in patients, and its protective effect on myocardial remodeling will cause great inhibition[5]. Therefore, it is recommended to use sacubitril/valsartan combined with metoprolol in the therapy of CHF.
Herein, our study was intended to assess the therapeutic effect of sacubitril/valsartan combined with metoprolol in CHF therapy.
Materials and Methods
General data:
A total of 120 CHF patients admitted to our hospital from June 2020 to October 2022 were selected, followed by random separation into Observation Group (OG) along with Control Group (CG), with 60 cases in each group. In the CG, 40 males as well as 20 females were contained. The average age was (72.6±2.71) y, ranging from 62 y to 83 y. In the OG, 39 males together with 21 females were contained. The average age was (72.8±2.69) y, ranging from 61 y to 84 y. No statistical significance was discovered in the comparison of general data between both groups (p>0.05), reflecting comparability.
Methods:
Patients in the CG received metoprolol treatment. The patient was given metoprolol tartrate tablets (Shanghai Xinyi Bailu Da Pharmaceutical Co., Ltd., National drug approval H31021417) orally, twice/ day, 25 mg/time and the dosage were doubled after 1 w of medication.
Patients in the OG received sacubitril/valsartan in combination with metoprolol treatment. The treatment method of metoprolol was the same as that of CG. On this basis, patients were given sacubitril/ valsartan sodium tablets (Trade name: Novartis Singapore Pharmaceutical Manufacturing Private. Ltd. (Beijing Novartis Pharmaceutical Co., Ltd., National Drug approval number J20190001) orally, 1 time/day and 80 mg/time.
Observation indicators and judgment criteria:
Cardiac function indexes including Left Ventricular End-Diastolic Diameter (LVEDD), Left Ventricular Ejection Fraction (LVEF), Left Ventricular End- Systolic Diameter (LVESD) and Strike Volume (SV) were examined by Color Doppler ultrasound before and after treatment. Myocardial injury indexes, 5 ml of venous blood were extracted before and after treatment, and the upper serum was retained after centrifugation. The detection indexes included Lactate Dehydrogenase (LDH), Creatine Kinase Isoenzyme (CK-MB) along with myocardial troponin I (cTnI).
Inflammatory cytokines, containing Tumor Necrosis Factor-Alpha (TNF-α), Interleukin (IL)-6) as well as C-Reactive Protein (CRP). 5 ml of fasting venous blood was gathered from the patients before and after treatment. After serum separation, the changes of the above inflammatory indicators were measured by Enzyme-Linked Immunosorbent Assay (ELISA).
Oxidative stress index Malondialdehyde (MDA) together with Total Antioxidant Capacity (TAC) was measured by immunoturbidimetry method in fasting vein serum of patients with automatic biochemical analyzer. The occurrence of adverse reactions, including rash, dizziness, fatigue, abnormal renal function and bradycardia. N Terminal pro B Type Natriuretic Peptide (NT-proBNP) was evaluated based on the NT-proBNP test board.
Treatment efficacy criteria were obvious; patients’ clinical symptoms were significantly improved, cardiac function grade improvement ≥2. The patient’s clinical symptoms were improved, and the cardiac function grade was improved by 1 grade which was effective and no change in clinical symptoms which was ineffective.
Total effective rate=(obvious+effective)/total cases×100 %
Statistical analysis:
Statistical Package for the Social Sciences (SPSS) 19.0 statistical software was implemented for analysis. T-test was adopted for measurement data and Chi-square (χ2) test was adopted for counting data. p<0.05 was statistically significant.
Results and Discussion
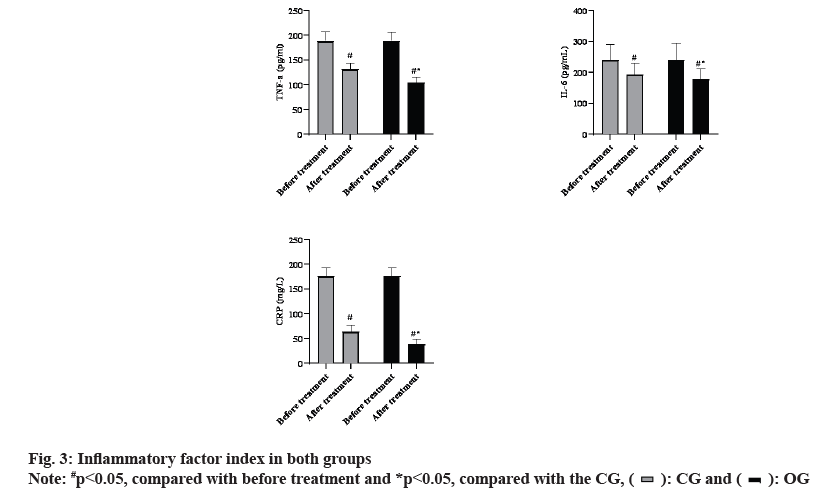
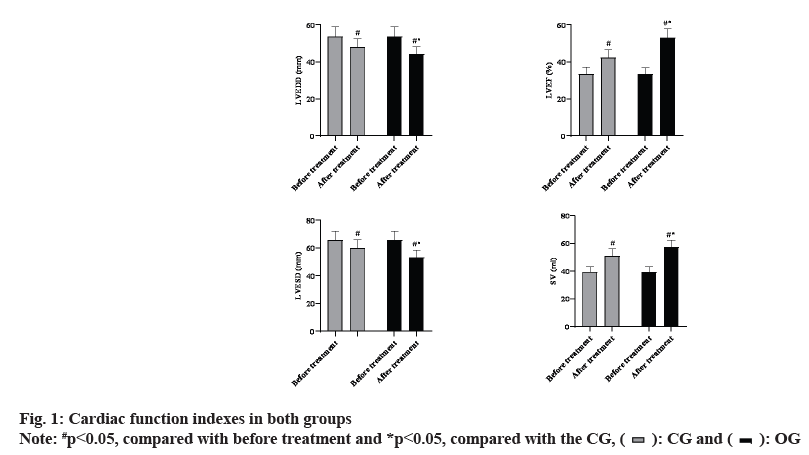
It was revealed in fig. 1 that, prior to treatment, no difference was observed in LVEDD, LVEF, LVESD as well as SV levels between both groups (p>0.05). After treatment, LVEDD and LVESD of the OG were declined in contrast to the CG, while LVEF and SV of the OG were elevated in comparison with the CG (p<0.05).
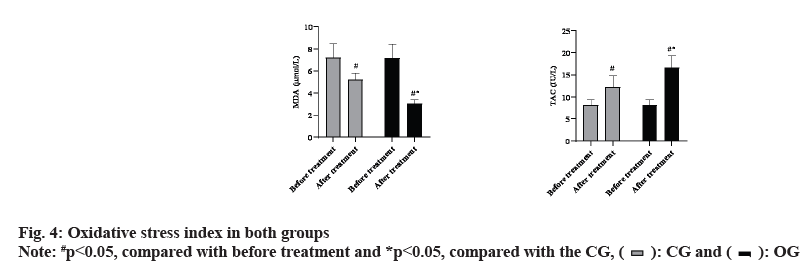
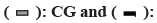
It was revealed in fig. 2 that, prior to treatment, no difference was observed in LDH, CK-MB and cTnI levels between both groups (p>0.05). After treatment, levels of the above myocardial injury indexes in the OG were declined in comparison with the CG (p<0.05). It was revealed in fig. 3 that, prior to treatment, no difference was discovered in TNF-α, IL-6 and CRP levels between both groups (p>0.05). After treatment, levels of the above inflammatory factors in the OG were declined in contrast to the CG (p<0.05).
It was revealed in fig. 4 that, prior to treatment, no difference was observed in MDA and TAC levels between both groups (p>0.05). After treatment, MDA of the OG was declined in contrast to the CG, while TAC of the OG was elevated in comparison with the CG (p<0.05). The incidence of adverse reactions in OG was declined in contrast to the CG (p<0.05) as shown in Table 1.
| Group | n | Rash | Dizziness | Fatigue | Abnormal renal function | Bradycardia | Total incidence rate (%) |
|---|---|---|---|---|---|---|---|
| OG | 60 | 0 | 1 | 1 | 0 | 0 | 2 (3.33 %) |
| CG | 60 | 1 | 1 | 2 | 1 | 3 | 8 (13.33 %) |
| χ2 | 3.93 | ||||||
| p | <0.05 | ||||||
Table 1: Occurrence of Adverse Reactions in Both Groups
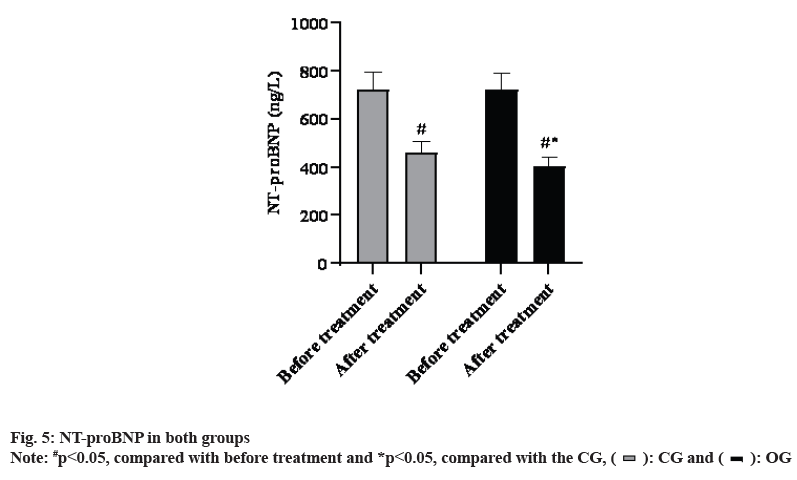
It was revealed in fig. 5 that, prior to treatment, no difference was discovered in NT-proBNP levels between both groups (p>0.05). After treatment, NTproBNP levels in the OG were declined in comparison with the CG (p<0.05). The total effective rate of OG was higher in comparison with the CG (P<0.05) as shown in Table 2.
| Group | n | Obvious effective | Effective | Ineffective | Total effective rate (%) |
|---|---|---|---|---|---|
| OG | 60 | 35 | 20 | 5 | 55 (91.67 %) |
| CG | 60 | 22 | 24 | 14 | 46 (76.67 %) |
| χ2 | 5.07 | ||||
| p | <0.05 | ||||
Table 2: Therapeutic Effect in Both Groups
CHF disease progresses rapidly after the onset of the patient, is unable to effectively control the rapid atrial fibrillation ventricular rate of the body, the rhythm is in a disordered state, the heartbeat rate is accelerated and a large amount of congestion appears in the organs and lungs[6]. During the therapy of CHF, it is necessary to improve the clinical symptoms of patients and eliminate the etiology as the main treatment content. At present, metoprolol and sacubitril/valsartan are the most extensively used drugs for CHF therapy[7,8]. Metoprolol can prolong the diastolic period, promote more relaxed cardiomyocytes, and have an organizing or delaying effect on the formation of decompensation[9]. However, if single drug therapy is used in the treatment of diseases, the inhibition will be enhanced and the use of a single dose will lead to further aggravation of the patient’s condition, and patients need long-term medication in the treatment of diseases[10]. The drug advantage of sacubitril/valsartan is to avoid the proliferation of myocardial epithelial cells, inhibit tissue fluid edema and vascular tension and improve the problem of insufficient cardiac output that cannot meet the needs of the body[11]. In clinical treatment, sacubitril/ valsartan is usually used in combination with other drugs.
The outcomes of this study displayed that, after treatment, LVEDD and LVESD in the OG were declined compared to the CG, while LVEF and SV in the OG were elevated compared to the CG. LDH, CK-MB along with cTnI levels of the OG were declined in contrast to the CG. TNF-α, IL-6 along with CRP levels in the OG were declined in contrast to the CG. MDA of the OG was declined in contrast to the CG, while TAC of the OG was elevated in contrast to the CG. The incidence of adverse reactions in OG was declined in contrast to the CG. NT-proBNP levels in the OG were declined in contrast to the CG. The total effective rate of OG was higher in contrast to the CG. All above data suggested that the combination of metoprolol and sacubitril/valsartan could effectively improve cardiac function, alleviate myocardial injury, reduce inflammatory response, oxidative stress reaction and the incidence of adverse reactions, as well as have a better therapeutic effect than metoprolol alone, which were consistent with previous literature[12,13].
On the one hand, the combination of the two drugs can reduce the myocardial load and cardiac load by lowering blood pressure; on the other hand, it can reduce the oxidative stress response by reducing the release of aldosterone and promote the improvement of patient’s cardiac function. Since CK-MB and cTnI are the main markers to reflect myocardial injury (ischemia and hypoxia)[14], combined therapy can improve cardiac function, reduce the levels of inflammatory factors and oxidative stress response, reduce endogenous sympathetic nerve activity in vivo, delay or reverse cardiac remodeling process, and reduce myocardial oxygen consumption. The myocardial damage caused by oxygen free radicals is reduced, and the myocardial damage index of patients is improved.
After observing the function of cardiac Beta (β) 3 receptor in human body, the contractility and agility of cardiomyocytes will be weakened under the effect of this index, which will lead to the failure of synthesis of Adenine Nucleoside Triphosphate (ATP), so as to achieve the purpose of regulation, avoid the synthesis of calcium ions and play an inhibitory role in toxins[15]. Metoprolol inhibits the proliferation of β3 receptors and enhances β1 division[16]. In addition, through the understanding of the medication mechanism of metoprolol, it can effectively block the sympathetic nerve pathway, thus destroying the negative feedback regulation of heart rate disorder, slowing down the malignant process, and promoting the reduction of NT-proBNP index[17]. The upregulation of β receptors helps to prevent the oversensitivity of catecholamine, while inhibiting renin to prevent damage to the cardiovascular circulatory system of patients[18]. The use of metoprolol drugs in treating CHF diseases will act in the local position of the patient’s heart and complete the mobilization of the systemic circulatory-neuro-endocrine system, but clinical studies have confirmed that the clinical treatment effect of metoprolol drug alone is not good, which will cause great stimulation to the patient’s circulatory system[19], so it is recommended to combine with sacubitril/valsartan in the therapy of CHF diseases to reduce the loss of sodium ions and, avoid water and sodium retention, has a blocking effect on aldosterone and angiotensin II, thereby reducing the patient’s peripheral resistance and cardiac load.
In conclusion, in the therapy of CHF, the use of sacubitril/valsartan combined with metoprolol can help to promote the cardiac function of patients, reduce the level of inflammatory factors and clinical symptoms, and the therapeutic effect is good.
Conflict of interests:
The authors declared no conflict of interests.
References
- Hoffman TM. Chronic heart failure. Pediatr Crit Care Med 2016;17(8):S119-23.
[Crossref] [Google Scholar] [PubMed]
- Ziaeian B, Fonarow GC. Epidemiology and aetiology of heart failure. Nat Rev Cardiol 2016;13(6):368-78.
[Crossref] [Google Scholar] [PubMed]
- McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2021;42(36):3599-726.
[Crossref] [Google Scholar] [PubMed]
- Cheng X, Zhu M, Liu Q, Feng Z, Meng Y. Effectiveness of metoprolol in improving cardiac and motor functions in patients with chronic heart failure: A prospective study. Drug Des Dev Ther 2020:3485-94.
[Crossref] [Google Scholar] [PubMed]
- Pontremoli R, Borghi C, Perrone Filardi P. Renal protection in chronic heart failure: Focus on sacubitril/valsartan. Eur Heart J Cardiov Pharmacother 2021;7(5):445-52.
[Crossref] [Google Scholar] [PubMed]
- Dick SA, Epelman S. Chronic heart failure and inflammation: What do we really know? Circ Res 2016;119(1):159-76.
[Crossref] [Google Scholar] [PubMed]
- Hjalmarson Å, Goldstein S, Fagerberg B, Wedel H, Waagstein F, Kjekshus J, et al. Effects of controlled-release metoprolol on total mortality, hospitalizations and well-being in patients with heart failure: The metoprolol CR/XL randomized intervention trial in congestive heart failure (MERIT-HF). JAMA 2000;283(10):1295-302.
[Crossref] [Google Scholar] [PubMed]
- Pieske B, Wachter R, Shah SJ, Baldridge A, Szeczoedy P, Ibram G, et al. Effect of sacubitril/valsartan vs. standard medical therapies on plasma NT-proBNP concentration and submaximal exercise capacity in patients with heart failure and preserved ejection fraction: The PARALLAX randomized clinical trial. JAMA 2021;326(19):1919-29.
[Crossref] [Google Scholar] [PubMed]
- Prakash A, Markham A. Metoprolol: A review of its use in chronic heart failure. Drugs 2000;60(3):647-78.
[Crossref] [Google Scholar] [PubMed]
- Sessa M, Mascolo A, Mortensen RN, Andersen MP, Rosano GM, Capuano A, et al. Relationship between heart failure, concurrent chronic obstructive pulmonary disease and beta-blocker use: A Danish nationwide cohort study. Eur J Heart Fail 2018;20(3):548-56.
[Crossref] [Google Scholar] [PubMed]
- Abdin A, Schulz M, Riemer U, Hadëri B, Wachter R, Laufs U, et al. Sacubitril/valsartan in heart failure: Efficacy and safety in and outside clinical trials. ESC Heart Fail 2022;9(6):3337-50.
[Crossref] [Google Scholar] [PubMed]
- Ding Y, Wei Z, Li J, Zhu L. Effects of metoprolol succinate combined with entresto on cardiac function indexes and coagulation function in patients with congestive heart failure. Comput Math Methods Med 2022;2022:9765884.
[Crossref] [Google Scholar] [PubMed]
- Xu X, Yang Y, Zhou G, Du Z, Zhang X, Mao W, et al. Clinical efficacy of qili qiangxin capsule combined with western medicine in the treatment of chronic heart failure: A systematic review and meta-analysis. Evid Based Complement Alter Med 2021;2021:1-8.
[Crossref] [Google Scholar] [PubMed]
- Zhao B, Sun S, Wang Y, Zhu H, Ni T, Qi X, et al. Cardiac indicator CK-MB might be a predictive marker for severity and organ failure development of acute pancreatitis. Annal Transl Med 2021;9(5):368.
[Crossref] [Google Scholar] [PubMed]
- Motiejunaite J, Amar L, Vidal-Petiot E. Adrenergic receptors and cardiovascular effects of catecholamines. Annal Endocrinol 2021;82(3-4):193-7.
[Crossref] [Google Scholar] [PubMed]
- Al Katat A, Zhao J, Calderone A, Parent L. Sympathetic stimulation up regulates the Ca2+ channel subunit, CaVα2δ1, via the β1 and ERK 1/2 pathway in neonatal ventricular cardiomyocytes. Cells 2022;11(2):188.
[Crossref] [Google Scholar] [PubMed]
- Ye L, Hu G, Yu H, Sun J, Yuan H. Metoprolol improves myocardial remodeling and cardiac function in patients with permanent pacemaker implantation. J Healthc Eng 2022;2022:7340992.
[Crossref] [Google Scholar] [PubMed]
- Steinberg SF. Beta1-adrenergic receptor regulation revisited: The role of the extracellular N-terminus. Circ Res 2018;123(11):1199-201.
- Jagdale SC, Chede SM, Gulwady R, Kuchekar BS, Lokhande PD, Shah TP, et al. Pulsatile multiparticulate drug delivery system for metoprolol succinate. Arch Pharm Res 2011;34(3):369-76.
[Crossref] [Google Scholar] [PubMed]
 OG
OG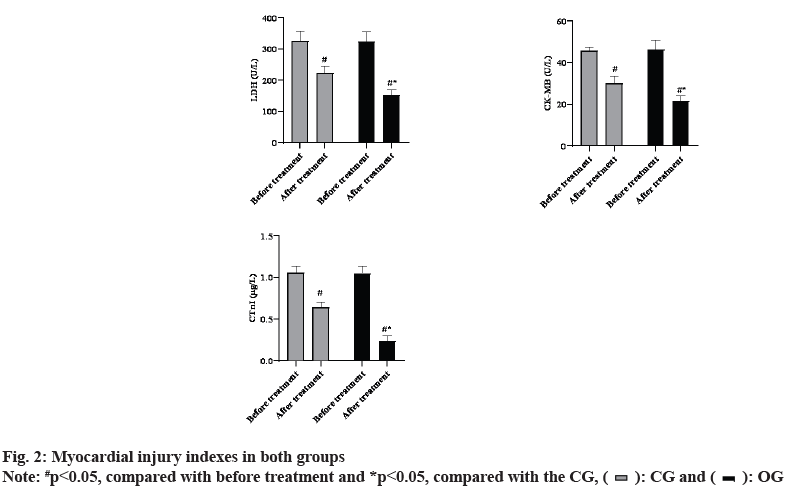
 OG
OG