- *Corresponding Author:
- Wen Qing Wang
Department of General Surgery, Taikang Xianlin Drum Tower Hospital, The Affiliated Hospital of Nanjing University Medical School, Nanjing, Jiangsu 210046, China
E-mail: 251590152@qq.com
| This article was originally published in a special issue, “Clinical Research in Pharmaceutical and Biomedical Sciences” |
| Indian J Pharm Sci 2021:83(1)Spl issue1;43-48 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To explore the practicability, feasibility and wound aesthetics of Gimmi ultra micro instrument in laparoscopic cholecystectomy. To retrospective analysis the clinical data of 75 patients undergoing elective surgery for gallbladder stones with chronic cholecystitis, gallbladder polyps and chronic cholecystitis who were admitted to the Department of General Surgery, Taikang Xianlin Drum Tower Hospital, Nanjing University School of Medicine, from October 2019 to October 2020. Among them, 35 cases used gimmi ultra micro instrument to remove the gallbladder (ultra-minimally invasive group) and 40 cases used the traditional three-hole method to remove the gallbladder (traditional group). The operation time, blood loss during operation, postoperative ventilation time, pain scores on the 1st and 3rd d after surgery, shortterm complications such as postoperative bleeding and bile leakage, incision scar satisfaction score, total hospital stay were compared between the two groups of patients and other indicators. Both groups of patients recovered and discharged without any bleeding or bile leakage after operation. The operation time of the ultra-minimally invasive group was slightly longer than that of the traditional group. There was no significant difference in the amount of blood loss, postoperative ventilation time and incision infection (p>0.05). The ultra-minimally invasive group was better than the traditional group in total hospital stay (p<0.05), on the 1st and 3rd d after operation, the ultra-minimally invasive group was better than the traditional group (p<0.05) and the ultra-minimally invasive group was significantly better than the traditional group (P<0.05). The gimmi ultra micro instrument is safe and reliable in laparoscopic cholecystectomy, the operation is not difficult, the postoperative pain of patients is low, the cosmetic effect is accurate and it is worthy of clinical application.
Keywords
Ultra-minimally invasive, Gimmi laparoscopic ultramicro instrument, laparoscopic cholecystectomy
Laparoscopic cholecystectomy is more and more widely used in the treatment of acute and chronic cholecystitis, asymptomatic gallstone, simple cholecystitis, gallbladder contraction dysfunction, gallstone pancreatitis and gallbladder polyps[1-2]. With the advantages of small trauma and rapid recovery, it has rapidly become the gold standard for the treatment of benign gallbladder Complications of laparoscopic gallbladder removal do not happen often. They can include bleeding, infection in the surgery area, hernias, blood clots, and heart problems. A hernia is when a small amount of your gut (intestine) or other tissue bulges through the muscles that cover it[3]. With the development of minimally invasive surgery and the continuous improvement of medical equipment, laparoscopic cholecystectomy has also developed a variety of improved methods, from the most classic four hole method to less invasive three hole, improved two hole, transumbilical single hole and natural orifice transluminal endoscopic surgery. However, due to ethical problems,high difficulty of operation and economic factors, it is difficult to popularize some improved surgical methods. On this basis, we use gimmi laparoscopic ultramicro instrument to further improve this kind of operation, so as to reduce the incision and achieve satisfactory minimally invasive effect. Therefore, we retrospectively analyzed the clinical data of 75 patients with cholecystolithiasis or gallbladder polyps complicated with chronic cholecystitis who underwent elective surgery in the general surgery department of our hospital from October 2019 to October 2020 and divided them into the Ultra minimally invasive group and Traditional group to explore the application value of Ultra minimally invasive technology in laparoscopic cholecystectomy.
Materials and Methods
General information:
75 patients with cholecystolithiasis or gallbladder polyps complicated with chronic cholecystitis who underwent elective surgery in the general surgery department of Taikang Xianlin Drum Tower Hospital from October 2019 to October 2020 were retrospectively analyzed and divided into the Ultra minimally invasive group and Traditional group. There were no significant statistical differences in general information between the two groups (p>0.05), as shown in Table 1.
| Group | N | Gender | Age | BMI | |
|---|---|---|---|---|---|
| Male | Female | (y) | (Kg/m2) | ||
| Traditional group | 40 | 18 | 22 | 50.15±14.71 | 24.875±2.97 |
| Ultra-minimally invasive group | 35 | 15 | 20 | 52±12.54 | 24.714±3.04 |
| t/?2 | 0.035 | -0.582 | 0.231 | ||
| p | 0.852 | 0.563 | 0.818 | ||
Table 1: Comparison of General Information between the Two Groups
Inclusion and exclusion criteria:
Inclusion criteria: All patients were confirmed by B-ultrasound and Magnetic resonance cholangiopancreatography (MRCP) examination and met the criteria of elective surgery and the case data were complete. All patients signed the relevant operation consent and actively cooperated with relevant treatment and inquiry.
Exclusion criteria: Diagnosed with Acute cholecystitis; Complicated with infectious diseases; Complicated with liver cancer, gallbladder cancer and gastrointestinal tumor; Complicated with severe heart and lung dysfunction; Complicated with hematological diseases; Complicated with severe mental disorders; Unwillingness to cooperate with diagnosis and treatment.
Introduction of special equipment:
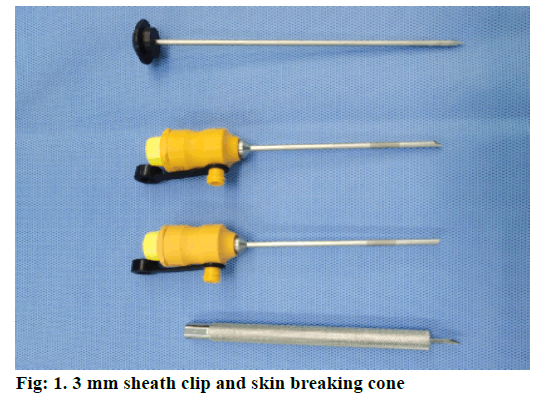
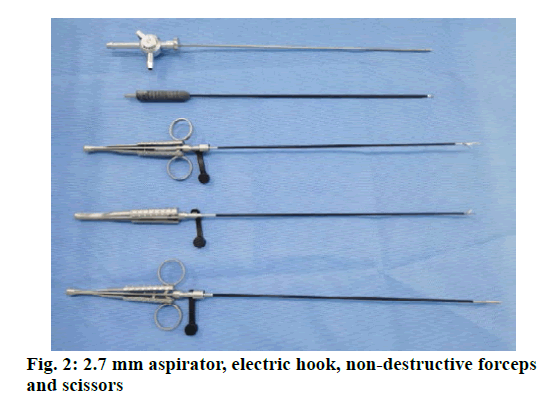
Surgical instruments used in the Traditional group: Hangzhou Kangji Medical Equipment Co., Ltd. Surgical instruments used in the Ultra-minimally invasive group: Gimmi, Germany (fig. 1 & fig. 2).
Surgical methods:
Traditional group
After tracheal intubation, patients under general anesthesia were placed in supine position and the operation field was routinely disinfected. Incision the navel 1.2 cm enters the abdomen under direct vision, place a 10 mm sheath clip and set the intraabdominal pressure of 14 mmHg. The body position was modified as head high foot low position and left lying position, about 30 degrees, respectively. A 10 mm sheath clip was placed under the xiphoid process while a 5 mm sheath clip was placed under the right costal margin to implant the laparoscopy and corresponding instruments, respectively. The cystic duct and blood vessels of the gallbladder were dissociated through the posterior triangle approach and then cut off after being clamped with absorbable clamp. The gallbladder bed was separated along and retrogrades and the gallbladder was completely stripped and put into the bag. After confirming that there was no active bleeding, the subxiphoid sheath card was removed under the monitoring of endoscopy. After excluding the pneumoperitoneum, the remaining sheath card was removed. Then the bag containing gallbladder was taken out from the umbilicus and each incision was sutured and bonded with fibrin glue layer by layer. Make sure there was no subcutaneous emphysema on the abdominal wall. The gallbladder was sent to the patient’s family members for examination and patients were returned to Pediatric Intensive Care Unit (PICU).
Ultra-minimally invasive group
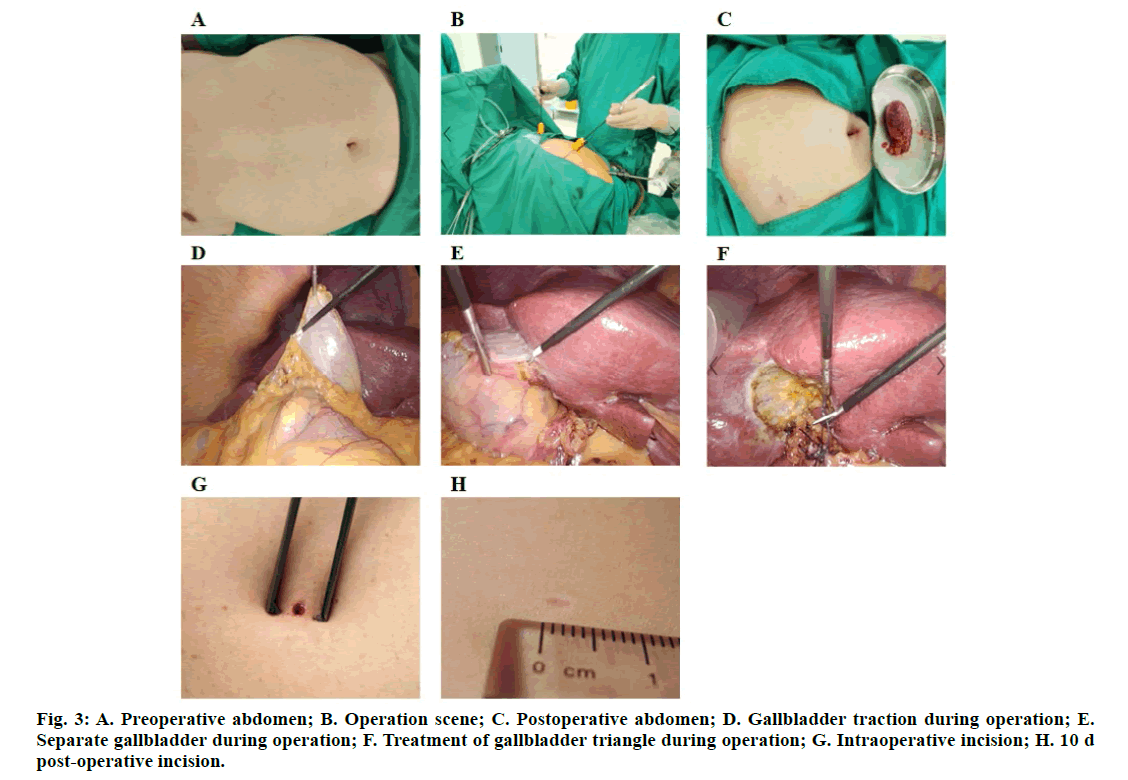
GIMMI laparoscopic ultramicro instruments were used in the ultra-minimally invasive group. The surgery method was the same as the traditional group except for some details. The original scabbard clips of 10 mm and 5 mm below the xiphoid process and right costal margin were changed into gimmi 3 mm puncture needle to puncture the skin and gimmi 3 mm special sheath clip was placed. Gimmi special 2.7 mm ultraminimally invasive electric hook (general equipment), non-invasive straight separation forceps, noninvasive separation curved forceps and aspirator (general equipment) were used. The cystic duct was cut off after double looped or ligated followed with looped with 2-0 absorbable suture, and the gallbladder vessels were cut off after looped or ligated with 3-0 absorbable suture. After the gallbladder was put into the bag, it was taken out from the umbilicus and the 3 mm incision was directly bonded with fibrin glue (fig. 3 A-H).
Observed indexes:
The operation time, blood loss, postoperative ventilation time, 1 d and 3 d postoperative pain degree, satisfaction of incision and hospital stay were compared between the two groups. The pain degree was evaluated using visual analog scale (VAS), with a range of 0-10 points, the higher the points, the stronger the pain. The satisfaction of incision was evaluated using a score system (10 points system): 0-1 points meant very dissatisfied, 2-3 points meant dissatisfied, 4-5 points meant not very satisfied, 6-7 points meant basically satisfied, 8-9 points meant satisfied, 10 points meant very satisfied, the higher of the score, the higher of the satisfaction.
The incidence of short-term complications such as postoperative bleeding, gallbladder and so on was recorded.
Statistical methods:
SPSS 22.0 was used to analyze the data. The measurement data in accordance with normal distribution was expressed as (x±s) and analyzed with t test. The measurement data that did not conform to the normal distribution were expressed as M (p25, p75) and analyzed with the Mann Whitney U test. Chi square test or Fisher exact probability method was used for counting data. p<0.05 meant the difference was statistically significant.
Results and Discussion
The patients in both groups recovered smoothly and discharged without bleeding and bile leakage. The median time of operation time in the Traditional group was 40 min, which was shorter than that of the Ultraminimally invasive group (55 min, p<0.05). There was no significant difference in blood loss between the traditional group (35 ml) and the ultra-minimally invasive group (30 ml, p>0.05). There was no significant difference in postoperative ventilation time between the traditional group and the ultra-minimally invasive group, with a median of 18 h and 20 h, respectively (p>0.05). The total hospital stay of the ultra-minimally invasive group was 5.68±1.20 d, which was shorter than that of the traditional group (6.36±1.34, p<0.05). There were 2 cases of incision infection in the traditional group and 0 in the ultra-minimally invasive group, though no significant statistical difference was found (p>0.05). The score of satisfaction of incision of the ultra-minimally invasive group was 9 points, which was significantly better than that of the traditional group (8 points, p<0.05), as shown in Table 2.
| Group | Operation time (min) | Blood loss (ml) |
Ventilation time (h) | Hospital stay (d) | Incision infection | Satisfaction of incision |
|---|---|---|---|---|---|---|
| Traditional group | 40 (30,45) | 35 (20,40) | 18 (15,26) | 6.36±1.34 | 2 | 8 (7,8) |
| Ultra-minimally invasive group | 55 (45,65) | 30 (25,40) | 20 (14,24) | 5.68±1.20 | 0 | 9 (9,10) |
| Z/χ2 | -4.881 | -0.167 | -0.554 | 2.316 | / | -5.804 |
| p | 0.000 | 0.867 | 0.58 | 0.023 | 0.498 | 0.000 |
Table 2: Comparison of Observed Indexes between the Two Groups
The VAS score of the traditional group was 4 points 1 d post-operation, while that of the ultra-minimally invasive group was 2 points. And the VAS score of the traditional group was 2 points 3 d post-operation, while that of the ultra-minimally invasive group was 1 point. Both the differences were statistically significant, as shown in Table 3.
| Group | 1 d post-operation | 3 d post-operation |
|---|---|---|
| Traditional group | 4(3,5) | 2(1,2) |
| Ultra-minimally invasive group | 2(2,3) | 1(1,2) |
| Z | -5.908 | -2.708 |
| p | 0.000 | 0.007 |
Table 3: Comparison of Pain Scores between the Two Groups
With the development of minimally invasive surgery and the continuous improvement of medical equipment,laparoscopic cholecystectomy has developed a variety of improved methods, from the most classic fourhole method to less invasive three-hole, improved two-hole, transumbilical single hole and natural orifice transluminal endoscopic surgery (NOTES). At present, the feasible modified two-hole method still needs multi trocar operation or auxiliary suspension. Suture hanging gallbladder is easy to cause gallbladder wall avulsion bleeding or bile overflow. Ranendra hajong showed that the probability of bile leakage in two-hole Laparoscopic Cholecystectomy (LC) reached 29 %, and two-hole LC may increase the incidence of postoperative abdominal abscess[4]. Nath SK found that the exposure angle of gallbladder was fixed after suspension, which was not conducive to anatomical exposure when the gallbladder was large[5]. What’s more, the double trocar operation in the same puncture hole will cause “chopstick effect”. Therefore, the improved two-hole method has higher requirements on the selection of cases and the operator’s technical level, which is only applicable to the non-inflammatory period and the situation without abdominal adhesion.
NOTES is still in the research stage and has not been widely carried out. The United States began to conduct preclinical feasibility study in 2004. A prospective randomized clinical trial jointly launched by the American Society of gastroenteroscopy surgeons and the American Society of gastroenteroscopy for Natural Orifice Surgery Consortium for Assessment and Research (NOSCAR) showed that, except for pain score, NOTES has no statistical difference with laparoscopic group in other aspects, including cosmetic effects[6]. A multicenter study in Switzerland has shown that NOTES has higher operation difficulty, conversion rate and incidence of complications than single port laparoscopic surgery and the surgeon’s self-evaluation is lower than that of single port laparoscopic surgery[7]. Transumbilical single port laparoscopic surgery is the most feasible minimally invasive surgical technique at this stage[8], but single port instruments have higher requirements on operation technology. Meta-analysis of Laura Evers shows that transumbilical single port laparoscopic surgery has no advantages over traditional LC except pain and cosmetic effect[9]. A randomized controlled trial conducted by Amro on American surgeons in 2015 showed that the pressure and physical requirements of doctors during single hole operation were significantly higher than those of traditional laparoscopic surgery by measuring the surgeon’s heart rate, salivary cortisol level, instrument availability survey and the surgery task load index (Surg TLX) score[10]. This is also one of the reasons why it has not been widely promoted. At the same time, a study by Madureira FA showed that patients undergoing single port cholecystectomy had a higher incidence of postoperative incisional hernia compared with conventional laparoscopic cholecystectomy[11].
In view of this situation, we tried to use the three hole method with gimmi laparoscopic ultra-micro instruments, so as to further reduce the incision to the maximum extent through ultra-minimally invasive technology and improved surgical instruments. We found that the pain of LC patients mostly came from the subxiphoid sheath hole and some patients’ pain even lasted for several months. Different from the location of sheath entrapment of traditional three hole method (10 mm below xiphoid process and 5 mm below right costal margin), we used 3 mm ultrafine sheath clamp to obtain the same wide operation space and reduce the incision to control the damage to the abdominal wall in a very small extent. Thus, the pain of stabbing hole under xiphoid process was hardly felt after operation. At the same time, the operation is completely the same as the three hole method, which is simple and easy to use. Grassroots doctors with laparoscopic cholecystectomy experience can quickly complete the learning curve after being familiar with the instruments. After comparison, we found that compared with the traditional three hole surgery, there was no bleeding, bile leakage and other conditions (p>0.05) and there was no significant difference in the amount of bleeding and postoperative ventilation time (p>0.05), suggesting that the use of ultra-minimally invasive instruments did not increase the incidence of surgical complications. The pain score of the ultra-minimally invasive group was better than that of the traditional group 1 and 3 d after operation (p<0.05) and the score of satisfaction of incision in the ultra-minimally invasive group was better than that in the traditional group (p<0.05). Besides, the total hospital stay of the ultra-minimally invasive group was shorter than that of the traditional group (p<0.05). Compared with surgery in the traditional group, we summarized different experience in the ultra-minimally invasive group as follows. Because the traditional absorbable clamp and locking clip could not be placed in the 3 mm trocar hole, the traditional suture was used to ligate the cystic duct. Besides, as the diameter of the gripper is too small and the strength is not enough, it is often unable to tighten when using two grab tongs at the same time. So, when tying a knot, one end of the thread should be left in the body through trocar and put a claw clamp into the same operation hole to grasp the other end of the thread and push forward. Thus, the direction of force conduction is changed from the angle between the thread and the gripper to parallel with the gripper to maintain enough tension to fully tighten the knot. In order to ensure that the knot will not fall off, we should tie the cystic duct with a bandage device after tying and cutting off the cystic duct. This is also the reason why the operation time in the ultra-minimally invasive group is slightly longer than that in the traditional group.
In conclusion, the gimmi ultramicro instrument is safe and reliable in laparoscopic cholecystectomy, the operation is not difficult, the postoperative pain of patients is low, the cosmetic effect is accurate and it is worthy of clinical application.
Conflicts of interest
The authors report no conflicts of interest.
Acknowledgements
This work was supported by Taikang Xianlin Drum Tower Hospital, The Affiliated Hospital of Nanjing University Medical School.
References
- Kapoor T, Wrenn SM, Callas PW, Abu-Jaish W. Cost analysis and supply utilization of laparoscopic cholecystectomy. Minim Invasive Surg 2018;2018:7838103.
- Strasberg SM. Tokyo Guidelines for the Diagnosis of Acute Cholecystitis. J Am Coll Surg 2018;227:624.
- Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, et al. Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc 2010;24:1842-8.
- Hajong R, Khariong PD. A comparative study of two-port versus three-port laparoscopic cholecystectomy. J Minim Access Surg 2016;12:311.
- Nath SK. Reduced Port Laparoscopic Cholecystectomy: Single and a Half Incision Lap Chole. Indian J Surg 2016;78:425-7.
- Schwaitzberg SD, Roberts K, Romanelli JR, Desilets DJ, Earle D, Horgan S, et al. The NOVEL trial: natural orifice versus laparoscopic cholecystectomy-A prospective, randomized evaluation. Surg Endosc 2018;32:2505-16.
- Steinemann DC, Zerz A, Adamina M, Brunner W, Keerl A, Nocito A, et al. Single-incision and natural orifice translumenal endoscopic surgery in Switzerland. World J Surg 2017;41:449-56.
- Langwieler TE, Nimmesgern T, Back M. Single-port access in laparoscopic cholecystectomy. Surg Endosc 2009;23:1138-41.
- Evers L, Bouvy N, Branje D, Peeters A. Single-incision laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy: A systematic review and meta-analysis. Surg Endosc 2017;31:3437-48.
- Abdelrahman AM, Bingener J, Yu D, Lowndes BR, Mohamed A, McConico AL, et al. Impact of single-incision laparoscopic cholecystectomy (SILC) versus conventional laparoscopic cholecystectomy (CLC) procedures on surgeon stress and workload: a randomized controlled trial. Surg Endosc 2016;30:1205-11.
- Madureira FA, Gomez CLT, Almeida EM. Comparison between incidence of incisional hernia in laparoscopic cholecystectomy and by single port. ABCD Arq Bras Cir Dig 2018;31:e1354.