- *Corresponding Author:
- Lili Wang
Department of Respiration, Lianshui County People’s Hospital, Huai’an 223400, China
E-mail: zsg_yf@163.com
| This article was originally published in a special issue, “Evolutionary Strategies in Biomedical Research and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2021:83(3) Spl issue;222-226 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
This study aims to observe and analyze the diagnostic value of T-cell enzyme linked immunospot assay for tuberculosis infection during the diagnosis of pulmonary tuberculosis and extrapulmonary tuberculosis. The study objects were 200 cases of tuberculosis patients in the outpatient department or inpatient department of our hospital, including 100 patients with active pulmonary tuberculosis, 100 patients with extrapulmonary tuberculosis. Meanwhile, we selected 90 non pulmonary tuberculosis patients with pulmonary disease, 90 cases of extrapulmonary nontuberculous disease and 90 cases with health examination. T-cell enzyme linked immunospot test for tuberculosis infection was used to detect tuberculosis antigen specificity and the frequency of T cells secreting Interferon gamma and the results were analyzed in detail. The positive rate of T-cell enzyme-linked immunospot assay for tuberculosis infection in pulmonary tuberculosis group was higher than that in non-pulmonary tuberculosis group and healthy control group (p<0.05). The positive rate of pulmonary tuberculosis group was significantly higher than that of non-pulmonary tuberculosis group and healthy control group (p<0.05). The diagnostic sensitivity of T-cell enzyme linked immunospot assay for tuberculosis infection was 88.56 % to bacteriological positive tuberculosis, 80.25 % to bacteriological negative tuberculosis and 93.36 % to extrapulmonary tuberculosis. The diagnosis specificity was respectively 85.67 %, 84.36 %, 89.73 %, the positive predictive values were respectively 93.95 %, 88.79 % and 96.56 %, while the negative predictive values were 74.00 %, 74.00 % and 80.00 %, respectively. By comparing the bacteriological positive tuberculosis and bacteriological negative tuberculosis, there is no significant difference in diagnostic efficiency of T-cell enzyme linked immunospot assay for tuberculosis infection (p>0.05). In comparison of extrapulmonary tuberculosis group, bacteriological negative pulmonary tuberculosis and bacteriological positive pulmonary tuberculosis group, result showed that T-cell enzyme linked immunospot assay for tuberculosis infection diagnostic efficacy was not statistically significant (p>0.05). T-cell enzyme linked immunosorbent assay has ideal sensibility, specificity in diagnosis of tuberculosis infection, which can be widely used in diagnosis of extrapulmonary tuberculosis and bacteriological negative pulmonary tuberculosis.
Keywords
T-cell enzyme linked immunospot assay for tuberculosis infection, pulmonary tuberculosis, extrapulmonary tuberculosis, diagnostic value, application significance
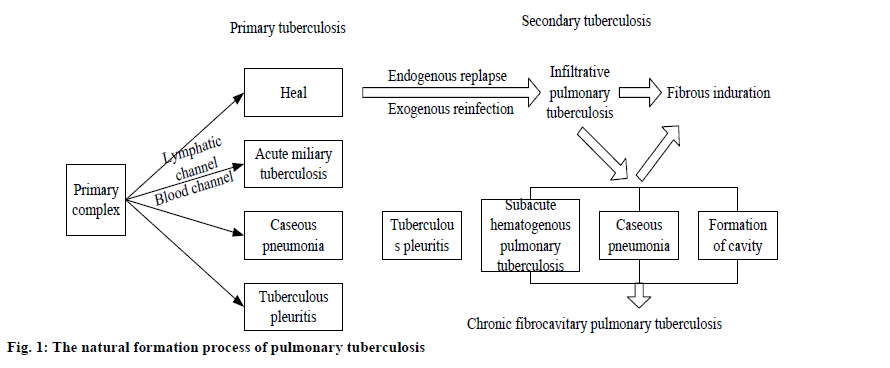
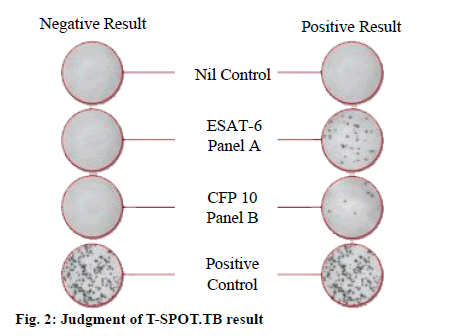
At present, one of the global public issues is tuberculosis. According to World Health Organization (WHO) statistics, around the world, about 2 billion people have Mycobacterium tuberculosis infection and tuberculosis deaths number 2 million people each year[1]. China is one of the 22 countries with high burden of tuberculosis in the world, ranking second. According to epidemiological survey results, every year, about 130 000 people die of tuberculosis. Hence, tuberculosis has become a national and even the world’s key controlled disease[2]. Tuberculosis has a variety of clinical manifestations and its natural formation process is shown in fig. 1 below. Tuberculosis can involve multiple systems of the body. With hidden or atypical symptoms, extrapulmonary tuberculosis is very prone to misdiagnosis, which causes a certain degree of difficulty for clinical diagnosis. There are many commonly used ways to detect Mycobacterium tuberculosis, including acid fast staining, culture and tuberculin test and tuberculosis antibody detection. Due to the defects of low sensitivity, specificity and relatively long detection cycle, it can no longer adapt to the current clinical development needs[3,4]. In recent years, with the continuous development of medical industry and update in new detection technology, T-cell enzyme linked immunospot assay for tuberculosis infection (T-SPOT.TB), with higher sensitivity and specificity, achieves good result in diagnosis of combined infection and is widely used. This study was to analyze value of T cell enzyme-linked immunospot assay for tuberculosis infection (T-SPOT.TB) in the diagnosis of tuberculosis and extrapulmonary tuberculosis. This study was to investigate 200 cases of tuberculosis patients in the outpatient department or inpatient department of respiratory medicine department of our hospital from August 2014 to August 2016. Including 108 males and 92 females, the patients were aged 19 to 80 y, with mean age at (42.18±12.34) y. Tuberculosis group included 100 cases, with 65 cases and 35 cases respectively with positive and negative sputum acid fast bacilli smear. The extrapulmonary tuberculosis group included 100 cases respectively with 38 cases, 22 cases, 18 cases, 10 cases, 7 cases, 5 cases of tuberculous pleurisy, tuberculous meningitis, lymphatic tuberculosis, tuberculosis peritonitis, pelvic tuberculosis and bone tuberculosis. All enrolled patients met the following conditions: Cases were clinically diagnosed as tuberculosis though there still lack etiological basis, which were effectively treated by diagnostic anti tuberculosis treatment; Mycobacterium tuberculosis culture showed positive in sputum or cheese necrotic granulomatous biopsy specimen. Exclusion criteria: With silicosis, diabetes, cancer; with positive antibody in human immunodeficiency virus detection; pregnancy, breast feeding women; mental disorders. In addition, 90 cases were selected as non-tuberculosis group, including 70 patients with extrapulmonary nontuberculous disease patients and 20 patients with pulmonary disease (non-tuberculosis). Moreover, 90 healthy persons were selected as the control group. First, samples were collected: Peripheral venous blood (8 ml) of the research objects was put into the cell preparation tube (CPT) vessels containing sodium citrate, to be centrifuged at 1600 g for 30 min at 18°[5]. Then, the mononuclear cell layer in the CPT tube was transferred to new sterile 15 ml tip bottom centrifuge tube, AIM-V medium (10 ml) was added, to be centrifuged at 600 g for 8 min at 18°. The supernatant was removed and AIM-V (1 ml) was added. The AIM-V culture solution was added to 10 ml after resuspension of the cell pellet, to be centrifuged at 350 g for 8 min at 18°[6] After the centrifugation, the supernatant was removed and the cells were resuspended in AIM-V culture (0.7 ml). After dilution of the mixed cell suspension, the cells were counted and concentration of the cell suspension was adjusted appropriately (2.5×106/ml) on the basis of the counting results. Next, carry out the enzyme linked immunospot assay: AIM-V cell culture medium (50 μl) was added to 4 holes with anti-Interferon gamma (IFN-γ) antibody micro plate as negative control, while positive control was 50 μl phytohemagglutinin[7]. The 50 μl Mycobacterium tuberculosis specific hybrid polypeptide A, i.e., early secretory antigenic target (ESAT)-6 antigen, was taken as test hole A and 50 µl Mycobacterium tuberculosis specific hybrid polypeptide B, i.e., culture filtrate protein (CFP-10) antigen, was taken as test hole B. The above suspension with 250 000 cells was added into each hole. Then, the microplate was placed in a 37°, 5 % carbon dioxide (CO2) incubator for about 18 h, to be washed 4 times with phosphate buffered saline (PBS). The prepared alkaline phosphatase labeled mouse anti-IFN-γ monoclonal antibody was added (50 µl) and the plate was incubated at 6° for 1 h[8]. After incubation, the plate was washed 4 times with PBS. Finally, 50 μl substrate working solution was added to each hole. The reaction time was 8 min. Then, the reaction was terminated by washing with distilled water. The culture plate was dried at 37° for 3 h or overnight at room temperature. And the spot forming cells (SFCs) were counted. Finally, judge the results: With reaction of antigen A or (and) antigen B hole as the basis, judge the results, that is, if negative control hole SFCs is 0-5, (antigen A or (and) antigen B hole SFCs) to (negative control hole SFCs) is ≥6, it is negative[9]. If negative control hole SFCs, (antigen A or (and) antigen B hole SFCs) is ≥2 times of (negative control hole SFCs), it is positive (fig. 2). Steinberg WN diagnostic test was used to evaluate the value of T-SPOT.TB in diagnosis of tuberculosis and extrapulmonary tuberculosis. The count data involved in this study were expressed as (n, %), comparison between the two groups was tested by chi square and SPSS 21.0 statistical software was employed for data processing. As shown in Table 1, the sensitivity and specificity of T-SPOT-TB detection in extrapulmonary tuberculosis were 93.35 % and 89.90 %, respectively. As shown in Table 2, positive rate of T-SPOT.TB in pulmonary tuberculosis group was higher than that in non-pulmonary tuberculosis group and healthy control group (p<0.05). The positive rate of extrapulmonary tuberculosis group was higher than that in non-pulmonary tuberculosis group and healthy control group (p<0.05), with significant difference. As shown in Table 3 below, T-SPOT.TB showed a diagnostic sensitivity of 88.56 % to bacteriological positive pulmonary tuberculosis, 80.25 % to bacteriological negative pulmonary tuberculosis, 93.36 % to extrapulmonary tuberculosis, while diagnostic specificity was respectively 85.67 %, 84.36 %, 89.73 %, positive predictive values were 93.95 %, 88.79 % and 96.56 % respectively and negative predictive values were 74.00 %, 74.00 % and 80.00 % respectively. T-SPOT.TB showed no significant differences in diagnostic efficacy by comparison between bacteriological positive pulmonary tuberculosis group and bacteriological negative pulmonary tuberculosis group (p>0.05). In comparison among extrapulmonary tuberculosis group, bacteriological negative pulmonary tuberculosis and bacteriological positive pulmonary tuberculosis, the results show that there is no statistical significance in T-SPOT.TB diagnostic efficacy (p>0.05). Tuberculosis is a chronic infectious disease, caused by Mycobacterium tuberculosis (Fig. 3). Due to common atypical bacteriological negative pulmonary tuberculosis and extrapulmonary tuberculosis, there is a high diagnosis delay rate in tuberculosis[10,11]. Therefore, use of tuberculosis antigen composition with high sensitivity, high specificity to establish a method for more rapid and accurate diagnosis of tuberculosis is the key. T-SPOT.TB technology is currently the most sensitive technology for detection of tuberculosis antigen specific T lymphocytes and also the main way for T cell based interferon-gamma release assays (TIGRAs) diagnosis of tuberculosis infection. There is high sensitivity and specificity in diagnosis of tuberculosis infection[12]. Clinical studies have shown that, there is a higher diagnostic efficacy in immune compromised individuals. Also, there is a high sensitivity in the diagnosis of extrapulmonary tuberculosis. It has important application significance in diagnosis of atypical bacteriological negative pulmonary tuberculosis and extrapulmonary tuberculosis, children tuberculosis whose test specimens are difficult to obtain. According to the study result, the positive rate of T-SPOT.TB in pulmonary tuberculosis group was higher than that in non-pulmonary tuberculosis group and healthy control group (p<0.05). The positive rate of pulmonary tuberculosis group was significantly higher than that of non-pulmonary tuberculosis group and healthy control group (p<0.05). The diagnostic sensitivity of T-SPOT.TB was 88.56 % to bacteriological positive tuberculosis, 80.25 % to bacteriological negative tuberculosis and 93.36 % to extrapulmonary tuberculosis. The diagnosis specificity was respectively 85.67 %, 84.36 %, 89.73 %, the positive predictive values were respectively 93.95 %, 88.79 % and 96.56 %, while the negative predictive values were 74.00 %, 74.00 % and 80.00 %, respectively, which indicated that T-SPOT.TB has an ideal sensitivity and specificity. In summary, T-SPOT.TB in the diagnosis of tuberculosis infection, there is ideal sensitivity and specificity. Therefore, it can be widely used in diagnosis of pulmonary tuberculosis and bacteriological negative tuberculosis, with great practice value.
| Group | Case number | T-SPOT.TB positive | T-SPOT.TB negative | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|
| Pleural disease | 38 | 28 | 10 | 90.00 | 80.00 |
| Tuberculosis | 30 | 28 | 2 | ||
| Non-tuberculous | 8 | 1 | 7 | ||
| Lymphadenitis | 18 | 16 | 2 | 100.00 | 100.00 |
| Tuberculosis | 15 | 15 | 0 | ||
| Non-tuberculous | 3 | 0 | 3 | ||
| Central Nervous System | 22 | 20 | 2 | 100.00 | 100.00 |
| Tuberculosis | 20 | 20 | 0 | ||
| Non-tuberculous | 2 | 0 | 2 | ||
| Abdominal tuberculosis | 10 | 8 | 2 | 67.85 | |
| Pelvic tuberculosis | 7 | 7 | 0 | 100.00 | |
| Bone tuberculosis | 5 | 5 | 0 | 100.00 | |
| Extrapulmonary tuberculosis total | 100 | 68 | 2 | 93.35 | 89.90 |
| Extrapulmonary non-tuberculous lesion total | 70 | 4 | 46 |
Table 1: T-Spot.Tb Test Results for Extrapulmonary Tuberculosis and Extrapulmonary Non-Tuberculous Disease
| Group | Case number |
T-SPOT.TB positive case number |
Proportion |
|---|---|---|---|
| Nontuberculous disease group | 90 |
16 |
17.78 |
| Extrapulmonary nontuberculous lesions | 70 |
10 |
14.29 |
| Health control group | 90 |
5 |
5.56 |
| Tuberculosis group | 100 |
85 |
85.00 |
| Extrapulmonary tuberculosis group | 100 |
94 |
94.00 |
Table 2: Comparison of T-Spot.Tb Test Results in Each Group
| Group | Case number |
T-SPOT.TB positive case number |
Sensitivity (%) |
Specificity (%) |
Positive predictive value (%) |
Negative predictive value (%) |
|---|---|---|---|---|---|---|
| Bacteriological positive pulmonary tuberculosis | 88 |
80 |
88.56 |
85.67 |
93.95 |
74.00 |
| Bacteriological negative pulmonary tuberculosis | 30 |
22 |
80.25 |
84.36 |
88.79 |
74.00 |
| Extrapulmonary tuberculosis | 82 |
80 |
93.36 |
89.73 |
96.56 |
80.00 |
Table 3: T-Spot.Tb Diagnostic Performance for Pulmonary Tuberculosis and Extrapulmonary Tuberculosis
Acknowledgements:
These authors contributed equally to this work.
Conflicts of Interest:
The authors declared no conflict of interest.
References
- Tao X, Wang J, Li Y, Wang H. Diagnostic value of T-cell enzyme-linked immunospot assay for tuberculosis infection in pulmonary tuberculosis and extrapulmonary tuberculosis. Zhejiang J Prev Med 2012;13(11):4-7.
- Li S, Li L, Zheng H, Wang Y, Zhu X, Yang Y, et al. Relationship between multifaceted body image and negative affect among women undergoing mastectomy for breast cancer: a longitudinal study. Arch Womens Ment Health 2018;21(6):681-8.
- Blumberg HM, Ernst JD. The challenge of latent TB infection. J Am Med Assoc 2016;316(9):931-3.
- Halliday A, Masonou T, Tolosa Wright M, Mandagere V, Lalvani A. Immuno diagnosis of active tuberculosis. Expert Rev Respir Med 2019;13(6):521-32.
- Ghoneum M, Felo N, Nwaogu OM, Fayanju IY, Jeffe JA, Margenthaler DB. Clinical trials in surgical oncology. Asian Pac J Surg Oncol 2015;1(2):73-82.
- Du S, Hou X. Meta-Analysis of Diagnostic Value of T cell enzyme-linked immunospot assay for tuberculosis infection in tuberculosis. Chin J Clin Res 2014;12(5):526-9.
- Liu B, Qi F, Zhang J, Zhai Y, Yang L. Application value of T cell enzyme-linked immunospot assay in the differential diagnosis of tuberculous pleurisy. J Pract Med 2015;23(21):3592-4.
- Wu K, Yao R, Lin W. Diagnosis of pulmonary tuberculosis and extrapulmonary tuberculosis by T-Cell enzyme-linked immunospot assay for tuberculosis infection. Health Res 2016;11(3):342-3.
- Wang L, Lin Q, Yang T, Liang Y, Nie Y, Luo Y, et al. Oryzanol modifies high fat diet induced obesity, liver gene expression profile and inflammation response in mice. J Agric Food Chem 2017;65(38):8374-85.
- Kawamura LM, Grinsdale JA, Ho CS, Jereb JA. Interferon-γ release assays for prediction of tuberculosis. Lancet Infect Dis 2012;12(8):584.
- Dutta RK, Kathania M, Raje M, Majumdar S. IL-6 inhibits IFN-γ induced autophagy in Mycobacterium tuberculosis H37Rv infected macrophages. Int J Biochem Cell Biol 2012;44(6):942-54.
- Adekambi T, Ibegbu CC, Cagle S, Kalokhe AS, Wang YF, Hu Y, et al. Biomarkers on patient T cells diagnose active tuberculosis and monitor treatment response. J Clin Invest 2015 May 1;125(5):1827-38.