- *Corresponding Author:
- Biwei Zhan
Department of Anesthesiology, Hubei Hanchuan People’s Hospital, Hanchuan, Hubei 431600, China
E-mail: zjy20180306@163.com
| This article was originally published in a special issue, “Role of Biomedicine in Pharmaceutical Sciences” |
| Indian J Pharm Sci 2023:85(2) Spl Issue “174-181” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
This study mainly explores the clinical effects of dexmedetomidine and dezocine assisted ultrasound-guided nerve block in thyroid surgery. The data from a total of 72 patients who underwent thyroid surgery in our hospital were analyzed. All patients were given ultrasound-guided cervical plexus block anesthesia and divided into three groups. Group A (n=20) and group B (n=22) received dexmedetomidine and dezocine assisted anesthesia respectively, and group C (n=30) was given dexmedetomidine plus dezocine assisted anesthesia. Anesthesia time, operation time and other clinical indicators were compared among the three groups. The results showed that at 12 h and 24 h, group C had a lower degree of pain than groups A and B. The postoperative comfort score of group C was higher compared to groups A and B. The incidence of postoperative adverse reactions reported was lower in group C compared with the other two groups. The above outcomes shows that the combined use of dexmedetomidine and dezocine in ultrasound-guided assisted nerve block during thyroid surgery contributes to better clinical efficacy compared with their single use.
Keywords
Dexmedetomidine, dezocine, cervical plexus block, thyroid surgery, sedation, analgesia
Epidemiological statistics has shown that prevalence of thyroid diseases remarkably rises globally, particularly among women[1-3]. Surgical intervention is a well-established treatment for several thyroid diseases, including thyroid adenoma, retrosternal goiter and thyroid tumors[4]. However, the degree of pain during thyroidectomy is relatively moderate, but there is still a risk of postoperative complications during thyroid surgery[5]. Despite the great advancement in medical instrumentation that has refined surgical procedures, postoperative complications remain inevitable after thyroidectomy. The most common complication following thyroid surgery is recurrent laryngeal nerve injury[6,7] which can be temporary or permanent. Although the incidence of permanent nerve injury is lower than temporary injury, the minimum recovery time of patients with minor temporary laryngeal nerve injury is around 4 w[8,9]. However, in complex clinical scenarios which may involve neurovascular or peripheral soft tissue injury, it may require longer time for recovery[10].
Cervical Plexus Block (CPB) anesthesia can be operated during thyroid surgery to improve analgesia after thyroidectomy and cut the demand for opiates during and after anesthesia[11]. CPB is an ideal method of anesthesia during thyroid surgery as it is easy to perform and cost-effective compared to general anesthesia[12,13]. However, dense blood vessels and nerves in the neck can limit the probability of obtaining a complete nerve block resulting in tachycardia and hypertension[14,15], particularly in patients with comorbidities such as hypertension[16] and coronary heart disease[17]. Therefore, Intravenous (IV) anesthesia is required while performing a CPB.
Dexmedetomidine is an alpha-2 (α2) type adrenergic receptor agonist that offers cooperative sedation without highly selective complications[18]. Dezocine is a new type of opioid receptor agonist-antagonist[19]. This study compared the sedative and analgesic effects of ultrasound-guided nerve block anesthesia using dexmedetomidine or dezocine as single drugs or in combination during thyroid surgery.
Our study hypothesis is that ultrasound-guided cervical plexus nerve block may improve postoperative analgesia when assisted with dexmedetomidine combining dezocine during thyroid surgery.
Materials and Methods
Clinical data:
A total of 72 patients who underwent thyroid surgery at Hanchuan People’s Hospital from March 2017 to March 2018 were retrospectively analyzed. All patients were given ultrasound-guided CPB anesthesia along with dexmedetomidine and/or dezocine sedative drug. The patients were divided into three groups according to the type of drugs administered. Group A (n=20) received dexmedetomidine assisted anesthesia, group B (n=22) received dezocine assisted anesthesia and group C (n=30) received dexmedetomidine combined with dezocine assisted anesthesia. No significant differences were observed in the general clinical baseline characteristics of the patient groups (p>0.05) (Table 1). All patients had American Society of Anesthesiologists (ASA) physical status range between grade I-II and no history of allergy to the drugs before the operation. There were no contraindications of CPB in all patients. This study was approved by the Ethics Committee of Hanchuan People’s Hospital and all patients were recruited under written informed consent after the surgery, we paid attention to personal privacy and confidentiality when collecting the data and did not disclose the identity of the patients to anyone. Sample size was calculated using an “A Priori” power analysis of G-power 3.1 to analyze the difference between two-independent equal groups, with effect size 0.8 to achieve a power of 80 %, yielding a total sample size of 42 (21 patients in each group), with alpha error 0.05. Therefore, our sample size for each group is above 20.
| Variables | Group A (n=20) | Group B (n=22) | Group C (n=30) | χ2/t | p |
|---|---|---|---|---|---|
| Gender (Male/Female) | 9/11 | 8/14 | 10/20 | 0.7143 | 0.6997 |
| Age (y) | 43.5±8.5 | 42.9±8.8 | 43.1±9.1 | 0.0007 | 0.9754 |
| ASA status | |||||
| I | 12 | 15 | 18 | 0.4364 | 0.804 |
| II | 8 | 7 | 12 | ||
| Approach of surgery | |||||
| Subtotal thyroidectomy | 8 | 11 | 14 | 1.774 | 0.7767 |
| Unilateral thyroid lobectomy | 5 | 4 | 10 | ||
| Bilateral subtotal thyroidectomy | 6 | 5 | 6 |
Table 1: General Data Of Three Groups
Treatment plan:
In the preparation room of central operating theater, IV access was obtained and ringer lactate 10 ml/kg intravenously was administered. In the operating room, the subject received oxygen supplementation 2 l/min through a nasal cannula. Philips MP50 multi parameter monitor was used to monitor Electrocardiogram (ECG), Mean Arterial Pressure (MAP), Heart Rate (HR) and Saturation of peripheral Oxygen (SpO2) of blood. The puncture sites of all patients were routinely disinfected and the CPB was performed under ultrasound guidance employing a one-point block. 5 ml of 0.4 % ropivacaine (10 ml:75 mg) for deep cervical plexus on one side and 10 ml of 0.4 % ropivacaine (10 ml:75 mg) for superficial cervical plexus on each side. To relieve intraoperative discomfort 10 min after the block, patients in group A were given IV dexmedetomidine (0.5 μg/kg)+IV of normal saline infusion (15 ml/h). Patients in group B were given IV dezocine (0.1 mg/kg)+IV pump of normal saline infusion (15 ml/h). Patients in group C were given IV dexmedetomidine (0.5 μg/ kg)+dezocine (0.1 mg/kg)+IV infusion of normal saline (15 ml/h). The administration of all drugs was stopped 30 min before the end of the operation.
Anesthesia depth monitoring and indicators observation:
The anesthesia time, operation time and the recovery time after anesthesia were recorded in the Post- Anesthesia Care Unit (PACU) and compared amongst the three groups. Moreover, to monitor the indicators of anesthesia depth, including the hemodynamic marker changes (MAP, HR and SpO2) and Ramsay sedation scores were recorded before anesthesia (T1), 10 min after anesthesia (T2), the beginning of the skin incision (T3), before dissecting the thyroid (T4) and at the end of the operation (T5).
The Visual Analog Scale (VAS) scores were compared across the three groups at 2, 6, 12 and 24 h after operation according to the following system (0: Painless; <3: Excellent analgesia; 3-5: Satisfactory analgesia; >5: Unsatisfactory analgesia and 10: Severe pain). The Bruggemann Comfort Scale (BCS) [20] were evaluated according to the following scores (0: Continuous pain; 1: No pain when quiet but with pain in deep breathing and coughing; 2: No pain when lying in the supine position but slight pain while deep breathing and coughing; 3: No pain during deep breathing and 4: No pain while coughing). The postoperative adverse reactions and anesthesia satisfaction of the three groups were also recorded.
Statistical methods:
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) 21.0 software (SPSS Inc.). Measurement data were expressed as the mean±standard deviation (x±s) while the counts data were expressed as percentages. T-test was used for the comparison between the two groups of quantitative data and Chi square test was used for the comparison between the two groups of qualitative data. Differences between the means were analyzed using single, two or three-factor Analysis of Variance (ANOVA), with or without repeated measures, followed by Bonferroni correction (Bonferroni post-mortem analysis). α=0.05 was used as the test standard and p<0.05 was considered as statistically significant difference.
Results and Discussion
Anesthesia time, operation times and recovery room residence times were explained here. We have recorded all clinical information to investigate the effect of the sedative drugs on anesthesia time, operation time and postoperative recovery time and status. Our results showed no significant differences in the anesthesia time, operation time, PACU completion and the length of stay in the recovery room amongst the three groups (p>0.05) according to the recorded times. These data indicate that the use of dexmedetomidine and/or dezocine have no significant effect on the basic characteristics of anesthesia (Table 2).
| Groups | Anesthesia completion time (min) | Time of operation (min) | PACU completion time (min) |
|---|---|---|---|
| Group A (n=20) | 14.5±1.3 | 68.7±13.2 | 28.2±3.9 |
| Group B (n=22) | 15.1±1.8 | 69.4±12.9 | 29.3±4.3 |
| Group C (n=30) | 14.2±1.7 | 67.3±13.5 | 28.8±4.0 |
| χ2/t | 0.0533 | 0.0049 | 0.011 |
| p | 0.1506 | 0.8436 | 0.6829 |
Table 2: Basic Information of Surgical Anesthesia
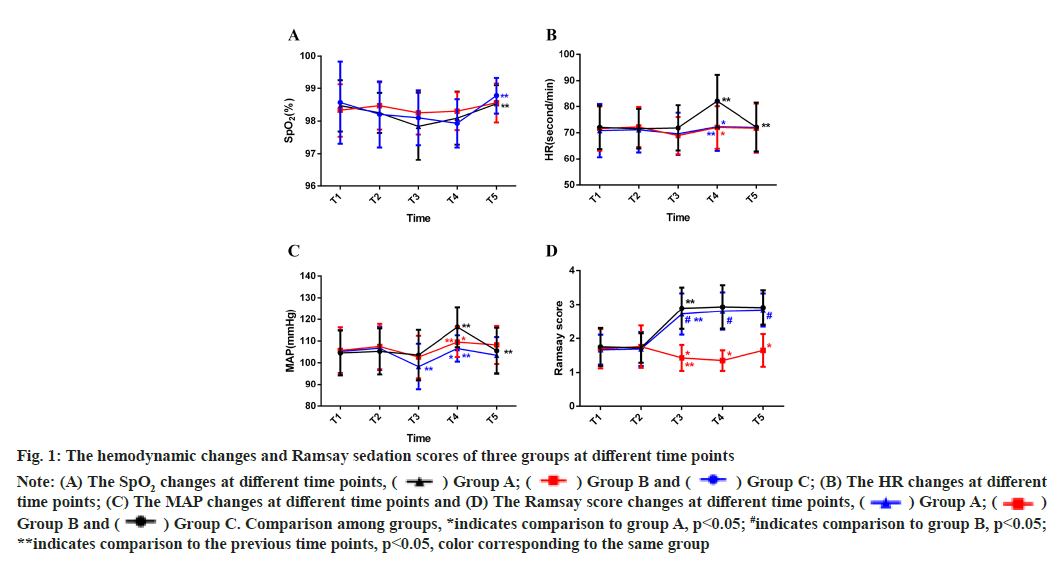
Administration of dexmedetomidiχne and dezocine during CPB improves sedative effects is shown here. The anesthesia indicators information was recorded to monitor the anesthetic depth in dexmedetomidine and/or dezocine three groups. The changes in hemodynamic markers of the three groups were compared before CPB anesthesia, 10 min after CPB anesthesia, at the beginning of the operation, before dissecting the thyroid and at the end of the operation.
Our results have shown that the difference in SpO2 percentage among groups wasn’t significant, although it was significantly elevated at T5 in the dexmedetomidine-administered group (group A) and dexmedetomidine combined with dezocine (group C) compared to T4 (fig. 1A). On the other hand, we observed that the MAP and HR rates in dexmedetomidine administered group (group A) was significantly higher before dissecting the thyroid in comparison to dezocine administered group (group B) and dexmedetomidine combined with dezocine (group C) (p<0.05) (fig. 1B and fig. 1C). While the Ramsay sedation scores in dezocine administered group (group B) at the beginning of skin incision, before dissecting the thyroid and at the end of operation was significantly lower compared to dexmedetomidine (groups A) and dexmedetomidine combined with dezocine (group C) (p<0.05) (fig. 1D). Overall, these data showed that the effect of dexmedetomidine combined with dezocine on hemodynamics is relatively stable and that the combination has a better sedative effect compared to the single drugs.
Fig. 1: The hemodynamic changes and Ramsay sedation scores of three groups at different time points
Note: (A) The SpO2 changes at different time points, Group C; (B) The HR changes at different
time points; (C) The MAP changes at different time points and (D) The Ramsay score changes at different time points,
Group C; (B) The HR changes at different
time points; (C) The MAP changes at different time points and (D) The Ramsay score changes at different time points,  Group B and
Group B and  Group C. Comparison among groups, *indicates comparison to group A, p<0.05; #indicates comparison to group B, p<0.05;
**indicates comparison to the previous time points, p<0.05, color corresponding to the same group
Group C. Comparison among groups, *indicates comparison to group A, p<0.05; #indicates comparison to group B, p<0.05;
**indicates comparison to the previous time points, p<0.05, color corresponding to the same group
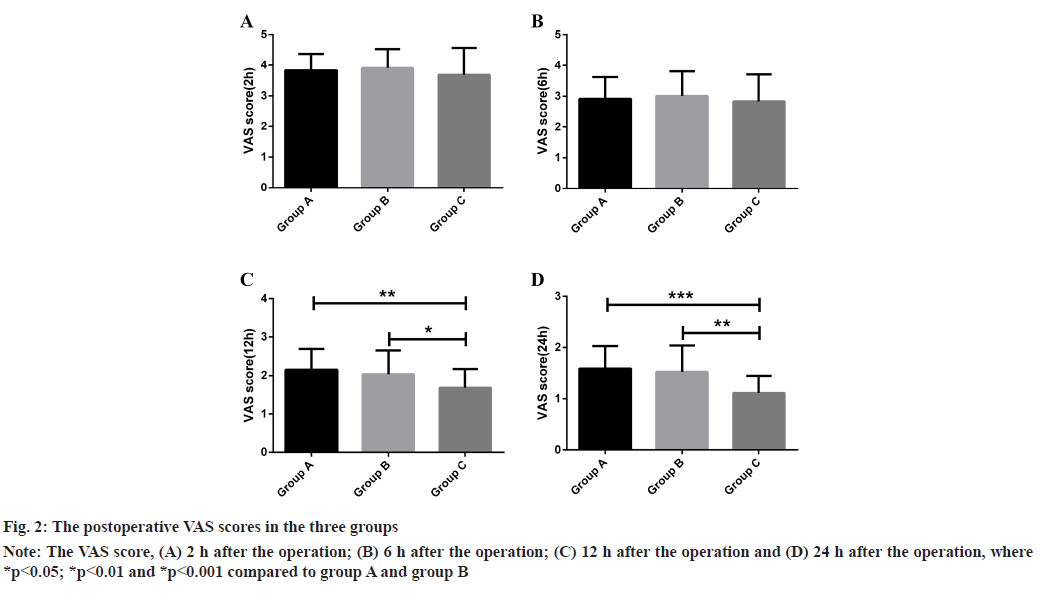
Administration of dexmedetomidine and dezocine during CPB reduces VAS scores postoperative pain. After thyroid surgery, the effects of Bilateral Superficial Cervical Plexus Block (BSCPB) are on cutaneous, subcutaneous and muscular layers which are under post-thyroidectomy analgesia but pain arises from areas that cannot be blocked by a simple approach[21]. To investigate the postoperative pain in the patients who underwent thyroid surgery, we analyzed the VAS scores at different time points after surgery. No significant differences were observed in the VAS scores between administering dexmedetomidine and/or dezocine three groups at 2 h and 6 h after the operation (p>0.05) (fig. 2A and fig. 2B). Interestingly, at 12 h and 24 h after the operation, the VAS scores of groups administered with dexmedetomidine and dezocine (i.e., group C) was significantly lower (p<0.05) than group administered with dexmedetomidine or dezocine (i.e., groups A and B, respectively) (fig. 2A and fig. 2B).
Thyroidectomy patient’s postoperative voice and comfort significantly improved in CPB administered with dexmedetomidine and dezocine. Phonatory, comfort and swallowing symptoms are wellknown postoperative complications after early thyroidectomy, even without laryngeal nerve injuries[22]. To monitor the patient’s voice and comfort after thyroid surgery, we have recorded the BCS scores. Our results have shown that patients have no temporary or permanent recurrent laryngeal nerve injury in the three groups. The BCS scores showed that the comfort levels of patients administered with dexmedetomidine and dezocine (group C) were significantly higher compared to the patients administered with dexmedetomidine or dezocine (group A and B respectively) (p<0.05) (Table 3).
| Groups | Temporary or permanent recurrent laryngeal nerve injury | BCS score |
|---|---|---|
| Group A (n=20) | 0 | 2.64±0.37 |
| Group B (n=22) | 0 | 2.77±0.49 |
| Group C (n=30) | 0 | 3.14±0.45*# |
Note: *Compared to group A, p<0.05 and #compared to group B, p<0.05
Table 3: Postoperative Voices and Comfort Level
Thyroidectomy patients administered with dexmedetomidine and dezocine have lower postoperative adverse reactions and higher anesthesia satisfaction. Postoperative Nausea and Vomiting (PONV), respiratory depression, headache and other adverse reactions are common in patients subjected to thyroidectomy treatment[23]. We analyzed the adverse reactions in the patients who underwent thyroidectomy employing CPB and administered dexmedetomidine and/or dezocine. Our results showed that the incidence of postoperative adverse reactions were 35 % in group A, 31.8 % in group B and 10 % in group C (p<0.05) (Table 4).
| Groups | Nausea | Emesis | Respiratory depression | Headache | Exudation | Total incidence (%) |
|---|---|---|---|---|---|---|
| Group A (n=20) | 2 | 1 | 1 | 2 | 1 | 7 (35.0) |
| Group B (n=22) | 3 | 1 | 1 | 2 | 0 | 7 (31.8) |
| Group C (n=30) | 1 | 1 | 0 | 1 | 0 | 3 (10.0)*# |
Note: *Compared to group A, p<0.05 and #compared to group B, p<0.05
Table 4: Postoperative Adverse Reactions
However, no significant difference in anesthesia satisfaction was observed amongst the three groups (p<0.05). These data suggested that the three modes of anesthesia administration had minimal impact on patient satisfaction (Table 5). From the above, the incidence of postoperative adverse reactions in patients administered with dexmedetomidine and dezocine was significantly lower than in patients administered with dexmedetomidine or dezocine, and it has minimal impact on anesthesia satisfaction.
| Groups | Great satisfaction | Quite satisfaction | Dissatisfaction | Total satisfaction rate |
|---|---|---|---|---|
| Group A (n=20) | 10 | 4 | 6 | 14 (70.0) |
| Group B (n=22) | 12 | 5 | 5 | 17 (77.3) |
| Group C (n=30) | 16 | 9 | 5 | 25 (83.3) |
Table 5: Anesthesia Satisfaction among Three Groups
Currently, thyroid diseases that include lesions and cancers are mainly treated by surgery, which is considered an effective and safe treatment. However, patients who undergo thyroid surgery treatment often experience relatively high levels of postoperative pain and postoperative recurrent laryngeal nerve injury[21,24]. The effective reduction of thyroidectomy postoperative complications and postoperative analgesia remain as urgent clinical needs.
In this study, we used CPB anesthesia under ultrasound guidance for thyroid surgery. This surgery procedure was accompanied by administering dexmedetomidine and/or dezocine anesthesia to determine the sedative and analgesic effects of the different drugs on thyroidectomy patients during and after surgery.
According to our observations, there were no significant differences in anesthesia response time, operation time and the length of anesthesia recovery duration in all three patient groups. These data suggest that auxiliary anesthesia with dexmedetomidine and/ or dezocine has minimal impact on the anesthesia basic clinical indicators during the operation. On the other hand, the changes in the hemodynamics markers (MAP, HR and SpO2) and the Ramsay sedation scores in the thyroid surgery patient groups who administered with dexmedetomidine and/or dezocine showed that the MAP and HR rates in the patients groups who were given dexmedetomidine alone were higher compared to those who were given dezocine alone or in combination with dexmedetomidine. These results suggest that dexmedetomidine elevated the MAP and HR compared to dezocine and both combinations. On the other hand, Ramsay sedation scores of the dezocine administered patient’s group was significantly lower at the beginning of the operation, before dissection of the thyroid and at the end of operation compared to the patient’s groups given dexmedetomidine and combination. In accordance with previously reported results that dexmedetomidine administered with ropivacaine or different doses of only dexmedetomidine and the Ramsay sedation score was higher and improved the duration of the analgesia[25,26]. These results were suggesting that dexmedetomidine combined with dezocine had a stronger sedative effect.
However, no significant difference in SpO2 percentage was observed in all groups of patients at any time point. Previously, it has been shown that dexmedetomidine didn’t affect SpO2 compared to propofol in patients with obstructive sleep apnea undergoing drug-induced sleep endoscopy[27].
As patients undergoing CPB anesthesia may experience fear or anxiety during the perioperative period, the body produces corresponding stress response hormones[28]. After the CPB, there is an interaction between the arterial sinus and the vagus nerve, resulting in increased plasma catecholamine levels through sympathetic nerve excitation[29].
Consequently, this causes physiological reactions that result in tachycardia and hypertension during the operation. Dexmedetomidine has a low-level inhibitory effect on respiration and can effectively release histamine to offset the hemodynamic effects of the nerve block to a certain extent.
Postoperative pain was commonly observed in the cohort of patients. No significant differences were observed in the pain scores amongst the three groups at 2 h and 6 h after the operation. However, at 12 h and 24 h after the operation, the pain score of the dexmedetomidine and dezocine combination group was significantly lower than the dexmedetomidine or dezocine only groups. These data suggest that dexmedetomidine combined with dezocine can effectively relieve postoperative pain.
Acute pain is one of the most common complaints after surgery, which seriously impacts adverse cardiovascular, pulmonary, metabolic and psychological outcomes[30,31]. Thyroid surgery can be very painful in the early postoperative period. According to the results reported in previous studies, the VAS scores after thyroid surgery can reach 6.9±1.7 points and up to 90 % of patients require morphine for pain relief[12]. Dexmedetomidine combined with dezocine can effectively relieve acute postoperative pain. These effects occur because dexmedetomidine can effectively reduce the concentration of catecholamines in the plasma to play an anti-sympathetic role and reduce the stress response caused by surgery[32].
Dezocine is an opioid receptor agonist and antagonist that is more effective in relieving pain than morphine, to which patients fail to develop dependence[33]. We found that dexmedetomidine combined with dezocine in assisted CPB greatly reduced the incidence of adverse reactions in patients after operation. Similarly, Tan et al. have suggested a sedative effect of dexmedetomidine with patients who experience no temporary or permanent recurrent laryngeal nerve injury[34]. Moreover, our results have shown that dexmedetomidine and dezocine improved postoperative thyroid surgery adverse reactions such as voice and comfort. Similarly, dexmedetomidine could minimize polypharmacy by providing adequate sedative, analgesic and anxiolytic effects with no accompanying respiratory depression[35]. Henceforth, our observations suggest that dexmedetomidine and dezocine can be used as sedative drugs after thyroid surgery to reduce the adverse effects and reduces polypharmacy.
In conclusion, administering the dexmedetomidine combined with dezocine in ultrasound-guided nerve block for thyroid surgery has improved the hemodynamic indicators like MAP and HR compared to a single drug. Moreover, dexmedetomidine combined with dezocine has remarkably improved Ramsay sedation scores, which means these drugs combination has a sedative effect during thyroid surgery. The combination of drugs also produce a strong postoperative analgesic effect and can reduce the incidence of postoperative complications and is a safe form of anesthesia auxiliary drugs. Furthermore, our results suggest that dexmedetomidine and dezocine sedative drugs have minimal impact on the anesthesia process during the operation and recovery.
But still, due to the design of this study, it is not without several limitations. The retrospective nature of analysis does not allow randomization of patients in each group, so that the similarity of patients in groups is jeopardized. A well-designed, randomized and controlled trial with prospective data collection and sample size calculation is needed to further confirm the findings in our study in the future.
Author’s contributions:
Yongjun Zeng and Biwei Zhan: Methodology, investigation, data curation, original draft; Biwei Zhan: Writing, review and editing; Yongjun Zeng: Review and editing and Jingjing Liu: Idea, supervision, review and editing.
Acknowledgements:
I would like to express my gratitude to all those who helped me during the writing of this thesis. I acknowledge the help of my colleagues Jingjing Liu and Biwei Zhan for the suggestions they offered me in academic studies.
Conflict of interests:
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
- Luster M, Duntas LH, Wartofsky L. The thyroid and its diseases. 1st ed. Springer International Publishing AG; 2019.
- Vanderpump MP. Epidemiology of thyroid disorders. In: Luster M, Duntas LH, Wartofsky L, editors. The thyroid and its diseases. 1st ed. Cham: Springer International Publishing; 2019. p. 75-85.
- Mehran L, Amouzegar A, Azizi F. Thyroid disease and the metabolic syndrome. Curr Opin Endocrinol Diabetes Obes 2019;26(5):256-65.
[Crossref] [Google scholar] [PubMed]
- Zbären P, Shah JP, Randolph GW, Silver CE, Olsen KD, Shaha AR, et al. Thyroid surgery: Whose domain is it? Adv Ther 2019;36:2541-6.
[Crossref] [Google scholar] [PubMed]
- Uhlmann RA, Reinhart III HA, Postevka E, Snyder SK, Arenas MR. A review of postoperative pain management for thyroid and parathyroid surgery. J Surg Res 2019;241:107-11.
[Crossref] [Google scholar] [PubMed]
- Lynch J, Parameswaran R. Management of unilateral recurrent laryngeal nerve injury after thyroid surgery: A review. Head Neck 2017;39(7):1470-8.
[Crossref] [Google scholar] [PubMed]
- Joliat GR, Guarnero V, Demartines N, Schweizer V, Matter M. Recurrent laryngeal nerve injury after thyroid and parathyroid surgery: Incidence and postoperative evolution assessment. Medicine 2017;96(17):e6674.
[Crossref] [Google scholar] [PubMed]
- Higgins TS, Gupta R, Ketcham AS, Sataloff RT, Wadsworth JT, Sinacori JT. Recurrent laryngeal nerve monitoring versus identification alone on post‐thyroidectomy true vocal fold palsy: A meta‐analysis. Laryngoscope 2011;121(5):1009-17.
[Crossref] [Google scholar] [PubMed]
- Aspinall S, Oweis D, Chadwick D. Effect of surgeons’ annual operative volume on the risk of permanent hypoparathyroidism, recurrent laryngeal nerve palsy and haematoma following thyroidectomy: Analysis of United Kingdom Registry of Endocrine and Thyroid Surgery (UKRETS). Langenbecks Arch Surg 2019;404(4):421-30.
[Crossref] [Google scholar] [PubMed]
- Gualniera P, Scurria S, Mondello C, Asmundo A, Sapienza D, Gianlorenzo D. Narrative review of proving the causal link of recurrent laryngeal nerve injury and thyroidectomy: A medico legal appraisal. Gland Surg 2020;9(5):1564-72.
[Crossref] [Google scholar] [PubMed]
- Elmaddawy AE, Mazy AE. Ultrasound-guided bilateral superficial cervical plexus block for thyroid surgery: The effect of dexmedetomidine addition to bupivacaine-epinephrine. Saudi J Anaesth 2018;12(3):412-8.
[Crossref] [Google scholar] [PubMed]
- Woldegerima YB, Hailekiros AG, Fitiwi GL. The analgesic efficacy of bilateral superficial cervical plexus block for thyroid surgery under general anesthesia: A prospective cohort study. BMC Res Notes 2020;13(1):1-6.
[Crossref] [Google scholar] [PubMed]
- Banerjee S, Acharya R, Sriramka B. Ultrasound-guided inter-scalene brachial plexus block with superficial cervical plexus block compared with general anesthesia in patients undergoing clavicular surgery: A comparative analysis. Anesth Essays Res 2019;13(1):149-54.
[Crossref] [Google scholar] [PubMed]
- Kim JS, Kim HY. Cervical plexus block. Korean J Anesthesiol 2018;71(4):274-88.
[Crossref] [Google scholar] [PubMed]
- Arjun BK, Vinod CN, Puneeth J, Narendrababu MC. Ultrasound-guided interscalene block combined with intermediate or superficial cervical plexus block for clavicle surgery: A randomised double blind study. Eur J Anaesthesiol 2020;37(11):979-83.
[Crossref] [Google scholar] [PubMed]
- Michalek P, David I, Adamec M, Janousek L. Cervical epidural anesthesia for combined neck and upper extremity procedure: A pilot study. Anesth Analg 2004;99(6):1833-6.
[Crossref] [Google scholar] [PubMed]
- Gassner M, Bauman Z, Parish S, Koenig C, Martin J, Hans S. Hemodynamic changes in patients undergoing carotid endarterectomy under cervical block and general anesthesia. Ann Vasc Surg 2014;28(7):1680-5.
[Crossref] [Google scholar] [PubMed]
- Bekker A, Sturaitis MK. Dexmedetomidine for neurological surgery. Neurosurgery 2005;57(1):1-10.
[Crossref] [Google scholar] [PubMed]
- Zhou C, Yang Y, Zhu Y, Ruan L. Effects of dezocine on prevention of propofol injection pain: A meta-analysis. J Pain Res 2017;10:1369-75.
[Crossref] [Google scholar] [PubMed]
- Su S, Ren C, Zhang H, Liu Z, Zhang Z. The opioid-sparing effect of perioperative dexmedetomidine plus sufentanil infusion during neurosurgery: A retrospective study. Front Pharmacol 2016;7:407.
[Crossref] [Google scholar] [PubMed]
- Eti Z, Irmak P, Gulluoglu BM, Manukyan MN, Gogus FY. Does bilateral superficial cervical plexus block decrease analgesic requirement after thyroid surgery? Anesth Analg 2006;102(4):1174-6.
[Crossref] [Google scholar] [PubMed]
- Lombardi CP, Raffaelli M, de Crea C, D'Alatri L, Maccora D, Marchese MR, et al. Long-term outcome of functional post-thyroidectomy voice and swallowing symptoms. Surgery 2009;146(6):1174-81.
[Crossref] [Google scholar] [PubMed]
- Won YJ, Yoo JY, Chae YJ, Kim DH, Park SK, Cho HB, et al. The incidence of postoperative nausea and vomiting after thyroidectomy using three anaesthetic techniques. J Int Med Res 2011;39(5):1834-42.
[Crossref] [Google scholar] [PubMed]
- Chen Y, Nwaogu I, Chomsky-Higgins K, Gosnell JE, Seib C, Shen WT, et al. Postoperative pain and opioid use after thyroid and parathyroid surgery-a pilot, prospective SMS-based survey. J Surg Res 2019;240:236-40.
[Crossref] [Google scholar] [PubMed]
- Lee MH, Ko JH, Kim EM, Cheung MH, Choi YR, Choi EM. The effects of intravenous dexmedetomidine on spinal anesthesia: Comparision of different dose of dexmedetomidine. Korean J Anesthesiol 2014;67(4):252-7.
[Crossref] [Google scholar] [PubMed]
- Lin YN, Li Q, Yang RM, Mao ZX, Liu JC. Addition of dexmedetomidine to ropivacaine improves cervical plexus block. Acta Anaesthesiol Taiwan 2013;51(2):63-6.
[Crossref] [Google scholar] [PubMed]
- Yoon BW, Hong JM, Hong SL, Koo SK, Roh HJ, Cho KS. A comparison of dexmedetomidine versus propofol during drug‐induced sleep endoscopy in sleep apnea patients. Laryngoscope 2016;126(3):763-7.
[Crossref] [Google scholar] [PubMed]
- Wattier JM, Caiazzo R, Andrieu G, Kipnis E, Pattou F, Lebuffe G. Chronic post-thyroidectomy pain: Incidence, typology and risk factors. Anaesth Crit Care Pain Med 2016;35(3):197-201.
[Crossref] [Google scholar] [PubMed]
- Takemoto Y, Hasegawa Y, Hayashi K, Cao C, Hamasaki T, Kawano T, et al. The stabilization of central sympathetic nerve activation by renal denervation prevents cerebral vasospasm after subarachnoid hemorrhage in rats. Transl Stroke Res 2020;11(3):528-40.
[Crossref] [Google scholar] [PubMed]
- Krishna SN, Chauhan S, Bhoi D, Kaushal B, Hasija S, Sangdup T, et al. Bilateral erector spinae plane block for acute post-surgical pain in adult cardiac surgical patients: A randomized controlled trial. J Cardiothorac Vasc Anesth 2019;33(2):368-75.
[Crossref] [Google scholar] [PubMed]
- Turan A, Leung S, Bajracharya GR, Babazade R, Barnes T, Schacham YN, et al. Acute postoperative pain is associated with myocardial injury after noncardiac surgery. Anesth Analg 2020;131(3):822-9.
[Crossref] [Google scholar] [PubMed]
- Wang L, Wang S, Xing Z, Li F, Teng J, Jia T. Application of dexmedetomidine in cardiopulmonary bypass prefilling. Dose Response 2020;18(3):1-5.
[Crossref] [Google scholar] [PubMed]
- Wu FX, Babazada H, Gao H, Huang XP, Xi CH, Chen CH, et al. Dezocine alleviates morphine-induced dependence in rats. Anesth Analg 2019;128(6):1328-35.
[Crossref] [Google scholar] [PubMed]
- Tan JA, Ho KM. Use of dexmedetomidine as a sedative and analgesic agent in critically ill adult patients: A meta-analysis. Intensive Care Med 2010;36:926-39.
[Crossref] [Google scholar] [PubMed]
- Manasa CR, Padma L, Ramanujam R. Evaluation of efficacy of sedative and analgesic effects of single IV dose of dexmedetomidine in post-operative patients. Int J Pharmacol Clin Sci 2013;2(3):75-81.