- *Corresponding Author:
- Jinjing Lu
Department of Emergency, Linxia People's Hospital, Linxia, Gansu 731100, China
E-mail: 19909306789@163.com
| This article was originally published in a special issue, “New Research Outcomes in Drug and Health Sciences” |
| Indian J Pharm Sci 2023:85(6) Spl Issue “216-222” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the effect of Qingyi decoction with modification adjunctive western medicine in the treatment of acute pancreatitis and the effect on high mobility group protein B1 and receptor for advanced glycation end products levels. In order to compare the improvement of clinical symptoms, traditional Chinese medicine evidence score, inflammatory factor levels, gastrointestinal hormone levels, and serum. 108 patients with acute pancreatitis treated in our hospital from January 2021 to January 2022 were chosen and randomly divided into the research group (n=54, treated with conventional western medicine) and the control group (n=54, treated with Qingyi decoction with modification on top of conventional western medicine). The length of hospital stay, acute physiological and chronic health status scores, and the times it took for abdominal pain, bloating, gas, and pressure to go away were all lower in the research group than in the control group (p<0.05). Following treatment, the research group had lower scores for abdominal discomfort, fullness, dryness, and firmness, nausea, vomiting, tidal fever, dry mouth and thirst, and short and red urine than the control group (p<0.05). Following therapy, the research group's levels of the inflammatory proteins tumor necrosis factor, hypersensitive C-reactive protein, and interleukin-6 were all lower than those of the control group (p<0.05). Following treatment, the levels of motilin were greater in the research group than in the control group (p<0.05), and the levels of gastrointestinal inhibitory peptide, vasoactive intestinal peptide, and gastrointestinal inhibitory peptide were lower in the research group than in the control group (p<0.05). Following treatment, the research group's levels of high mobility group protein B1 and receptor for advanced glycation end products were both lower than those of the control group (p<0.05). With some modifications, Qingyi decoction is effective in the treatment of acute pancreatitis with western medicine. It has significant effects on clinical symptoms, the inflammatory response, and high mobility group protein B1 and receptor for advanced glycation end products levels, and is highly valuable for clinical use and promotion.
Keywords
Acute pancreatitis, Qingyi decoction, inflammatory response, gastrointestinal hormones, malformation, glycosylation
Due to the activation of pancreatic proteases and the pancreatic self-digestive reaction, which mostly manifests as a systemic inflammatory response syndrome, acute pancreatitis is a common clinical emergency[1]. If neglected, 25 % of individuals with acute pancreatitis can progress to severe pancreatitis, which can cause multi-organ failure, a severe systemic reaction, and a death risk of 5 % to 10 %[2]. The majority of standard therapeutic methods, including suppression of digestive enzyme secretion and anti-inflammation, are employed to treat acute pancreatitis at the moment. These methods have positive results but clear limitations, and some patients have a terrible prognosis. The primary cause of this is that the center is humid and hot, the liver and gallbladder are unfavorable, and the spleen and stomach are unable to transport and transform, which leads to internal qi blockage and vein stagnation. The main direction of treatment is to clear heat, detoxify toxins and remove dampness[3,4]. The majority of recent researches have concluded that combining Chinese and western treatment to treat acute pancreatitis is effective. The primary method of acute pancreatitis is Qingyi decoction, which is an important medicine for dipping the internal organs and clearing heat and detoxifying the toxins, but the clinical research on Qingyi decoction with modification for the treatment of acute pancreatitis is relatively small, which is not enough to support Qingyi decoction with modification to supplement western medicine as an effective treatment option for acute pancreatitis. We believe that Qingyi decoction with modification adjunct to western medicine for acute pancreatitis will achieve more satisfactory results, and this protocol is expected to become an effective combined Chinese and western medicine treatment protocol for acute pancreatitis.
Serum High Mobility Group Protein B1 (HMGB1) and Receptor for Advanced Glycation Endproducts (RAGE) are significant for the assessment of acute pancreatitis because new signs that have been connected to the beginning of acute pancreatitis in recent years. Understanding the roles performed by HMGB1 and RAGE in the development of acute pancreatitis is crucial for improving clinical understanding of the condition.
To offer a reliable resource for the clinical management of acute pancreatitis, the current study will examine the effects of Qingyi decoction with modification as a supplement to western medicine when treating severe pancreatitis and the changes in HMGB1 and RAGE levels before and after treatment.
Materials and Methods
Experimental preparation:
88 acute pancreatitis patients who were treated in our hospital between January 2021 and January 2022 were chosen as study participants and randomly assigned to one of two groups; the research group (n=54; treated with traditional western medicine); or the control group (n=54; treated with Qing Yi Tang plus reduction in addition to traditional western medicine). Once the study was approved by our hospital’s medical ethics committee, all study participants gave their assent and signed the informed consent form.
Inclusion and exclusion criteria:
Inclusion criteria: Patients who met the criteria for acute pancreatitis diagnosis as outlined in the "Guidelines for the diagnosis and treatment of acute pancreatitis[5]" and "Expert consensus on the treatment of acute pancreatitis in Chinese medicine"[6]; first onset of the disease; onset of the disease ≤72 h; and received complete treatment in our hospital after admission were included.
Exclusion criteria: Patients with other digestive system diseases; patients with pancreatic cancer; patients with biliary tract malformation; patients with pancreatic abscess or hemorrhagic necrotizing pancreatitis; patients with severe infections, patients who are allergic to the medications used in this trial, patients with cardiac, hepatic, renal and other significant organ dysfunction, and women who are pregnant or nursing were excluded.
Methods:
The control group received conventional western medicine treatment, routine water fasting, correction of water-electrolyte disorders, gastrointestinal decompression, prevention and control of infections and nutritional support and other conventional treatments. Statin injection (Guangdong Tianpu Biochemical Medicine Co., Ltd., specification of 1 ml:50 000 units) initially 2 ml in 5 % glucose injection 500 ml intravenously, 2 times/d, the dosage can be reduced as the symptoms subside. Esomeprazole sodium for injection (AstraZeneca AB, approval no: Guodianzhi J20120035, specification of 40 mg) 40 mg dissolved in 0.9 % sodium chloride solution 100 ml intravenously, 2 times/d. Meropenem for injection (Shenzhen Binhai Pharmaceutical Co. (Specification of 0.5 g) 1 g each time dissolved in 100 ml of 0.9 % sodium chloride solution for intravenous infusion, 3 times/d.
In the research group, we added Qingyi decoction with modification to the control group. In case of heavy damp-heat, add 5 g each of Yin Chen and Gardenia jasminoides; in case of nausea and vomiting, add 10 g each of Zhushu and radix et Rhizoma; in case of heavy heat, add 5 g each of Sheng Shi and Zhi mu; in case of food stagnation, add 5 g each of Ji Nei Jin, Lycopodium and Shen Qu; decoct in water and extract 400 ml of juice, 1 dose/d, morning and evening once.
Observation indicators:
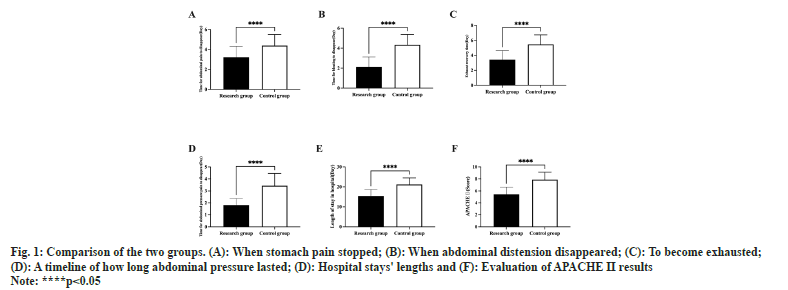
Improvement of clinical symptoms: Compare the time to disappearance of abdominal pain, time to disappearance of abdominal distension, time to recovery of exhaustion, time to disappearance of abdominal pressure pain, length of hospital stay and between the two groups, the Acute Physiological and Chronic Health Status Score (APACHE II) can vary from 0 to 71, with higher numbers indicating more severe disease.
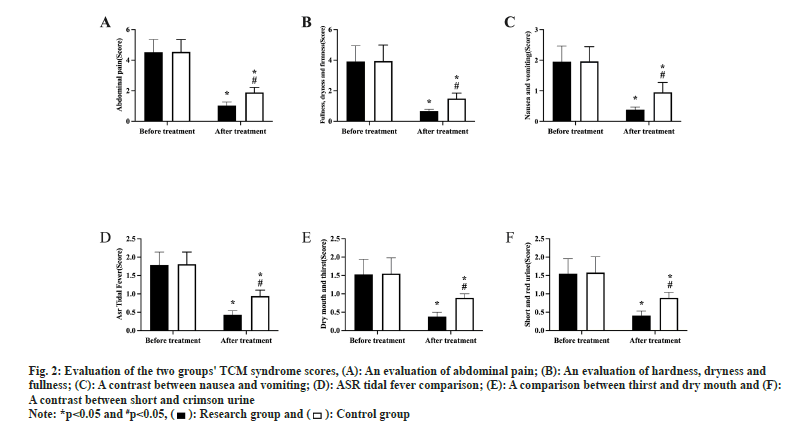
Chinese medicine evidence score: In line with the 2017 expert consensus on the management of acute pancreatitis in Chinese medicine, abdominal pain and fullness and dryness of the abdomen were divided into light (2 points), moderate (4 points) and severe (6 points) levels for scoring, the lower the score, the less severe the symptoms. Nausea and vomiting, daytime hot flushes, dry mouth and thirst, and short, red urine are given a score out of three, with mild symptoms receiving one point, moderate symptoms receiving two points, and severe symptoms receiving three points.
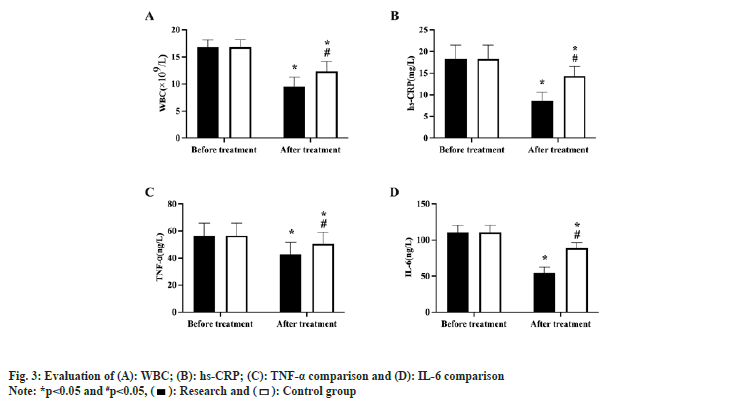
Inflammatory factor levels: They were assessed using a blood cell analyzer to determine the levels of whole blood White Blood Cells (WBC), hypersensitive C-Reactive Protein (hs-CRP), Tumour Necrosis Factor (TNF), and Interleukin-6 (IL-6), as well as an Enzyme-Linked Immunosorbent Assay (ELISA), both before and after treatment.
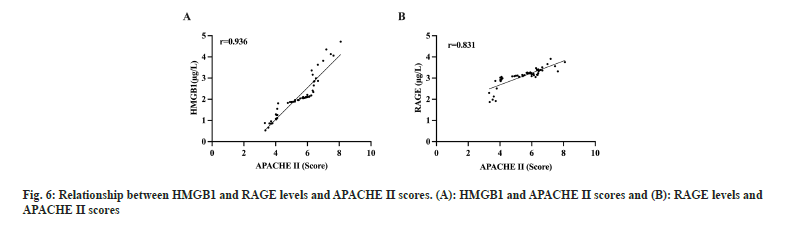
Compare the levels of Vasoactive Intestinal Peptide (VIP), Gastrointestinal Inhibitory Peptide (GIP) and Motilin (MTL) before and after treatment, using ELISA. HMGB1 and RAGE levels were measured by ELISA. And relationship between HMGB1, RAGE levels and APACHE II score.
Statistical process:
The data results were statistically evaluated using the statistical software Statistical Package for the Social Sciences (SPSS) 23.0. Measurement data were compared between groups using the t-test, before and after treatment using the paired t-test, and relationships were looked at using Pearson's correlation coefficient. The Chi-square (χ2) test was used to compare groups using the count data, which were given as rate. The statistical significance of a difference was defined as p<0.05.
Results and Discussion
Basic information like age and gender were gathered to compare the two groups, however there was no statistically significant difference between them (p>0.05, Table 1). The length of hospital stay, APACHE II score, time to resolution of abdominal pain, time for bloating to go away, time for exhaustion to come back, time for abdominal pressure to go away, and all of these things were shorter (lower) in the research group than in the control group (p<0.05, fig.1A- fig.1F).
| Group | n | Gender [n (%)] | Age (year) | Course of disease (h) | Chinese medicine evidence type | |||
|---|---|---|---|---|---|---|---|---|
| Female | Male | Stagnant air symptoms | Humidity and heat symptoms |
Real heat symptoms | ||||
| Research | 54 | 26 | 28 | 44.12±3.29 | 18.73±2.18 | 26 | 16 | 14 |
| Control | 54 | 25 | 29 | 44.15±3.23 | 18.79±2.15 | 24 | 17 | 15 |
| χ2or t | - | 0.037 | 0.048 | 0.144 | 0.149 | 0.044 | 0.047 | |
| p | - | 0.487 | 0.962 | 0.886 | 0.700 | 0.835 | 0.828 | |
Table 1: Basic information of the two groups of patients
There was no statistically significant difference between the two groups pre-treatment assessments for abdominal discomfort, fullness, dryness, firmness, nausea and vomiting, temperature, dry mouth and thirst, short urine, and redness (p>0.05). Following treatment, the Traditional Chinese Medicine (TCM) points in both groups dropped, but the research group had lower points for abdominal discomfort, fullness, dryness and hardness, nausea and vomiting, tidal temperature, dry mouth and thirst, and short and red urine than the control group (p<0.05, fig. 2A-fig. 2F). Prior to therapy, there was no statistically significant difference between the two groups' levels of WBC, hs-CRP, TNF-α, and IL-6 (p>0.05). Following treatment, the levels of inflammatory factors decreased in both groups, with the research group showing lower levels of WBC, hs-CRP, TNF-α, and IL-6 than the control group (p<0.05, fig. 3).
Fig. 2: Evaluation of the two groups' TCM syndrome scores, (A): An evaluation of abdominal pain; (B): An evaluation of hardness, dryness and
fullness; (C): A contrast between nausea and vomiting; (D): ASR tidal fever comparison; (E): A comparison between thirst and dry mouth and (F):
A contrast between short and crimson urine
Note: *p<0.05 and #p<0.05,
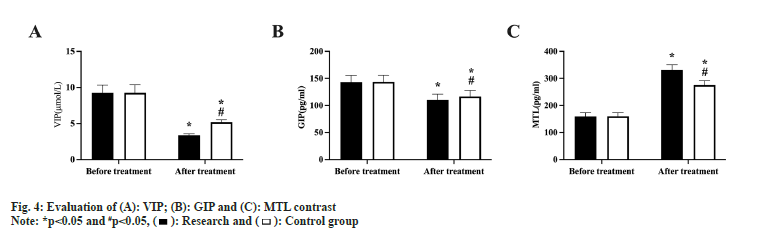
Prior to treatment, there were no statistically significant variations between the two groups' VIP, GIP, and MTL levels (p>0.05). Following treatment, MTL levels increased in both groups, with the research group being higher than the control group (p<0.05, fig. 4), whereas VIP and GIP levels declined in both groups, with the observation group being lower than the control group (p<0.05, fig. 4A-fig. 4C). VIP and GIP levels also decreased in both groups.
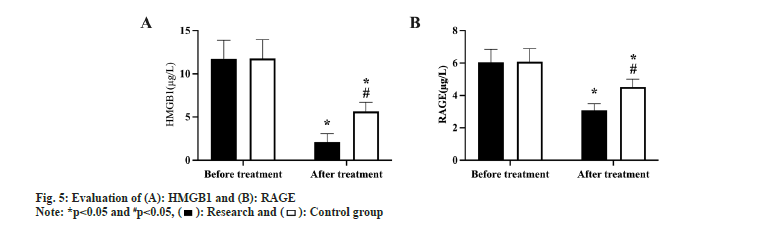
Prior to treatment, there was no statistically significant difference in the levels of HMGB1 and RAGE between the two groups (p>0.05). Following treatment, HMGB1 and RAGE levels dropped in both groups, with the research group experiencing a greater decline than the control group (p<0.05, fig. 5A and fig. 5B).
After treatment, RAGE, sTREM-1, and APACHE II score all increased in the research group according to Pearson correlation coefficients (p<0.05, fig. 6A and fig. 6B), indicating that an increase in APACHE II score was accompanied by a corresponding increase in RAGE and sTREM-1 levels.
Acute pancreatitis is mainly characterized by sudden onset of severe abdominal pain, most patients are self-limited and have a good prognosis, but some patients develop into severe pancreatitis due to untimely treatment or low effectiveness of treatment, which seriously affects health and even life safety[7]. Hypercalcemia, heavy alcohol usage, overeating, among many other factors, can induce acute pancreatitis. TCM has a history of thousands of years and its treatment methods include internal medicine and external treatment such as acupuncture, which has been useful in the management of many medical and surgical diseases. Qingyi decoction is a Chinese herbal preparation consisting of a variety of Chinese herbs. The formula includes Chai Hu, which can clear the liver and regulate Qi to relieve pain. Combined with Bai Shao, the formula is effective in nourishing the blood and softening the liver, effectively relieving pain; Scutellaria baicalensis, rhubarb, Huang Lian and Jin Yin Hua are efficient in removing fire and poisons, drying dampness, and clearing heat; Hou Pu can help relieve Qi and pain and eliminate fullness; Citrus aurantium and Sha Ren can warm the middle of the body and regulate Qi, harmonies the stomach and clear the spleen; tiger Balm and Dan Shen can invigorate the blood and disperse stasis, cool the blood and eliminate carbuncles. The whole formula has the effect of draining the liver and Qi, clearing heat and toxins, and clearing the lining and attacking the bottom[8-10]. Our research showed that Western medicine and modified Qingyi decoction had positive synergistic effects and effectively decreased the severity of the condition in individuals with acute pancreatitis. This was consistent with the findings of previous studies that showed Qingyi decoction with modification and western medicine could effectively alleviate clinical symptoms and shorten the improvement time of clinical symptoms in the research group compared to that in the control group[11].
In our study, we investigated the effects of Qingyi decoction in combination with western therapy on inflammatory variables in patients with acute pancreatitis. The difference between the research group and the control group in WBC, hs-CRP, TNF-, and IL-6 levels demonstrated that Qingyi decoction with modification assisted in lowering the inflammatory response in patients with acute pancreatitis. We speculate that the reason for this is that the saponins and flavonoids in Bei Chai Hu have immunomodulatory, hepatoprotective, antipyretic and anti-inflammatory pharmacological effects and can control WBC proliferation and aggregation. Paeoniflorin and paeonilactone glycosides in Baishu have a reducing and increasing effect, promote the secretion of anti-inflammatory factors, exert antiinflammatory and analgesic effects, and regulate the apoptotic rhythm[12,13]. The "waterfall-like" inflammatory response and the unbalanced proinflammatory- anti-inflammatory equilibrium in the early stages of acute pancreatitis can therefore be eased by Qingyi decoction, leading to a substantial decrease in the level of inflammatory components in the body.
Gastrointestinal hormone levels are an important indicator of gastrointestinal function, Therefore, in two patient groups, we also examined and compared the levels of gastrointestinal hormones. VIP, GIP and MTL are common gastrointestinal hormones. Among them, VIP and GIP are hormones of the glucagon family, and the regulation of their expression is important for the control of acute pancreatitis; MTL is an indicator closely related to gastrointestinal function[14,15]. VIP, GIP, and MTL levels were found to be lower in the research group than in the control group, while VIP and GIP levels were higher in the research group than in the control group. This finding suggests that the Qingyi decoction with modification, combined with traditional western medicine, helped to promote gastrointestinal hormone normalization and pancreatic tissue repair in patients with acute pancreatitis.
Acute pancreatitis induces a stress response in the body that causes massive secretion of HMGB1 by damaging pancreatic cells as well as activating monocytes and epithelial cells[16]. A late proinflammatory factor known as HMGB1 interacts with RAGE and Toll-like receptors to set off a series of metabolic processes that support the generation and secretion of inflammatory mediators and maintain the chronic inflammatory state associated with pancreatitis[17]. The HMGB1-RAGE signaling pathway can further promote the activation of nuclear factor-κB, leading to the development of multi-organ dysfunction syndrome[18]. Therefore, by further investigating the mechanisms of HMGB1- RAGE signaling pathway in acute pancreatitis may provide us with new targets in order to treat severe pancreatitis. In previous studies, HMGB1 and RAGE levels have been initially shown to have a connection to the onset of acute pancreatitis[19,20].
Therefore, we also further investigated the significance of changes in HMGB1 and RAGE during the treatment of acute pancreatitis with Qingyi decoction with modification adjunctive western medicine. The results showed that both levels decreased after treatment and were positively correlated with the patients APACHE II scores. This again confirmed the good therapeutic effect of Qingyi decoction with modification adjunctive western medicine in acute pancreatitis and the close correlation between HMGB1 and RAGE and acute pancreatitis. At the same time, the above experimental results also suggest that by serving as clinical references and enabling prompt patient interventions, HMGB1 and RAGE can be employed as markers to predict the future course and prognosis of acute pancreatitis.
Although this study confirmed the significant role of Qingyi decoction with modification as an adjunct to western medicine in the treatment of acute pancreatitis in several ways, we only included a small number of cases due to objective limits, which could have led to statistical computation chance, and we did not follow up with the patients to find out their prognosis. To give a more trustworthy resource for acute pancreatitis clinical treatment, future studies will increase the number of cases chosen and conduct patient follow-up in order to conduct more in-depth studies on the mechanism of action and the impact on prognosis of Qingyi decoction with modification adjunctive western medicine.
Western medicine may effectively cure acute pancreatitis using Qingyi decoction with a few adjustments. Clinical symptoms can be efficiently treated with it, and it can also reduce inflammatory reactions and regulate HMGB1 and RAGE levels.
Conflict of interests:
The authors declared no conflict of interests.
References
- Lankisch PG, Apte M, Banks PA. Acute pancreatitis. Lancet 2015;386(9988):85-96.
[Crossref] [Google Scholar] [PubMed]
- Lee PJ, Papachristou GI. New insights into acute pancreatitis. Nat Rev Gastroenterol Hepatol. 2019;16(8):479-96.
[Crossref] [Google Scholar] [PubMed]
- Li J, Cao H, Xiao T. Clinical observation on the treatment of gastrointestinal dysfunction in patients with acute pancreatitis with da cheng qi tang. Chin J Integ Med Digestion 2021;29(10):686-90.
- Li H, Chi ZT, Song WJ. Effects of dahuang cheng qi tang combined with ustekin on intestinal mucosal function and immune function in patients with severe acute pancreatitis. World Chin Med 2018;13(06):1412-5.
- Wang CY, Li F, Zhao YP. Guidelines for the diagnosis and treatment of acute pancreatitis. J Clin Hepatobiliary Dis 2015;31(1):17-20.
- Zhang SS, Li HZ. Expert consensus opinion on the diagnosis and treatment of acute pancreatitis in Chinese medicine. J Clin Hepatobiliary Dis 2017;33(11):2052-7.
- Gardner TB. Acute pancreatitis. Ann Intern Med 2021;174(2):ITC17-32.
[Crossref] [Google Scholar] [PubMed]
- Cao WJ, Wei FX, Su GH. Evaluation of the efficacy of Qing pancreatic tang combined with growth inhibitor in the treatment of severe acute pancreatitis. Chin Tradit Chin Med Emerg 2018;27(9):1542-51.
- Wang Z, Fu T, Liu K. Effect of Qing pancreatic tang combined with early micro ecological enteral nutrition on serum amylase, inflammatory cytokines and prognosis in patients with acute pancreatitis. J Liaoning Univ Chin Med 2018;20(3):95-8.
- Yu Z, Liu Y, Wan Y. Efficacy of chai hu qing pancreatic tang combined with Chinese herbal preserved enema in the treatment of acute pancreatitis (damp-heat internalized type) and the effect on serum inflammatory factors and gastrointestinal function of patients. Sichuan Tradit Chin Med 2022;40(10):107-10.
- Luan XF, Wang L, Gai XEF. Adjuvant treatment of severe pancreatitis with qing pancreatic tang plus reduction and its effect on the levels of blood amylase, tumor necrosis factor-α and interleukin-6. Chin J Tradit Chin Med 2020;38(3):50-3.
- Yao HM, Fu XX, Lu L. Clinical observation on the treatment of severe acute pancreatitis-associated lung injury with Qing pancreatic tang enema combined with ambroxol hydrochloride. Chin Tradit Chin Med Emerg 2021;30(7):1257-60.
- Feng Y, He CW, Li B. Efficacy of Qing pancreatic tang with acupuncture in treating patients with acute severe pancreatitis of liver-depression and qi stagnation type and the effect on serum inflammatory factors. World Chin Med 2018;13(4):857-60.
- Storgaard H, Cold F, Gluud LL, Vilsboll T, Knop FK. Glucagon-like peptide-1 receptor agonists and risk of acute pancreatitis in patients with type 2 diabetes. Diabetes Obes Metab 2017;19(6):906-8.
[Crossref] [Google Scholar] [PubMed]
- Sandrasegaran K, Tahir B, Barad U, Fogel E, Akisik F, Tirkes T, et al. The Value of secretin-enhanced MRCP in patients with recurrent acute pancreatitis. AJR Am J Roentgenol 2017;208(2):315-21.
[Crossref] [Google Scholar] [PubMed]
- Kang R, Zhang Q, Hou W, Yan Z, Chen R, Bonaroti J, et al. Intracellular Hmgb1 inhibits inflammatory nucleosome release and limits acute pancreatitis in mice. Gastroenterology 2014;146(4):1097-107.
[Crossref] [Google Scholar] [PubMed]
- Irie Y, Tsubota M, Ishikura H, Sekiguchi F, Terada Y, Tsujiuchi T, et al. Macrophage-derived HMGB1 as a pain mediator in the early stage of acute pancreatitis in mice: Targeting RAGE and CXCL12/CXCR4 axis. J Neuroimmune Pharmacol 2017;12(4):693-707.
[Crossref] [Google Scholar] [PubMed]
- Yang J, Tang X, Wu Q, Ren P, Yan Y, Liu W, et al. Heparin protects severe acute pancreatitis by inhibiting HMGB-1 active secretion from macrophages. Polymers (Basel) 2022;14(12):2470.
[Crossref] [Google Scholar] [PubMed]
- Wang J, Zou Y, Chang D, Hong DQ, Zhang J. Protective effect of Dachengqi decoction on the pancreatic microcirculatory system in severe acute pancreatitis by down-regulating HMGB-TLR-4-IL-23-IL-17A mediated neutrophil activation by targeting SIRT1. Gland Surg 2021;10(10):3030-44.
[Google Scholar] [PubMed]
- Wang YS, Li YY, Wang LH, Kang Y, Zhang J, Wang K, et al. Tanshinone IIA attenuates chronic pancreatitis-induced pain in rats via downregulation of HMGB1 and TRL4 expression in the spinal cord. Pain Physician 2015;18(4):E615-28.
[Google Scholar] [PubMed]