- *Corresponding Author:
- Lu Yanan
Department of Neurology, Xuchang University, Xuchang, Henan Province 461000,China
E-mail: luyanannursing@163.com
| This article was originally published in a special issue, “Current Trends in Pharmaceutical and Biomedical Sciences” |
| Indian J Pharm Sci 2022:84(5) Spl Issue “193-198” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
To explore the effects of ADOPT-based problem solving model on cognitive impairment and motor function in stroke patients. A retrospective selection of 60 patients who came to our hospital for treatment and treatment due to stroke from December 2020 to December 2021. According to different nursing methods, they were divided into two groups. The research group adopted the nursing method based on the ADOPT problem-solving model and the control group adopted the conventional nursing model. Before nursing, the difference of positive and negative emotional performance between the two groups was not comparable (p>0.05). After nursing, the scores of negative emotions of the two groups of patients decreased, while the scores of positive emotions increased. In the control group, the difference was statistically significant (p<0.05). There was no comparable difference in mini-mental state examination scores between the two groups before nursing (p>0.05). After nursing, mini-mental state examination in both groups was improved and the research group was higher than the control group, and the difference was comparable (p<0.05). There was no comparable difference in CCS scores between the two groups before nursing (p>0.05). The CCS scores of both groups decreased after nursing and the difference between the study and the control group was comparable (p<0.05). The Barthel index in both groups increased after treatment and the research group was higher than the control group, and the difference was comparable (p<0.05). The nursing method based on the ADOPT problem solving model has a positive effect in the nursing of stroke patients, which is beneficial to regulate cognitive function, improve the motor function of stroke patients and promote the recovery of patients.
Keywords
Stroke, cognitive function, motor function, malnutrition
Deaths from stroke have decreased over the past decade. In addition, the incidence of new and recurrent strokes is declining, likely due to increased use of specific preventive medicines such as statins and antihypertensives[1,2]. Despite these positive trends in morbidity and mortality, many strokes are still preventable. The main modifiable risk factors were hypertension, diabetes, smoking and hyperlipidemia, as well as lifestyle factors such as obesity, diet/ malnutrition and physical inactivity. However, cognitive and motor functions are severely affected in stroke patients[3]. After a stroke occurs, in addition to treatment, scientific and precise care is essential. ADOPT-based problem solving model is a new type of intervention model with problem-solving as its main purpose. Patient relationship, mobilize patients’ subjective initiative and encourage patients to carry out self-care activities[4]. It is worth exploring whether the application of this model in stroke care has a positive effect. Therefore, this study mainly explored the effects of ADOPT-based problem solving model on cognitive impairment and motor function in stroke patients.
Materials and Methods
General information:
A retrospective selection of 60 patients who came to our hospital for treatment and treatment due to stroke from December 2020 to December 2021. According to different nursing methods, they were divided into two groups. The research group adopted the nursing method based on the ADOPT problem solving model and the control group adopted the conventional nursing model. The general information of the patients was shown in Table 1.
| Group | Research group | Control group | t/χ2 | p |
|---|---|---|---|---|
| n | 30 | 30 | 5.255 | 0.000 |
| Age | 46.9±5.1 | 46.5±6.7 | 6.134 | 0.001 |
| Gender | ||||
| Man | 18 | 17 | 5.113 | 0.001 |
| Woman | 12 | 13 | 4.131 | 0.002 |
| Course of disease | 2.5±1.1 | 2.9±1.5 | 6.454 | 0.000 |
| Have received treatment | ||||
| Yes | 8 | 5 | 3.120 | 0.001 |
| No | 22 | 25 | 4.970 | 0.000 |
| Serious condition | ||||
| Mild | 11 | 9 | 5.124 | 0.002 |
| Moderate | 14 | 15 | 4.621 | 0.003 |
| Severe | 5 | 6 | 5.389 | 0.000 |
| Education level | ||||
| Primary school | 4 | 3 | 3.455 | 0.000 |
| Junior high school | 18 | 20 | 5.152 | 0.000 |
| High school | 8 | 7 | 5.410 | 0.000 |
Table 1: Comparison of General Data Between two Groups of Patients (n %)
Inclusion criteria: Those who meet the diagnostic criteria for stroke; aged 30-68 y old, male or female; voluntarily participate in clinical research and sign informed consent.
Exclusion criteria: Patients with psychotic disorders and patients who are participating in other clinical trials.
Methods:
Patients in the control group: Traditional nursing methods were adopted. After admission, the patients underwent complete relevant examinations, given standardized stroke treatment and cooperated with routine nursing care.
Basis of routine treatment: On the basis of routine treatment, patients in the study group were given a 6 mo intervention based on the ADOPT problem- solving model to implement health education. The main contents were to evaluate the patient’s self- management attitude, incentive interviews were used and open-ended questions were used to guide patients to conduct autonomous conversations such as: “Do you understand blood pressure and blood sugar monitoring at home?” “What do you think about your own management?” patiently answering patient questions, giving affirmation and encouragement when appropriate and emphasizing long-term self-management; carry out peer education and invite patients with better self-control to communicate with each other, so as to enhance the self-confidence of patients; through family intervention, encourage the main family nursing staff to provide more support and supervision to the patient, so as to create a healthy living environment for the patient. Helping patients identify their health problems, such as major problems they encounter at home, through the analysis of the patient’s inpatient nursing records, the “Stroke Patient Self-Management Questionnaire” was analyzed from the aspects of self-management confidence, daily maintenance, compliance, etc.; their strengths and weaknesses were dissected, helping them to define and identify problems, thereby motivating them to actively change their bad behaviors; open- mindedness, with a creative and open-minded way of thinking, to promote patients to play an active role in setting self-management goals, in the above defined self-management issues, patients are encouraged to put forward their own opinions or opinions and to formulate their own preliminary self-care goals. Provide appropriate guidance from a professional perspective. Provide help for patients to develop effective programs. According to the above self-care goals, the patient made a detailed plan by himself, and the nursing staff provided professional support, and invited the main family nursing staff to participate, and provided encouragement and assistance. Implement, instruct and urge patients to implement the program. Help patients list their own goals and plans, and record daily self-care in detail in the “Self-Management Manual” and check with nurses to evaluate efficacy, summarize successful experiences, and help patients based on existing problems, develop goals and plans in a timely manner.
Observation indicators:
Before nursing and after the nursing cycle, the two groups of patients were evaluated. The Mini-mental State Examination (MMSE) was used to judge the cognitive ability and the comprehensive score was 30. The higher the score, the stronger the cognitive ability; using the Chinese version of the Cognitive Emotional Regulation Questionnaire (CERQ-C) to evaluate the cognitive coping strategies that individuals often use when facing negative life events. The higher the score, the more frequent use of a certain cognitive method; in the neurological function, the CSS is used as the evaluation standard and its score is between 0-45, the damage to neurological function is severe as the score increases. Activities of daily living were assessed by the Barthel index, with a total of 100 points. The higher the score, the greater the living ability.
Statistical methods:
The data were analyzed by Statistical Package for the Social Sciences (SPSS) 19.0 and the count was tested by Chi-sqaure (χ2), and the measurement was tested by t test (x? ±s). p<0.05 indicated a significant difference.
Results and Discussion
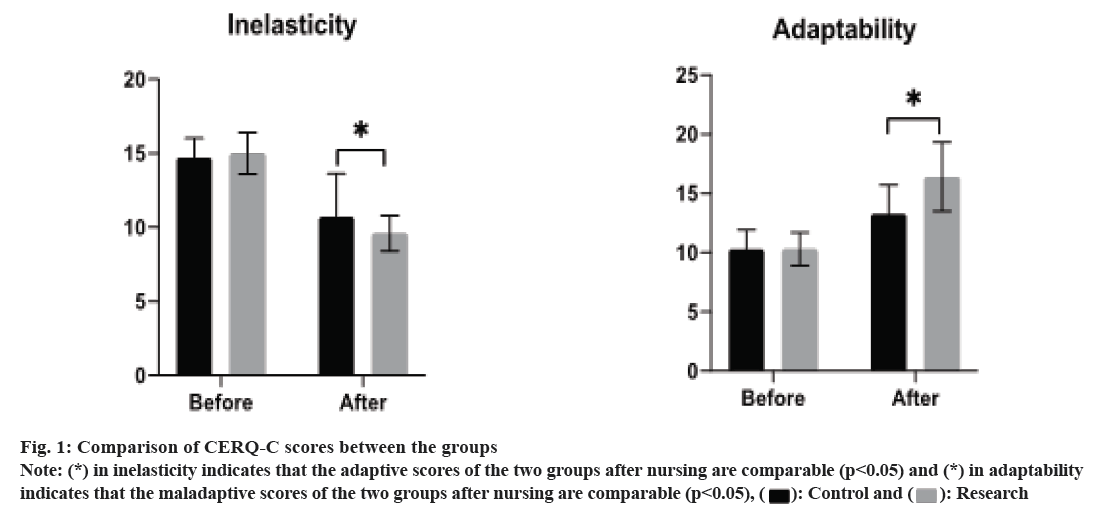
Comparison of CERQ-C scores between the two groups of patients; before nursing, there was no significant difference in the performance of positive and negative emotions between the two groups of patients (p>0.05). After nursing, the scores of negative emotions of the two groups of patients decreased, while the scores of positive emotions increased and the scores of the patients in the study group changed more than in the control group, the difference was statistically significant (p<0.05), as shown in Table 2 and fig. 1.
| Group | Time | Adaptability (positive emotions) | Maladaptability (negative emotions) |
|---|---|---|---|
| Control group | Before nursing | 10.3±1.6 | 14.7±1.3 |
| After nursinga | 13.3±2.4 | 10.7±2.9 | |
| Research group | Before nursing | 10.3±1.4 | 15.0±1.4 |
| After nursingab | 16.4±2.9 | 9.6±1.2 |
Table 2: Comparison Of CERQ-C Scores Between two Groups of Patients (Fraction, x?±s)
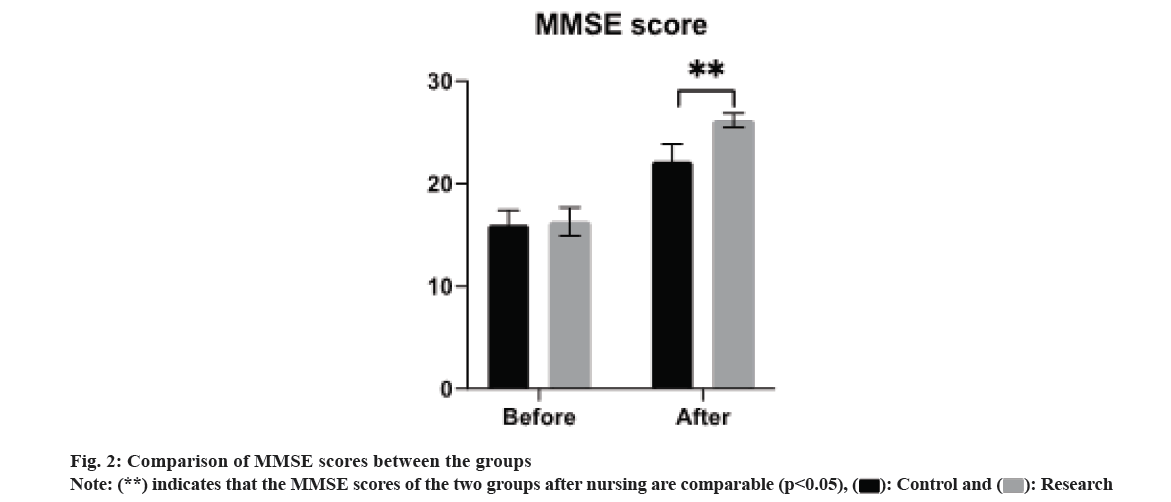
Before nursing, there was no significant difference in the MMSE scores of the two groups of patients (p>0.05). After nursing, the MMSE scores of the two groups of patients gradually increased. The MMSE scores of the patients in the study group were significantly higher than those in the control group, and the difference was statistically significant (p<0.05), as shown in Table 3 and fig. 2.
| Group | n | Before nursing | After nursing |
|---|---|---|---|
| Control group | 30 | 16.02±1.40 | 22.20±1.70 |
| Research group | 30 | 16.30±1.40 | 26.20±0.70 |
| t | 1.295 | 12.126 | |
| p | >0.05 | <0.05 |
Table 3: Comparison of MMSE Scores Between the two Groups of Patients (Fraction, x?±s)
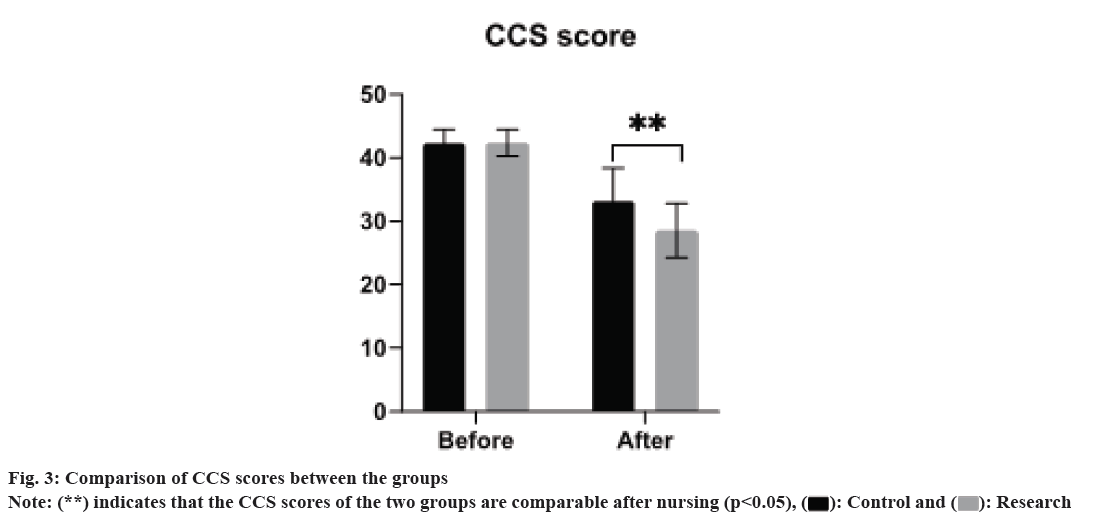
Before nursing, there was no general difference in the CCS scores of the two groups of patients (p>0.05). After nursing, The CCS scores of both groups decreased and the research group was lower than the control group, and the differences were comparable (p>0.05), as shown in Table 4 and fig. 3.
| Group | n | Before nursing | After nursing |
|---|---|---|---|
| Control group | 30 | 42.26±2.22 | 33.20±5.18 |
| Research group | 30 | 42.35±2.14 | 28.51±4.24 |
| t | 1.295 | 12.126 | |
| p | >0.05 | <0.05 |
Table 4: Comparison of CCS Scores Between the two Groups of Patients (FRACTION, x?±s)
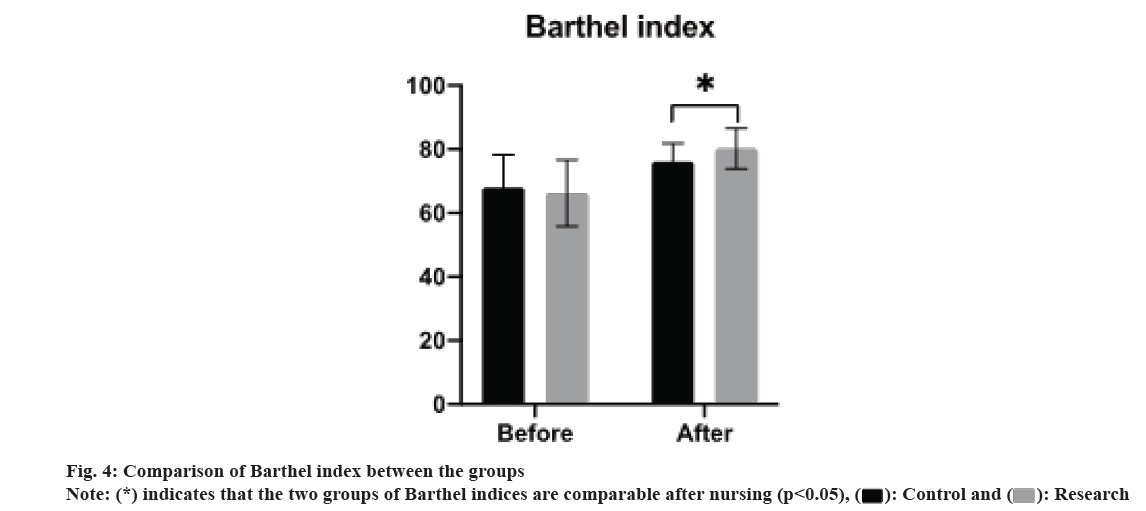
Before nursing, there was no significant difference in the Barthel index between the two groups of patients (p>0.05). After nursing, the Barthel index of the two groups of patients gradually increased. The Barthel index of the patients in the study group was significantly higher than that of the patients in the control group and the difference was statistically significant (p<0.05), as shown in Table 5 and fig. 4.
| Group | n | Before nursing | After nursing |
|---|---|---|---|
| Control group | 30 | 68.04±10.25 | 76.20±5.71 |
| Research group | 30 | 66.30±10.43 | 80.23±6.30 |
| t | 1.295 | 12.126 | |
| p | >0.05 | <0.05 |
Table 5: Comparison Of Barthel Index Between two Groups of Patients (Fraction, x?±s)
With the aging of the world population, stroke has become the second most common disease and the incidence rate is increasing year by year. In recent reports, there are nearly 2000 new stroke cases worldwide. In my country’s stroke survey report, the incidence of 40-70 y old increased from 198/100 000 in 2002 to 379/100 000 in 2013, with an average annual increase of 8.3 %[5-8]. The recurrence rate in patients following their first stroke was 17.1 % in the subsequent year.
Stroke is mainly due to poor cerebral blood flow and is divided into two types as hemorrhagic stroke and ischemic stroke. Among them, more than 80 % of stroke patients are ischemic strokes. Stroke accounts for nearly 30 % of global deaths and is a common neurological disease[9,10]. Up to 50 % of stroke survivors have chronic disabilities that severely impact their daily activities and quality of life. In stroke patients, loss of balance and gait, as well as cognitive and motor impairments is major factors affecting the patient’s independent functioning and participation in activities. Nursing care of stroke patients is more complicated. Nursing staff is not only responsible for nursing, but also needs to cooperate with multidisciplinary teams to help patients recover, interact and support patients in nursing, and respect patients. Various rehabilitation needs, support and encourage patients to carry out rehabilitation exercises, can master and give feedback on the progress of rehabilitation, help rehabilitation teachers to adjust the plan, so that patients can quickly integrate into the life of society.
The prognosis of stroke patients depends on the impact of complications such as chronic functional impairment and cognitive impairment. Mortality rates are generally 15 % and 50 % at 1 mo and 5 y after stroke, respectively. Movement disorders are the most common after stroke, the main cause of long-term disability in the world. Among them, 85 % of patients have movement disorders after acute stroke and it is calculated that about 55 %-75 % of patients have upper or lower extremity functional limitations[11]. 50 %–60 % of patients have some degree of motor dysfunction after stroke. Nearly 60 % of stroke patients experience cognitive decline in attention, memory and executive function[12]. Due to functional and cognitive impairments in post-stroke patients, limb function and daily activities are restricted, which are key factors in decreased quality of life.
Stroke patients are mainly treated in nursing care. At this stage, the research on nursing intervention is more concerned[13,14]. For patients who had undergone surgery, the implementation of systematic nursing interventions resulted in a reduction in complications and an increase in nursing satisfaction. When the routine nursing program is adopted, the patients have obvious psychological problems during their stay in the hospital, which seriously affects the rehabilitation effect. Many scholars have made great efforts to find an effective nursing intervention plan and the study found that the ADOPT problem-solving model has unique advantages in clinical practice. The ADOPT problem-solving model emphasizes the fundamental role of attitude in problem-solving and actively guides patients to adopt an open-minded approach to finding practical solutions by defining their health problems. After comprehensively assessing the patient’s problem-solving ability, clinical nurses’ work with patients to actively solve problems, formulate plans and implement them using existing clinical nursing resources. Problem management is one of the four management methods. It focuses on problem solving and solves problems through problem discovery, retrospective analysis, and four performance improvement processes. It is a kind of administration using problems. Nursing management method mainly includes nursing problems in terms of lifestyle, diet, functional exercise and psychology[15]. Problem-based care can better meet the needs of the patient than traditional care. Problem-based care is based on the patient’s Glasgow Coma Scale (GCS) score, cognitive function (orientation, immediate or delayed memory and writing instructions etc.), neurological function (consciousness, horizontal gaze and muscle strength); in terms of daily diet, clothing, etc., the recovery effect of recovery activities was significantly better than that of the control group.
The nursing method of the solution model has a positive effect in the nursing of stroke patients, which is conducive to regulating cognitive function, improving the motor function of stroke patients and promoting the recovery of patients.
Conflict of interests:
The authors declared no conflict of interests.
References
- Delavaran H, Jönsson AC, Lövkvist H, Iwarsson S, Elmståhl S, Norrving B, et al. Cognitive function in stroke survivors: A 10-year follow-up study. Acta Neurol Scand 2017;136(3):187-94.
[Crossref] [Google Scholar] [PubMed]
- Yeh TT, Wu CY, Hsieh YW, Chang KC, Lee LC, Hung JW, et al. Synergistic effects of aerobic exercise and cognitive training on cognition, physiological markers, daily function and quality of life in stroke survivors with cognitive decline: Study protocol for a randomized controlled trial. Trials 2017;18(1):405.
[Crossref] [Google Scholar] [PubMed]
- Zhang B, Li D, Liu Y, Wang J, Xiao Q. Virtual reality for limb motor function, balance, gait, cognition and daily function of stroke patients: A systematic review and meta-analysis. J Adv Nurs 2021;77(8):3255-73.
[Crossref] [Google Scholar] [PubMed]
- Bo W, Lei M, Tao S, Jie LT, Qian L, Lin FQ, et al. Effects of combined intervention of physical exercise and cognitive training on cognitive function in stroke survivors with vascular cognitive impairment: A randomized controlled trial. Clin Rehabil 2019;33(1):54-63.
[Crossref] [Google Scholar] [PubMed]
- Dharmasaroja PA. Temporal changes in cognitive function in early recovery phase of the stroke. J Stroke Cerebrovasc Dis 2021;30(10):106027.
- Renton T, Tibbles A, Topolovec-Vranic J. Neurofeedback as a form of cognitive rehabilitation therapy following stroke: A systematic review. PloS one 2017;12(5):e0177290.
[Crossref] [Google Scholar] [PubMed]
- Hugues N, Pellegrino C, Rivera C, Berton E, Pin-Barre C, Laurin J. Is high-intensity interval training suitable to promote neuroplasticity and cognitive functions after stroke? Int J Mol Sci 2021;22(6):3003.
[Crossref] [Google Scholar] [PubMed]
- Samuelsson H, Viken J, Redfors P, Holmegaard L, Blomstrand C, Jern C, et al. Cognitive function is an important determinant of employment amongst young ischemic stroke survivors with good physical recovery. Eur J Neurol 2021;28(11):3692-701.
[Crossref] [Google Scholar] [PubMed]
- Viktorisson A, Andersson EM, Lundström E, Sunnerhagen KS. Levels of physical activity before and after stroke in relation to early cognitive function. Sci Rep 2021;11(1):1-7.
[Crossref] [Google Scholar] [PubMed]
- Kannan L, Vora J, Bhatt T, Hughes SL. Cognitive-motor exergaming for reducing fall risk in people with chronic stroke: A randomized controlled trial. NeuroRehabilitation 2019;44(4):493-510.
[Crossref] [Google Scholar] [PubMed]
- Broersen LH, Siegerink B, Sperber PS, von Rennenberg R, Piper SK, Nolte CH, et al. High-sensitivity cardiac troponin T and cognitive function in patients with ischemic stroke. Stroke 2020;51(5):1604-7.
[Crossref] [Google Scholar] [PubMed]
- Einstad MS, Saltvedt I, Lydersen S, Ursin MH, Munthe-Kaas R, Ihle-Hansen H, et al. Associations between post-stroke motor and cognitive function: A cross-sectional study. BMC Geriatr 2021;21(1):103.
[Crossref] [Google Scholar] [PubMed]
- Suri R, Rodriguez-Porcel F, Donohue K, Jesse E, Lovera L, Dwivedi AK, et al. Post-stroke movement disorders: The clinical, neuroanatomic and demographic portrait of 284 published cases. J Stroke Cerebrovasc Dis 2018;27(9):2388-97.
[Crossref] [Google Scholar ] [PubMed]
- Sutherly LJ, Belair T, Nahab F. Embolic stroke of undetermined source: A primer for nursing. J Neurosci Nurs 2021;53(1):26-8.
[Crossref] [Google Scholar] [PubMed]
- Harciarek M, Ma?kowska A. Hemispheric stroke: Mood disorders. Handb Clin Neurol 2021;183:155-67.
[Crossref] [Google Scholar] [PubMed]