- *Corresponding Author:
- Z. T. Huang
Department of Trauma Centre, The Third Affiliated Hospital, Hengyang Medical School, University of South China, Hengyang, Hunan 421900, China
E-mail: hzthzt2h@163.com
| This article was originally published in a special issue, “Recent Developments in Biomedical Research and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2022:84(4) Spl Issue “239-248” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To explore the clinical value of damage control resuscitation combined with alanyl glutamine in the treatment of severe multiple trauma sufferers is the main objective of the study. A total of 120 sufferers with injury severity score≥16 points of severe multiple trauma who were admitted to our hospital from November 2019 to February 2022 were selected and separated into blank group and intervention group (group J and group M) according to random grouping method with 40 people in each group. The general information, clinical indicators, thromboelastography indicators, complications and survival rate of the sufferers were recorded. The operation time, coagulation function time, hospitalization time, body temperature recovery time, prothrombin time, activated partial thromboplastin time, blood loss, total fluid input and mortality of the study subjects were statistically significant. The coagulation indexes of the three groups of research subjects before blood transfusion were not statistically significant and the coagulation indexes of the intervention group (J and M groups) after blood transfusion were statistically significant compared with the blank group. Damage control resuscitation combined with alanyl glutamine significantly reduces complication rates in sufferers with severe polytrauma, thereby improving the survival rate of sufferers after surgery.
Keywords
Damage control resuscitation, alanyl glutamine, severe polytrauma, survival rate, traumatic coagulopathy
Clinically serious multiple trauma refers to the trauma of two or more anatomical parts or organs of the body under the action of the same injury factor and at least one injury is life-threatening. It is a prevalent reason of death in developed countries that causes trauma related coagulopathy[1].
Polytrauma is distinct from trauma, which is severe trauma to two or more anatomical sites or organs like trauma in chest with tracheal laceration, trauma in liver, kidney, heart and brain[2]. This disease not only recurs repeatedly, but also accumulates in more parts. While, according to a study which was investigated the simple traumatic wounds in patients who referred to emergency department of Shahid Rajaei Hospital in Tonekabon city in Iran, the simple traumatic wound healing duration was shorter than polytrauma[3].
Experimental models have shown apoptosis in some organs like heart and brain after Ischemia/ Reperfusion (I/R) damage during trauma. Moreover, apoptosis may be a significant factor to develop serious hemorrhagic shock in trauma[1]. In a study which was done on patients with chest trauma and stable hemodynamics, who underwent Video- Assisted Thoracoscopic Surgery (VATS), organ damage was observed[4]. In addition, accidentally falling from the height leads to trauma in chest with tracheal laceration.
Most sufferers are prone to malnutrition due to severe stress, high energy consumption and fast body metabolism. Sufferers with multiple injuries are often in a state of severe physiological dysfunction and a state of bodily metabolic dysfunction, manifested by the "fatal triad" of hypothermia, acidosis and coagulation disorders. About 60 % of severe multi-trauma sufferers are complicated with traumatic coagulopathy on admission, which is associated with systemic inflammatory response syndrome and increases the chance of infection and sepsis, and is an important cause of death in severe multitrauma sufferers[5-7]. Damage Control Resuscitation (DCR) is an extension of the principles of damage control surgery used by trauma surgeons to limit surgical intervention to the management of lifethreatening injuries, while delaying all other surgical interventions until metabolic and physiological impairments are resolved and controlled. The core key to the DCR protocol is to allow lowpressure resuscitation and hemostasis-controlled resuscitation, with the ultimate goal of preventing the occurrence of acute coagulation disorders. Alanyl glutamine is an important substance for cell growth and development in the body. It can provide certain energy for neutrophils and lymphocytes, and is a nutrient that can improve the immune function of sufferers. It is suitable for critically ill sufferers and perioperative sufferers[8,9].
According to a study which was done on young rats with acute hypoxia, glutamine had the ability to inhibit the intestinal mucosa injury and had protective effect. This ability was due to the inflammatory factors, regulation and autophagy[10]. In another study, glutamine remarkably reduced the inflammatory cascade reaction of patients[11].
Not only does it comprehensively relieve the sufferer’s inflammatory response and reduce muscle breakdown, it also enhances autoimmune function. Some scholars have found that DCR combined with alanyl glutamine had a positive therapeutic effect on the intervention of severe multi-injury disease, but there are few related studies where further confirmation is needed[12,13]. Based on this, the study proposes a combined scheme and uses a controlled experiment to analyze its effect on the survival rate and complications of severe multiple trauma sufferers.
Materials and Methods
General information:
A total of 120 sufferers with severe multiple injuries who were admitted to our hospital from October 2019 to February 2022 with an Injury Severity Score (ISS)≥16 were selected and randomly divided into blank group and intervention group (group J, group M), with 40 people in each group. The inclusion criteria were as follows. All sufferers met the diagnostic criteria for severe multi-trauma disease; the coagulation function was normal; the family members signed the informed consent; the sufferers had good cooperation and compliance; Systolic Blood Pressure (SBP)≤90 mmHg. The exclusion criteria were as follows. Death within 30 min after admission; death due to severe craniocerebral injury; severe mental disorder; difficulty in language communication and understanding; incomplete or missing clinical data were excluded from the study. The study was reviewed and approved by the hospital’s bioethics committee.
Research methods:
The treatment plan of the blank group: The blank group was treated with ordinary resuscitation program and parenteral nutrition, mainly for the rapid establishment of venous access depending on the sufferer’s condition, and the use of traditional fluid resuscitation. Sufferers with combined shock need to replenish blood volume in a timely manner, that is, enter a large amount of plasma substitutes, such as hydroxyethyl starch 40, sodium chloride injection, red cell suspension and dextran. The preparation process of the red cell suspension is as follows. Whole blood is collected through triple bags, most of the plasma is removed by centrifugation and red blood cell preservation solution is introduced in a ratio of 1:4 to obtain the final liquid. When the sufferer’s blood pressure basically returns to normal, the sufferer is transferred to the operating room for surgical treatment, that is, the damage control compulsory surgery. After the surgical treatment is completed, the sufferer is transferred to the intensive care unit. After the physical indicators of the sufferer in the ward are stable, the following operations are performed on the sufferer, such as hematoma debridement, major blood vessel repair, partial bowel resection and re-anastomosis. Appropriate treatment should be performed with confirmatory surgery with plate fixation or intramedullary nailing when sufferers have fractures. Table 1 refers to the basic information on the drugs used. During the treatment, it is necessary to ensure that the nitrogen amount is 0.13 g/(kg.d) and the heat is 20 kcal/(kg.d) on the 1st-3rd d, and the nitrogen amount is 0.19 g/(kg.d) during the treatment period of 4-15 d, the heat is 30 kcal/(kg.d). Enteral nutrition interventions were not administered until the sufferer’s gastrointestinal function returned to normal.
| Drugs | Approval batch number | Manufacturing enterprise |
|---|---|---|
| Structural fat emulsion injection (C6-24) | J20160046 | Fresenius Kabi AB, Sweden |
| Fat soluble vitamin for injection (Ⅱ) | H20052572 | Chengdu Tiantaishan Pharmaceutical Co., Ltd. |
| Compound amino acid injection (15-Hemoglobin C (HBC)) | H20065290 | Fuzhou Haiwang Fuyao Pharmaceutical Co., Ltd. |
| 50 % glucose injection | E10983058 | Jiangxi Kelun Pharmaceutical Co., Ltd. |
| Multi trace element injection (Ⅱ) | H20055173 | Guangdong Shixin Pharmaceutical Co., Ltd. |
Table 1: Basic Information of Drugs
The treatment plan of the intervention group: On the basis of the blank group, the intervention group J added the DCR program and firstly, the SBP was maintained at 80-90 mm Hg (1 mm Hg=0.1333 kPa) during the low-pressure resuscitation that was acceptable to the sufferers, so as to effectively grasp the introduction of crystalloids. Most of the resuscitation fluid plasma injected by the sufferer is the main infusion fluid. During the sufferer’s blood volume recovery period, the pH index of the sufferer should be observed to prevent the occurrence of acidosis symptoms. On this basis, hemostatic resuscitation of the sufferer is also required and the resuscitation solution is mainly concentrated solution. After thorough mixing of cryoprecipitated red blood cells, fresh frozen plasma and platelets in a 1:1:1 ratio, tranexamic acid was used to stop the bleeding. During the treatment of the sufferer, the sufferer should be given heat preservation measures, especially during the blood transfusion process, the intravenous warmer can be used to keep warm, and the temperature of the breathing tube should be kept at about 40° to avoid the symptoms of hypothermia. If the sufferer’s body temperature is lower than 35° during the treatment, normal saline gastric treatment can be given. Intestinal perfusion measures normalize the sufferer’s body temperature, with the caveat that the saline temperature needs to be maintained at 40°-42°. The sufferer was then transferred to the intensive care unit after treatment was completed. Intervention group M was given alanyl glutamine injection on the basis of intervention group J, the drug’s national medicine approval name is H20066620, and the manufacturer is Jichuan Pharmaceutical Group Co., Ltd., and the duration is 15 d.
Observation indicators:
The general information, clinical indicators, Thromboelastography (TEG) indicators, complications and survival rate of the sufferers were recorded. General information included gender, age, Body Mass Index (BMI), cause of injury and location of injury. Clinical indicators include operation time, coagulation function time, blood loss, hospitalization time, total fluid input, case fatality rate, body temperature recovery time, Prothrombin Time (PT), Activated Partial Thromboplastin Time (APTT), SBP and venous pressure (Central Venous Pressure, CVP) before, 2 h and 4 h after transfusion. The TEG index was obtained by the Haemoscope Corporation Model 5000 Thrombelastograph by viscometry and the Maximum Amplitude (MA) of clot formation, thrombin formation time (K), and coagulation factor reaction time before and 2 h after blood transfusion were compared, time (R), the origin of clot formation and the angle alpha (α) was formed by the tangent line formed by the arc and the horizontal line. Complications include hypothermia, traumatic coagulopathy and metabolic acidosis. Survival rate was calculated by Kaplan-Meier method for Overall Survival (OS), Progression-Free Survival (PFS) and Local Control (LC), and the follow-up time was 3 y.
Statistical methods:
Statistical Package for the Social Sciences (SPSS) 22.0 was used for data analysis. The test method used to compare data at different time points is the repeated measures variance test; If the measurement data do not follow a normal distribution, they can be related to a quartile and the difference between groups is measured by the non-parametric test method 1; otherwise, the expression method is mean±standard deviation, the intergroup study method is 2, and the intergroup study method is one-way Analysis of Variance (ANOVA). Count data is expressed in columns or percentages and three test methods are used. In the case of data correlation analysis, the Spearman correlation coefficient is a test method for data with a non-normal distribution; otherwise, the Pearson correlation coefficient is used. The detection standard was 0.05 bi-tails.
Results and Discussion
Baseline data comparison of research subjects was explained here. The baseline data is presented in Table 2. There were no significant difference in gender, age, BMI, cause of injury, and injury site among the three groups (p>0.05) and the follow-up experiments were comparable.
| Category | Blank group | Experimental group J | Experimental group M | F | p value | |
|---|---|---|---|---|---|---|
| Gender | Male [n (%)] | 18/45.0 | 19/47.5 | 17/42.5 | 0.958 | >0.05 |
| Female [n (%)] | 22/55.0 | 21/52.5 | 23/48.5 | |||
| Age (y) | 35.26±5.16 | 34.16±4.98 | 36.28±5.64 | 1.121 | >0.05 | |
| BMI (kg/m2) | 22.21±3.21 | 23.15±3.10 | 22.86±2.96 | 0.865 | >0.05 | |
| Cause of injury [n (%)] | Fall | 8/20.0 | 9/22.5 | 8/20.0 | 0.652 | >0.05 |
| Stab | 12/30.0 | 9/22.5 | 11/27.5 | 0.451 | >0.05 | |
| Crush | 9/22.5 | 9/22.5 | 13/32.5 | 0.386 | >0.05 | |
| Traffic accident | 11/27.5 | 13/32.5 | 8/20.0 | 0.698 | >0.05 | |
| Injury site [n (%)] | Limb | 7/17.5 | 9/22.5 | 9/22.5 | 0.968 | >0.05 |
| Pelvis | 11/27.5 | 12/30.0 | 9/22.5 | 0.635 | >0.05 | |
| Chest | 8/20.0 | 7/17.5 | 13/32.5 | 0.988 | >0.05 | |
| Abdomen | 14/35.0 | 12/30.0 | 9/22.5 | 1.021 | >0.05 | |
Table 2: Baseline Data of Study Subjects
Table 3 shows the comparison of clinical indicators related to study subjects and time. The operation time, coagulation function time, hospitalization time, body temperature recovery time, PT, APTT, blood loss, total fluid input and mortality were statistically significant among the three groups (p<0.05).
| Index | Blank group | Experimental group J | Experimental group M | F | p value |
|---|---|---|---|---|---|
| Operation time (h) | 2.36±0.65 | 16.25±3.26 | 29.23±5.26 | 3.251 | <0.05 |
| Coagulation function time (h) | 31.26±3.16 | 19.26±4.16 | 13.21±3.16 | 4.120 | <0.05 |
| Hospitalization time (d) | 26.58±4.25 | 22.16±3.12 | 17.21±1.29 | 3.255 | <0.05 |
| Temperature recovery time (h) | 20.56±5.22 | 12.36±3.15 | 8.91±2.01 | 4.120 | <0.05 |
| PT (h) | 10.56±3.15 | 7.16±2.26 | 5.16±1.68 | 5.261 | <0.05 |
| APTT (h) | 11.54±3.78 | 7.26±2.64 | 5.41±1.32 | 6.121 | <0.05 |
| Bleeding volume (ml) | 2689.26±35.26 | 2232.25±28.52 | 1865.32±21.23 | 7.251 | <0.05 |
| Total liquid input (ml) | 3265.12±587.26 | 2856.26±426.26 | 2038.26±347.21 | 6.584 | <0.05 |
| Case fatality rate (%) | 6//15.0 | 3/7.5 | 2/2.5 | 5.261 | <0.05 |
Table 3: Clinical Indicators Related to Study Object and Time
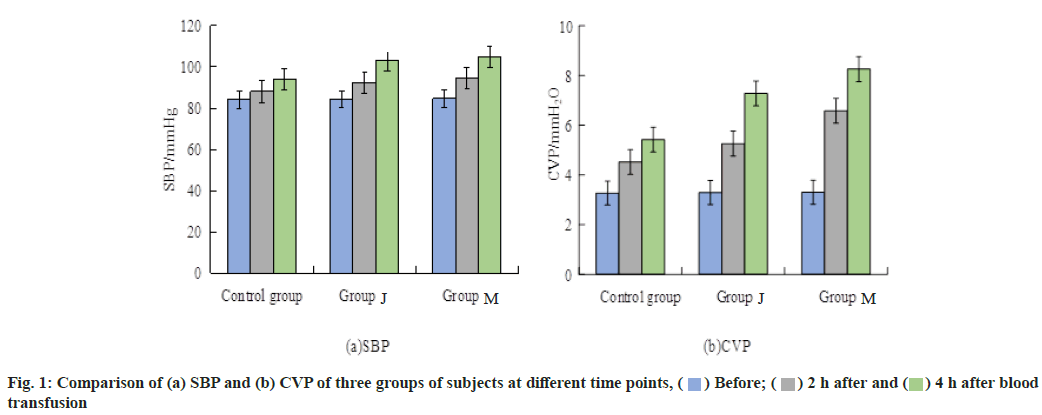
The comparison of SBP and CVP of the three groups of subjects at different time points are shown in fig. 1a and fig. 1b, respectively. Before the sufferers were treated with blood transfusion, the SBP and CVP of the three groups of subjects were not statistically significant (p>0.05). After 2 h and 4 h of blood transfusion treatment, the SBP and CVP of the three groups were statistically significant (p<0.05). For the blank group, the SBP and CVP at different time points were not statistically significant (p>0.05); while for the intervention group J and M, the SBP and CVP at different time points were both statistically significant (p>0.05).
The TEG comparison results of the research subjects are shown in Table 4. It can be seen from Table 4 that the coagulation indexes of the three groups of subjects before blood transfusion were not statistically significant (p>0.05). After blood transfusion, the coagulation indexes of intervention group J and M were statistically significant compared with the blank group (p<0.05).
| Index | Time | Blank group | Experimental group J | Experimental group M | F | p value |
|---|---|---|---|---|---|---|
| Angle (α ) measured in degrees (°) | Before | 75.65±3.26 | 75.46±4.26 | 76.21±4.86 | 1.032 | >0.05 |
| After | 66.32±4.12 | 69.56±5.26*# | 71.21±5.86*# | 4.351 | <0.05 | |
| - | 1.231 | 5.213 | 4.261 | - | - | |
| - | >0.05 | <0.05 | <0.05 | - | - | |
| MA (mm) | Before | 72.36±3.51 | 73.16±4.16 | 72.53±3.84 | 0.987 | >0.05 |
| After | 48.58±12.56 | 72.36±8.59*# | 65.28±10.26*# | 5.231 | <0.05 | |
| - | 1.021 | 4.132 | 3.988 | - | - | |
| - | >0.05 | <0.05 | <0.05 | - | - | |
| R (min) | Before | 3.65±1.05 | 3.68±1.02 | 3.71±1.01 | >0.05 | |
| After | 9.46±2.16 | 7.15±1.62*# | 5.26±1.36*# | <0.05 | ||
| - | 1.002 | 4.651 | 3.562 | - | - | |
| - | >0.05 | <0.05 | <0.05 | - | - | |
| K (min) | Before | 1.20±0.23 | 1.18±0.23 | 1.19±0.24 | >0.05 | |
| After | 2.46±1.21 | 1.86±1.26*# | 1.51±0.37*# | <0.05 | ||
| - | 1.230 | 4.211 | 3.864 | - | - | |
| - | >0.05 | <0.05 | <0.05 | - | - |
Note: *means that there is statistical significance compared with the group before blood transfusion; #means that there is statistical significance compared with the blank group at the same time point
Table 4: TEG Comparison Results of the Subjects
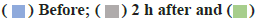
Fig. 2 refers to the comparison of complications among study subjects. The proportions of three types of complications of hypothermia, traumatic coagulopathy and metabolic acidosis in the blank group were significantly higher than those in the intervention group J and the intervention group M (p<0.05). The overall complication rates of group M and three groups were 25.0 %, 12.5 % and 7.5 %, respectively.
Comparison of survival rates of study subjects was explained here. The study divided SBP into two subgroups: Low SBP group and high SBP group. The 3 y OS curves are shown in fig. 3a and fig. 3b. In the low SBP subgroup, the 1 y, 2 y and 3 y OS rates in the blank group were 75.3 %, 40.8 % and 40.8 %, respectively. In the high SBP subgroup, the OS rates were 75.8 %, 42.1 % and 42.1 %, respectively. The corresponding values were significantly higher than those of the other two intervention groups (p<0.05).
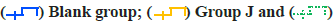
Comparision of 3y PFS curve of two subgroups in low SBP and high SBP groups are shown in fig. 4a and fig. 4b. The 1 y, 2 y and 3 y PFS rates of the blank group in the low SBP subgroup were 72.3 %, 48.9 % and 48.9 %, respectively, and the PFS rates in the high SBP subgroup were 79.3 %, 48.6 % and 48.6 %, respectively. The corresponding values were significantly higher than the values of the other two intervention groups (p<0.05).
Comparision of 3 y LC survival curve of two subgroups in low SBP and high SBP groups are shown in fig. 5a and fig. 5b. The 1 y, 2 y and 3 y LC rates of the blank group in the low SBP group were 68.5 %, 48.5 % and 48.5 %, and the LC rates in the high SBP group were 78.6 %, 48.6 % and 48.69, respectively, and the corresponding values were significantly higher than those of the other two intervention groups (p<0.05).
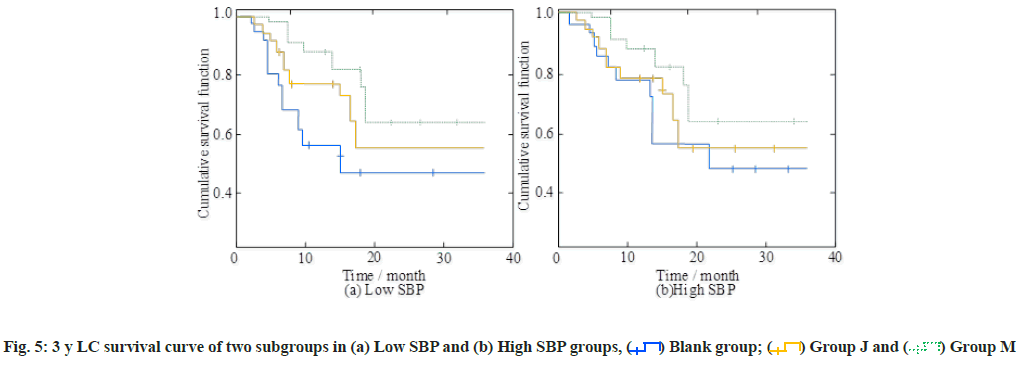
Correlation analysis between survival rate and corresponding indicators was explained here. In order to further verify the correlation between survival time and SBP, fig. 6a and fig. 6b show the correlation between survival time and SBP and CVP in the three groups, respectively.
Different icons in the figure represent different groups of study samples. The correlation of survival time with SBP and CVP were 0.524 and 0.564, respectively, and both were significant (p<0.05).
Sufferers with multiple injuries often have serious, complex and rapidly changing clinical characteristics, which can easily lead to the decrease of sufferer resistance, the increase of susceptibility to infection, the increase of misdiagnosis in clinical treatment, the treatment conflict and other problems, resulting in various physiological dysfunctions. Among them, coagulation dysfunction, hypothermia and metabolic acidosis are the most ordinary causes of death in the treatment of patients with multiple severe injuries, which seriously affect the first aid and clinical efficacy and threaten the life, health and safety of sufferers. In the clinical treatment of sufferers with severe multiple injuries, it is necessary to effectively control the rapidly fatal and reversible serious injuries to ensure the stability of the internal environment. The targeted treatment scheme is adopted at the first time of onset, which can debase incidence of disease aporia and the mortality of sufferers and achieve a very outstanding clinical effect.
The traditional surgical concept emphasizes that one operation can solve all the problems of the sufferer, but due to the long operation time, the operation itself will cause serious damage to the sufferer, which usually leads to the phenomenon that the sufferer is difficult to correct or has a poor prognosis due to shock after the operation and further increases mortality rate. Scholars such as Satoh et al. have found that strict control of surgical indicators and timing according to damage control surgery and reasonable arrangement of surgical procedures can significantly improve the prognosis of sufferers[14,15]. The main purpose of damage control surgery is to use various surgical methods to quickly stop bleeding, control pollution and save lives, thus creating a good opportunity for deterministic surgery, thereby avoiding loss of control, and can reduce the number of deterministic surgery in the treatment of severe multiple trauma risk and improved prognosis. Huang et al. and other scholars have found that the basic requirements and blood perfusion requirements of important organs can be met by infusing a relatively small amount of fluid. The successful implementation of various damage control operations can reduce blood volume, avoid large infusions and large outflows and increase the burden on the body, improve and reduce the interference of fluid resuscitation on the internal environment of the body, promote the recovery of body temperature and coagulation function, and then exert the body’s own hemostatic function and reduce complications, which is also instrumental in long-term improvement of survival rate[16,17].
Compared with traditional Cardiopulmonary Resuscitation (CPR) regimens, medical experts believe that trauma-controlled CPR pays more attention in regulating the abnormal clotting mechanism, especially in patients with unstable hemodynamics, which can correct and deal with a clotting dysfunction over time. Injury control CPR uses plasma for fluid resuscitation to recover the blood volume in the patient’s blood vessels. It can, not only maintain the stability of blood pressure and urine volume, correct metabolic abnormalities, but also regulate the patient’s coagulation mechanism, break down hypothermia, acidosis and clotting function. A vicious circle is formed between the disturbances, thus correcting the disturbed physiological environment. At the same time, the use of trauma control resuscitation minimizes the infusion of crystalloid fluid, thereby reducing the risk and mortality of traumatic coagulation disease.
The overall complication rates of the blank group, intervention group J and intervention group M were 25.0 %, 12.5 % and 7.5 %, respectively. The proportions were significantly higher than those of intervention group J and intervention group M, respectively. It can be inferred that alanyl glutamine combined with DCR can improve the success cure of treatment of sufferers with multiple injuries. Alanyl glutamine can be regarded as a nutritional supplement, which has a role in intervening in the course of sufferers with multiple injuries[18]. Early malnutrition is a common symptom of severe trauma sufferers and the clinical incidence is high. Sufferers are prone to decreased serum protein and autoimmune function, and the incidence of clinical complications will continue to increase, which will affect the clinical treatment and prognosis of sufferers which have a certain impact. Scientific and rational nutritional intervention can increase protein formation in sufferers, mainly due to poor gastrointestinal tolerance in sufferers. Safe infusion methods can meet the basic nutritional needs of sufferers, but due to the high price of parenteral nutrition, the effect of single use is also relatively poor. Therefore, combined with alanyl glutamine therapy, it can fully supplement the energy needed by the sufferer’s body and play an important role in promoting the recovery of the sufferer’s prognosis. It is a reasonable and effective option.
The study found that there were no statistically significant differences in gender, age, BMI, cause of injury and injury site among the three groups. Therefore, the follow-up experimental data comparisons were comparable. The operation time, coagulation function time, hospitalization time, body temperature recovery time, PT, APTT, blood loss, total fluid input and fatality rate of the three groups of subjects were statistically significant. This shows that in the early treatment work, the improvement of the sufferer’s vital signs creates a prerequisite for DCR surgery[19-21]. During the treatment process, it is necessary to keep the sufferer warm and detect blood volume, and take targeted measures according to the actual situation. Many researchers such as Lukin et al. believe that blood volume supplementation can effectively prevent acidosis and effectively reduce postoperative adverse reactions and mortality[22-24]. DCR therapy has a significant effect on the choice of resuscitation scheme and the choice of resuscitation fluid mainly composed of plasma, has a good effect on preventing acidosis.
Predictability of blood loss may also be associated with permissive hypotensive resuscitation and hemostatic resuscitation. The study found that the coagulation indexes of the three groups of subjects before blood transfusion were not statistically significant; but after blood transfusion, the coagulation indexes of the two intervention groups were statistically significant compared with the blank group. Among them, K and R were significantly lower than the blank group, MA and α were significantly higher than the blank group. It can be seen that the combination therapy can greatly improve the blood pressure and blood coagulation status of sufferers due to multiple injuries[13,16,25]. DCR can reduce the risk of traumatic coagulopathy and protect sufferer’s lives. Compared with traditional resuscitation methods, DCR pays more attention in regulating abnormal coagulation mechanism, especially for sufferers with unstable hemodynamics, which can correct and deal with their coagulation dysfunction in time[26-28]. DCR uses plasma for fluid resuscitation to restore blood volume in the sufferer’s blood vessels, which not only maintains stable blood pressure and urine output, corrects metabolic abnormalities, but also regulates the sufferer’s coagulation mechanism, breaking hypothermia, acidosis and coagulation. That is to say, the scheme will form a vicious circle between disorders, thereby correcting the disordered physiological environment[29-31]. At the same time, the use of DCR can minimize crystalloid infusion, thereby reducing the risk and mortality of traumatic coagulopathy[5,6,32].
The results showed that in the low and high SBP subgroups, the 1-3 y OS rate, PFS rate and LC rate of the blank group were significantly lower than those of the two intervention groups. Taking the LC rate as an example, the LC rates of group J in the low SBP subgroup in 1 y, 2 y and 3 y were 77.8 %, 57.2 % and 57.2 % respectively. The LC rates of the high SBP subgroup in the corresponding years were 79.9 %, 54.6 % and 54.6 % respectively. The corresponding LC rates of group M in the intervention group were significantly higher than that of group J in the intervention group. Meanwhile, the values of the corresponding indicators in the blank group were lower than those of the two intervention groups. The study on the survival curve of sufferers with multiple injuries has not been confirmed in the clinic at present and the follow-up clinical experiments need further experiments. The correlation between survival time and SBP and CVP was 0.524 and 0.564 respectively, and both were significant. Therefore, clinicians should pay close attention to the changes of blood pressure during and after the operation in order to improve the success rate of treatment.
Combined with the research reports of the current authoritative medical scholars and the demonstration of the research results, DCR combined with alanyl glutamine can reduce the incidence of complications in sufferers with severe multiple injuries to a great extent, prevent the occurrence of metabolic acidosis, traumatic coagulation disease, hypothermia and other “death triangle” phenomena, and then improve the survival rate of sufferers after surgery and the success rate of clinical treatment of sufferers with multiple injuries. In the follow-up clinic, the number of samples in different regions can be further increased to verify the research conclusions obtained in the study, so as to facilitate its application and promotion in the clinic.
Conflict of interests:
The authors declared no conflict of interest.
References
- Saracoglu A, Tetik S. Trauma-induced apoptosis of endothelial cells. J Med Chem Sci 2019;2(3):92-5.
- Cai Q, Li L, Zhang J, Zhang L, Shen M, Huang Y, et al. The first hybrid surgery in China: Repair of tracheal laceration with extracorporeal membrane oxygenation. Acta Med Mediterr 2022:38(2):1099-102.
- Farzaneh R, Arvan M, Khodaie N, Rahsepar S, Hakemi A, Maleki F, et al. Wounding-to-door time metrics outcome of traumatic simple wounds in emergency department. J Med Chem Sci 2023;6(2):304-12.
[Crossref]
- Khosravi M, Jahanshahi F, Tafreshian A, Kian SMH. Medical evaluation of mortality and complications of thoracoscopic surgery with the help of primary video in patients with thoracic trauma with stable hemodynamics, 2019-2020. J Med Chem Sci 2022;5(3):361-8.
[Crossref]
- Ma J, Han S, Liu X, Zhou Z. Sodium bicarbonated Ringer’s solution effectively improves coagulation function and lactic acid metabolism in patients with severe multiple injuries and traumatic shock. Am J Transl Res 2021;13(5):5043-50.
- Feng J, Zhang Y, Gao X. Experience on single-lung mechanical ventilation combined with damage control in treatment of patients with severe multiple trauma. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2020;32(9):1128-30.
[Crossref] [Google Scholar] [PubMed]
- Sulen N, Šimurina T, Karuc E, Tolić A. Epidural analgesia in multiple injured patients with severe chest trauma: Two case reports and literature review. Acta Clin Croat 2019;58(1):118-23.
[Crossref] [Google Scholar] [PubMed]
- Prata MM, Cavalcante PA, da Silva AV, de Medeiros PH, de Assis Júnior EM, Reyes MA, et al. Alanyl-glutamine protects against damage induced by enteroaggregative Escherichiacoli strains in intestinal cells. J Pediatr Gastroenterol Nutr 2019;68(2):190-8.
[Crossref] [Google Scholar] [PubMed]
- Liu BX, Lo HC, Lee CH. The mechanisms of glutamine-and fish oil-supplemented resuscitation fluids on alleviating oxidative stress of the lung and liver in rats with trauma-hemorrhagic shock. Curr Dev Nutr 2020;4(2):429.
- Shen Y, Zhang ZF, Huang SF, Min JK, Dou XJ, Li HD, et al. The effect of two kinds of modified broström surgeries on pain and aofas score in patients with lateral collateral ligament injury of ankle. Acta Med Mediterr 2022;38:2917-21.
[Crossref]
- Zhang L, Li F, Bai Y, Liu K, Liu M. Effects of glutamine on inflammatory cascade, serum high mobility group protein 1 and heat shock protein in patients with severe pancreatitis. Acta Med Mediterr 2020;36(1):281-5.
- Carter AJ, MacDonald RD. Damage control resuscitation initiated in the prehospital and transport setting: A systems approach to increasing access to blood transfusion. Can J Emerg Med 2019;21(3):318-20.
[Crossref] [Google Scholar] [PubMed]
- Cap AP, Pidcoke HF, Spinella P, Strandenes G, Borgman MA, Schreiber M, et al. Damage control resuscitation. Mil Med 2018;183(2):36-43.
[Crossref] [Google Scholar] [PubMed]
- Satoh K, Furuya T, Okuyama M, Nakae H. A case of refractory serum sodium disorders with severe multiple trauma. Per Med Univ 2019;8:38-40.
- Skoog B, Hedman B. Intrathecal baclofen dosage for long-term treatment of patients with spasticity due to traumatic spinal cord injuries or multiple sclerosis. Ann Rehabil Med 2019;43(5):555-61.
[Crossref] [Google Scholar] [PubMed]
- Huang GB, Hu P, Gao JM, Lin X. Analysis of early treatment of multiple injuries combined with severe pelvic fracture. Chin J Traumatol 2019;22(03):129-33.
[Crossref] [Google Scholar] [PubMed]
- Lu Y, Liu L, Wang J, Cui L. Controlled blood pressure elevation and limited fluid resuscitation in the treatment of multiple injuries in combination with shock. Pak J Med Sci 2018;34(5):1120-4.
[Crossref] [Google Scholar] [PubMed]
- Xiong LJ, Shang LH, Ou XQ, Li Y, Xie XL. Clinical effect of alanyl-glutamine-enriched nutritional support in the treatment of children with abdominal Henoch-Schönlein purpura. Zhongguo Dang Dai Er Ke Za Zhi 2019;21(2):168-171.
- Hayase N, Doi K, Hiruma T, Inokuchi R, Hamasaki Y, Noiri E, et al. Damage-associated molecular patterns in intensive care unit patients with acute liver injuries: A prospective cohort study. Medicine 2018;97(41):e12780.
[Crossref] [Google Scholar] [PubMed]
- Vehviläinen J, Brinck T, Lindfors M, Numminen J, Siironen J, Raj R. Occurrence and prognostic effect of cervical spine injuries and cervical artery injuries with concomitant severe head injury. Acta Neurochir 2020;162(6):1445-53.
[Crossref] [Google Scholar] [PubMed]
- Posada MG, Suñe AB, Sieiro JN, de Arzuaga CS, Soler MC. Damage control resuscitation in polytrauma patient. Rev Esp Anestesiol Reanim 2019;66(7):394-404.
[Crossref] [Google Scholar] [PubMed]
- Ibragimov FI, Kasumov NA. Surgical treatment of multiple and concomitant injuries. Vestn Khir Im I I Grek 2018;177(5):30-5.
[Crossref]
- Martinez F, Alegret N, Carol F, Laso MJ, Zancajo J, García E, et al. Pelvic fracture in the patient with multiple injuries: Factors and lesions associated with mortality. Emergencias 2018;30(2):91-7.
[Google Scholar] [PubMed]
- Lukin SY, Soldatov YP, Diachkov AN. Treatment outcomes in patients with multiple and concomitant trauma managed with minimally invasive osteosynthesis technologies and electromagnetic waves of the terahertz range. Genij Ortop 2021;27(1):6-12.
- Cannon JW. Prehospital damage-control resuscitation. N Engl J Med 2018;379(4):387-8.
[Crossref] [Google Scholar] [PubMed]
- Satyvaldayev MN, Akselrov MA. External stabilization of the thorax in complex treatment of children with severe chest injuries: Description of clinical cases. Pediatric Traumatol Orthop Reconstr Surg 2018;6(2):73-8.
- Singh R, Tripathi D, Jaiswal SP, Singh P, Balar T, Viradiya C. Use of negative pressure wound therapy as a bolster over skin grafts in patients with severe burn injuries at a tertiary care burn centre in India. Burns Open 2021;5(3):137-40.
- Tamás V, Kocsor F, Gyuris P, Kovács N, Czeiter E, Büki A. The young male syndrome-An analysis of sex, age, risk taking and mortality in patients with severe traumatic brain injuries. Front Neurol 2019;10:366.
[Crossref] [Google Scholar] [PubMed]
- Saeednejad M, Zafarghandi M, Khalili N, Baigi V, Khormali M, Ghodsi Z, et al. Evaluating mechanism and severity of injuries among trauma patients admitted to Sina hospital, the National Trauma Registry of Iran. Chin J Traumatol 2021;24(3):153-8.
[Crossref] [Google Scholar] [PubMed]
- Motomiya M, Watanabe N, Konno T, Yasui K. Investigation of work-related injuries in a core hospital in an agriculture and forestry region. J Jpn Assoc Rural Med 2018;67(1):52-7.
- Khalyapina A, Parshikov M, Bolotov D, Zhuravlyova G, Yarygin N. Evaluation of cytokine dynamics in patients with multiple and concomitant closed chest injuries. Russ Sklifosovsky J Emerg Med Care 2021;10(2):318-27.
- Jacq G, Valera S, Muller G, Decormeille G, Youssoufa A, Poiroux L, et al. Prevalence of pressure injuries among critically ill patients and factors associated with their occurrence in the intensive care unit: The pressure study. Aust Crit Care 2021;34(5):411-8.
[Crossref] [Google Scholar] [PubMed]
 4 h after blood transfusion
4 h after blood transfusion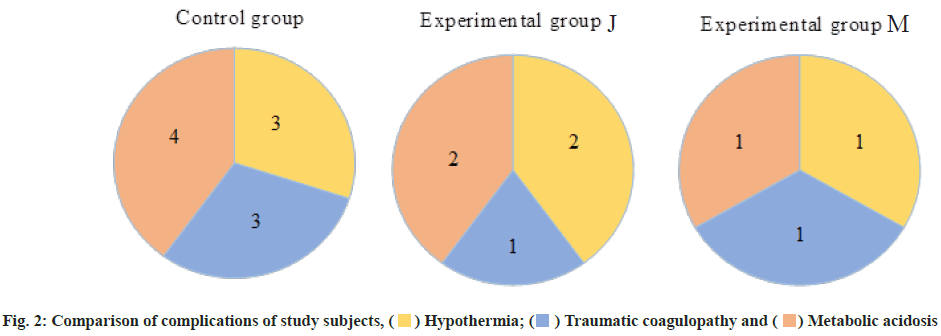
 Metabolic acidosis
Metabolic acidosis
 Group M
Group M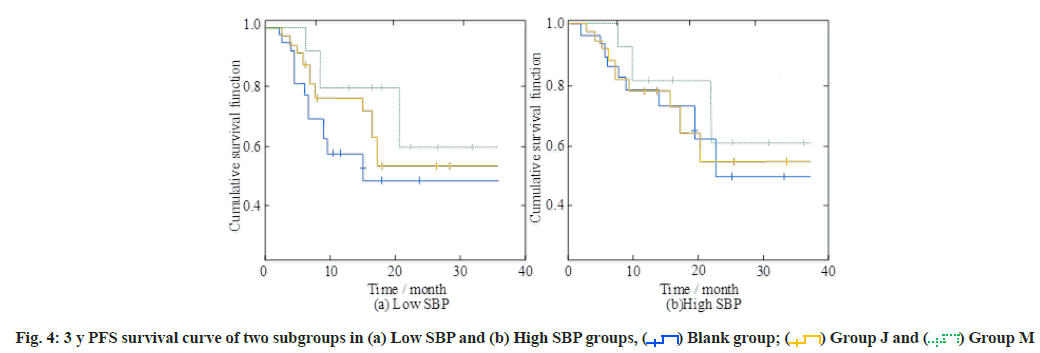
 Group M
Group M



