- *Corresponding Author:
- Jianbin Chen
Jianbin Traditional Chinese Medicine Surgery Clinic, Fuzhou, Fujian 350003, China
E-mail: 18650088878@163.com
| This article was originally published in a special issue, “Recent Progression in Pharmacological and Health Sciences” |
| Indian J Pharm Sci 2024:86(2) Spl Issue “33-39” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To analyze the efficacy of Qingshuanglu in improving burn scars. First, 120 burn individuals were recruited and all the participants were given oral administration of diosmin and then randomized to Meibao Shi Run Shao Shang Gao and Qingshuanglu. Efficacy, visual analogue scale, vancouver scar scale score, pigmentation rate, wound drying time, healing time, safety, and serum inflammatory factor levels were comparatively analyzed. Patients receiving Qingshuanglu treatment showed shorter wound drying and healing time, lower visual analogue score, vancouver scar score, reduced pigmentation rate and total incidence of adverse reactions than those treated with Meibao. Moreover, markedly decreased levels of various serum inflammatory factors were observed in patients receiving Qingshuanglu, lower than the pre-treatment levels and those receiving Meibao. The study demonstrates that Qingshuanglu exposure could effectively repair burn injury, attenuate the inflammatory response, and reduce the scar formation for burn patients.
Keywords
Burn injury, burn scar, Qingshuanglu, diosmin, tumor necrosis factor alpha, C-reactive protein, interleukin-6
Burn injuries represent an under-appreciated medical condition that cause negative physical and emotional consequences to poorly affect quality of life[1]. Burn injuries result from heat, cold, radiation, friction, chemical or electric sources, and most burn injuries are caused by heat from fire, hot liquids, or solids[2]. The severity of burn injuries can be graded into 4 degrees according to the depth and size[3]. The 1st degree burns are superficial burns that only affect the uppermost layer of the skin (epidermis), and the skin becomes red with limited pain experienced in duration. The 2nd degree burns involve superficial partial-thickness, that require dressing and wound care, possibly accompanied by pathologic scar formation, but do not require surgery. However, deep partial-thickness burns might require surgery and will scar. The 3rd degree burns seem to be full-thickness burns that extend through the full dermis and they require protection against infection and surgical management. The 4th degree burns affect deeper tissues, such as muscle or bone, and usually result in loss of the burned part. According to the World Health Organization (WHO), there is an estimated 11 million burn injuries of all types around the world each year. A multitude of studies have shown that severe burns contribute to inflammatory and stress responses, insufficient extracellular matrix production, and declined angiogenesis within a few hours of injury[4]. Although the 1st and 2nd degree burns could heal and do not require surgical intervention, the treatment and recovery from burn injuries is profoundly painful which requires an approach base on interdisciplinary team[5]. Yet, experimental and clinical studies have yielded results with less expectation to improve clinical treatment for burn injuries.
Traditional Chinese Medicine (TCM) and Chinese herbs have extensively demonstrated their values in substantial achievement in anti-inflammatory, anti-bacteria, and tissue reconstruction during the wound closure[6]. The powder made by TCM allows for the growth of new skin and muscle regeneration by clearing heat and toxins, absorbing necrotic tissue and exudate from the wound surface, and activating blood circulation[7]. Diosmin is a flavone glycoside that exhibits multiple pharmacological activities, such as antioxidant activities and anti-inflammatory effects and it has been reported to reduce burn edema[8]. Qingshuanglu, a TCM formula, was developed by The Second Affiliated Hospital of Fujian University of Traditional Chinese Medicine hospital, which primarily contained Taraxacum mongolicum, Myrica rubra root, Ilex pubescens, borneol, bear bile, Callicarpa macrophylla leaves, Cirisum arvense. Qingshuanglu exposure has the ability to promote dryness on the wound surface, accelerate scab formation and healing, achieve pain relief, effectively reduce or repair scars. The primary objective of the study is to investigate the efficacy of Qingshuanglu’s exposure for burn scar improvement compared to Meibao Shi Run Shao Shang Gao, which is the current drug for treating superficial and superficial partial-thickness burns.
Materials and Methods
General information:
This study consecutively considered 120 patients who were treated for burn injuries at the Second Affiliated Hospital of Fujian University of Traditional Chinese Medicine during the period of January 2021 to January 2023.
Inclusion criteria:
The severity of burn injuries was determined by the dermatologist according to the depth and size and classified into different grades. Patients of all the grades, like grade I (superficial burns), grade IIA (superficial partial-thickness burns), grade IIB (deep partial-thickness burns), and grade III (full- thickness burns); patients having total burn area <30 % of the Total Body Surface Area (TBSA); and patients aged (18-65) y were included in the study.
Exclusion criteria:
Presence of a known skin condition, such as psoriasis and skin cancer; presence of caustic burns of upper respiratory and digestive tract; any current ongoing pulmonary, hepatic, renal, hematological, neurological, neoplastic diseases, or psychiatric abnormalities; and pregnancy (tested with Beta (β)-human chorionic gonadotropin test) or breastfeeding patients were excluded.
The study protocols were approved by the Ethics Committee of the Second Affiliated Hospital of Fujian University of Traditional Chinese Medicine. The study was in accordance with the Declaration of Helsinki. All the participants provided written informed consent to participate in the study.
Treatment protocols:
After admitting into the hospital, all the patients were treated with debridement technique according to the cause and degree of burn injury, followed by anti-infection treatment, rehydration treatment, and were orally administered with 500 mg/time of diosmin for 10 d, and twice daily (Aimailang, approval number: X980598, specification: 500 mg×20 tablets). Next, the patients were randomized to different treatment arms: Meibao Shi Run Shao Shang Gao mainly consisting of Coptis chinensis, Phellodendron amurense, Scutellaria baicalensis, earthworm and shell of opium poppy, and Qingshuanglu. The wounds were rinsed with normal saline and then disinfected. Under the sterile condition, the wounds were covered either with with 0.15-0.30 mm of thickness of Shi Run ShaoShang Gao (Meibao) (Shantou Meibao Pharmaceutical Co., Ltd., Z20000004, specification: 40 g per tube), daily once for 10 d, or Qingshuanglu (no dressing or covering), three times for 10 d.
Outcome measurements:
The primary outcome was effectiveness of wound healing where 100 % wound healing without whole-body symptoms was deemed as cure; >90 % wound healing without whole-body symptoms was considered as excellent response while >50 % wound healing without whole-body symptoms as good response otherwise it is considered to have no response. While the secondary outcomes used the Visual Analogue Score (VAS) for assessing the degree of pain during wound dressing and Vancouver Scar Scale (VSS) scores for scar assessment after treatment. Further, pigmentation rate, wound drying time, healing time, and safety profile were also studied. VAS is an assessment tool that is employed to quantify pain, ranging from 1-10 in which higher number indicates greater severity. VSS is comprised of 4 domains including pliability, pigmentation, vascularity, and scar height, with the total score ranging from 0 to 15 where higher VSS score reflects a greater scar.
Enzyme-Linked Immunosorbent Assay (ELISA): The patients were requested to provide peripheral blood after overnight fasting at baseline before and after 10 d of treatment. The peripheral blood samples were then placed into pyrogen/endotoxin- free tubes, followed by centrifugation at 2000 ×g for 10 min, and then the serum was obtained. The serum samples were submitted to commercially available human ELISA kits for Tumor Necrosis Factor Alpha (TNF-α) (ab181421, Abcam) and Interleukin (IL)-6 (ab178013, Abcam). The serum samples were also allowed to measure the concentration of C-Reactive Protein (CRP) by turbidimetric method with automatic biochemical instruments.
Statistical analysis:
Continuous data was obtained using mean±Standard Deviation (SD). Difference for data at baseline to 10 d after treatment in the group was determined by using the paired t test. While, in the patients receiving Meibao and those receiving Qingshuanglu difference for data was estimated using the unpaired t test, which was completed in GraphPad Prism version 8.0 for Windows (GraphPad Software, San Diego, California, USA).
Results and Discussion
Baseline data of patients was studied. A total of 120 patients were consecutively recruited and randomized into Meibao treatment and Qingshuanglu exposure, 60 patients for each group. Among 60 patients who were scheduled to receive Qingshuanglu exposure, there were 36 males and 24 females, with a mean age of 43.77 y. Their burn injuries involved a flame (n=22), hot grease (n=28), and other reasons (n=10), with the burn area ranging from 5 % to 29 % and a mean of 17.03 %. Similarly, among 60 patients who were scheduled to receive Meibao treatment, there were 33 males and 27 females, with a mean age of 42.22 y. Their burn injuries involved a flame (n=23), hot grease (n=25), and other reasons (n=12), with the burn area ranging from 5 % to 29 % and a mean area of 16.53 %. Two randomized groups were compared for treatment outcomes and no significant difference was observed on their characteristics at baseline (p>0.05) (Table 1).
| Characteristics | Qingshuanglu | Meibao | p |
|---|---|---|---|
| Age (y) | 43.77±10.37 | 42.22±9.14 | 0.387 |
| Gender distribution (n/%) | 36 (60.00 %) | 33 (55.00 %) | 0.712 |
| Burn injury (n/%) | 0.83 | ||
| Flame | 22 (36.67 %) | 23 (38.33) | 0.475 |
| Hot grease | 28 (46.67 %) | 25 (41.67 %) | |
| Other reason | 10 (16.66 %) | 12 (20.00 %) | |
| Burn area (%) | 17.02±4.71 | 16.39±4.91 |
Table 1: Baseline Characteristics of Patients
Primary outcomes were evaluated. After 10 d Qingshuanglu exposure, cure was achieved in 28 patients, excellent response was achieved in 20 patients, good response was achieved in 10 patients and no response was observed in 2 patients. Similarly after 10 d Meibao treatment, cure was achieved in 24 patients, excellent response was achieved in 16 patients, good response was achieved in 10 patients, and no response was observed in 10 patients. The total response rates were 96.67 % and 83.33 % between patients receiving Qingshuanglu exposure and those receiving Meibao treatment, respectively (p=0.030) (Table 2).
| Treatment arm | Cure | Excellent response | Good response | No response | Total response rate |
|---|---|---|---|---|---|
| Qingshuanglu exposure | 28 | 20 | 10 | 2 | 58 (96.67 %) |
| Meibao treatment | 24 | 16 | 10 | 10 | 50 (83.33 %) |
Table 2: The Total Response Rates of Patients Receiving Either 10 d Qingshuanglu Exposure or Meibao Treatment
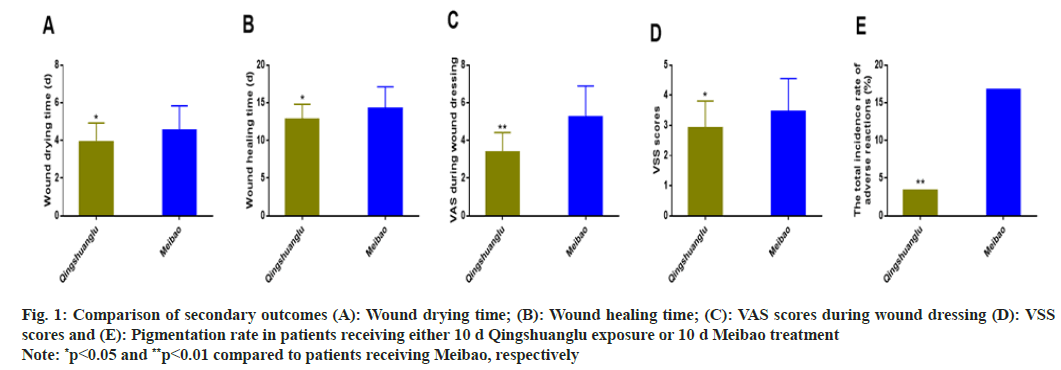
Similarly, secondary outcomes were also evaluated. The patients receiving 10 d Qingshuanglu exposure was observed with reduced wound drying time and healing time compared to those receiving 10 d Meibao treatment (p<0.05) (Table 3). The VAS scores, the summarized VSS scores, and the pigmentation rates were notably lower in the patients receiving 10 d Qingshuanglu exposure than those receiving 10 d Meibao treatment (p<0.05) (Table 3 and fig. 1).
| Secondary outcomes | Qingshuanglu | Meibao | p |
|---|---|---|---|
| Wound drying time (d) | 3.92±1.01 | 4.52±1.32 | 0.006 |
| Wound healing time (d) | 12.80±2.00 | 14.19±2.93 | 0.003 |
| VAS during wound dressing | 3.38±1.04 | 5.22±1.67 | <0.001 |
| VSS scores | 2.92±0.89 | 3.45±1.10 | 0.004 |
| Pigmentation rate (n/%) | 1 (1.67 %) | 8 (13.33 %) | 0.032 |
Table 3: Secondary Outcomes of Patients Receiving Either 10 d Qingshuanglu Exposure or 10 d Meibao Treatment
Fig. 1: Comparison of secondary outcomes (A): Wound drying time; (B): Wound healing time; (C): VAS scores during wound dressing (D): VSS scores and (E): Pigmentation rate in patients receiving either 10 d Qingshuanglu exposure or 10 d Meibao treatment
Note: *p<0.05 and **p<0.01 compared to patients receiving Meibao, respectively
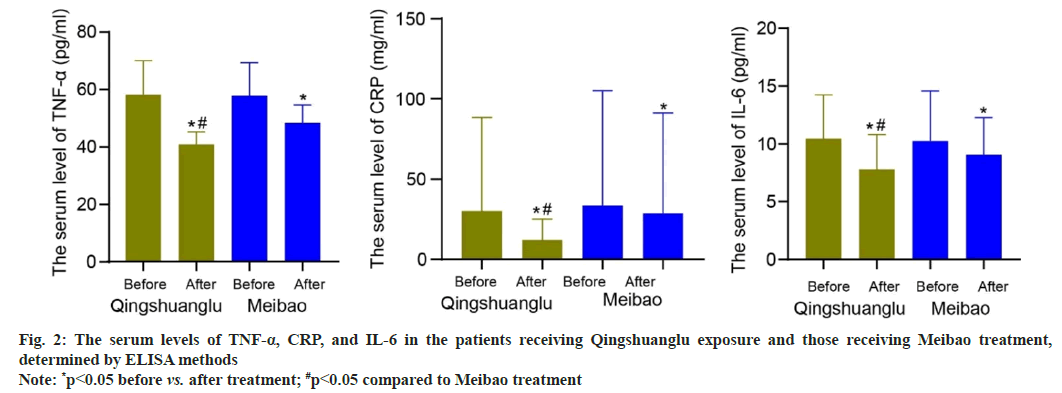
Further, production of pro-inflammatory factors was studied. The patients receiving Qingshuanglu exposure and those receiving Meibao treatment did not differ regarding the serum levels of TNF-α, CRP, and IL-6 at baseline (p>0.05). The mean serum levels of TNF-α, CRP, and IL-6 decreased from 58.04 pg/ml, 30.15 mg/l, and 10.46 pg/ml at baseline to 40.80 pg/ml, 12.03 mg/l, and 7.79 pg/ ml after 10 d Qingshuanglu exposure (p<0.05). The mean serum levels of TNF-α, CRP, and IL-6 reduced from 57.65 pg/ml, 33.62 mg/l, and 10.26 pg/ml at baseline to 48.24 pg/ml, 28.77 mg/l, and 9.06 pg/ml after 10 d Meibao treatment (p<0.05). More importantly, these reductions were greater in the patients receiving Qingshuanglu exposure than those receiving Meibao treatment (p<0.05) (fig. 2).
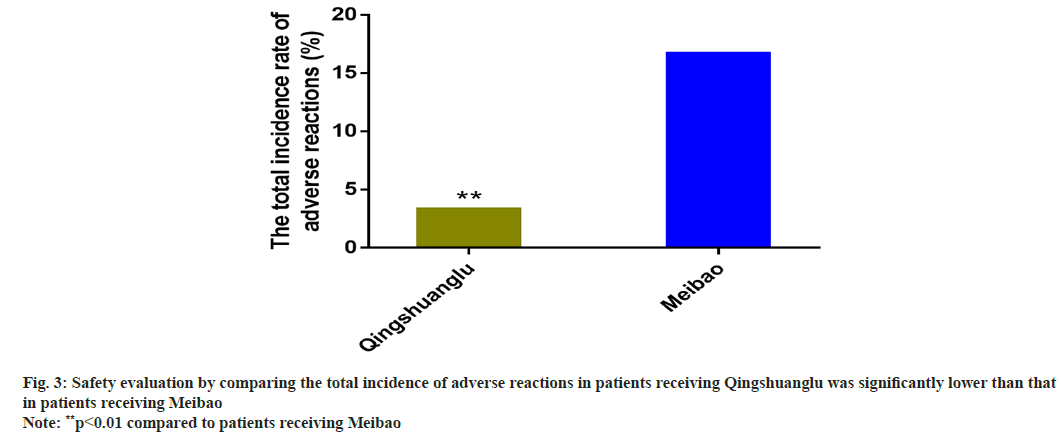
Safety evaluation was studied. After 10 d Qingshuanglu exposure, the infection occurred in one patient and pigmentation occurred in one patient. The total incidence rate of adverse reactions was 3.33 %. After 10 d Meibao treatment, infection occurred in one patient, pigmentation occurred in 8 patients, and neutrocytopenia occurred in one patient. The total incidence rate of adverse reactions was 16.67 %. The patients receiving Qingshuanglu exposure and those receiving Meibao treatment showed significant difference with regard to the total incidence rate of adverse reactions (p=0.030) (fig. 3).
Currently, burn patients often leave scars after treatment, which significantly affects the quality of life of patients. It is important to provide timely and effective treatment to improve the clinical symptoms of patients and reduce the scars formed after wound healing. The study demonstrated Qingshuanglu exposure could effectively repair burn injury, attenuate the inflammatory response, reduce the scar formation for burn patients.
Tissue damage caused by burn injury triggers increased release of numerous inflammatory mediators and vasoactive substances such as TNF-α, CRP, IL-6, and oxygen free radicals, which leads to an increased microcirculation permeability, with fluid extravasation from blood vessels into the tissue space, primarily manifested as local and generalized acute edema[9]. Acute edema exacerbates blood stasis, resulting in inadequate oxygen and nutrient supply, accumulation of metabolic waste products and inflammatory mediators, and finally causing severe impairment of wound healing[10,11].
Burn associated local and general tissue edema is induced by local cell destruction and capillary leak syndrome, which involves reduced capillary permeability with prevention of fluid extravasation from blood vessels[12,13]. Diosmin exerts a strong protective effect on blood vessels against vascular leakage and inflammation by increasing the elasticity of vessel walls and reducing the permeability of capillary walls, thereby producing an anti-edematous effect[14,15]. The clinical drug treatment for superficial and superficial partial-thickness burns is Meibao Shi Run Shao Shang Gao[16]. However, adverse reactions may occur after treatment, such as scar formation. Qingshuanglu is a medicinal liquid made from Taraxacum mongolicum, Myrica rubra root, Ilex pubescens, borneol, bear bile, Callicarpa macrophylla leaves, Cirisum arvense, and other traditional Chinese medicines through a specific process to dissolve its effective ingredients in ethanol, which has good therapeutic effects on various types of burn patients. Taraxacum mongolicum, Ilex pubescens, and Myrica rubra root have the capability of heat-clearing and detoxifying, eliminating carbuncle and dispersing swelling[17-19]. Borneol shows anti-inflammatory, detumescence, analgesic, and antiseptic effects[20]. Bear bile has antibacterial and anti-inflammatory effects[21]. Callicarpa macrophylla leaves have the effect of astringency, hemostasis, detoxification, and detumescence[22]. Cirisum arvense have the effect of cooling blood, stopping bleeding, promoting blood stasis, and reducing swelling[23]. Ethanol has certain physiological activities, which can promote blood circulation, dissipate blood stasis, promote qi, relieve pain, and relax muscles and activate collaterals. Accordingly, Qingshuanglu can promote tissue growth and repair, diminish inflammation and relieve pain, and effectively treat wound injuries. In this study, the total response rates were 96.67 % and 83.33 % between patients receiving Qingshuanglu exposure and those receiving Meibao treatment, respectively, showing significant difference.
Qingshuanglu can form a protection between the exudates and the body, maintain a stable wound environment, accelerate the drying of the wound surface and effectively reduce the further damage caused by external harmful substances to the wound surface. Through the pharmacological effects of its various components, it can alleviate the spasm of the hair follicle, improve microcirculation, and improve vascular permeability thereby playing an effective analgesic role. At the same time, it can effectively alleviate inflammatory reactions, promote granulation tissue proliferation, accelerate wound healing, and improve the wound healing rate through the functions of Qingshuanglu in promoting blood circulation and resolving stasis, clearing heat and detoxifying, and removing putrefaction and generating muscle[24]. On the other hand, exposure therapy enhances the anti-inflammatory and sedative effects of Qingshuanglu, dispels blood stasis, and promotes regeneration, effectively preventing infection on the wound surface, reducing blood stasis, and promoting the growth of epithelial tissue, thereby further improving the treatment effect and reducing the occurrence of scars and pigmentation[25]. The patients receiving 10 d Qingshuanglu exposure was demonstrated with reduced wound drying and healing time compared to those receiving 10 d Meibao treatment.
In conclusion, Qingshuanglu exposure combined with oral treatment of diosmin can could effectively repair burn injury, attenuate the inflammatory response, reduce the scar formation for burn patients, showing high safety profiles, which is worthy to further promote in the clinical practice. However, due to the limitations of this study, such as a small sample size and short study time, it is recommended to increase the sample size and extend the study time in future clinical studies to further investigate effects of Qingshuanglu exposure therapy on scar improvement, hemostasis, and analgesia.
Funding:
The study was supported by Fujian Provincial Department of Science and Technology University Production and Learning Cooperation Project (No. 2021Y4014).
Conflict of interests:
The authors declared no conflict of interest.
References
- Spronk I, Legemate C, Oen I, van Loey N, Polinder S, van Baar M. Health related quality of life in adults after burn injuries: A systematic review. PloS One 2018;13(5):1-21.
[Crossref] [Google Scholar] [PubMed]
- Rex S. Burn injuries. Curr Opin Crit Care 2012;18(6):671-6.
[Crossref] [Google Scholar] [PubMed]
- Jeschke MG, van Baar ME, Choudhry MA, Chung KK, Gibran NS, Logsetty S. Burn injury. Nat Rev Dis Primers 2020;6(1):11.
[Crossref] [Google Scholar] [PubMed]
- Nielson CB, Duethman NC, Howard JM, Moncure M, Wood JG. Burns: Pathophysiology of systemic complications and current management. J Burn Care Res 2017;38(1):e469-81.
[Crossref] [Google Scholar] [PubMed]
- Young AW, Dewey WS, King BT. Rehabilitation of burn injuries: An update. Phys Med Rehabil Clin N Am 2019;30(1):111-32.
[Crossref] [Google Scholar] [PubMed]
- Chi J, Sun L, Cai L, Fan L, Shao C, Shang L, et al. Chinese herb microneedle patch for wound healing. Bioact Mater 2021;6(10):3507-14.
[Crossref] [Google Scholar] [PubMed]
- Li FL, Wang GC, Wu BQ. Clinical application of traditional Chinese medicine powder in the treatment of acute and chronic wounds. Int Wound J 2023;20(3):799-805.
[Crossref] [Google Scholar] [PubMed]
- Huwait E, Mobashir M. Potential and therapeutic roles of diosmin in human diseases. Biomedicines 2022;10(5):1076.
[Crossref] [Google Scholar] [PubMed]
- Edgar DW, Fish JS, Gomez M, Wood FM. Local and systemic treatments for acute edema after burn injury: A systematic review of the literature. J Burn Care Res 2011;32(2):334-47.
[Crossref] [Google Scholar] [PubMed]
- Hellenthal KE, Brabenec L, Wagner NM. Regulation and dysregulation of endothelial permeability during systemic inflammation. Cells 2022;11(12):1935.
[Crossref] [Google Scholar] [PubMed]
- Chi Y, Liu X, Chai J. A narrative review of changes in microvascular permeability after burn. Ann Transl Med 2021;9(8).
[Crossref] [Google Scholar] [PubMed]
- Cancio JM, Dewey WS. Critical care rehabilitation of the burn patient. Surg Clin North Am 2023;103(3):483-94.
[Crossref] [Google Scholar] [PubMed]
- Zdolsek M, Hahn RG, Sjöberg F, Zdolsek JH. Plasma volume expansion and capillary leakage of 20 % albumin in burned patients and volunteers. Crit Care 2020;24:1-9.
[Crossref] [Google Scholar] [PubMed]
- Zou J, Yuan D, Yang J, Yu Y. Effects of diosmin on vascular leakage and inflammation in a mouse model of venous obstruction. Front Nutr 2022;9:1-9.
[Crossref] [Google Scholar] [PubMed]
- Feldo M, Wójciak M, Ziemlewska A, Dresler S, Sowa I. Modulatory effect of diosmin and diosmetin on metalloproteinase activity and inflammatory mediators in human skin fibroblasts treated with lipopolysaccharide. Molecules 2022;27(13):1-13.
[Crossref] [Google Scholar] [PubMed]
- Baroni A, Ruocco E, Russo T, Piccolo V, Geng L, Zhou H, et al. The use of traditional Chinese medicine in some dermatologic diseases: Part II-autoimmune bullous disorders and lichen planus. Skinmed 2015;13(3):195-203.
[Google Scholar] [PubMed]
- Yang N, Li C, Tian G, Zhu M, Bu W, Chen J, et al. Organic acid component from Taraxacum mongolicum Hand.-Mazz alleviates inflammatory injury in lipopolysaccharide-induced acute tracheobronchitis of ICR mice through TLR4/NF-κB signaling pathway. Int Immunopharmacol 2016;34:92-100.
[Crossref] [Google Scholar] [PubMed]
- Jiang S, Cui H, Wu P, Liu Z, Zhao Z. Botany, traditional uses, phytochemistry, pharmacology and toxicology of Ilex pubescens Hook et Arn. J Ethnopharmacol 2019;245:1-17.
[Crossref] [Google Scholar] [PubMed]
- Li G, Wang D, Xu S. Two new compounds from the roots of Myrica rubra. Nat Prod Res 2011;25(2):136-40.
[Crossref] [Google Scholar] [PubMed]
- Mei Y, Li L, Fan L, Fan W, Liu L, Zhang F, et al. The history, stereochemistry, ethnopharmacology and quality assessment of borneol. J Ethnopharmacol 2023;300:115697.
[Crossref] [Google Scholar] [PubMed]
- Kalogeropoulu SK, Lloyd EJ, Rauch H, Redtenbacher I, Häfner M, Burgener IA, et al. Chronic cholecystitis: Diagnostic and therapeutic insights from formerly bile-farmed Asiatic black bears (Ursus thibetanus). Plos One 2022;17(3):1-15.
[Crossref] [Google Scholar] [PubMed]
- Xu J, Sun Y, Wang M, Ren Q, Li S, Wang H, et al. Bioactive diterpenoids from the leaves of Callicarpa macrophylla. J Nat Prod 2015;78(7):1563-9.
[Crossref] [Google Scholar] [PubMed]
- Luo W, Wu B, Tang L, Li G, Chen H, Yin X. Recent research progress of Cirsium medicinal plants in China. J Ethnopharmacol 2021;280:114475.
[Crossref] [Google Scholar] [PubMed]
- Firat C, Samdanc? E, Erbatur S, Aytekin AH, Ak M, Turtay MG, et al. β-Glucan treatment prevents progressive burn ischaemia in the zone of stasis and improves burn healing: An experimental study in rats. Burns 2013;39(1):105-12.
[Crossref] [Google Scholar] [PubMed]
- Dallal MS, Safdari R, Koochak HE, Sharifi-Yazdi S, Akhoondinasab MR, Pourmand MR, et al. A comparison between occlusive and exposure dressing in the management of burn wound. Burns 2016;42(3):578-82.
[Crossref] [Google Scholar] [PubMed]