- *Corresponding Author:
- Ying Zhang
Department of Anesthesiology, The Second Hospital of Tangshan, Tangshan, Hebei Province 063000, China
E-mail: zy15230535099@126.com
| This article was originally published in a special issue, “Role of Biomedicine in Pharmaceutical Sciences” |
| Indian J Pharm Sci 2023:85(2) Spl Issue “203-208” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
compromising early postoperative recovery. Previous studies have reported favorable results using anterior, posterior and lateral quadratus lumborum block for pain control during hip surgery. In this study, we evaluate the effectiveness of ultrasound-guided quadratus lumborum block in postoperative analgesia of total hip replacement. 200 patients who underwent total hip arthroplasty in our hospital between January 2020 and January 2021 were recruited and assigned via random number table method to receive either ultrasoundguided quadratus lumborum block (study group) or fascia iliaca block (observation group) for anesthesia. All patients were given self-administered intravenous analgesia postoperatively. Outcome measures included cumulative postoperative sufentanil use, resting pain, motor pain, postoperative hip mobility and incidence of nausea and vomiting. Ultrasound-guided quadratus lumborum block resulted in significantly less sufentanil use in patients at 24 h and 48 h postoperatively (52.14±5.11, 105.74±8.14) vs. fascia iliaca block (77.58±7.93, 150.18±10.58) (p<0.05). Patients in the study group showed lower visual analogue scale scores both at rest and at exercise than those in the observation group at 12, 24 and 48 h postoperatively (p<0.05). The study group had significantly greater maximum hip flexion and abduction mobility at 24 h and 48 h postoperatively than the observation group (p<0.05). Ultrasound-guided quadratus lumborum block was associated with a lower incidence of nausea and vomiting (7.00 %) vs. fascia iliaca block (39.00 %) (p<0.05). Ultrasoundguided quadratus lumborum block reduces the use of opioids in total hip replacement patients, significantly alleviates surgical pain, promotes early functional recovery and lowers the incidence of adverse effects.
Keywords
Ultrasound, quadratus lumborum block, hip joint, analgesia, fracture
Total hip arthroplasty is a common procedure for the treatment of severe hip disease and reconstruction of joint function[1,2]. However, the severe postoperative pain seriously compromises postoperative recovery, which underlines the significance of preoperative and postoperative analgesia for hip fracture[3]. The PROSPECT 2010 guidelines recommend various methods to minimize perioperative pain during total hip arthroplasty in elderly patients, such as intravenous analgesia, epidural analgesia, local anesthetic infiltration techniques and peripheral nerve blocks. Nevertheless, due to the complex innervation of the hip, there is a critical need for a new approach to block the surgical area of the hip while preserving muscle motility.
Existing analgesic modalities for hip fractures rely on ultrasound-guided nerve block techniques as well as intravenous and oral analgesics[4]. Currently, peripheral nerve block is a key component of perioperative multimodal analgesia that provides site-specific and fast-acting analgesia[5]. Quadratus Lumborum Block (QLB) is new multimodal analgesia with established postoperative analgesic effects in abdominal surgery in recent years[6,7]. Since the muscles and skin sensation involved in total hip arthroplasty are innervated by branches of the superior knee nerve, the inferior costal nerve, the inferior ilioinguinal nerve, the ilioinguinal nerve, the femoral nerve, the foramen ovale nerve, the sciatic nerve and the lateral femoral cutaneous nerve, which accounts for the difficulty of QLB to meet the anesthetic needs in total hip arthroplasty[8,9]. Furthermore, the effectiveness of QLB in hip arthroplasty has been marginally explored.
To this end, this study was conducted to evaluate the effectiveness of ultrasound-guided QLB in postoperative analgesia of total hip replacement and to explore a more appropriate analgesic solution for better rehabilitation surgery.
Materials and Methods
General information:
In this retrospective study, 200 patients (127 males and 73 females, aged under 80 y) who underwent total hip arthroplasty in our hospital between January 2020 and January 2021 were recruited and assigned via random number table method to receive either ultrasound-guided QLB (study group) or fascia, all patients received self-administered intravenous analgesia postoperatively. Patients provided written informed consent and the study was approved by the ethics committee of our hospital.
Inclusion and exclusion criteria:
Inclusion criteria: Patients who underwent primary unilateral hip arthroplasty, regardless of gender; with American Society of Anesthesiologists (ASA) classification of II-III and, with complete clinical data and no hospital referral.
Exclusion criteria: With morbid obesity, i.e., Body Mass Index (BMI) >35 kg/m2; with hypersensitivity to study-related drugs or severe coagulation disorders; with chronic pain, long-term use of analgesics or other psychotropic drugs and with puncture site infection.
Methods:
Preoperative preparation: All patients fasted for (6- 8) h before surgery and no preoperative medication was administered. After entering the operating room, peripheral venous access was established and the Electrocardiogram (ECG), invasive arterial blood pressure and pulse oximetry of the patients were monitored using an ultrasound machine (diagnostic ultrasound system, model Wisonic Navis, Shenzhen Wisonic Medical Technology Co). The depth of anesthesia was controlled with an Electroencephalography (EEG) Bispectral Index (BIS) monitor. Mask oxygenation and invasive arterial monitoring were performed under local anesthesia. All patients received intravenous inhalation compound general anesthesia.
Nerve block: In the study group, nerve blocks were performed under ultrasound guidance after hip arthroplasty. With the patients in a lateral position, after routine disinfection, the nerve block was performed using a short 20 G beveled needle (10 cm, Braun, Germany) under the guidance of the Terason T3000 portable ultrasound device (Terason, United States of America (USA)). The ultrasound probe was first placed along the mid-axillary line between the iliac crest and the edge of the costal arch, and then slowly moved dorsally. Under the short-axis plane method, the puncture needle was inserted between the lumbar square and lumbar major muscles (at the level of lumbar 4/5), 1-2 ml of saline was injected to determine the tip position and then 30 ml of ropivacaine at a concentration of 0.375 % was injected[10,11].
Patients in the observation group were placed in the supine position with the high-frequency linear transducer placed parallel to the inguinal region. The femoral artery was first located and then moved laterally to locate the femoral nerve, broad fascial tensor, suture muscle, iliac spine and iliac fascia. 30 ml of ropivacaine at a concentration of 0.375 % was injected into the iliac fascia gap. 13 min after the block, the effect of the block was assessed by one investigator using pinprick sensation in each cortical distribution of the closed foraminal nerve, lateral femoral cutaneous nerve and femoral nerve.
Anesthesia method: With the patient in the supine position, a subarachnoid puncture was performed at L4 and L5 after sterilization. After the presence of cerebrospinal fluid reflux, 2 ml of bupivacaine at a concentration of 5 % was injected. Midazolam and sufentanil were used intraoperative as adjunctive analgesic sedatives and 4.5 mg of tropisetron was used to prevent nausea and vomiting. Patient- controlled analgesia was administered in all patients (150 μg of sufentanil, 8.96 mg of tropisetron and saline supplementation to 300 ml, background dose of 4 ml/h, a self-controlled dose of 4 ml, lock time of 20 min, maximum dose of 20 ml/h).
Observation indicators:
Postoperative analgesia included oral non-steroidal anti-inflammatory drugs, patient-controlled intravenous analgesia and rescue analgesia. Self- controlled intravenous analgesia consisted of 100 μg sufentanil and 8 mg of tropisetron, diluted to 100 ml with saline, delivered in 2 ml per dose, with a lock time of 15 min and background-free infusion.
The doses of sufentanil at 24 h and 48 h postoperatively were compared between the two groups of patients. Pain at rest and during exercise was assessed at different time points (6 h, 12 h, 24 h and 48 h) after surgery in both groups using a Visual Analogue Scale (VAS) (total score of 10 points; the score is proportional to pain). Maximum hip flexion and abduction mobility were measured in all patients at 24 h and 48 h postoperatively. The occurrence of nausea and vomiting was recorded for all patients.
Statistical data:
GraphPad Prism 8 was used for image processing and Statistical Package for the Social Sciences (SPSS) 26.0 software was used to organize and statistically analyze the data. The measurement data were expressed by (x̄ ±s) and a t-test was used for analysis. Count data were expressed as rate (%) and analyzed using the Chi-square (χ2) test. p<0.05 indicates that the difference is statistically significant.
Results and Discussion
The observation group had 62 male and 38 female cases, aged 55-78 y (65.84±6.37) y, with a height of 163.83±7.14 cm, weight of 69.38±15.98 kg, BMI of 23.21±2.78 kg/m2, ASA classification grade II in 44 cases and grade III in 56 cases, operative time of 80.98±19.78 min, preoperative resting VAS score of 4.12±0.58 and preoperative exercise VAS score of 8.02±0.87.
The study group had 65 males and 35 females, aged 58-77 y (65.53±6.48) y, with a height of 163.25±7.36 cm, weight of 69.11±16.08 kg, BMI of 23.04±2.93 kg/m2, ASA classification grade II in 41 cases and grade III in 59 cases, operative time of 81.23±19.65 min, preoperative resting VAS score of 4.21±0.47 and preoperative exercise VAS score of 8.04±0.79. The patient characteristics between the two groups were comparable (p>0.05) as shown in Table 1.
| Observation group (n=100) | Study group (n=100) | t | p | ||
|---|---|---|---|---|---|
| Gender | Male | 62 (62.00) | 65 (65.00) | ||
| Women | 38 (38.00) | 35 (35.00) | |||
| Age (years) | 55-78 (65.84±6.37) | 58-77 (65.53±6.48) | 0.341 | 0.733 | |
| Height (cm) | 163.83±7.14 | 163.25±7.36 | 0.566 | 0.572 | |
| Body weight (kg) | 69.38±15.98 | 69.11±16.08 | 0.119 | 0.905 | |
| BMI (kg/m2) | 23.21±2.78 | 23.04±2.93 | 0.421 | 0.674 | |
| ASA grade II | 44 (44.00) | 41 (41.00) | |||
| Grading grade III | 56 (56.00) | 59 (59.00) | |||
| Surgery time (min) | 80.98±19.78 | 81.23±19.65 | 0.090 | 0.928 | |
| Preoperative resting VAS score | 4.12±0.58 | 4.21±0.47 | 1.206 | 0.229 | |
| Preoperative exercise VAS score | 8.02±0.87 | 8.04±0.79 | 0.17 | 0.865 | |
Table 1: Patient Characteristics (x͞±s)
Ultrasound-guided QLB resulted in significantly less sufentanil use in patients at 24 h and 48 h postoperatively (52.14±5.11, 105.74±8.14) vs. fascia iliaca block (77.58±7.93, 150.18±10.58) (p<0.05) as shown in Table 2.
| Group | n | 24 h (μg) | 48 h (μg) |
|---|---|---|---|
| Observation | 100 | 77.58±7.93 | 150.18±10.58 |
| Study | 100 | 52.14±5.11 | 105.74±8.14 |
| t | 26.967 | 33.291 | |
| p | <0.001 | <0.001 |
Table 2: Sufentanil Dosage (x͞±s)
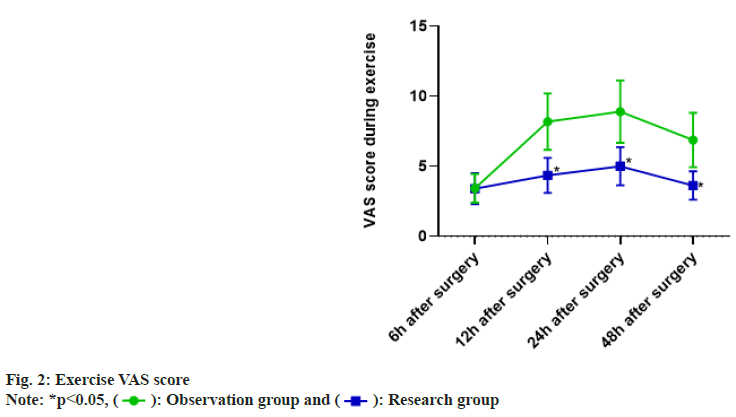
The patients in the observation group had resting VAS scores of (1.51±0.21) at 6 h postoperatively, (1.80±0.35) at 12 h postoperatively, (2.61±0.48) at 24 h postoperatively and (2.42±0.45) at 48 h postoperatively. The resting VAS scores of patients in the study group were (1.53±0.22) at 6 h postoperatively, (1.78±0.41) at 12 h postoperatively, (2.11±0.23) at 24 h postoperatively and (1.91±0.33) at 48 h postoperatively. The difference in pain at rest between the two groups at 6 h and 12 h postoperatively was not significant (p>0.05) and the VAS scores at rest in the study group were lower than those in the observation group at 24 h and 48 h postoperatively (p<0.05) as shown in fig. 1.
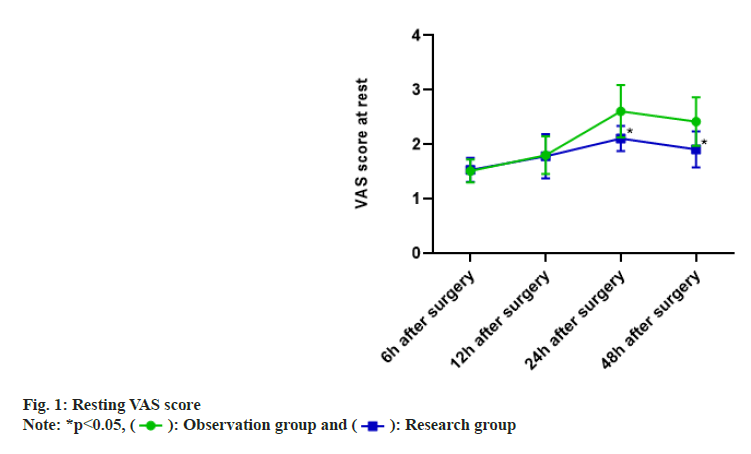
The motor VAS scores of patients in the observation group were (3.42±1.02) at 6 h postoperatively, (8.18±2.01) at 12 h postoperatively, (8.89±2.23) at 24 h postoperatively and (6.87±1.94) at 48 h postoperatively. Patients in the study group had (3.39±1.11) at 6 h postoperatively, (4.35±1.25) at 12 h postoperatively, (4.99±1.37) at 24 h postoperatively and (3.62±1.01) at 48 h postoperatively. The difference in pain during exercise was not significant between the two groups at 6 h postoperatively (p>0.05) and the VAS scores during exercise were lower in the study group than in the observation group at 12 h, 24 h and 48 h postoperatively (p<0.05) as shown in fig. 2.
The study group had significantly greater maximum hip flexion and abduction mobility at 24 h and 48 h postoperatively (68.88±10.45, 77.15±12.95, 25.98±4.45 and 28.47±5.89) than the observation group (55.41±10.84, 64.54±12.45, 19.65±3.44 and 22.41±4.41) (p<0.05) as shown in Table 3. Ultrasound-guided QLB was associated with a lower incidence of nausea and vomiting (7 %) vs. fascia iliaca block (39 %) (p<0.05) as shown in Table 4.
| Group | n | Maximum hip flexion (°) | Outreach activity (°) | ||
|---|---|---|---|---|---|
| 24 h after surgery | 48 h after surgery | 24 h after surgery | 48 h postoperative | ||
| Observation | 100 | 55.41±10.84 | 64.54±12.45 | 19.65±3.44 | 22.41±4.41 |
| Study | 100 | 68.88±10.45 | 77.15±12.95 | 25.98±4.45 | 28.47±5.89 |
| t | 8.946 | 7.02 | 11.254 | 8.236 | |
| p | <0.001 | <0.001 | <0.001 | <0.001 | |
Table 3: Postoperative HIP Mobility (x͞±s)
| Group | n | Number of cases of nausea and vomiting | Incidence |
|---|---|---|---|
| Observation | 100 | 39 | 39.00 |
| Study | 100 | 7 | 7.00 % |
| t | 28.910 | ||
| p | <0.001 |
Table 4: Incidence of Nausea and Vomiting (%)
The anterior segment of the hip capsule is innervated by the femoral and foraminal nerves, and the posterior segment is innervated by the femoral square muscle nerve and occasionally by the superior gluteal nerve (poster-lateral region) and sciatic nerve (poster superior region). Intravenous sufentanil analgesia is a common clinical analgesic method for hip replacement surgery, but it is predisposed to various adverse effects such as nausea and vomiting, and respiratory depression. It was found that regional block anesthesia is effective in analgesia with fewer adverse effects[12]. One of the regional anesthetic options for hip surgery is iliac fascia compartment block, which acts on the nerve-femoral nerve, closed foraminal nerve and lateral femoral cutaneous nerve. QLB is a posterior abdominal wall block performed entirely under ultrasound guidance[13]. Recent findings suggest that the branches of the femoral nerve innervating the hip are located deep and that the lateral femoral cutaneous nerve has significant anatomical variability in its location under the inguinal ligament[14]. Therefore, traditional analgesic modalities are considered insufficient to meet the analgesic needs of patients[15,16].
Conventional analgesia is usually injected at the level of lumbar 2-4, with the blocking range covering chest 4-lumbar 1. In the present study, the injection location was shifted to the level of lumbar 4/5 (low QLB). Results of prior studies showed that the blocking range of this approach could reach the level of thorax 8-waist 2/3, theoretically fulfilling the analgesic needs of hip surgery. Moreover, QLB shows no implications for postoperative hip movement. Experimental studies have shown that ultrasound- guided QLB could significantly reduce postoperative sufentanil dosage, decrease pain scores and improve the quality of early recovery without increasing complications.
In the present study, ultrasound-guided QLB resulted in significantly less sufentanil use in patients at 24 h and 48 h postoperatively vs. fascia iliaca block; patients in the study group showed lower VAS scores both at rest and at exercise than those in the observation group at 12, 24 and 48 h postoperatively. QLB extends the anesthetic effects through the thoracolumbar fascia to the paravertebral space, effectively blocking partial sympathetic nerve, promoting the establishment of collateral circulation, increasing blood supply and reducing the level of inflammatory mediators, thus relieving pain[17,18]. The results of this study showed that the study group had significantly greater maximum hip flexion and abduction mobility at 24 h and 48 h postoperatively than the observation group. Ultrasound-guided QLB was associated with a lower incidence of nausea and vomiting vs. fascia iliaca block, suggesting that patients in the study group had better pain relief, lower opioid requirements and enhanced quality of recovery. The lower drug requirement was attributable to the potentiated analgesic effect of QLB, which provides pain relief in the incisional area for patients undergoing total hip arthroplasty primarily by blocking the thoracic 10-lumbar 3 nerve region and skin tissue[19]. The QLB provides pain relief in the incision area for patients undergoing total hip arthroplasty primarily by blocking the thoracic 10-lumbar 3 nerve region and skin tissue. In addition, all anesthetic blocks were performed before induction of anesthesia, which facilitates the correct deposition of local anesthetic and thus increases the success rate of the block. Besides, the risk of unrecognized vascular bleeding and nerve injury is reduced due to the shallow injection site of the needle[20]. Kadane et al. found that QLB reduced pain scores and the need for analgesic medication at 24 h postoperatively, which is consistent with the results of the current study.
The present study has the following limitations; due to the absence of objective indicators to quantify the effect of nerve block on muscle strength and the potential implications for motor function by severe postoperative pain, medically induced nerve injury and transient nerve palsy, subjective issues that compromise the reliability of the results of the current study exist and the postoperative decrease in motor function is not entirely ascribed to nerve block. In addition, the current study lacks parameters such as time lapses before first out-of-bed activity, length of stay and patient satisfaction, which will be further, investigated in future studies.
Ultrasound-guided QLB reduces the use of opioids in total hip replacement patients, significantly alleviates surgical pain, promotes early ultrasound- guided QLB reduces the use of opioids in total hip replacement patients, significantly alleviates surgical pain, promotes early functional recovery and lowers the incidence of adverse effects.
Conflict of interests:
The authors declared no conflict of interests.
References
- Petis S, Howard JL, Lanting BL, Vasarhelyi EM. Surgical approach in primary total hip arthroplasty: Anatomy, technique and clinical outcomes. Can J Sur 2015;58(2):128-39.
[Crossref] [Google Scholar] [PubMed]
- Slavković N, Vukašinović Z, Baščarević Z, Vukomanović B. Total hip arthroplasty. Srp Arh Celok Lek 2012;140(5-6):379-84.
- Talia AJ, Coetzee C, Tirosh O, Tran P. Comparison of outcome measures and complication rates following three different approaches for primary total hip arthroplasty: A pragmatic randomised controlled trial. Trials 2018;19(1):13.
[Crossref] [Google Scholar] [PubMed]
- Korgvee A, Junttila E, Koskinen H, Huhtala H, Kalliomaki ML. Ultrasound-guided quadratus lumborum block for postoperative analgesia: A systematic review and meta-analysis. Eur J Anaesthesiol 2021;38(2):115-29.
[Crossref] [Google Scholar] [PubMed]
- He J, Zheng XQ, Luo CH, Huang ZX, He WY, Wang HB, et al. Effects and safety of quadratus lumborum block in analgesia after hip arthroplasty. Zhonghua Yi Xue Za Zhi 2018;98(8):565-9.
[Crossref] [Google Scholar] [PubMed]
- Li J, Wei C, Huang J, Li Y, Liu H, Liu J, et al. Efficacy of quadratus lumborum block for pain control in patients undergoing hip surgeries: A systematic review and meta-analysis. Front Med 2022;8:3030.
[Crossref] [Google Scholar] [PubMed]
- Xia Q, Ding W, Lin C, Xia J, Xu Y, Jia M. Postoperative pain treatment with transmuscular quadratus lumborum block and fascia iliaca compartment block in patients undergoing total hip arthroplasty: A randomized controlled trial. BMC Anesthesiol 2021;21(1):188.
[Crossref] [Google Scholar] [PubMed]
- Plečko M, Bohaček I, Tripković B, Čimić M, Jelić M, Delimar D. Applications and critical evaluation of fascia iliaca compartment block and quadratus lumborum block for orthopedic procedures. Acta Clin Croat 2019;58(1):108-13.
[Crossref] [Google Scholar] [PubMed]
- Kayani B, Konan S, Chandramohan R, Haddad FS. The direct superior approach in total hip arthroplasty. Br J Hosp Med 2019;80(6):320-4.
- Ueshima H, Otake H, Lin JA. Ultrasound-guided quadratus lumborum block: An updated review of anatomy and techniques. Biomed Res Int 2017;2017:2752876.
[Crossref] [Google Scholar] [PubMed]
- Brixel SM, Biboulet P, Swisser F, Choquet O, Aarab Y, Nguyen H, et al. Posterior quadratus lumborum block in total hip arthroplasty: A randomized controlled trial. Anesthesiology 2021;134(5):722-33.
[Crossref] [Google Scholar] [PubMed]
- Li J, Tang S, Lam D, Hergrueter A, Dennis J, Liu H. Novel utilization of fascial layer blocks in hip and knee procedures. Best Pract Res Clin Anaesthesiol 2019;33(4):539-51.
[Crossref] [Google Scholar] [PubMed]
- Li J, Dai F, Schonberger RB. Transmuscular quadratus lumborum block in total hip replacement: A response. Clin J Pain 2021;37(12):940-1.
[Crossref] [Google Scholar] [PubMed]
- Steingrimsdottir G, Hansen CK, Dam M, Tanggaard KB, Nielsen MV, Børglum J. Quadratus lumborum block for total hip arthroplasty: Anatomical knowledge is always key for choice of blocks and execution. Reg Anesth Pain Med 2021;46(1):92-3.
[Crossref] [Google Scholar] [PubMed]
- Wang Q, Hu J, Zhang W, Zeng Y, Yang J, Kang P. Comparison between ultrasound-guided suprainguinal fascia iliaca block and anterior quadratus lumborum block for total hip arthroplasty: A prospective, double-blind, randomized controlled trial. J Arthroplasty 2022;37(4):763-9.
[Crossref] [Google Scholar] [PubMed]
- Elsharkawy H, El-Boghdadly K, Barrington M. Quadratus lumborum block: Anatomical concepts, mechanisms and techniques. Anesthesiology 2019;130(2):322-35.
[Crossref] [Google Scholar] [PubMed]
- Hu J, Xu M, Wang Q, Yang J. Quadratus lumborum block in total hip replacement: Comment. Anesthesiology 2021;135(5):927.
[Crossref] [Google Scholar] [PubMed]
- Haskins SC, Tseng A, Zhong H, Mamic M, Cheng SI, Nejim JA, et al. Anterior quadratus lumborum block does not provide superior pain control after hip arthroscopy: A double-blinded randomized controlled trial. Anesthesiology 2021;135(3):433-41.
[Crossref] [Google Scholar] [PubMed]
- Gonçalves J, Almeida CR, Cunha F, Pinto M. Quadratus lumborum block for acute visceral pain. Anaesth Crit Care Pain Med 2021;40(2):100811.
[Crossref] [Google Scholar] [PubMed]
- Nassar H, Hasanin A, Sewilam M, Ahmed H, Abo-Elsoud M, Taalab O, et al. Transmuscular quadratus lumborum block vs. suprainguinal fascia iliaca block for hip arthroplasty: A randomized, controlled pilot study. Local Reg Anesth 2021:67-74.
[Crossref] [Google Scholar] [PubMed]
 Observation group and
Observation group and  Research group
Research group