- *Corresponding Author:
- Xi Jin
Department of Neurology, Changchun University of Traditional Chinese Medicine Affiliated to Third Clinical Hospital, Changchun, Jilin, China
E-mail: jizhan67631@163.com
| This article was originally published in a special issue,“Transformative Discoveries in Biomedical and Pharmaceutical Research” |
| Indian J Pharm Sci 2023:85(4) Spl Issue “246-256” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Post-stroke sleep disorder is one of the most common post-stroke complications in patients with stroke. The purpose of this study is to summarize and evaluate the evidence for the effectiveness of acupuncture therapy for post-stroke sleep disorder and provide a factual basis for future clinical decisions. As of August 9, 2022, we searched six databases with a total of 138 documents, and the retrieved literature was thoroughly evaluated according to the inclusion and exclusion criteria developed, and valid data from them were extracted and included in the analysis. We evaluated the effectiveness of acupuncture therapy in the treatment of poststroke sleep disorder patients using clinical efficiency rate and the Pittsburgh sleep quality index as outcome indicators. Finally, 18 randomized controlled trials met our inclusion criteria. Meta-analysis showed that the clinical efficiency rate of acupuncture therapy for post-stroke sleep disorder was statistically significant compared with that of the control group (relative risk=1.20, 95 % confidence interval (1.15, 1.25), p<0.00001); the Pittsburgh sleep quality index scores of patients with post-stroke sleep disorder treated with acupuncture therapy were statistically significant compared with that of the control group (relative risk=-1.06, 95 % confidence interval (-1.38, -0.75), p<0.00001). In conclusion, acupuncture therapy is clinically significant in the treatment of post-stroke sleep disorder. Although acupuncture has shown good efficacy in the treatment of post-stroke sleep disorder, further studies are needed to confirm the role of acupuncture in the treatment of such disorders.
Keywords
Acupuncture therapy, insomnia, stroke, meta-analysis, hypoxia
Stroke is an acute cerebrovascular disease, also known as "stroke" and "cerebrovascular accident", which is a general term for a series of clinical syndromes such as monoplegia and blindness due to sudden rupture and bleeding or blockage of cerebral blood vessels, resulting in ischemia and hypoxia in brain tissue[1]. Stroke has become one of the major killers threatening human health worldwide, with its incidence increasing year by year and trending younger, making it the second leading cause of death. Stroke can affect 13.7 million people worldwide each year and can cause 5.5 million deaths, including 2.7 million deaths due to ischemic stroke in 2017 alone[2]. There are many risk factors for stroke, including smoking, alcohol consumption, hypertension, diabetes, heart disease, and low frequency of physical activity, while sudden increases in social stress and depressed emotional states are also possible causes of stroke[3]. The mortality rate of stroke is currently decreasing year by year with the development of medical technology, but the aging process of society is increasing its incidence year by year, which aggravates the burden of social medical resources[4]. The onset of stroke is often accompanied by a variety of physical and mental dysfunction, which is not only a blow to the patient's emotions and will, but also a heavy burden on the patient's family and their social network. Early detection and timely intervention of possible post-stroke complications, so as to maintain the quality of life of the patient before the disease is one of our most important concerns, and is also a concentrated expression of medical humanistic care and medical temperature.
There are many complications of stroke, including infection, pain, paralysis, decubitus ulcers, depression, deep vein thrombosis, pulmonary embolism, angina pectoris, heart failure, myocardial infarction, dysphagia, incontinence, and gastrointestinal bleeding[5]. As one of the most common post-stroke complications, Post-Stroke Sleep Disorder (PSSD) is characterized by reduced sleep duration and difficulty in sleep maintenance[6], which has a negative impact on patients' mental health, physical rehabilitation and quality of life. Long-term sleep deprivation can also greatly affect the endocrine status of the patient, causing metabolic disorders in the patient's body and increasing the risk of coronary heart disease, diabetes, hypertension and other diseases[7]. The main clinical treatment for PSSD is currently pharmacological, usually with sedative-hypnotics or antidepressants, such as benzodiazepines and selective 5-Hydroxytryptamine (5-HT) reuptake inhibitors. However, the addiction, dependence, tolerance and adverse effects of these drugs limit their scope of use to a certain extent, without significantly improving the quality of life of patients, instead, they may increase the risk of other diseases, which can be more than worth the loss. Therefore, in recent years, there has been a wave of non-pharmacological treatments, such as cognitive-behavioral therapy, transcranial magnetic stimulation therapy and light therapy, etc. In this process, acupuncture therapy in traditional Chinese medicine has shown good efficacy and the lack of accompanying serious adverse effects is its main advantage while significantly improving patients' sleep disorders. A study by Qiu et al. showed that acupuncture therapy reduced the risk of insomnia in stroke patients after the disease[8]. With the increasing awareness of acupuncture therapy, there have been more Randomized Controlled Trials (RCT) on acupuncture therapy for PSSD in China and abroad. Meta-analysis was used in this study to evaluate the clinical efficacy of acupuncture therapy in the treatment of PSSD, with the aim of providing evidence-based medical for the clinical treatment of PSSD.
Materials and Methods
Literature inclusion and exclusion criteria:
Inclusion criteria: The following criteria were required for inclusion in the analysis; the included literature was all of the RCT of acupuncture therapy for PSSD. Patients with PSSD in the included literature met the diagnostic criteria established at the 4th Cerebrovascular Academic Conference in 1995, with consciousness and good cooperation, as well as the Chinese Classification Scheme and Diagnostic Criteria for Mental Disorders 3 (CCMD3); the 3rd edition of (CCMD3) diagnostic criteria for organic insomnia[9,10]. The interventions were as follows; conventional therapy was used in the control group, and acupuncture therapy was used on top of conventional therapy in the experimental group. Conventional therapy refers to various treatment modalities other than acupuncture therapy, and the conventional therapy used in the test and control groups must be the same. The outcome indicator was the score of clinical effectiveness or the Pittsburgh Sleep Quality Index (PSQI).
Exclusion criteria: Reviews, cohort studies, animal experiments, case studies, basic studies, crosssectional studies, case reports, etc.; literature with outcome indicators that did not meet the inclusion criteria; literature for which the full text was not available; literature for which information could not be extracted, complete raw data were not provided, and data requests were fruitless; literature with a sample size <15 cases; literature for which the control group included acupuncture, auricular acupuncture and electro acupuncture.
Literature search strategies:
First, we developed search strategies according to the "PICOS principles" in the Cochrane System Evaluation Manual and the literature databases searched were mainly Chinese databases and English databases, among which there were three main sources of English databases like PubMed, EMBASE and Cochrane Central Register of Controlled Trials; the three main sources of Chinese databases are China National Knowledge Infrastructure (CNKI), Wanfang Database and Sinomed. The search was limited to the period from the creation of the database to August 9, 2022.
For both English and Chinese databases, the search terms were different, with the English database using "stroke", "cerebrovascular accident", "sleep initiation and maintenance disorders", "poststroke insomnia", "sleep disordered after stroke", "acupuncture", "acupuncture treatment", "insomnia", "RCT" and other free words combined with subject words. The search strategies were determined after several pre-searches. The search terms "stroke", "cerebrovascular accident", "stroke", "poststroke insomnia", "post-stroke sleep disturbance", "sleep onset and sleep disturbance", "insomnia", "acupuncture", "acupuncture" and "RCT" were used in the Chinese databases and searched in the CNKI, Wanfang and Sinomed database.
Literature quality evaluation and data extraction:
The literature was screened separately by two trained researchers according to the inclusion criteria such as literature. The initial screening was based mainly on the title and abstract, after which the literature fitting the inclusion criteria was found and read in full, and the original authors were contacted if necessary to avoid data omission. In case of inconsistency with the literature evaluation results, a third party was asked to participate in the discussion and to resolve the issue.
The methodological quality of the included studies was evaluated in accordance with the RCT risk of bias assessment tool of the Cochrane Collaboration Network in a total of six areas, including random assignment methods, protocol concealment, blinding, completeness of outcome data, study results of selective reporting and other sources of bias[11]. The results of the methodological quality assessment were classified into three risk levels; low risk of bias, high risk of bias and unclear, each of which has a specific entry corresponding to it in the Cochrane risk of bias assessment guidelines[12]. Cochrane scoring was done independently by 2 assessors and a third party was invited to discuss the decision in case of inconsistent results. Data items extracted included baseline information of patients, randomly assigned groups and the number of cases per group (including the ratio of men to women in the test and control groups, disease duration, age, etc.), Cochrane score, interventions, outcome indicators (mainly clinical efficiency, PSQI score), etc.
Statistical methods:
Data statistical analysis was performed with RevMan 5.4 software and Stata 15 software recommended by the Cochrane collaboration. Relative Risk (RR) was used for dichotomous variables, and Mean Difference (MD) or Standard Mean Difference (SMD) was used as an indicator of efficacy for continuous variables included in the analysis, both with 95 % Confidence Interval (CI) for effect size. The experimental results were analyzed using Chi-square (χ2) test; if p≥0.1 and I2≤50 %, it indicated statistical homogeneity between tests and meta-analysis was performed using fixedeffect model; if p<0.1 and I2>50 %, it indicated statistical heterogeneity between tests, and randomeffect model was used for combined analysis of tests. Subgroup analysis and sensitivity analysis were used to analyze the causes and sources of heterogeneity. If the number of literature was sufficient, an inverted funnel plot was used to analyze the included literature for publication bias. The test level for meta-analysis was set uniformly at α=0.05, with results presented in the form of forest plots.
Results and Discussion
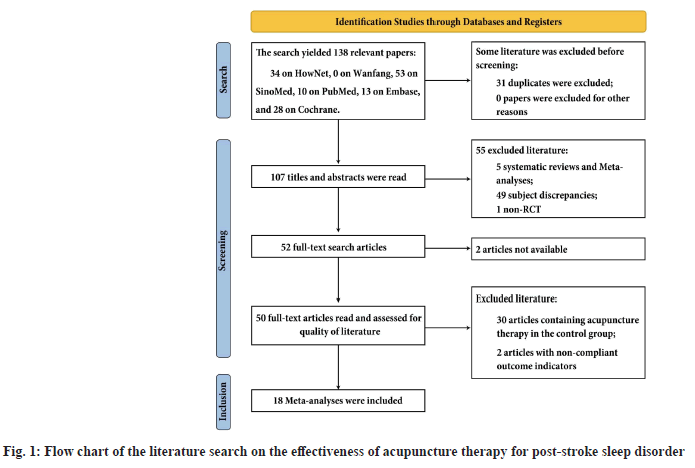
A total of 138 papers were obtained, including 87 from Chinese databases (34 from HowNet and 54 from Sinomed) and 51 from English databases (10 from PubMed, 13 from EMBASE and 28 from Cochrane). Endnote X9 was used to manage the above literature schematically, and 31 duplicates were excluded after the initial screening and duplicate check, leaving 107; 55 were excluded after reading the titles and abstracts. There were three main reasons, the literature was a systematic review or meta-analysis; the topic did not match the purpose of this study; the type of study was non-RCT. Subsequently, a search of the above initially screened literature revealed that the corresponding article content was not available for two of them, and they were excluded. Finally, a final screening of the above literature was performed, and 32 papers were excluded after reading the full text for the following reasons: The control group contained acupuncture therapy; the outcome indicators did not match those developed in this study. The total number of papers included in this study was 18 after the above-mentioned rigorous screening[13-30]. The literature search process and results are shown in fig. 1.
The 18 included studies were published between 2006 and 2020, with a total of 1475 patients, including 745 in the test group and 730 in the controsl group. The test groups included in the study used acupuncture therapy, with three main types; acupuncture alone, eye acupuncture and electro acupuncture. Twelve of the 18 studies were simple acupuncture therapy, three were acupuncture therapy combined with medication, and three were acupuncture therapy combined with physical therapy (including auricular point, ear pressure and scraping). Regarding the outcome indicators, 4 of the 18 studies used only clinical efficiency as an outcome indicator, 2 studies used only PSQI scores as an outcome indicator, and the remaining 12 studies used both of these as an outcome indicator. The basic characteristics of the included literature are shown in Table 1.
| Included study | Sample size [T/C (case)] | Age (year) | Disease Duration (day) | Interventions | Outcome Indicators | |||
|---|---|---|---|---|---|---|---|---|
| T | C | T | C | T | C | |||
| Liu et al.[13] | 32/30 | 69.9±6.9 | 67.5±8.2 | 34.4±7.2 | 33.1±8.2 | Acupuncture | Oral diazepam 2.5 mg/dose or estazolam 1 mg/dose, once a night | Clinical efficiency, PSQI |
| Ye et al.[14] | 43/42 | 62.8±7.2 | 67.3±8.3 | 21.3±7.4 | 24.6±6.9 | Acupuncture | Alprazolam 0.4 mg, once daily | Clinical efficiency, PSQI |
| Wu et al.[15] | 32/32 | 66.73±10.69 | 67.12±11.09 | 28.34±4.98 | 28.15±5.12 | Electro acupuncture with auricular points | Oral Sweet Dreams capsules, 3 capsules twice daily | Clinical efficiency |
| Sun et al.[16] | 30/30 | 40±15 | 40±15 | 1467.3±934.4 | 1408.9±1011.05 | Acupuncture with ear pressure | Oral estazolam 2 mg, once daily | Clinical efficiency, PSQI |
| Xu et al.[17] | 30/30 | 62.48±3.66 | 62.40±4.78 | 343.3±190.5 | 318.0±138.0 | Acupuncture | Oral diazepam 5.0 mg, once daily | Clinical efficiency, PSQI |
| Cao et al.[18] | 36/36 | 63±9 | 63±6 | 405.0±492.6 | 348.3±385.2 | Acupuncture | Pseudo acupuncture therapy | PSQI |
| Chen et al.[19] | 52/44 | 75.2±1.3 | 74.3±2.9 | 8.5±1.5 | 8.7±1.6 | Acupuncture | Oral diazepam | Clinical efficiency, PSQI |
| Li et al.[20] | 150/150 | 49.2 | 51.3 | Acupuncture combined with estazolam, 0.5 mg/day | Oral estazolam 0.5 mg/day | Clinical efficiency | ||
| Taibiao et al.[21] | 32/32 | 69.8±7.1 | 67.3±8.3 | 48±4.6 | 46±5.3 | Acupuncture | Oral diazepam 2.5 mg/dose or estazolam 1 mg/dose, once a night | Clinical efficiency, PSQI |
| Xi et al.[22] | 50/50 | 65±9 | 67±5 | 36±8 | 42±6 | Acupuncture combined with estazolam, 4 mg/day, then tapered | Estazolam 4 mg/day, then taper | Clinical efficiency |
| Yu et al.[23] | 40/38 | 61.5±2.1 | 63.1±2.5 | 45.2±3.4 | 42.5±2.5 | Acupuncture | Estazolam 2 mg/day | Clinical efficiency, PSQI |
| Wang et al.[24] | 32/30 | Acupuncture | Estazolam 1 mg/day | Clinical efficiency | ||||
| Hu et al.[25] | 30/30 | Eye acupuncture | Oral zopiclone 2.5 mg/day | Clinical efficiency, PSQI | ||||
| Jia et al.[26] | 30/30 | 62.5±6.4 | 63.1±7.0 | 31.2±6.6 | 36.5±8.1 | Acupuncture | Estazolam 2 mg/day | Clinical efficiency, PSQI |
| Guo et al.[27] | 30/30 | 65.23±11.29 | 63.50±10.93 | Acupuncture | Diazepam 5 mg/day | PSQI | ||
| Yan et al.[28] | 36/36 | 55.1±7.9 | 54.8±8.5 | Acupuncture combined with scraping therapy | Dexzopiclone 1 mg/day | Clinical efficiency, PSQI | ||
| Huang et al.[29] | 30/30 | 64 | 67 | Acupuncture combined with Bailemian capsules, 4 capsules/dose, 2 times/day | Bailemian capsules, 4 capsules/dose, 2 times/day | Clinical efficiency, PSQI | ||
| Huang et al.[30] | 30/30 | 60.17±10.12 | 59.47±8.34 | 10.77±5.15 | 11.53±4.17 | Acupuncture | Estazolam 1mg/day | Clinical efficiency, PSQI |
Table 1: Basic Characteristics of the Literature Included in the Effectiveness of Acupuncture Therapy for Post-Stroke Sleep Disorder (X̄±S)
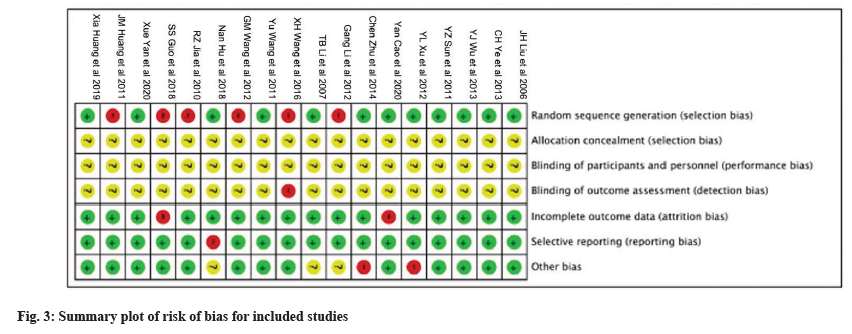
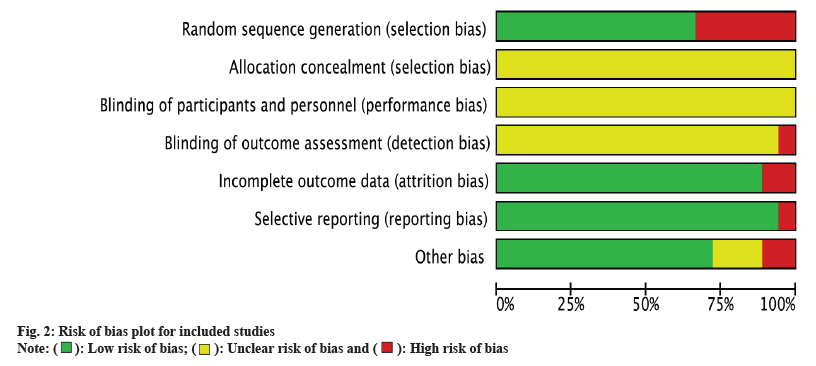
Of the 18 included studies, all mentioned random assignment, with 8 studies describing the use of the "random number table method" to generate random sequences, 2 studies describing random numbering by order of visit, 1 study describing random assignment by single or double number of admission date, and 1 study using central stratified, variable group randomization for random assignment, while the remaining 6 studies did not explicitly mention the method of random assignment. It was not stated in all studies whether the implementers, subjects were blinded (both single- and double-blind), and only one study had a high risk assessment for the outcome indicator; the rest were not specified; the use of allocation concealment was not mentioned in all studies; it was not clear whether the outcome indicator was selectively reported biased or otherwise biased; and all studies indicated that the baseline information was comparable. The risk of bias assessment tool recommended by the Cochrane collaboration was used to evaluate the methodological quality of the literature for the included studies. The risk of bias for the 18 studies is shown in fig. 2 and fig. 3.
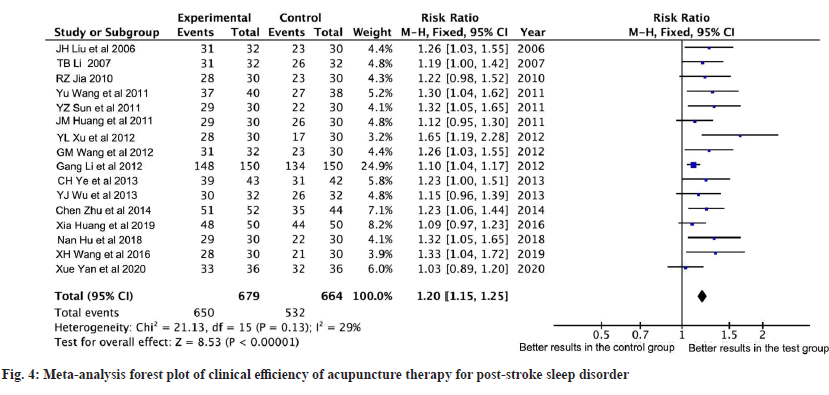
Clinical efficiency was used as an outcome indicator in a total of 16 studies, and the heterogeneity test results showed I2=29 %, p=0.13, indicating that there was no statistical heterogeneity among studies, so a fixed-effects model was used. The results showed that the clinical efficiency of acupuncture therapy for PSSD was statistically significant compared with the control group (RR=1.20, 95 % CI (1.15, 1.25), p<0.00001), indicating that the efficacy of acupuncture therapy for PSSD was better than that of the control group. The results are shown in fig. 4.
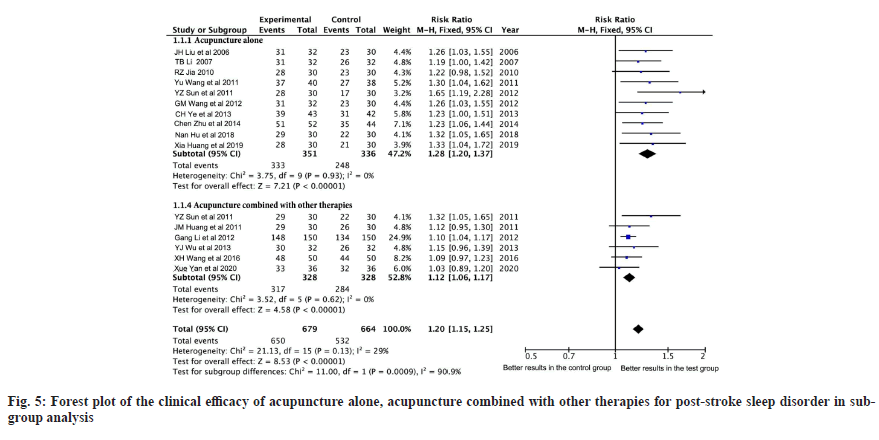
The interventions in the test groups of the 18 studies included in the analysis varied and were divided into 2 main types; acupuncture therapy alone and acupuncture combined with other therapies. The test groups of 10 of the studies were acupuncture therapy alone, and the results of the heterogeneity test showed I2=0 % and p=0.93 compared with their corresponding control groups, so a fixed-effect model was used. The results showed a statistically significant difference between acupuncture therapy alone compared to the control group (RR=1.28, 95 % CI (1.20, 1.37), p<0.00001), and the results are shown in fig. 5. The test group in six studies was acupuncture combined with other therapies, and the heterogeneity test showed I2=0 %, p=0.62, so a fixed-effects model was used. The results showed a statistically significant difference in acupuncture combined with other treatments compared with that of the control group (RR=1.12, 95 % CI (1.06, 1.17), p<0.00001), and the results are shown in fig. 5. When the subgroups were combined, the heterogeneity test resulted in I2=29 % and p=0.0009, indicating that acupuncture combined with or without other therapies did not affect its efficiency in treating post-stroke sleep disorder patients, i.e., acupuncture improved sleep disturbance in post-stroke sleep disorder patients.
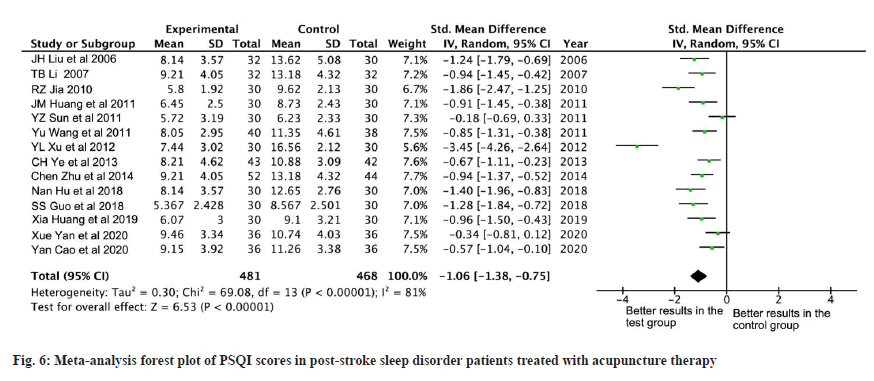
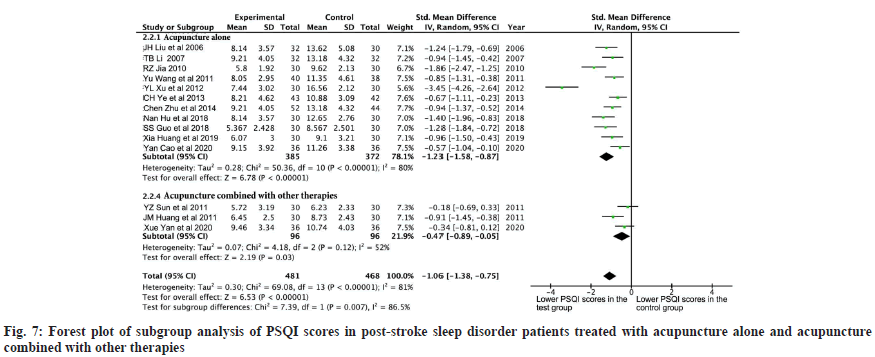
PSQI scoring was used as an outcome indicator in a total of 14 studies, and the heterogeneity test results showed I2=81 %, p<0.00001, indicating statistical heterogeneity among studies, so a random-effects model was used. The results showed a statistically significant difference in PSQI scoring in patients with post-stroke sleep disorder treated with acupuncture therapy compared with the control group (RR=-1.06, 95 % CI (-1.38, -0.75), p<0.00001), indicating that PSQI scores were lower in patients with post-stroke sleep disorder treated with acupuncture therapy compared with the control group. The results are shown in fig. 6.
Because of the large heterogeneity of the 14 papers included in this study and the different interventions in the test groups in different studies, we performed subgroup stratification analysis based on the different interventions in the test groups, which were further divided into 2 subgroups, namely; acupuncture alone and acupuncture combined with other therapies. A random-effects model was used in 11 studies in which only acupuncture therapy was used, as the heterogeneity test showed I2=80 %, p<0.00001. The results showed a statistically significant difference between acupuncture therapy alone compared to that of the control group (RR=-1.23, 95 % CI (-1.58, -0.87), p<0.00001), and the results are shown in fig. 7. In three studies, acupuncture was used in combination with other therapies and their heterogeneity test showed I2=52 %, p=0.12, so a random effects model was used. The results showed a statistically significant difference between acupuncture combined with physiotherapy compared to that of the control group (RR=-0.47, 95 % CI (-0.89, -0.05), p=0.03), and the results are shown in fig. 7. When the subgroups were merged, the test for heterogeneity was I2=81 % and p=0.007, indicating that acupuncture combined with or without other therapies may have been a source of heterogeneity in this study, but not the only source of heterogeneity. The RR values of all subgroups were statistically different regardless of whether acupuncture was combined with other treatments, indicating that acupuncture therapy did significantly reduce PSQI scores in patients with post-stroke sleep disorder.
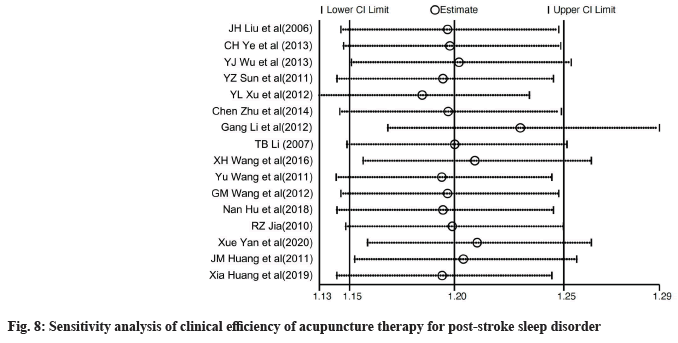
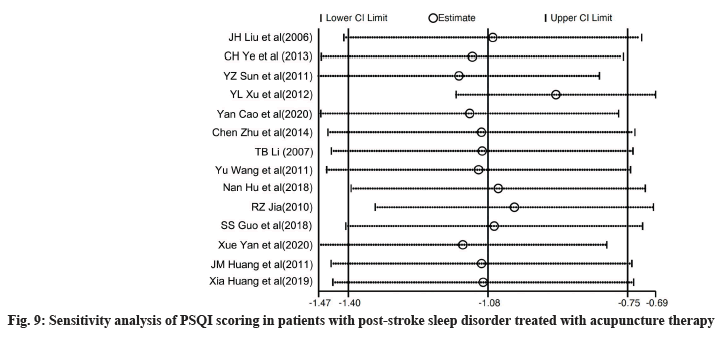
From the above analysis, it is clear that the heterogeneity among the studies in this metaanalysis was large, especially in the analysis of PSQI scores for post-stroke sleep disorder patients treated with acupuncture therapy, and the results of the heterogeneity test were >50 % in both subgroup and combined analyses, suggesting a high degree of heterogeneity, so a sensitivity analysis is needed to explore the sources of heterogeneity. Fig. 8 demonstrates the results of the sensitivity analysis for clinical efficiency. It is easy to see that the study by Li et al.[20] had a greater effect on clinical effectiveness compared to other studies, which may be due to the larger sample size of this study compared to other studies, but this is insufficient to be a major source of heterogeneity in this study and does not significantly interfere with the results of this meta-analysis. Fig. 9 demonstrates the results of the sensitivity analysis for the PSQI score. Unlike the findings of the sensitivity analysis of clinical efficiency, the effect of the study by Xu et al.[17] on PSQI scores was larger but within a reasonable interval and not sufficient to affect the results of this meta-analysis, so the source of heterogeneity in this study needs to be further explored.
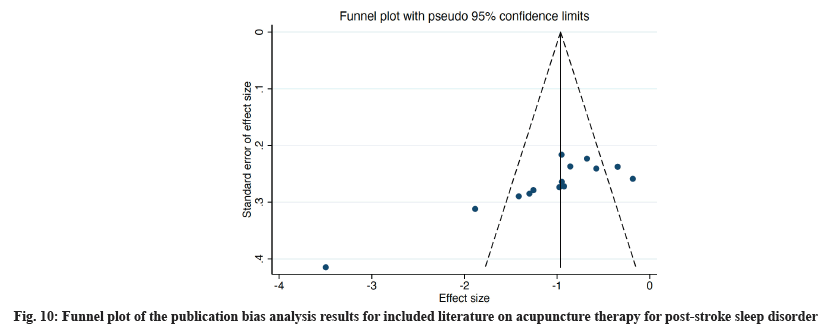
A funnel plot was used to evaluate the publication bias of the included literature, and the results are shown in fig. 10. As shown in fig. 10, most of the points are distributed more evenly in the middle of the funnel, but some points are still located outside the funnel, presenting an overall incomplete symmetry, and there are almost no scattered points at the top of the funnel, suggesting the possibility of publication bias in the included studies. It was considered that the reasons for bias may be related to the site of acupuncture and the duration of treatment used in the test group, or to the different interventions, doses, types and duration of treatment used in the control group, as well as to the small sample size.
PSSD refers to insomnia that occurs after stroke, a type of secondary insomnia, which mainly manifests as reduced sleep duration, difficulty in falling asleep, difficulty in maintaining sleep, etc. It seriously affects the sleep quality of patients and can cause great harm to their physical and mental health and physiological functions[31]. Patients with severe sleep deprivation have a higher risk of secondary strokes, which will further aggravate the patient's condition. Acupuncture, as a unique treatment modality in TCM, has many advantages in the treatment of PSSD, such as less invasive, low incidence of adverse reactions, and no tolerance and dependence[32]. Acupuncture is based on the theory of meridians, which promotes sleep by stimulating specific points to open up the meridians and soothe the body and mind.
A total of 18 randomized controlled trials on the treatment of PSSD with acupuncture therapy involving 1475 patients were included in this meta-analysis. The analysis showed that the clinical effectiveness of acupuncture therapy was better than that of the control group and that PSSD patients treated by acupuncture therapy had lower PSQI scores than those in the control group. All of these results suggest that acupuncture therapy can significantly improve sleep in PSSD patients and promote sleep to some extent. Because of differences in the interventions in the trial groups of the literature included in this meta-analysis, we analyzed the study by subgroups according to whether acupuncture therapy was combined with other treatment modalities. The results showed that the heterogeneity of the study and the final conclusions obtained did not change significantly with or without the combination of other treatment modalities, suggesting further that other treatment modalities were not a source of heterogeneity in this analysis and that evaluation effectiveness of acupuncture therapy in the treatment of PSSD patients was more reliable. Since during the evaluation of the effectiveness of acupuncture therapy for PSSD according to PSQI scores, we found a large heterogeneity between trials, a random-effects model was used to perform a subgroup analysis of the study, which showed that whether or not to combine other treatments was not the only or main source of heterogeneity in this study, i.e., the differences between the test and control groups were statistically significantly different regardless of the combination. Subsequently, we performed sensitivity analyses for the two analyses mentioned above and found that the studies by Li et al. and Xu et al. may be one of the sources of heterogeneity in this study, which may be due to the larger sample size of the above studies and therefore more relevant to the conclusions. Finally, we performed an assessment of publication bias and the results showed that the study had a more significant publication bias, which may be related to the different interventions, doses, types of drugs used and duration of treatment in the different subgroups of the trial, as well as the small sample size.
From the above analysis, it is clear that this study has certain limitations and shortcomings as follows; most of the included studies were small-sample randomized controlled studies, and the methodological quality of the included RCTs was not high enough, so the possibility of heterogeneity between studies was great. Moreover, all the literature included in this paper was in Chinese, and all the relevant English literature searched by English databases were excluded due to the inclusion and exclusion criteria or because the corresponding literature could not be searched, which may be one of the sources of bias in this study. There was publication bias in the literature included in this study, with funnel plots suggesting that the scatters were all located in the middle of the funnel in an incomplete symmetry, and some of the scatters were visible outside the funnel, which may suggest the possibility of unpublished negative outcome trials. The lack of long-term follow-up information in the included studies, with only a very small number of studies mentioning follow-up information of PSSD patients' 1-3 mo after treatment with acupuncture, is of great clinical importance to assess the long-term efficacy of acupuncture therapy for PSSD. The different treatment of the control group in this study was also one of the main sources of heterogeneity, so it is recommended that uniform interventions, drug doses and types be used in future studies for either the test or control group.
In summary, based on current evidence, the clinical effectiveness of acupuncture therapy in treating patients with post-stroke sleep disorder has been more than adequately confirmed, helping to relieve the psychosomatic stress caused by sleep deprivation and improving the quality of life of patients after the disease to some extent. Meanwhile, acupuncture therapy, as a characteristic treatment modality of traditional Chinese medicine, can be fully promoted in clinical practice because of its low side effects, low trauma and good therapeutic effects. However, the heterogeneity and publication bias of this study should not be ignored, so in the future, a welldesigned, large-sample, multicenter RCT with long-term follow-up should be conducted to further evaluate the efficacy and safety of acupuncture therapy in the treatment of patients with PSSD.
Funding:
This research was supported by Jilin Province Science and Technology Development Program, No. 20210401150YY.
Conflict of interests:
The authors declared no conflict of interests.
References
- Hankey GJ. Stroke. Lancet 2017;389(10069):641-54.
[Crossref] [Google Scholar] [PubMed]
- Campbell BC, de Silva DA, Macleod MR, Coutts SB, Schwamm LH, Davis SM, et al. Ischaemic stroke. Nat Rev Dis Primers 2019;5(1):70.
[Crossref] [Google Scholar] [PubMed]
- Tuo QZ, Zhang ST, Lei P. Mechanisms of neuronal cell death in ischemic stroke and their therapeutic implications. Med Res Rev 2022;42(1):259-305.
[Crossref] [Google Scholar] [PubMed]
- Stinear CM, Lang CE, Zeiler S, Byblow WD. Advances and challenges in stroke rehabilitation. Lancet Neurol 2020;19(4):348-60.
[Crossref] [Google Scholar] [PubMed]
- Kumar S, Selim MH, Caplan LR. Medical complications after stroke. Lancet Neurol 2010;9(1):105-18.
[Crossref] [Google Scholar] [PubMed]
- Cai H, Wang XP, Yang GY. Sleep disorders in stroke: An update on management. Aging Dis 2021;12(2):570-85.
[Crossref] [Google Scholar] [PubMed]
- Cao Y, Yin X, Soto-Aguilar F, Liu Y, Yin P, Wu J, et al. Effect of acupuncture on insomnia following stroke: Study protocol for a randomized controlled trial. Trials 2016;17:546.
[Crossref] [Google Scholar] [PubMed]
- Qiu X, Han NS, Yao JX, Yu FR, Lin YY, Zhuang X. Acupuncture reduced the risk for insomnia in stroke patients: A propensity-score matched cohort study. Front Aging Neurosci 2021;13:698988.
[Crossref] [Google Scholar] [PubMed]
- Chinese Medical Association. Essentials of diagnosis of various cerebrovascular diseases. Chin J Neurol 19967;60-1.
- Chinese Medical Association Psychiatric Branch. Classification Scheme and Diagnostic Criteria for Mental Disorders in China. 3rd ed. Shandong Science and Technology Press; 2001.p. 87.
- Cochrane handbook for systematic reviews of interventions: Cochrane book series; 2008.
- Gu H, Wang Y, Li W. Application of the cochrane risk of bias assessment tool in meta-analysis of randomized controlled studies. Chin Circ J 2014;29:147-8.
- Liu J, Huang J, Chen X. Efficacy observation of acupuncture in the treatment of 32 cases of post-stroke insomnia. Int Med Health J 2006;5:23-9.
- Ye C, Ou C, Xu Z, He Y. Clinical observation of acupuncture for the treatment of post-stroke sleep disorders. Chin J New Clin Med 2013;8(2):65-8.
- Wu Y, Yu D, Chen H. Clinical study of electro acupuncture with auricular points for the treatment of post-stroke sleep disorders. J Chin Med 2013;84:796-9.
- Sun Y, Xia K. Clinical Observation on the Treatment of Post-stroke Sleep Disorders by Acupuncture with Auricular Point Applying Pressure. Shanghai J Acupunct Moxibustion 2011.
- Xu Y, Chen J, Ye F. Clinical study on the treatment of post-stroke sleep disorders by acupuncture of Baihui point as the main method of regulating Du meridian. Chin J Rehabil Med 2012;9(5):84-9.
- Cao Y, Yan Y, Liu Y, Xu S. Randomized controlled study on the treatment of post-stroke sleep disorders with regulating Du and tranquilizing acupuncture. Shanghai J Acupunct Moxibustion 2020;280-4.
- Chen Z. Clinical observation of acupuncture for post-stroke sleep disorders. Guangxi J Tradit Chin Med 2014;4:12-6.
- Li G, Zhang Y, Luo H. Efficacy observation of acupuncture combined with estazolam in the treatment of post-stroke sleep disorders. Med J Natl Chin 2012;5:54-8.
- Taibiao L. Observation on the efficacy of acupuncture in the treatment of post-stroke sleep disorders. Chin J Rehabil Theory Pract 2007.
- Xi W, Zhou Z, Wang Y. Effect of regulating mind and sleep acupuncture combined with estazolam on insomnia after cerebral infarction. Hebei Tradit Chin Med J 2016;3:43-8.
- Yu W. Clinical observation on the treatment of post-stroke sleep disorders by the acupuncture method of "Du Yuan co-regulation". Guangxi Tradit Chin Med 2011;5:21-7.
- Wang G, Zhao H. Clinical observation of 32 cases of acupuncture for post-stroke sleep disorders. Shanxi J Tradit Chin Med 2012;56:81-9.
- Hu N, Yu R. Clinical observation of eye acupuncture combined with Baoshentang in the treatment of post-stroke sleep disorders. J Liaoning Univ Tradit Chin Med 2018;7:51-8.
- Jia R. Clinical study of acupuncture to improve the state of patients with post-stroke sleep disorders. Guangming J Chin Med 2010;2:24-7.
- Guo S. A randomized controlled study of eye acupuncture therapy for post-stroke sleep disorders. Liaoning Univ Tradit Chin Med 2018;6:72-6.
- Yan X. Clinical study of acupuncture with scraping therapy for the treatment of post-stroke sleep disorders. World J Sleep Med 2020;3:45-9.
- Huang J, Wang K. 30 cases of acupuncture and medicine combination for post-stroke sleep disorders. Shaanxi J Tradit Chin Med 2011;14:654-68.
- Huang X, Su S, Chen S, Huang Xi. Clinical efficacy observation of spleen strengthening and mind regulating method of acupuncture for post-stroke sleep disorders. Liaoning J Tradit Chin Med 2019;85:54-7.
- Rost NS, Brodtmann A, Pase MP, van Veluw SJ, Biffi A, Duering M, et al. Post-stroke cognitive impairment and dementia. Circ Res 2022;130(8):1252-71.
[Crossref] [Google Scholar] [PubMed]
- Guo J, Wang J, Sun W, Liu X. The advances of post-stroke depression: 2021 update. J Neurol 2021;269(3):1236-49.
[Crossref] [Google Scholar] [PubMed]
 ): Low risk of bias; (
): Low risk of bias; ( ): Unclear risk of bias and (
): Unclear risk of bias and ( ): High risk of bias
): High risk of bias