- *Corresponding Author:
- Shue Wang
Department of Internal Medicine and Endocrinology, Zhongnan Hospital, Wuhan University, Wuhan, Hubei Province 430071, China
E-mail: yiwuzhijing2023@163.com
| This article was originally published in a special issue, “Clinical Advancements in Life Sciences and Pharmaceutical Research” |
| Indian J Pharm Sci 2024:86(5) Spl Issue “239-252” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Chinese herbal medicine and telemedicine are two promising approaches to enhancing the management of chronic diseases. Chinese herbal medicine offers a diverse range of treatments based on traditional knowledge, utilizing bioactive compound with anti-inflammatory, immunomodulatory, antioxidant and other beneficial effects. Increasingly rigorous studies are validating the effectiveness of Chinese herbal medicine in various chronic conditions such as cardiovascular diseases, diabetes, respiratory ailments, and cancer. At the same time, telemedicine has revolutionized healthcare by enabling remote diagnosis, treatment, and patient monitoring. It overcomes geographical barriers, facilitates continuous communication between patients and healthcare providers, promotes treatment adherence through education, and enhances cost-effectiveness. The integration of Chinese herbal medicine and telemedicine has the potential to provide personalized and holistic care, leveraging technological advancements. However, this integration also presents challenges, including standardizing herbal formulations, understanding pharmacological mechanisms, managing drug interactions, generating robust clinical evidence, navigating regulatory complexities, and addressing cultural barriers. These challenges require rigorous scientific investigation. Nonetheless, this integrative approach aligns with current healthcare trends, offering a patient-centric model that combines traditional wisdom with modern innovations. The aim of this review is to critically analyze the potential synergies between Chinese herbal medicine and telemedicine in chronic disease management. This analysis aims to establish a foundation for future research directions and the practical application of this integrated approach.
Keywords
Chronic diseases, telemedicine, Chinese herbal medicine, neuro-biochemical processes, diabetes
Chronic diseases, characterized by their prolonged course and gradual progression, pose a growing global health challenge. Non-Communicable Diseases (NCDs) like cardiovascular disease, cancer, and diabetes are the leading cause of death worldwide, demanding innovative approaches to management[1]. Traditional management relies on a combination of medications, lifestyle changes, and regular monitoring, focusing on slowing disease progression and symptom relief. While pharmacotherapy has achieved significant advancements, limitations like patient non-adherence and adverse drug reactions necessitate alternative strategies[2,3].
Chinese Herbal Medicine (CHM), with its holistic approach and generally well tolerated treatment profiles, offers a complementary or alternative option. While its use for various ailments spans centuries, recent studies have validated its efficacy[4]. The bioactive compounds in CHM exert diverse effects, often modulating the neuro-biochemical pathways implicated in chronic disease development[5].
Telemedicine, a digital health intervention, has revolutionized healthcare delivery by enabling remote diagnosis, treatment, and patient monitoring. It overcomes geographical barriers and improves access to care, particularly crucial for chronic disease management, which requires ongoing patient engagement and monitoring[6]. The synergy between CHM and telemedicine in chronic disease management holds significant promise[7]. CHM provides a diverse therapeutic arsenal that can be tailored to individual patient needs. Telemedicine, on the other hand, fosters continuous patient-provider communication and promotes treatment adherence through targeted education and follow-ups. Additionally, telemedicine platforms can serve as repositories of patient data, potentially aiding future evidence-based CHM implementation and furthering our understanding of its impact on chronic diseases[8,9].
This review aims to critically analyze the potential synergies between CHM and telemedicine for chronic disease management. We will explore recent neuro-biochemical evidence on CHM’s effects, assess its safety and efficacy, and evaluate the role of telemedicine in improving patient-centered outcomes and healthcare delivery efficiency. Ultimately, this review seeks to establish a platform for future research directions and the practical application of CHM within telemedicine platforms, paving the way for a unified, patient-focused, and sustainable approach to chronic disease management.
The Increasing Burden of Chronic Diseases
A renewed warning by the global risks report 2011 identifies five chronic diseases that will have a significant impact on China’s medical and economic systems in the next two decades. These diseases are cardiovascular diseases, tumors, diabetes, respiratory diseases and mental disorders[10,11]. In fact, chronic diseases are responsible for 87 % of total deaths in China. They also account for about 70 % of the country’s total disease burden, posing a significant challenge for prevention and treatment. Additionally, nearly 300 million Chinese people suffer from hypertension and obesity. It is estimated that approximately 100 million Chinese people are affected by diabetes and Chronic Obstructive Pulmonary Disease (COPD), while >10 million people suffer from stroke, Coronary Heart Disease (CHD) and obesity, respectively[12-14]. These diseases not only consume a significant number of medical resources but also impose a heavy burden on individuals, their families, and society at large.
The prevalence of cardiovascular diseases is increasing in China. The cardiovascular disease report in China 2022, released by China’s National Center for Cardiovascular Disease[15], indicates that approximately 290 million people in China have cardiovascular diseases. This includes 250 million people with hypertension and 11 million people with CHD[16,17]. Evidence-based medicine studies have shown that hypertension has become one of the most significant risk factors for cardiovascular and cerebrovascular diseases among the Chinese population. It accounts for more than half of the incidence and mortality related to these diseases[18,19]. The prevalence of hypertension among adults rises significantly with age. For instance, nearly 1/3rd of the population aged (45-59) y and half of the elderly population suffer from hypertension[20]. However, it is concerning that awareness, treatment, and control rates for hypertension are low while the prevalence, disability, and mortality rates remain high. Therefore, it is crucial to prioritize the prevention and treatment of cardiovascular and cerebrovascular diseases by addressing the issue of hypertension[21].
Stroke is the 2nd leading cause of death among individuals aged 60 y and older in China. It has become a significant global public health concern due to its high incidence, disability, and mortality rates[22]. In the past three decades, the incidence of stroke has increased by 32 % among rural residents and by 18.1 % among urban residents. Furthermore, strokes are now affecting people at a younger age[15,23]. According to the 2010 China Chronic Disease and Risk Factor Surveillance (CCDRFS), the age-standardized prevalence of Transient Ischemic Attack (TIA) in China was approximately 2 %, with awareness and treatment rates below 10 %. Since TIA is considered a precursor to stroke, proactive intervention could effectively prevent stroke incidence[24]. It is worth noting that the mortality rate of ischemic stroke has increased, while the rate of hemorrhagic stroke has decreased [22]. This trend can be attributed to efforts in hypertension prevention and treatment, as well as primary prevention.
It is projected that chronic respiratory diseases, specifically COPD, will become the 3rd leading cause of death globally by 2022, following ischemic heart disease and cerebrovascular disease[25]. According to the global burden of disease, the number of disability-adjusted life years lost to COPD in China is estimated to exceed 2000 per 100 000 individuals, significantly impacting the prognosis and quality of life for middle-aged and elderly patients. The estimated total number of COPD patients is 100 million, making COPD a prevalent chronic disease on par with hypertension and diabetes[26]. Between 1990 and 2019, China’s COPD diagnosis rate varied from 23.6 % to 30.0 %, and only half of those diagnosed received treatment. There is a low level of awareness among frontline doctors regarding COPD prevention and treatment, highlighting the need for enhancements in basic health services and efforts to prevent COPD[26].
Diabetes is the leading cause of kidney failure worldwide, particularly in developing countries such as China, where glomerulonephritis is the predominant cause. The prevalence of obesity and diabetes has significantly increased, causing a shift in the patterns of Chronic Kidney Disease (CKD). In China, diabetes-related CKD has surpassed glomerulonephritis-related CKD since 2011, resulting in the emergence of hypertensive nephropathy and obstructive kidney disease. To address this issue, public health interventions have been implemented, including the establishment of a national CKD surveillance system, improved management of diabetes and hypertension, and enhanced affordability of kidney replacement therapy[27,28].
The Role of CHM in Treating Chronic Diseases
The global prevalence of chronic illnesses has created an urgent need to explore a diverse range of treatment approaches. CHM, with its extensive historical background and holistic principles, emerges as a highly valuable contender in this field. CHM is based on the concept of Qi, the vital energy that flows throughout the body. Its treatment approach aims to restore balance within this energy system by addressing the root causes of chronic conditions, rather than simply alleviating symptoms[29,30].
The vast array of CHM encompasses thousands of medicinal plants, minerals, and animal products, forming a unique therapeutic treasure trove[31]. Modern scientific research is shedding light on the scientific basis for the effectiveness of CHM. These traditional remedies contain bioactive compounds exhibiting various pharmacological properties, including anti-inflammatory, immunomodulatory, and antioxidant effects[32,33]. For example, astragaloside IV, a compound found in Astragalus membranaceus, demonstrates immunomodulatory properties, suggesting its potential use in managing autoimmune diseases[34]. Moreover, CHM targets inflammation effectively, a common underlying factor in the progression of many chronic disease[35]. Berberine, an alkaloid present in Coptis chinensis, has been shown to inhibit inflammatory responses and decrease the production of pro-inflammatory cytokines[36]. Additionally, CHM constituents with antioxidant properties, such as epigallocatechin gallate found in green tea, help reduce oxidative stress, a contributing factor to chronic conditions like cardiovascular disease and diabetes[37]. CHM also holds potential for benefiting neurodegenerative diseases and chronic pain, which often involve neuro-biochemical pathways[38]. Ginkgo biloba, renowned for its neuroprotective effects, enhances cerebral blood flow and interacts with neurotransmitter systems, offering potential relief for these conditions[39]. Diseases related to chronic metabolism, such as diabetes and obesity, are particularly relevant areas where CHM shows promise[40]. Certain CHM formulations have been shown to improve insulin sensitivity and regulate lipid metabolism by influencing complex metabolic networks[41-46]. Table 1 represents a compilation of studies that have investigated the possible impact of CHM on the management of chronic diseases[47-54].
| Author | Type of disease | Study type | Samples size | Country | Goals of study | Results | Conclusion |
|---|---|---|---|---|---|---|---|
| Huang et al.[47] | CKD | Retrospective cohort | 14 718 CKD patients | Taiwan | Treatment with CHM affected the survival rate of CKD patients undergoing conventional Western medical management | The long-term survival rate demonstrated significant benefits for CHM users within a 12 y follow-up period | CHM improves long-term survival in patients with CKD |
| Coyle et al.[42] | COPD | Systematic Review | 11 999 participants | - | Adverse events reported in clinical studies of CHM for COPD | The rate of adverse events was slightly lower in the CHM groups compared with controls. The most frequently reported adverse event was nausea | Overall, CHM appears to be well tolerated in people with COPD |
| Li et al.[48] | CHF | Systematic review and meta-analysis | 3170 participants | - | Evaluate published clinical trials of OCHM for the improvement of quality of life in patients with CHF | There is encouraging evidence of OCHM combined with CMT to improve quality of life in CHF patients | The evidence remains weak due to the small sample size, high clinical heterogeneity, and poor methodological quality of the included trials |
| Tsai et al.[49] | HCV | Longitudinal and retrospective cohort | 98 788 patients | Taiwan | Investigate the effects of the long-term use of CHM for the treatment of liver diseases | The CHM users had a lower risk of liver cirrhosis than non-users after adjustment for comorbidities | CHM as adjunctive therapy may reduce the overall mortality and the risk of liver cirrhosis in patients with HCV |
| Tsai et al.[50] | HIV-infected patients | Retrospective cohort | 21 846 HIV-infected patients | Taiwan | Assess the long-term effects of CHM on hyperlipidemia and cardiovascular disease events in HIV-infected patients | CHM users had a lower risk of hyperlipidemia compared with non-users after adjusting for comorbidities by using a multivariate Cox proportional hazard model. In addition, the CHM users had a lower risk of cardiovascular disease compared with non-users after adjusting for comorbidities | CHM as adjunctive therapy may reduce hyperlipidemia and the risk for cardiovascular disease in HIV-infected patients |
| Coyle et al.[51] | Psoriasis vulgaris and chronic urticaria | Qualitative study | 20 participants | China/Australia | Experience of using CHM for psoriasis vulgaris and chronic urticaria | Motivators included wanting an alternative to conventional medicine, beliefs about CHM and previous experience | Previous experience of using CHM, desire to prevent relapse, and safety are important motivators for choosing CHM in people with psoriasis vulgaris and chronic urticaria |
| Zhang et al.[52] | DKD | Systematic review and meta-analysis | 2719 DKD patients | - | Evaluation of the efficacy and safety of oral CHM as an adjunctive treatment for DKD | CHM was associated with a greater reduction of albuminuria than placebo | CHM may have beneficial effects on renal function and albuminuria in adults with DKD |
| Tsai et al.[53] | Stroke patients with T2D | Retrospective cohort | 3079 stroke patients with T2D | Taiwan | Investigate the frequencies and patterns of CHM treatment for stroke patients with T2D and the outcomes of long-term | The cumulative survival probability was higher in the CHM group | The use of CHM as adjunctive therapy may improve the overall survival of stroke patients with T2D |
| Zhang et al.[54] | CHD | Systematic review | 305 765 patients with CHD | - | Investigate the efficacy and safety of CHM for CHD based on high-quality randomized controlled trials | Meta-analyses showed CHM can significantly reduce the incidence of myocardial infarction and percutaneous coronary intervention, and cardiovascular mortality, and increase systolic function of heart, the ST-segment depression, and clinical efficacy | CHMs are beneficial for CHD and are generally safe |
Note: CHF: Chronic Heart Failure; OCHM: Oral Chinese Herbal Medicine; CMT: Chinese Medicine Treatment; HCV: Hepatitis C Virus and DKD: Diabetic Kidney Disease
Table 1: Some studies that investigated the effect of CHM on chronic diseases.
Rigorous scientific research, including randomized controlled trials, is increasingly validating the clinical efficacy of CHM in managing chronic diseases. Studies have reported significant improvements in symptoms and overall quality of life for patients with conditions such as COPD after receiving CHM treatment. However, it is crucial to address safety and quality control concerns. Ensuring potential interactions with pharmaceuticals are identified, standardizing herbal preparations, and accurately identifying medicinal plants are paramount to guarantee patient safety[42,43].
The recent rise of telemedicine presents a unique opportunity to integrate CHM into mainstream healthcare. Telemedicine enables remote consultations, allowing practitioners to efficiently diagnose, prescribe, and adjust CHM treatments regardless of location. This can be particularly useful for patients with chronic diseases that require long-term care and continuous monitoring[44]. Telemedicine fosters a more accessible, personalized, and efficient delivery of CHM[45]. Furthermore, telemedicine platforms can serve as valuable tools for monitoring the safety and efficacy of Traditional Chinese Medicine (TCM) treatments[46]. Real-time reporting of adverse effects and monitoring of adherence can be facilitated, leading to optimized patient outcomes. This synergy between TCM and telemedicine has the potential to revolutionize chronic disease care, offering a comprehensive approach that bridges the gap between traditional and modern medicine[6].
In conclusion, TCM presents a significant and complementary approach to conventional medicine for chronic disease treatment. Its complex array of bioactive compounds and holistic treatment strategies offer immense promise. Integrating TCM with contemporary telemedicine services has the potential to create a more personalized and effective healthcare system for chronic disease management. Further rigorous research is crucial to fully understand TCM’s mechanisms of action, ensure patient safety, and validate its clinical efficacy. As the bridge between traditional knowledge and modern science continues to strengthen, the role of TCM in the global healthcare system is poised to become increasingly prominent, offering new hope and treatment options for patients with chronic conditions.
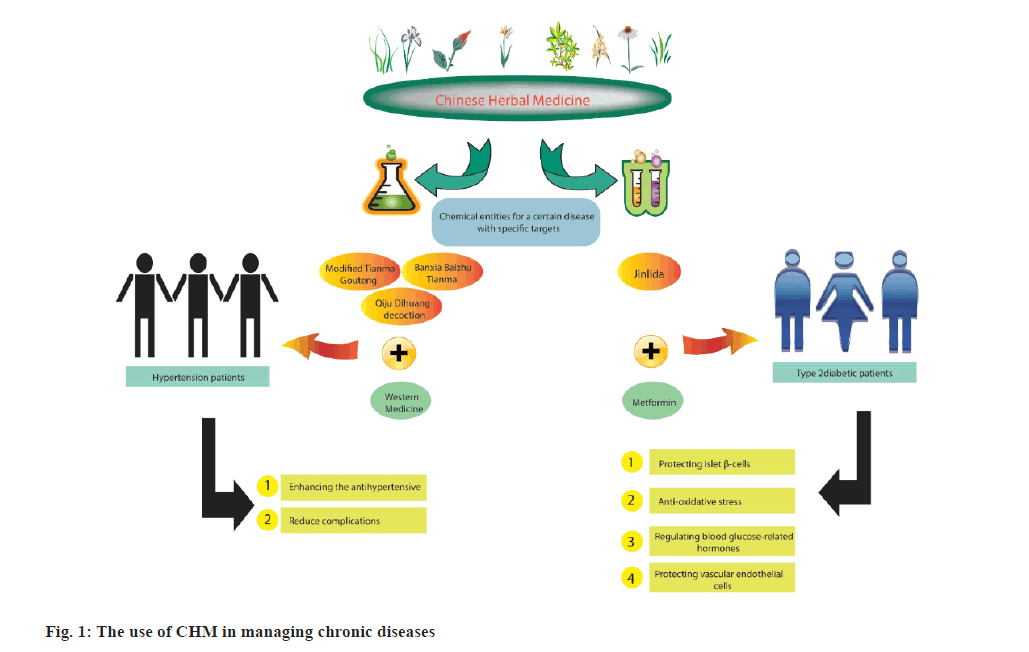
Hypertension is a significant global health concern, affecting approximately one billion people worldwide and over three hundred million patients in China. It is responsible for approximately seven million deaths annually. Studies have shown that individuals between the ages of 40 y and 70 y with high blood pressure have a two-fold increased risk of developing cardiovascular disease when their blood pressure increases by 20 mmHg and 10 mmHg, respectively[55,56]. Moreover, the risk of stroke and fatal myocardial infarction increases by 53 % and 31 %, respectively, for each 10 mmHg increase in Systolic Blood Pressure (SBP)[57]. Antihypertensive drugs, such as diuretics, long-acting Calcium Channel Blockers (CCB), Angiotensin-Converting Enzyme Inhibitors (ACEI), Angiotensin II Receptor Blockers (ARB), and beta-blockers, have been used as primary therapeutic agents for managing hypertension[58]. However, their clinical application has been limited by adverse reactions, including headache, dizziness, orthostatic hypotension, sexual dysfunction, and other issues[59]. In China, approximately 20 % of hypertension patients have been treated with TCM. Several studies have demonstrated that CHM can effectively lower systolic and diastolic blood pressure and reduce complications. CHM has been used as an adjuvant therapy alongside Western Medicine (WM) for patients with Pulmonary Hypertension (PHTN), resulting in improved antihypertensive efficacy without an increase in adverse effects[60,61]. The national incidence of Type 2 Diabetes (T2D) in China is increasing annually, with an estimated overall prevalence of 10.9 % among adults[62]. TCM has been widely used in China, providing additional benefits such as ameliorating glycemic control, improving insulin resistance and pancreatic islet function, inducing weight loss, and low incidence of adverse events[63,64]. Jinlida, a CHM approved by the China food and drug administration, has been clinically used in China as an anti-diabetic agent. It is a multi-targeted hypoglycemic medication consisting of Danshensu sodium salt, puerarin, salvianolic acid B, epimedin B, epimedin C, icariin, and ginsenosides Rb1, Rc, and Rb2[64]. Evidence from pharmacological and basic research has demonstrated its function, including protecting islet β-cells, anti-oxidative stress, regulating blood glucose-related hormones, and protecting vascular endothelial cells[65]. The use of CHM to treat chronic diseases including diabetes and hypertension was shown in fig. 1. Several clinical studies have been conducted in China to assess the efficacy of Jinlida for T2D treatment[64,66,67].
The Role of Telemedicine in Chronic Diseases
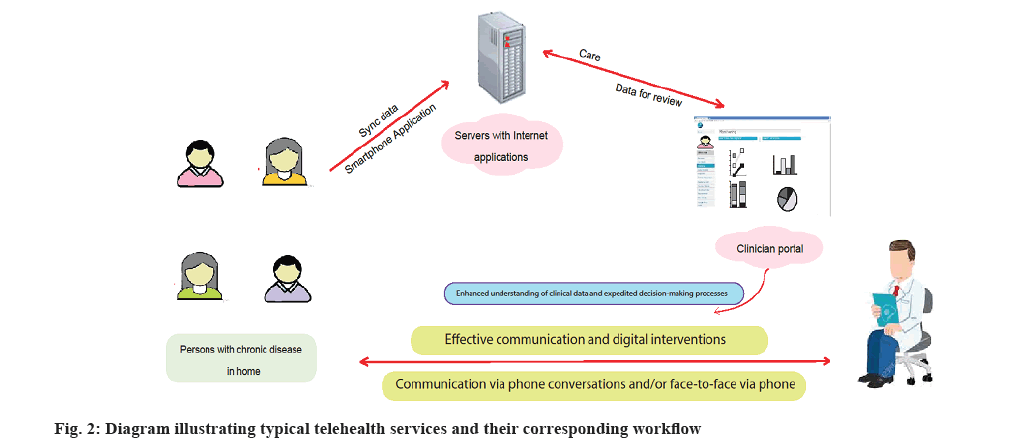
Telemedicine represents a significant breakthrough in the field of managing chronic diseases. It brings about a fundamental change inpatient engagement, access to healthcare, and the continuous delivery of care[6]. Telemedicine involves the use of technology to provide clinical services from a distance. These services include patient consultations through video conferencing, remote monitoring of vital signs, easy access to electronic health records, and communication through mobile health applications[68]. Telemedicine, which refers to the use of technology for delivering healthcare services remotely, has seen a considerable increase in popularity in recent times (fig. 2).
Accessibility and continuity of care:
Access to specialized healthcare services can be a challenge for patients with chronic diseases, especially those in remote or underprivileged areas. Telemedicine seeks to tackle this issue by enabling patients to receive care at their convenience, enhancing the continuity of care. Patients with chronic conditions need regular monitoring and adjustments to their treatment plans, which can be facilitated by telemedicine platforms. This eliminates the need for frequent travel, saving them from inconveniences and expenses[69].
Remote Patient Monitoring (RPM):
RPM is a crucial aspect of telemedicine because it allows for the ongoing monitoring of a patient’s health data overtime. This is particularly valuable when it comes to chronic diseases, as RPM has the potential to significantly enhance health outcomes by enabling the early detection of complications and allowing for prompt intervention. To illustrate, RPM for diabetic patients permits continuous glucose monitoring, which provides timely information for making insulin adjustments[70,71].
Self-management and education:
Telemedicine enables patients to receive education and training on self-management techniques that are crucial for effectively managing chronic diseases. Digital platforms provide resources such as medication reminders, dietary guidelines, and exercise protocols that are tailored to meet the individual needs of each patient. Consequently, this foster increased self-efficacy and improved adherence to treatment regimens[69,71].
Enhanced communication and patient engagement:
Telemedicine facilitates improved communication between patients and healthcare providers, as it offers platforms such as secure messaging, email, and video conferencing. These channels allow patients to ask questions, report symptoms, and receive immediate feedback. This is especially beneficial for managing chronic conditions that require continuous monitoring[72]. By utilizing these communication channels, patients become actively engaged in their own care, which leads to higher levels of patient satisfaction and involvement[73].
Cost-effectiveness:
A growing body of evidence supports the cost-effectiveness of telemedicine in managing chronic diseases. By reducing the need for in-person visits, telemedicine has proven its ability to lower healthcare costs for both providers and patients. One significant advantage of telemedicine is the reduction in hospital readmissions, which is a common issue among patients with chronic diseases. This further contributes to the cost-saving benefits of telemedicine[74].
Quality of life improvements:
Telemedicine has been associated with enhanced quality of life for patients suffering from chronic diseases. Through the provision of responsive and personalized care, patients frequently encounter improved symptom management, decreased rates of depression related to chronic illnesses, and an increased sense of autonomy over their health[75].
Integration with traditional healthcare:
To ensure optimal management of chronic diseases, it is imperative to have a seamless integration between telemedicine and traditional healthcare services. This integration requires the development of hybrid care models, where telemedicine acts as a complement to in-person care. This guarantees that patients have access to the appropriate level of care when needed. Equally important is the training of healthcare providers to effectively operate within these models, enabling the delivery of high-quality telemedicine services[76].
In conclusion, telemedicine has become an essential part of managing chronic diseases. It offers many benefits, such as improved accessibility, increased patient engagement, cost-effectiveness, and an overall better quality of life. Although there are still challenges to overcome, particularly in terms of policy and integration, the future looks promising thanks to the development of new technologies and ongoing research that supports the expansion of telemedicine services.
Integrating CHM and Telemedicine
Telemedicine refers to the use of electronic information and communication technology to improve healthcare delivery when individuals are physically separated. Online healthcare services cover a wide range of functions, such as medical consultations, disease diagnosis, prescription of medication, and management of chronic conditions[8]. It is important to note that regulations, laws, and Medicaid program policies regarding telehealth vary greatly across different states in the United States. Additionally, many countries within the European Union do not have an official definition for telemedicine services[77]. In Southwest England, an online consultation system has been implemented to enable adult patients to communicate with their primary care physicians[78]. However, available evidence suggests that the adoption of e-consultations remains relatively low[79]. Contrary to developed nations, telehealth has the potential to significantly impact developing countries, where limited medical resources and suboptimal healthcare services are prevalent challenges. In response to the global pandemic of the novel coronavirus, many countries have expanded access to telemedicine to maintain essential medical care when face-to-face visits are unsafe. While there has been considerable attention paid to the accelerated growth of telemedicine services in the United States and other high-income countries, the telemedicine revolution may have an even greater benefit in terms of improving healthcare access for vulnerable and geographically remote patients[80,81]. Patients with chronic NCDs such as hypertension, diabetes, or COPD require more control and treatment support[1]. Consequently, patients with chronic diseases residing in rural areas must travel long distances at significant out-of-pocket costs to reach the nearest healthcare facility. In some challenging circumstances, such as the covid-19 pandemic, face-to-face clinical care is often limited. The imposition of government-mandated travel restrictions, the pressure on infection control measures at the center and the advice to people with chronic illness to reduce contact with others may exacerbate chronic conditions, precipitate acute complications, and thereby increase stress on already overburdened hospitals. This is particularly the case when there is a postponement of outpatient clinic visits and prescription renewals.
The rise of telemedicine-promoting policies and the widespread availability of mobile phone access in numerous Low-and Middle-Income Countries (LMICs) have opened new avenues for utilizing telemedicine to address gaps in care for chronic medical conditions[82]. Telemedicine offers the potential to overcome longstanding challenges in primary health care, including a shortage of skilled healthcare professionals, difficulties inpatient transportation, and the financial burden of in-person care. To ensure the successful implementation or expansion of telemedicine services, a systematic approach is needed that ensures secure and equitable access to essential chronic disease care[83].
Previous research has shown that telemedicine has the potential to incorporate complementary, alternative, and integrative medicine, which aligns with cultural values and ancestral knowledge[76]. Chinese medicine health management combines TCM principles with contemporary health management theories and methods. This is achieved through TCM health counseling for both healthy individuals and patient groups, with the aim of managing risk factors associated with diseases comprehensively. Various approaches are used to promote disease prevention and healthcare, with a specific focus on disease management[84]. The proactive approach to managing health before and during the development process aligns with the illness prevention philosophy of Chinese medicine healthcare. The use of telemedicine to deliver CHM has the potential to improve access to CHM practices for individuals in remote areas or facing accessibility challenges. Increased accessibility to CHM through telemedicine can enhance clinical outcomes, reduce patient healthcare use, and improve patient satisfaction with mental health and chronic disease management[76,85]. By integrating CHM and telemedicine, a more comprehensive and patient-centered approach to managing chronic diseases can be implemented. Therefore, it is important to explore how telemedicine is used within the context of CHM, especially as CHM continues to be incorporated into treatment plans and telemedicine is increasingly utilized to extend healthcare services to remote and rural communities as shown in Table 2[86-89].
| Author | Population | Herbal medicine | Study type | Samples size | Goals of study | Results |
|---|---|---|---|---|---|---|
| Kim et al.[86] | COVID-19 patients who received at least one telemedicine session | 4552 herbal medicines were prescribed/among which 30 % were Qing-Fei-Pai-Du-tang | Retrospective review | 1742 patients | Introduce the KM telemedicine center for treatment of COVID-19 patients in Korea | Telemedicine care also has shown that even with patient's residence transition, medical care can be continued without pause |
| Jang et al.[87] | COVID-19 patients participated in and completed the KM telemedicine program | Kyung-Ok-Ko and Qingfei Paidu decoction herbal medicine, prescribed | Observational | 2324 patients | Describe the results of the KM telemedicine center and the clinical possibility of using herbal medicines for COVID-19 | All COVID19-related symptoms improved after treatment |
| Jang et al.[88] | COVID-19 patients who had completed two consultations | CHM | Retrospective case-controlled | 311 patients | Evaluate the effectiveness of CHM using data extracted from the Hong Kong Baptist University Telemedicine Chinese Medicine Center database | CHM treatment significantly reduced the total score of individual symptoms and the number of reported symptoms |
| He et al.[89] | Participants who requested telemedicine consultation and medication at rural sanitary stations | CHM | Retrospective and descriptive study | 22740 participants | The objective was to describe the effectiveness and challenges of telemedicine for providing health care from Guangzhou to rural areas in Guangdong Province | It saves costs, has high patient satisfaction and price acceptability, and can relieve disease and syndromes. |
Note: KM: Korean Medicine
Table 2: Several studies have examined the combination of CHM and telemedicine.
Challenges and Considerations
The integration of CHM with telemedicine in the management of chronic diseases represents a unique blend of traditional knowledge and modern technological advancements. This approach has significant potential for enhancing patient care and accessibility. However, it also presents several challenges and considerations that need to be carefully addressed to ensure effectiveness, safety, and scientific validation.
One of the main challenges in integrating CHM into telemedicine is the standardization of herbal formulations. Unlike conventional pharmaceuticals, herbal medicines are derived from natural sources and therefore show inherent variability in their composition[90]. The concentration of bioactive compounds can vary considerably depending on factors such as source, harvest time, and preparation method[91]. Ensuring consistent quality and therapeutic effects across batches is crucial, which requires rigorous standardization protocols and quality control measures in the supply chain[92].
The pharmacological complexity of CHM, which is known for its extensive use of multi-ingredient formulations, poses a considerable challenge in comprehending the neuro-biochemical mechanisms that underlie its therapeutic effects[93]. The interaction among various herbal components can lead to synergistic, antagonistic, or additive effects that are not yet fully understood. Consequently, advanced analytical methods and bioinformatics tools are essential for unraveling the intricate interactions at the molecular level[93,94].
Patients with chronic conditions often take multiple medications, which raises concerns about potential interactions between drugs and herbal medicine when traditional CHM is introduced[95]. These interactions can affect how conventional drugs are absorbed, distributed, metabolized and excreted, as well as their effects on the body[95]. This can result in reduced effectiveness of the drugs or increased risk of side effects. To identify and manage these risks, it is necessary to use comprehensive electronic health records integrated with telemedicine platforms. Healthcare providers should have expertise in both conventional pharmacology and herbal medicine to effectively provide care in these situations[96].
Despite CHM's long historical use, there is still a need for substantial clinical evidence to support its effectiveness and safety in treating chronic diseases[97]. High-quality randomized controlled trials and meta-analyses play a critical role in validating the therapeutic claims of CHM and guiding clinical practice[98]. However, conducting such studies can be challenging due to the personalized nature of herbal prescriptions in CHM, which differs from the standardized treatment protocols used in conventional clinical trials[97-102].
The regulatory framework for CHM varies significantly across jurisdictions, resulting in a complex landscape for telemedicine services that may extend beyond national borders. Ensuring compliance with diverse regulations regarding the practice of herbal medicine, telehealth consultations, and cross-border medicine delivery presents a significant challenge. Moreover, it is crucial to carefully address legal considerations about to practitioner licensing, patient privacy, and data security to maintain trust and protect stakeholders. Integrating Complementary and Alternative Medicine (CHM) with telemedicine also involves overcoming cultural and educational barriers. Healthcare providers must receive adequate training to comprehend and effectively convey the principles of CHM to patients from diverse cultural backgrounds. Likewise, patients should be educated about the underlying reasons, potential benefits, and limitations of CHM, enabling them to make informed decisions about their healthcare.
The technological integration of CHM into telemedicine platforms necessitates the development of specialized software and databases to support the unique aspects of herbal medicine, such as personalized formulation and dosage adjustments. Ensuring interoperability with existing healthcare IT systems, while maintaining scalability and user-friendliness, represents a significant technical challenge. Finally, the integration of CHM and telemedicine must be approached with ethical considerations at the forefront. Issues such as informed consent, respect for patient autonomy, and equitable access to care are of paramount importance. It is crucial to actively mitigate the potential for health disparities to arise due to differential access to technology. In summary, the synergistic approach to chronic disease care via the integration of CHM and telemedicine is laden with challenges that require concerted efforts from researchers, clinicians, technologists, and policymakers. To fully realize the potential of this integrative healthcare model, it is essential to address the challenges through interdisciplinary collaboration and robust scientific inquiry.
Conclusion
Chronic disease management can benefit from the integration of CHM and telemedicine. This holistic approach combines the individualized and natural remedies of CHM with the convenience and accessibility of telemedicine, ultimately improving patient outcomes and enhancing the quality of care. As healthcare systems continue to evolve, bridging the gap between traditional and modern medicine approaches is a promising avenue for tackling the growing burden of chronic diseases.
Authors’ contributions:
Shue Wang and Yunpeng Li were involved in study design and article writing, Shue Wang and Jiazhong Sun were involved in article writing and final revision, and Shue Wang gave consent for the final version of the manuscript.
Conflict of interests:
The authors declared no conflict of interests.
References
- Chujie C, Huafeng P. Guangzhou city community health services utilization actuality and user demand for medical services in the analysis. Chin Gen Pract 2010;13:1742-4.
- Zhifang Z, Qing G. Research progress on the integration of disease and health management in traditional Chinese medicine. J Zhejiang Tradit Chin Med 2013;48:386-7.
- Fan X, Meng F, Wang D, Guo Q, Ji Z, Yang L, et al. Perceptions of traditional Chinese medicine for chronic disease care and prevention: A cross-sectional study of Chinese hospital-based health care professionals. BMC Complement Altern Med 2018;18:1-0.
[Crossref] [Google Scholar] [PubMed]
- State Administration of Traditional Chinese Medicine of the People’s Republic of China; 2017.
- Hua C, Conghua J. Preventing health care practitioners from preventive service for Chinese medicine investigation and analysis of current situation cognition. J Tradit Chin Med Manag 2009;17:906-9.
- Viswanathan M, Golin CE, Jones CD, Ashok M, Blalock SJ, Wines RCM, et al. Interventions to improve adherence to self-administered medications for chronic diseases in the United States: A systematic review. Ann Intern Med 2012;157:785–95.
- Burkhart PV, Sabate E. Adherence to long-term therapies: Evidence for action. J Nurs Scholar 2003;35:207.
- Choudhry NK, Dugani S, Shrank WH, Polinski JM, Stark CE, Gupta R, et al. Despite increased use and sales of statins in India, per capita prescription rates remain far below high-income countries. Health Aff 2014;33:273-82.
[Crossref] [Google Scholar] [PubMed]
- Beaglehole R, Epping-Jordan J, Patel V, Chopra M, Ebrahim S, Kidd M, et al. Improving the prevention and management of chronic disease in low-income and middle-income countries: A priority for primary health care. Lancet 2008;372:940-9.
[Crossref] [Google Scholar] [PubMed]
- . Zhang Y, Xie Z, Liu X, Fan C. The analysis of the influence factors on selecting hospital. Med Soc 2010;23:71-3.
[Crossref] [Google Scholar] [PubMed]
- Panahiazar M, Taslimitehrani V, Jadhav A, Pathak J. Empowering personalized medicine with big data and semantic web technology: Promises, challenges, and use cases. Proc IEEE Int Conf Big Data 2014;2014:790–5.
- Kong L. Healthy China: Mission and responsibility. Capital Public Health 2019;13(3):113-4.
- Xiong Z. Challenges and countermeasures of chronic disease prevention and control in China. Chin J Chron Dis Prev Control 2019;27(9):720-1.
- National Center for Cardiovascular Disease. Cardiovascular Disease Report in China 2018. Beijing, China: Encyclopedia China Press; 2018. p. 1-224.
- Task Force on Chinese Guidelines for the Prevention of Cardiovascular Diseases (2017), Editorial Board of Chinese Journal of Cardiology. Chinese guidelines for the prevention of cardiovascular diseases (2017). Zhonghua Xin Xue Guan Bing Za Zhi 2018;46:10-25
[PubMed]
- Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: A systematic review and meta-analysis. Lancet Diabetes Endocrinol 2018;6:41-50.
[Crossref] [Google Scholar] [PubMed]
- Revision Committee of Chinese Guidelines for Hypertension Prevention and Control. The 2018 revision of China’s hypertension prevention and treatment guidelines. Prevention and treatment of cardiovascular and cerebrovascular diseases 2019;19(1):6-49.
- Egan BM, Li J, Davis RA, Fiscella KA, Tobin JN, Jones DW, et al. Differences in primary cardiovascular disease prevention between the 2013 and 2016 cholesterol guidelines and impact of the 2017 hypertension guideline in the United States. J Clin Hypertens (Greenwich) 2018;20:991-1000.
[Crossref] [Google Scholar] [PubMed]
- GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1459-544.
- Sun H, Wang W. A Nationwide epidemiological sample survey on cerebrovascular disease in China. Chin J Mod Neurol Dis 2018;18(2):83-8.
- Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, incidence, and mortality of stroke in China: Results from a Nationwide population-based survey of 480 687 adults. Circulation 2017;135:759-71.
[Crossref] [Google Scholar] [PubMed]
- Weiwei C, Hui S, Liyuan MA. Epidemiology and prevention of cardiovascular and cerebrovascular diseases in China. J Cardiovasc Cerebrovasc Dis Prev 2016;16(2):79-83.
- Shilian H, Jing W, Cui C, Xinchun W. Analysis of epidemiological trends in chronic diseases of Chinese residents. Aging Med (Milton) 2020;3:226-33.
[Crossref] [Google Scholar] [PubMed]
- GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med 2017;5:691-706.
[Crossref] [Google Scholar] [PubMed]
- Wang C, Xu J, Yang L, Xu Y, Zhang X, Bai C, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health (CPH) study): A national cross-sectional study Lancet 2018;391:1706-17.
[Crossref] [Google Scholar] [PubMed]
- Chinese Expert Consensus Writing Group on Anti-Infective Therapy for Acute Exacerbation of Chronic Obstructive Pulmonary Disease. Chinese expert consensus on anti-infective therapy for acute exacerbation of chronic obstructive pulmonary disease. Int J Respir 2019;39(17):1281-96.
- Qiu C, Wang F, Chen R. Promoting the implementation of the action plan for the prevention and treatment of chronic respiratory diseases in healthy China. Chin J Med 2019;99(48):3761-4.
- Wang S, Zhu Y, Li G. Meta-analysis and comparison of the prevalence of chronic kidney disease in Chinese adults. Chin J Kidney Dis 2018;34(8):579-86.
- Normile D. Asian medicine. The new face of traditional Chinese medicine. Science 2003;299:188-90.
[Crossref] [Google Scholar] [PubMed]
- Li Z, Xu C. The fundamental theory of traditional Chinese medicine and the consideration in its research strategy. Front Med 2011;5:208-11.
[Crossref] [Google Scholar] [PubMed]
- Gu S, Pei J. Chinese herbal medicine meets biological networks of complex diseases: A computational perspective. Evid Based Complement Alternat Med 2017;2017:7198645.
[Crossref] [Google Scholar] [PubMed]
- Neill US. From branch to bedside: Youyou Tu is awarded the 2011 Lasker~DeBakey Clinical Medical Research Award for discovering artemisinin as a treatment for malaria. J Clin Invest 2011;121:3768-73.
- Su XZ, Miller LH. The discovery of artemisinin and the Nobel prize in physiology or medicine. Sci China Life Sci 2015;58(11):1175-9.
[Crossref] [Google Scholar] [PubMed]
- Gu S, Pei J. Innovating Chinese herbal medicine: From traditional health practice to scientific drug discovery. Front Pharmacol 2017;8:381.
[Crossref] [Google Scholar] [PubMed]
- Xie T, Song S, Li S, Ouyang L, Xia L, Huang J. Review of natural product databases. Cell Proliferation 2015;48(4):398-404.
- Feng Y, Wu Z, Zhou X, Zhou Z, Fan W. Knowledge discovery in traditional Chinese medicine: State of the art and perspectives. Artif Intell Med 2006;38(3):219-36.
[Crossref] [Google Scholar] [PubMed]
- Gu S, Yin N, Pei J, Lai L. Understanding traditional Chinese medicine anti-inflammatory herbal formulae by simulating their regulatory functions in the human arachidonic acid metabolic network. Mol BioSystems 2013;9(7):1931-8.
- Chang KW, Tsai TY, Chen KC, Yang SC, Huang HJ, Chang TT, et al. iSMART: An integrated cloud computing web server for traditional Chinese medicine for online virtual screening, de novo evolution and drug design. J Biomol Struct Dyn 2011;29(1):243-50.
[Crossref] [Google Scholar] [PubMed]
- Liang H, Ruan H, Ouyang Q, Lai L. Herb-target interaction network analysis helps to disclose molecular mechanism of traditional Chinese medicine. Sci Rep 2016;6(1):36767.
- Gu S, Yin N, Pei J, Lai L. Understanding molecular mechanisms of traditional Chinese medicine for the treatment of influenza viruses infection by computational approaches. Mol BioSystems 2013;9(11):2696-700.
- Li J, Lu C, Jiang M, Niu X, Guo H, Li L, et al. Traditional chinese medicine-based network pharmacology could lead to new multicompound drug discovery. Evid Based Complement Altern Med 2012;2012:149762.
[Crossref] [Google Scholar] [PubMed]
- World Health Organization. Hypertension; 2023.
- Huang K, Song YT, He YH, Feng XL. Health system strengthening and hypertension management in China. Global Health Res Policy 2016;1:13.
[Crossref] [Google Scholar] [PubMed]
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA 2003;289(19):2560-71.
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360(9349):1903-13.
[Crossref] [Google Scholar] [PubMed]
- Joint Committee for Guideline Revision. 2018 Chinese guidelines for prevention and treatment of hypertension-a report of the revision committee of Chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol 2019;16:182-241.
- Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 international society of hypertension global hypertension practice guidelines. Hypertension 2020;75(6):1334-57.
[Crossref] [Google Scholar] [PubMed]
- Yach D, Hawkes C, Gould CL, Hofman KJ. The global burden of chronic diseases: Overcoming impediments to prevention and control. JAMA 2004;291(21):2616-22.
[Crossref] [Google Scholar] [PubMed]
- Redon J, Mourad JJ, Schmieder RE, Volpe M, Weiss TW. Why in 2016 are patients with hypertension not 100 % controlled? A call to action. J Hypertension 2016;34(8):1480-8.
[Crossref] [Google Scholar] [PubMed]
- Shi WJ, Zhang YX, Xu GP, Ma QJ, Qin JH, Wu XH, et al. Extracorporeal membrane oxygenation-assisted percutaneous coronary intervention in extremely high-risk patients. Chin Med J 2018;131(13):1625-7.
[Crossref] [Google Scholar] [PubMed]
- Ozemek C, Laddu DR, Arena R, Lavie CJ. The role of diet for prevention and management of hypertension. Curr Opin Cardiol 2018;33(4):388-93.
[Crossref] [Google Scholar] [PubMed]
- Ozemek C, Tiwari S, Sabbahi A, Carbone S, Lavie CJ. Impact of therapeutic lifestyle changes in resistant hypertension. Prog Cardiovasc Dis 2020;63(1):4-9.
[Crossref] [Google Scholar] [PubMed]
- Ren W, Wang M, Liao J, Li L, Yang D, Yao R, et al. The effect of Chinese herbal medicine combined with western medicine on vascular endothelial function in patients with hypertension: A systematic review and meta-analysis of randomized controlled trials. Front Pharmacol 2020;11:823.
[Crossref] [Google Scholar] [PubMed]
- Tai J, Zou J, Zhang X, Wang Y, Liang Y, Guo D, et al. Randomized controlled trials of Tianma Gouteng decoction combined with nifedipine in the treatment of primary hypertension: A systematic review and meta-analysis. Evid Based Complement Altern Med 2020;2020:5759083.
[Crossref] [Google Scholar] [PubMed]
- Wang Y, Xu X, Pan M, Jin T. ELMO1 directly interacts with Gβγ subunit to transduce GPCR signaling to Rac1 activation in chemotaxis. J Cancer 2016;7(8):973.
[Crossref] [Google Scholar] [PubMed]
- Xiong X, Wang P, Duan L, Liu W, Chu F, Li S, et al. Efficacy and safety of Chinese herbal medicine Xiao Yao San in hypertension: A systematic review and meta-analysis. Phytomedicine 2019;61:152849.
[Crossref] [Google Scholar] [PubMed]
- Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA 2017;317(24):2515-23.
[Crossref] [Google Scholar] [PubMed]
- Liu Y, Song A, Zang S, Wang C, Song G, Li X, et al. Jinlida reduces insulin resistance and ameliorates liver oxidative stress in high-fat fed rats. J Ethnopharmacol 2015;162:244-52.
[Crossref] [Google Scholar] [PubMed]
- Pang J, Liang J, Wang Z, Wei C, Gao HL. Intervention and mechanism of Jinlida combined with Tongxinluo on high glucose-induced islet microvascular endothelial cell injury. Chin Pharmacol Bull 2015;31:430.
- Wang D, Tian M, Qi Y, Chen G, Xu L, Zou X, et al. Jinlida granule inhibits palmitic acid induced-intracellular lipid accumulation and enhances autophagy in NIT-1 pancreatic β cells through AMPK activation. J Ethnopharmacol 2015;161:99-107.
[Crossref] [Google Scholar] [PubMed]
- Jia W, Weng J, Zhu D, Ji L, Lu J, Zhou Z, et al. Standards of medical care for type 2 diabetes in China 2019. Diabetes Metab Res Rev 2019;35(6):e3158.
[Crossref] [Google Scholar] [PubMed]
- Jin D, Hou L, Han S, Chang L, Gao H, Zhao Y, et al. Basis and design of a randomized clinical trial to evaluate the effect of Jinlida granules on metabolic syndrome in patients with abnormal glucose metabolism. Front Endocrinol 2020;11:415.
- Shi YL, Liu WJ, Zhang XF, Su WJ, Chen NN, Lu SH, et al. Effect of Chinese herbal medicine Jinlida granule in treatment of patients with impaired glucose tolerance. Chin Med J 2016;129(19):2281-6.
[Crossref] [Google Scholar] [PubMed]
- Xing TJ, Mei LF, Bo YL, Lin TX. Evaluation of the Chinese herbal medicine Jinlida in type 2 diabetes patients based on stratification: Results of subgroup analysis from a 12-week trial. J Diabetes 2018;10(2):112-20.
[Crossref] [Google Scholar] [PubMed]
- Zhang Y, Wang W, Ning G. Study on the efficacy and safety of Jinlida in patients with inadequately controlled type-2 diabetes and dyslipidemia under life style intervention (Enjoy Life Study). J Diabetes 2015;7(2):268-9.
[Crossref] [Google Scholar] [PubMed]
- Lian F, Tian J, Chen X, Li Z, Piao C, Guo J, et al. The efficacy and safety of Chinese herbal medicine Jinlida as add-on medication in type 2 diabetes patients ineffectively managed by metformin monotherapy: A double-blind, randomized, placebo-controlled, multicenter trial. PLoS One 2015;10(6):e0130550.
[Crossref] [Google Scholar] [PubMed]
- Ceriello A, Monnier L, Owens D. Glycaemic variability in diabetes: Clinical and therapeutic implications. Lancet Diabetes Endocrinol 2019;7(3):221-30.
[Crossref] [Google Scholar] [PubMed]
- Frontoni S, di Bartolo P, Avogaro A, Bosi E, Paolisso G, Ceriello A. Glucose variability: An emerging target for the treatment of diabetes mellitus. Diabetes Res Clin Pract 2013;102(2):86-95.
[Crossref] [Google Scholar] [PubMed]
- Pan J, Xu Y, Chen S, Tu Y, Mo Y, Gao F, et al. The effectiveness of traditional Chinese medicine Jinlida granules on glycemic variability in newly diagnosed type 2 diabetes: A double-blinded, randomized trial. J Diabetes Res 2021;2021:6303063.
[Crossref] [Google Scholar] [PubMed]
- Colagiuri S. Optimal management of type 2 diabetes: The evidence. Diabetes Obesity Metab 2012;14:3-8.
[Crossref] [Google Scholar] [PubMed]
- Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, et al. National standards for diabetes self-management education. Diabetes Care 2009;32(1):87-94.
- Grady PA, Gough LL. Self-management: A comprehensive approach to management of chronic conditions. Am J Public Health 2014;104(8):25-31.
[Crossref] [Google Scholar] [PubMed]
- Zhao FF, Suhonen R, Koskinen S, Leino-Kilpi H. Theory-based self-management educational interventions on patients with type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. J Adv Nurs 2017;73(4):812-33.
[Crossref] [Google Scholar] [PubMed]
- Adu MD, Malabu UH, Callander EJ, Malau-Aduli AE, Malau-Aduli BS. Considerations for the development of mobile phone apps to support diabetes self-management: Systematic review. JMIR Mhealth Uhealth 2018;6(6):e10115.
[Crossref] [Google Scholar] [PubMed]
- Fu H, McMahon SK, Gross CR, Adam TJ, Wyman JF. Usability and clinical efficacy of diabetes mobile applications for adults with type 2 diabetes: A systematic review. Diabetes Res Clin Pract 2017;131:70-81.
[Crossref] [Google Scholar] [PubMed]
- Pfammatter AF, Mitsos A, Wang S, Hood SH, Spring B. Evaluating and improving recruitment and retention in an mHealth clinical trial: An example of iterating methods during a trial. Mhealth 2017;3:49.
[Crossref] [Google Scholar] [PubMed]
- Fleming T, Bavin L, Lucassen M, Stasiak K, Hopkins S, Merry S. Beyond the trial: Systematic review of real-world uptake and engagement with digital self-help interventions for depression, low mood, or anxiety. J Med Internet Res 2018;20(6):e199.
[Crossref] [Google Scholar] [PubMed]
- Wang Y, Xue H, Huang Y, Huang L, Zhang D. A systematic review of application and effectiveness of mHealth interventions for obesity and diabetes treatment and self-management. Adv Nutr 2017;8(3):449-62.
[Crossref] [Google Scholar] [PubMed]
- Helander E, Kaipainen K, Korhonen I, Wansink B. Factors related to sustained use of a free mobile app for dietary self-monitoring with photography and peer feedback: Retrospective cohort study. J Med Internet Res 2014;16(4):e3084.
[Crossref] [Google Scholar] [PubMed]
- National Health Commission of the People’s Republic of China and Pharmaceutical Administration. Notice on the issuance of three documents including the Administrative Measures for Internet Diagnosis and Treatment; 2018.
- Center for Connected Health Policy. Oakland, CA: Public Health Institute. State Telehealth Laws and Reimbursement Policies; 2023.
- Sara C, Alfredo R, Ana E, Carla P, Diogo M, LM. EU state of play on telemedicine services and uptake recommendations. Europe: Joint Action to support the eHealth Network; 2017;87.
- Edwards HB, Marques E, Hollingworth W, Horwood J, Farr M, Bernard E, et al. Use of a primary care online consultation system, by whom, when and why: Evaluation of a pilot observational study in 36 general practices in South West England. BMJ Open 2017;7(11):e016901.
[Crossref] [Google Scholar] [PubMed]
- Scott RE, Mars M. Telehealth in the developing world: Current status and future prospects. Smart Homecare Technold TeleHealth 2015;2015(3):25-37.
- Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med 2020;382(18):1679-81.
[Crossref] [Google Scholar] [PubMed]
- Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: A call to action. JMIR Public Health Surveill 2020;6(2):e18810.
[Crossref] [Google Scholar] [PubMed]
- Centers for disease control and prevention. People who are at higher risk for severe illness; 2020.
- Cash R, Patel V. Has COVID-19 subverted global health? Lancet 2020;395(10238):1687-8.
[Crossref] [Google Scholar] [PubMed]
- Resolve to save lives. Leveraging technology to improve health care during the COVID-19 pandemic and beyond; 2020.
- Kamsu-Foguem B, Foguem C. Could telemedicine enhance traditional medicine practices? Eur Res Telemed 2014;3(3):117-23.
- Niles BL, Klunk-Gillis J, Ryngala DJ, Silberbogen AK, Paysnick A, Wolf EJ. Comparing mindfulness and psychoeducation treatments for combat-related PTSD using a telehealth approach. Psychol Trauma 2012;4(5):538.
- Der-Martirosian C, Shin M, Upham ML, Douglas JH, Zeliadt SB, Taylor SL. Telehealth complementary and integrative health therapies during COVID-19 at the US department of veterans affairs. Telemed e-Health 2023;29(4):576-83.
[Crossref] [Google Scholar] [PubMed]
- Yu M, He S, Wu D, Zhu H, Webster C. Examining the multi-scalar unevenness of high-quality healthcare resources distribution in China. Int J Environ Res Public Health 2019;16(16):2813.
[Crossref] [Google Scholar] [PubMed]
- National Health Commission of the People’s Republic of China. China Health Statistics Yearbook 2020. Beijing, China: Peking Union Medical College Press; 2020.
- Wu D, Hesketh T, Shu H, Lian W, Tang W, Tian J. Description of an online hospital platform, China. Bull World Health Organ 2019;97(8):578.
[Crossref] [Google Scholar] [PubMed]
- Feng XL, Martinez-Alvarez M, Zhong J, Xu J, Yuan B, Meng Q, et al. Extending access to essential services against constraints: The three-tier health service delivery system in rural China (1949-1980). Int J Equity Health 2017;16(1):49.
[Crossref] [Google Scholar] [PubMed]
- Gong P, Liang S, Carlton EJ, Jiang Q, Wu J, Wang L, et al. Urbanisation and health in China. Lancet 2012;379(9818):843-52.
[Crossref] [Google Scholar] [PubMed]
- Li X, Krumholz HM, Yip W, Cheng KK, de Maeseneer J, Meng Q, et al. Quality of primary health care in China: Challenges and recommendations. Lancet 2020;395(10239):1802-12.
[Crossref] [Google Scholar] [PubMed]
- Yuan S, Wang F, Li X, Jia M, Tian M. Facilitators and barriers to implement the family doctor contracting services in China: Findings from a qualitative study. BMJ Open 2019;9(10):e032444.
[Crossref] [Google Scholar] [PubMed]
- Shang X, Huang Y, Li BE, Yang Q, Zhao Y, Wang W, et al. Residents’ awareness of family doctor contract services, status of contract with a family doctor, and contract service needs in Zhejiang Province, China: A cross-sectional study. Int J Environ Res Public Health 2019;16(18):3312.
[Crossref] [Google Scholar] [PubMed]
- Meyerowitz-Katz G, Ravi S, Arnolda L, Feng X, Maberly G, Astell-Burt T. Rates of attrition and dropout in app-based interventions for chronic disease: Systematic review and meta-analysis. J Med Internet Res 2020;22(9):e20283.
[Crossref] [Google Scholar] [PubMed]
- Perez MV, Mahaffey KW, Hedlin H, Rumsfeld JS, Garcia A, Ferris T, et al. Large-scale assessment of a smartwatch to identify atrial fibrillation. N Engl J Med 2019;381(20):1909-17.
[Crossref] [Google Scholar] [PubMed]