- *Corresponding Author:
- Jingjing Liu
Department of Anesthesiology, Hubei Hanchuan People's Hospital, Hanchuan, Hubei 431600, China
E-mail: liujingjing5353@sina.com
| This article was originally published in a special issue, “Innovations in Biomedical Research and Drug Development” |
| Indian J Pharm Sci 2023:85(3) Spl Issue “155-161” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the safety and changes of hemodynamic profiles when using etomidate for general anesthesia in laparoscopic cholecystectomy compared to propofol was the objective of the study. Adult patients who received laparoscopic cholecystectomy were retrospectively categorized as etomidate and propofol group. Time to extubation, time to eye opening, pain scores at rest, postoperative nausea, vomiting and lengths of hospital stay were studied as safety outcomes. Changes in hemodynamic profiles are evaluated by coefficients of variation of systolic blood pressure, diastolic blood pressure, mean arterial pressure and heart rates were compared between groups. 291 patients were categorized as the etomidate group and 388 patients as the propofol group. There was no significant difference in age, sex, body mass index and hemodynamic profiles at baseline between the two groups (p all>0.05). Compared to propofol, the etomidate group showed similar safety outcomes (p all>0.05). Similar change patterns in the hemodynamic profiles over time were observed between the two groups, but the coefficients of variation of systolic blood pressure, diastolic blood pressure and mean arterial pressure in the etomidate group were significantly lower than that in the propofol group (p<0.05). There was no difference in safety outcomes but a more stable hemodynamic profile when comparing intraoperative target-controlled infusion of etomidate to propofol used for general anesthesia in laparoscopic cholecystectomy.
Keywords
General anesthesia, laparoscopic cholecystectomy, etomidate, propofol, hemodynamic profile
Laparoscopic cholecystectomy is a common abdominal surgical procedure performed for gallstone diseases[1,2]. Compared to open cholecystectomy, patients who received laparoscopic cholecystectomy show less postoperative pain, better cosmesis and shorter lengths of hospital stay[3,4], but a higher overall serious complication rate[5,6]. There are directions for further improvement in prognosis of patients receiving laparoscopic cholecystectomy but they are not limited to the development of the surgical techniques[7,8]. Considering the physiological effects of laparoscopy, special anesthetic considerations for laparoscopic cholecystectomy are necessary, especially for the cardiovascular changes during the procedure[9]. Due to intraperitoneal carbon dioxide insufflation and variations in patient positioning, the cardiovascular changes during laparoscopy are variable and dynamic, which is usually well tolerated by healthy patients, but may have a major impact on the cardiorespiratory function in the elderly patients with comorbidities. Several studies have reported significant hemodynamic changes during laparoscopy in patients with severe cardiopulmonary disease including an increase in Mean Arterial Pressure (MAP), Systemic Vascular Resistance (SVR), central venous pressure, a decrease in cardiac output and stroke volume during peritoneal insufflation[10-14]. As a result, more pharmacologic interventions and intensive monitoring are needed in response to such changes.
A variety of inhalation and intravenous anesthetics can be used for induction and maintenance of general anesthesia. Considering the above mentioned cardiovascular changes during laparoscopy, anesthetics with lower impact on hemodynamic profiles of patients may be favored. Propofol and etomidate are the intravenous sedative-hypnotic agents commonly used to induce general anesthesia. Compared to propofol, etomidate is considered as the most hemodynamically neutral of the sedative- hypnotic agents used for induction of general anesthesia, since it has rapid onset of action without any changes in the blood pressure, cardiac output or Heart Rate (HR)[15,16]. However, etomidate has no analgesic effect and shows a higher risk of postoperative nausea and vomiting compared to propofol and may induce transient acute adrenal insufficiency[17,18]. It has been reported that the use of etomidate for general anesthesia in endoscopic retrograde cholangiopancreatography showed a more stable hemodynamic responses compared with propofol[19,20], but this benefit has not been specially investigated in laparoscopic cholecystectomy. Therefore, the study aimed to investigate the safety and change of hemodynamic profiles in patients who received intraoperative target-controlled infusion of etomidate (compared to propofol) for induction and maintenance of general anesthesia in laparoscopic cholecystectomy.
Materials and Methods
Subjects used in the study:
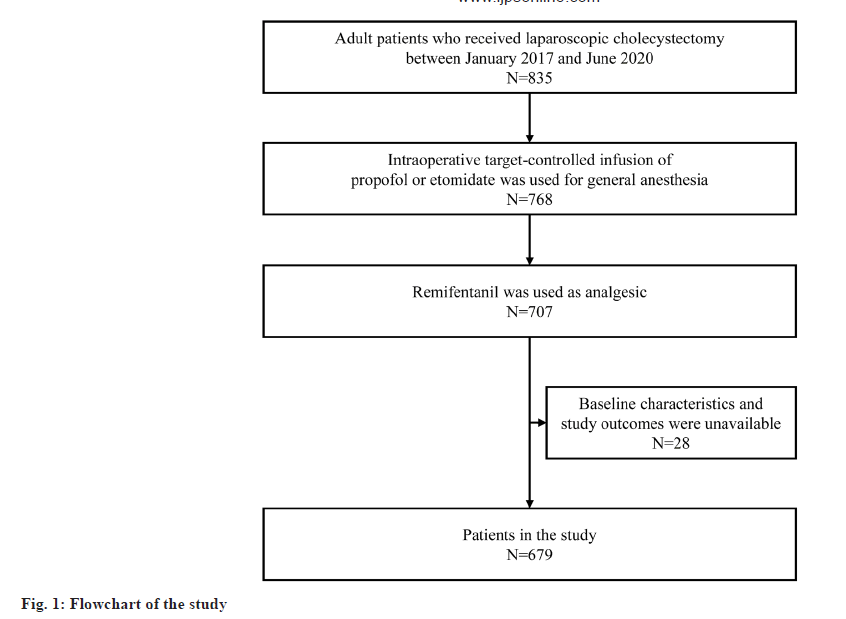
The study retrospectively included consecutive adult patients who received laparoscopic cholecystectomy between January 2017 and June 2020 in Hanchuan People’s Hospital. Data about hospitalization during this period were examined to identify patients who met all the inclusion criteria which includes patients who received laparoscopic cholecystectomy during the hospitalization; age≥18 y; patients who received general anesthesia; propofol or etomidate was used for induction and maintenance of general anesthesia; propofol or etomidate was administered via intraoperative target-controlled infusion and remifentanil was used as analgesic (which was the most commonly used analgesic during the study period).
We excluded patients who met any of the exclusion criteria like patients who received other procedures at the same time; other anesthetics or analgesics were used for general anesthesia; information for the baseline characteristics and study outcomes was unavailable.
The study was approved by the medical ethical committee of Hanchuan People’s Hospital and written informed consent was waived due to the retrospective study design. The study was conducted in accordance with the Declaration of Helsinki.
Methods:
For laparoscopic cholecystectomy performed during the study period in Hanchuan People’s Hospital, propofol was the most frequently used for general anesthesia, but the use of etomidate increased in recent years. The choices of anesthetics were mainly depended on the preference of the anesthetists. Except for the difference in anesthetics, the procedures of anesthesia were similar for patients receiving laparoscopic cholecystectomy. All the patients first received midazolam (0.03 mg/kg) and remifentanil (2 μg/kg), then the patients received intraoperative target-controlled infusion of either etomidate or propofol. The initiate drug concentration was set to 1.0 μg/ml every minute for propofol and increased by 0.3 μg/ml, until the Bispectral Index (BIS) reached 40-60 or set to 0.2 μg/ml for etomidate and increased by 0.1 μg/ml every minute until the BIS reached 40-60. When the consciousness of patients was lost, rocuronium (0.6 mg/kg) was given. After the induction of anesthesia, tracheal intubation was performed and intraoperative target-controlled infusion of either etomidate or propofol was maintained.
Baseline characteristics:
The following variables were extracted as baseline characteristics of the study patients. They are age, sex, Body Mass Index (BMI) and hemodynamic characteristics including Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), MAP and HR at baseline (i.e., T1, namely in wards before the surgery).
Study outcomes:
The following variables were extracted and studied as safety outcomes-The time to extubation, defined as the time from discontinuation of either etomidate or propofol to extubation; The time to eye opening, defined as the time from discontinuation of either etomidate or propofol to spontaneous eye opening; The pain score at rest, defined as the degree of pain assessed by a Visual Analogue Scale (VAS) (0 mm (no pain) to 100 mm (unbearable pain)) when the patients were transferred to the post-anesthesia care unit; postoperative nausea and/or vomiting and lengths of hospital stay.
To investigate the changes of hemodynamic profiles, we further extracted the recorded hemodynamic profiles of SBP, DBP, MAP and HR at the following time points i.e. before anesthesia induction (T2); after tracheal intubation (T3); at the end of surgery (T4). The coefficient of variation of each hemodynamic profile measured at the four time points (T1, T2, T3 and T4) was studied as the change of the hemodynamic metric.
Statistical analysis:
Data were presented as mean±standard deviation for continuous variables or number (percentage) for categorical variables. Comparisons between the two groups (i.e., the etomidate group or the propofol group) were examined by the student’s t-test for continuous variables or the chi-squared test for categorical variables. Coefficient of variation of hemodynamic metric in each group was calculated as follows. First we calculated the ratio of the standard deviation to the mean of each hemodynamic metric of each patient at the four time points, then the mean and standard deviations of the coefficients of variation of patients from the same group (i.e., the etomidate group or the propofol group) was calculated. Statistical analysis was done using Statistical Package for the Social Sciences (SPSS) 22 (IBM SPSS Statistics) and p value<0.05 was considered significant.
Results and Discussion
Baseline characteristics of the study patients were shown in Table 1. A total of 679 patients who received laparoscopic cholecystectomy were included (fig. 1), of which 291 (42.9 %) patients were categorized as the etomidate group and 388 (57.1 %) patients as the propofol group. The average age of the etomidate group was 49.34±10.63 y, which was not significantly different from that of the propofol group (49.44±10.78 y, p=0.909). There was no statistically significant difference in sex (male 55.67 % vs. 58.51 %, p=0.460), BMI (24.64±3.86 vs. 24.37±3.62 kg/ m2, p=0.353) and the studied hemodynamic profiles at baseline between two groups (p>0.05 for all).
| Characteristics | Propofol group (n=388) | Etomidate group (n=291) | p value |
| Age (y) | 49.44±10.78 | 49.34±10.63 | 0.909 |
| Male | 227 (58.51 %) | 162 (55.67 %) | 0.46 |
| BMI (kg/m2) | 24.37±3.62 | 24.64±3.86 | 0.353 |
| SBP at T1 (mmHg) | 122.95±13.22 | 122.80±7.98 | 0.863 |
| DBP at T1 (mmHg) | 79.62±9.18 | 80.27±6.25 | 0.292 |
| MAP at T1 (mmHg) | 94.07±7.53 | 94.44±4.55 | 0.459 |
| HR at T1 (per min) | 94.77±8.81 | 95.57±8.67 | 0.234 |
Note: T1: At baseline (in wards, before the surgery); BMI: Body Mass Index; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; MAP: Mean Arterial Pressure and HR: Heart Rate
Table 1: Baseline Characteristics of The Study Group
Safety outcomes of the study patients were described in Table 2. Compared to the propofol group, the etomidate group showed similar time to extubation (18.36±3.56 min vs. 18.30±3.40 min, p=0.821) and time to eye opening (10.00±5.81 min vs. 10.23±5.66 min, p=0.615). No significant difference was observed in pain score at rest, length of hospital stay and postoperative nausea and vomiting (p>0.05 for all).
| Outcomes | Propofol group (n=388) | Etomidate group (n=291) | p value |
|---|---|---|---|
| Time to extubation (min) | 18.30±3.40 | 18.36±3.56 | 0.821 |
| Time to eye opening (min) | 10.23±5.66 | 10.00±5.81 | 0.615 |
| Pain score at rest | 50.25±17.69 | 50.93±17.41 | 0.617 |
| Length of hospital stay (days) | 11.08±4.07 | 11.60±3.85 | 0.09 |
| Postoperative nausea and vomiting | 35 (9.02 %) | 23 (7.90 %) | 0.606 |
Table 2: Safety Outcomes of The Study Patients
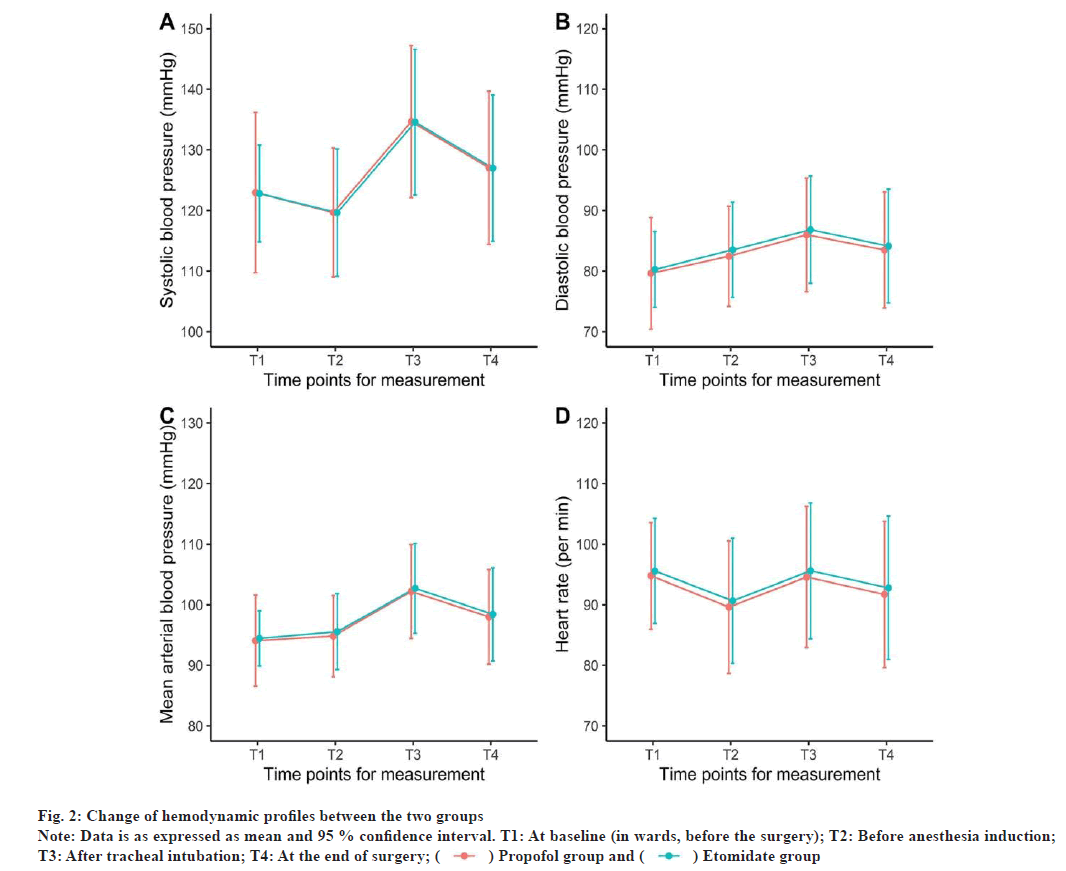
Changes in hemodynamic profiles of the study patients were shown in Table 3. Similar change patterns in the hemodynamic profiles over time were observed between the two groups (fig. 2). At each time point, there was no significant difference in the four studied hemodynamic profiles between the two groups (p>0.05 for all). Compared to the propofol group, the coefficients of variation of SBP (7.24±2.78 vs. 8.35±3.29, p<0.001), DBP (6.67±3.50 vs. 7.56±4.29, p=0.004) and MAP (5.36±2.27 vs. 6.19±3.00, p<0.001) in the etomidate group were significantly lower, but no significant difference in the coefficient of variation of HR was observed (p<0.05) (Table 4).
Fig. 2: Change of hemodynamic profiles between the two groups
Note: Data is as expressed as mean and 95 % confidence interval. T1: At baseline (in wards, before the surgery); T2: Before anesthesia induction; T3: After tracheal intubation; T4: At the end of surgery; ( ) Propofol group and (
) Propofol group and ( ) Etomidate group
) Etomidate group
| Hemodynamic profile | Propofol group (n=388) | Etomidate group (n=291) | p value |
|---|---|---|---|
| SBP (mmHg) | |||
| T2 | 119.66±10.64 | 119.63±10.50 | 0.97 |
| T3 | 134.65±12.55 | 134.57±12.03 | 0.939 |
| T4 | 127.05±12.63 | 127.00±12.06 | 0.962 |
| DBP | |||
| T2 | 82.44±8.27 | 83.51±7.85 | 0.087 |
| T3 | 85.98±9.38 | 86.82±8.84 | 0.241 |
| T4 | 83.49±9.57 | 84.13±9.40 | 0.387 |
| MAP | |||
| T2 | 94.82±6.70 | 95.56±6.28 | 0.145 |
| T3 | 102.19±7.76 | 102.71±7.41 | 0.373 |
| T4 | 98.01±7.83 | 98.42±7.69 | 0.494 |
| HR | |||
| T2 | 89.61±10.92 | 90.65±10.32 | 0.208 |
| T3 | 94.57±11.66 | 95.60±11.22 | 0.245 |
| T4 | 91.70±12.09 | 92.78±11.83 | 0.247 |
Note: T2: Before anesthesia induction; T3: After tracheal intubation and T4: At the end of surgery
Table 3: Hemodynamic Profile of The Study Patients Measured at Different Time Points
| Hemodynamic profiles | Propofol group (n=388) | Etomidate group (n=291) | p value |
|---|---|---|---|
| SBP | 8.35±3.29 | 7.24±2.78 | <0.001 |
| DBP | 7.56±4.29 | 6.67±3.50 | 0.004 |
| MAP | 6.19±3.00 | 5.36±2.27 | <0.001 |
| HR | 4.97±2.24 | 5.00±2.15 | 0.841 |
Table 4: Coefficient of Variation of Hemodynamic Profiles of The Study Patients
In this study, we specially investigated the safety and changes of hemodynamic profiles in patients who received intraoperative target-controlled infusion of etomidate for general anesthesia in laparoscopic cholecystectomy by comparison with another frequently used anesthetic (i.e., propofol). We found there was no significant difference in the studied safety outcomes but patients received etomidate for general anesthesia showed a more stable hemodynamic profile evaluated by coefficients of variation. This finding confirms a lower impact on hemodynamic profiles while using etomidate for general anesthesia in laparoscopic cholecystectomy compared to propofol, which has been observed in other surgeries and thus it supports the use of intraoperative target-controlled infusion of etomidate for general anesthesia in laparoscopic cholecystectomy.
Several studies had compared the use of etomidate for general anesthesia with that of propofol, but not specifically for laparoscopic cholecystectomy. Guo et al. investigated the feasibility of intraoperative target-controlled infusion of etomidate in patients with severe burns and found no significant difference in several safety outcomes except for lower cortisol and aldosterone levels in patients who received etomidate. This is consistent with our findings, but due to data limitation, we were unable to study the changes of cortisol and aldosterone levels. Guo et al. also reported no significant difference in MAP and HP between the two groups at the investigated time points and we had consistent findings, but we investigated the variations of the hemodynamic profiles and found a more stable hemodynamic profile[21]. Similar results were observed in a trial conducted by Song et al. in which the study population was patients who underwent endoscopic retrograde cholangiopancreatography[19]. Studies that investigated other types of surgery also reported a better hemodynamic stability when using etomidate compared to propofol[20,22], but all the above studies only included limited sample sizes and did not specially investigate patients who underwent laparoscopic cholecystectomy.
There are several mechanisms contributing to the cardiovascular changes during laparoscopy. First, increased intra-abdominal pressure due to carbon dioxide insufflation leads to catecholamine release and activation of the renin-angiotensin system with vasopressin release[23-25]. As a result, MAP increases and may contribute to the increase in SVR and Pulmonary Vascular Resistance (PVR)[26]. In addition, the compression of arterial vasculature with pneumoperitoneum may also increase SVR and PVR with variable effects on cardiac output and blood pressure[23-25]. Second, the head-up position, which is usually used in cholecystectomy may lead to venous pooling and therefore reduce venous return to the heart[23,27]. This may result in hypotension, especially in hypovolemic patients. Third, the absorption of carbon dioxide during laparoscopy can have direct and indirect cardiovascular effects. It leads to hypercarbia and associated acidosis including decreased cardiac contractility, sensitization to arrhythmias and systemic vasodilation. Meanwhile, as a result of sympathetic stimulation, it may induce tachycardia and vasoconstriction[23]. Etomidate is an imidazole derivative that acts directly on the Gamma-Aminobutyric Acid A (GABAA) receptor complex, blocking neuroexcitation and producing anesthesia. It has a feature of rapid onset and recovery, which is similar to propofol, but it does not cause vasodilation or myocardial depression and does not increase sympathetic tone, so it had fewer impacts on the hemodynamic profile. Another advantage of etomidate is its anticonvulsant properties, which makes it advantageous in hemodynamically unstable patients with head injury or stroke, because it can decrease cerebral metabolic rate of oxygen consumption and consequently reduce cerebral blood flow and intracranial pressure[28].
Strengths of this study included a large sample size and an unselected study population from real clinical settings. However, the study had some limitations. First, unlike a prospective study, our study was a retrospective observational study and therefore there might be variations in the anesthesia and/ or procedure, which might introduce confounding when comparing the study outcomes between the two groups. Second, we only studied blood pressure and HR as hemodynamic profiles, while there are other profiles such as cardiac output and other clinical outcomes with clinical importance. Due to data limitation, we were unable to study them, so the observed lower coefficients of variation of some hemodynamic profiles in the etomidate group may not be clinically relevant. Third, we only investigated hemodynamic profiles measured at the four time points, so it is unclear whether our findings would remain valid at other time points. Last, the study patients were from a single hospital, which might limit the generalizability of our findings.
There was no difference in safety outcomes but a more stable hemodynamic profile when comparing intraoperative target-controlled infusion of etomidate to propofol in laparoscopic cholecystectomy. This supports the use of intraoperative target-controlled infusion of etomidate for general anesthesia in laparoscopic cholecystectomy, but the findings need to be confirmed in other studies.
Author’s contributions:
Yongjun Zeng and Biwei Zhan contributed for methodology, investigation, data curation and original draft; Biwei Zhan contributed in writing, review and editing; Yongjun Zeng contributed for review and editing and finally idea, supervision, review and editing was done by Jingjing Liu.
Acknowledgements:
I would like to express my gratitude to all those helped me during the writing of this thesis. I acknowledge the help of my colleagues Jingjing Liu and Biwei Zhan. They have offered me suggestion in academic studies.
Conflict of interests:
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
- Csikesz NG, Singla A, Murphy MM, Tseng JF, Shah SA. Surgeon volume metrics in laparoscopic cholecystectomy. Dig Dis Sci 2010;55(8):2398-405.
[Crossref] [Google scholar] [PubMed]
- Overby DW, Apelgren KN, Richardson W, Fanelli R. SAGES guidelines for the clinical application of laparoscopic biliary tract surgery. Surg Endosc 2010;24(10):2368-86.
[Crossref] [Google scholar] [PubMed]
- Johansson M, Thune A, Nelvin L, Stiernstam M, Westman B, Lundell L. Randomized clinical trial of open versus laparoscopic cholecystectomy in the treatment of acute cholecystitis. Br J Surg 2005;92(1):44-9.
[Crossref] [Google scholar] [PubMed]
- Wilson RG, Macintyre IM, Nixon SJ, Saunders JH, Varma JS, King PM. Laparoscopic cholecystectomy as a safe and effective treatment for severe acute cholecystitis. BMJ 1992;305(6850):394-6.
[Crossref] [Google scholar] [PubMed]
- Vollmer CM, Callery MP. Biliary injury following laparoscopic cholecystectomy: Why still a problem? Gastroenterology 2007;133(3):1039-41.
[Crossref] [Google scholar] [PubMed]
- Khan MH, Howard TJ, Fogel EL, Sherman S, McHenry L, Watkins JL, et al. Frequency of biliary complications after laparoscopic cholecystectomy detected by ERCP: Experience at a large tertiary referral center. Gastrointest Endosc 2007;65(2):247-52.
[Crossref] [Google scholar] [PubMed]
- Comitalo JB. Laparoscopic cholecystectomy and newer techniques of gallbladder removal. JSLS 2012;16(3):406-12.
[Crossref] [Google scholar] [PubMed]
- Leggett PL, Churchman-Winn R, Miller G. Minimizing ports to improve laparoscopic cholecystectomy. Surg Endosc 2000;14(1):32-6.
[Crossref] [Google scholar] [PubMed]
- Leonard IE, Cunningham AJ. Anaesthetic considerations for laparoscopic cholecystectomy. Best Pract Res Clin Anaesthesiol 2002;16(1):1-20.
[Crossref] [Google scholar] [PubMed]
- Harris SN, Ballantyne GH, Luther MA, Perrino AC. Alterations of cardiovascular performance during laparoscopic colectomy: A combined hemodynamic and echocardiographic analysis. Anesth Analg 1996;83(3):482-7.
[Crossref] [Google scholar] [PubMed]
- Hein HT, Joshi GP, Ramsay MA, Fox LG, Gawey BJ, Hellman CL, et al. Hemodynamic changes during laparoscopic cholecystectomy in patients with severe cardiac disease. J Clin Anesth 1997;9(4):261-5.
[Crossref] [Google scholar] [PubMed]
- Kraut EJ, Anderson JT, Safwat A, Barbosa R, Wolfe BM. Impairment of cardiac performance by laparoscopy in patients receiving positive end-expiratory pressure. Arch Surg 1999;134(1):76-80.
[Crossref] [Google scholar] [PubMed]
- McLaughlin JG, Scheeres DE, Dean RJ, Bonnell BW. The adverse hemodynamic effects of laparoscopic cholecystectomy. Surg Endosc 1995;9:121-4.
[Crossref] [Google scholar] [PubMed]
- Safran D, Sgambati S, Orlando 3rd R. Laparoscopy in high-risk cardiac patients. Surg Gynecol Obstet 1993;176(6):548-54.
[Google scholar] [PubMed]
- Das S, Forrest K, Howell S. General anaesthesia in elderly patients with cardiovascular disorders: Choice of anaesthetic agent. Drugs Aging 2010;27:265-82.
[Crossref] [Google scholar] [PubMed]
- Forman SA, Warner DS. Clinical and molecular pharmacology of etomidate. Anesthesiology 2011;114(3):695-707.
[Crossref] [Google scholar] [PubMed]
- Fruergaard K, Jenstrup M, Schierbeck J, Wiberg-Jørgensen F. Total intravenous anaesthesia with propofol or etomidate. Eur J Anaesthesiol 1991;8(5):385-91.
[Google scholar] [PubMed]
- Cohan P, Wang C, McArthur DL, Cook SW, Dusick JR, Armin B, et al. Acute secondary adrenal insufficiency after traumatic brain injury: A prospective study. Crit Care Med 2005;33(10):2358-66.
[Crossref] [Google scholar] [PubMed]
- Song JC, Lu ZJ, Jiao YF, Yang B, Gao H, Zhang J, et al. Etomidate anesthesia during ERCP caused more stable haemodynamic responses compared with propofol: A randomized clinical trial. Int J Med Sci 2015;12(7):559.
[Crossref] [Google scholar] [PubMed]
- Aggarwal S, Goyal VK, Chaturvedi SK, Mathur V, Baj B, Kumar A. A comparative study between propofol and etomidate in patients under general anesthesia. Braz J Anesthesiol 2016;66(3):237-41.
[Crossref] [Google scholar] [PubMed]
- Guo Z, Pang L, Jia X, Wang X, Su X, Li P, et al. Intraoperative target-controlled infusion anesthesia application using remifentanil hydrochloride with etomidate in patients with severe burn as monitored using Narcotrend. Burns 2015;41(1):100-5.
[Crossref] [Google scholar] [PubMed]
- Zheng H, Zhu Y, Chen K, Shen X. The effect of etomidate or propofol on brainstem function during anesthesia induction: A bispectral index-guided study. Drug Des Devel Ther 2019;13:1941-6.
[Crossref] [Google scholar] [PubMed]
- Gutt CN, Oniu T, Mehrabi A, Schemmer P, Kashfi A, Kraus T, et al. Circulatory and respiratory complications of carbon dioxide insufflation. Dig Surg 2004;21(2):95-105.
[Crossref] [Google scholar] [PubMed]
- O'Malley C, Cunningham AJ. Physiologic changes during laparoscopy. Anesthesiol Clin North Am 2001;19(1):1-9.
[Crossref] [Google scholar] [PubMed]
- Myre K, Rostrup M, Buanes T, Stokland O. Plasma catecholamines and haemodynamic changes during pneumoperitoneum. Acta Anaesthesiol Scand 1998;42(3):343-7.
[Crossref] [Google scholar] [PubMed]
- Joris JL, Noirot DP, Legrand MJ, Jacquet NJ, Lamy ML. Hemodynamic changes during laparoscopic cholecystectomy. Anesth Analg 1993;76(5):1067-71.
[Crossref] [Google scholar] [PubMed]
- Hirvonen EA, Poikolainen EO, Pääkkönen ME, Nuutinen LS. The adverse hemodynamic effects of anesthesia, head-up tilt and carbon dioxide pneumoperitoneum during laparoscopic cholecystectomy. Surg Endosc 2000;14:272-7.
[Crossref] [Google scholar] [PubMed]
- Hoyer C, Kranaster L, Janke C, Sartorius A. Impact of the anesthetic agents ketamine, etomidate, thiopental and propofol on seizure parameters and seizure quality in electroconvulsive therapy: A retrospective study. Eur Arch Psychiatry Clin Neurosci 2014;264(3):255-61.
[Crossref] [Google scholar] [PubMed]