- *Corresponding Author:
- Jiqin Tang
Shandong University of Traditional Chinese Medicine, Jinan, Shandong Province 250300, China
E-mail: tangjiqin0312@163.com
| This article was originally published in a special issue, “Clinical Advancements in Life Sciences and Pharmaceutical Research” |
| Indian J Pharm Sci 2024:86(5) Spl Issue “306-314” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Glenohumeral subluxation has long plagued stroke individuals, and effective treatments remain to be further explored. In this study, we systematically evaluated the therapeutic effect of applying the kinesiology tape on glenohumeral subluxation after stroke. Randomized controlled trials on the application of kinesiology tape participation therapy in glenohumeral subluxation after stroke were collected by searching condition based maintenance, VIrus Protein database, WanFang database, China National Knowledge Infrastructure, PubMed, Embase and Cochrane library for the period of time from the establishment of the library to March 2024, which was the time period for the search. After screening the literature, Review Manager 5.4 software was used to perform meta-analysis of the data results of the outcome indicators in the included literature, and only descriptive analyses were performed for trials with effect sizes that could not be combined. A total of nine literatures were included. Meta-analysis results showed that eight randomized controlled trials that chose upper extremity Fugl-Meyer assessment rating as the outcome indicator scored better in the experimental group than in the control group after the application of kinesiology tape (95 % confidence interval (5.48, 12.46), p<0.0001); six randomized controlled trials that measured acromiohumeral interval values of the study subjects were unable to demonstrate that the experimental group scored better than in the control group after the application of kinesiology tape (95 % confidence interval (-3.84, 2.39), p=0.65), and after sensitivity analysis, two papers were excluded to re-run the meta-analysis, and the results proved that the difference between the data of the four papers was statistically significant (95 % confidence interval (-4.06, -2.50), p<0.05); the 4 randomized controlled trials that selected the modified Barthel index as an outcome indicator scored better in the experimental group than in the control group after the application of kinesiology tape (95 % confidence interval (1.69, 14.45), p=0.01). Clinical evidence from randomized controlled trials at this stage suggests that kinesiology tape is effective in improving disease progression in stroke glenohumeral subluxation.
Keywords
Stroke, glenohumeral subluxation, kinesiology tape, meta-analysis
Glenohumeral Subluxation (GHS) is a visible gap more than one finger width that can be felt below the acromion and above the humeral head, and the incidence of GHS in stroke is about 17 %-84 %[1], which is an important factor affecting the recovery of individual’s upper limb function, and the early intervention of rehabilitation will have a positive impact on the recovery of GHS. Modern treatment methods commonly used in rehabilitation include physiotherapy, neuromuscular facilitation techniques, upper limb rehabilitation robots, and Kinesiology Tape (KT) techniques. Among them, KT was created by Ramirez et al.[2]. KT is a thinner and more flexible tape than traditional tapes, and is mainly used to improve therapeutic outcomes by improving joint mobility[3], promoting lymphatic circulation[4], enhancing proprioception[5], and improving motor and postural control[6]. It is simple, portable, and easy to use, and thus has been adopted by an increasing number of therapists and individuals. This metaanalysis focused on the effects of KT on GHS in post-stroke individuals, with the aim of providing evidence-based clinical evidence.
Materials and Methods
Search strategy:
The Chinese Biomedical Literature Database (CMB), VIrus Protein database (VIP), Wanfang database, China National Knowledge Infrastructure (CNKI), PubMed, Embase, and Cochrane library were searched, and the search was conducted in English and Chinese languages only. Subject terms and keywords were combined during the search, and English search terms included stroke, cerebrovascular accident, cerebrovascular apoplexy, brain vascular accident, shoulder subluxation, shoulder dislocations, glenohumeral dislocations and KP. In the case of PubMed, for example, the search formula is ((stroke) or (cerebrovascular accident) or (cerebrovascular apoplexy)) or (brain vascular accident) and ((shoulder subluxation) or (shoulder dislocations) or (glenohumeral dislocations) or (review (filter))) and (KT) and (review (filter)).
Inclusion criteria includes the study language was limited to Randomized Controlled Trials (RCTs) type articles in Chinese and English; meet the diagnostic criteria of relevant cerebrovascular diseases[7] and/or The diagnostic criteria were based on the World Health Organization (WHO) guidelines[8], confirmed by Computed Tomography (CT) or Magnetic Resonance Imaging (MRI). The disease had its first onset with unilateral limb paralysis and met the GHS diagnostic criteria[9]. The intervention measures included conventional rehabilitation treatments such as exercise therapy, acupuncture, electrical stimulation, and massage in the control group. In addition, part of the control group applied comfort patches or external plasters as a supplement to conventional treatment. In the experimental group, the conventional rehabilitation treatment and the intervention of applying KT were used at the same time and the outcome indicators were summarized by Upper Extremity-Fugl Meyer Assessment (UE-FMA), Apnea-Hypopnea Index (AHI), Maslach Burnout Inventory (MBI), Patient‐ Reported Outcome Measures (PROMs) or Visual Analogue Scales (VAS).
Exclusion criteria include studies with unclear trial data, where means and standard deviations of outcome indicators are more difficult to calculate accurately; studies with inconsistent intervention methodologies; literature that is duplicated or where the full text is inaccessible; studies of low-quality studies or non-RCT types of studies and studies based on animal experiments.
Statistical methods:
Review Manager 5.4 software was selected for metaanalysis of the included literature. Mean Difference (MD) was selected as the effect indicator for the measurement data; if the literature data were measured with different measurement methods or measurement units, Standardized Mean Difference (SMD) was selected for the analysis of the results, and 95 % Confidence Interval (CI) were calculated for each effect size. Heterogeneity analysis of the included studies was performed using the Chi-square (χ2) test (test level α=0.05), which was also combined with I2 to quantify the magnitude of heterogeneity. If p<0.10 or I2>50 %, then there was statistical heterogeneity, in this case, the random effect model was used for meta-analysis; if p≥0.10 and I2≤50 %, then there was no statistical heterogeneity, in this case, the fixed effect model was used for meta-analysis. When there is obvious clinical heterogeneity between studies, subgroup analysis or sensitivity analysis will be used to deal with analysing the source of heterogeneity, or only descriptive analysis.
Results and Discussion
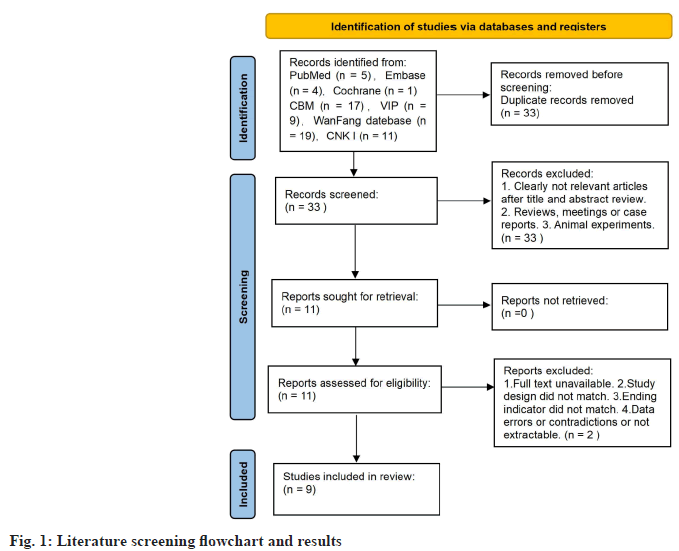
The preliminary search yielded 66 articles, including Condition-Based Maintenance (CBM) (17 articles), VIP database (9 articles), Wanfang database (19 articles), CNKI (11 articles), PubMed (5 articles), Embase (4 articles), and Cochrane Library (1 article). Duplicate articles were excluded to get 32 articles, and by screening the literature for research purpose, inclusion criteria, exclusion criteria, and diagnostic criteria, 9 RCT trials[10-18] were finally included, with a total of 497 individuals, 248 in the control group and 249 in the experimental group as shown in fig. 1.
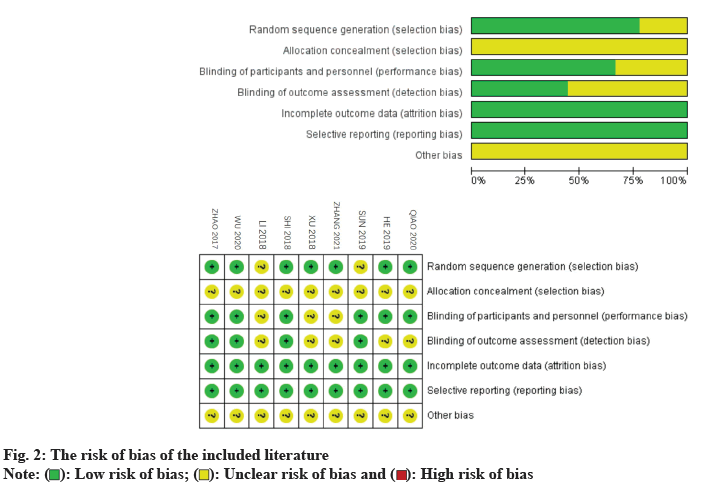
The basic characteristics of the included literature are shown in Table 1. 8 of the 9 included literature had clear inclusion and exclusion criteria, 7 were grouped using the randomized numeric table method, 1 was blinded, 5 had informed consent signed by family members and individuals, and none of the 9 literature mentioned allocation concealment. The analysis and summary of the risk of bias of the included literature was shown in fig. 2.
Study ID |
Randomization | Sample size (E/C) | Intervention (E) | Intervention (C) | Paste method | Treatment cycle | Outcome indicators |
|---|---|---|---|---|---|---|---|
Zhang et al.[17] |
Random number table method | 37/37 | Conventional treatment | Conventional treatment+KT | X-type | Not mentioned | ①② |
Qiao et al.[16] |
Random number table method | 30/30 | Conventional treatment | Conventional treatment+KT | X-type+I-type+I-type+I-type+Y-type | 4 w | ①②③ |
Wu et al.[15] |
Random number table method | 40/40 | Conventional treatment+control patch | Conventional treatment+KT | I-type+I-type+Y-type+X-type | 4 w | ①② |
Sun et al.[14] |
Integration in line with norms | 14/13 | Conventional treatment | Conventional treatment+KT | I-type+I-type | 4 w | ①③⑤ |
He et al.[13] |
Random number table method | 22/23 | Conventional treatment | Conventional treatment+KT | I-type+I-type | 4 w | ①②④ |
Shi et al.[12] |
Random number table method | 28/28 | Conventional treatment | Conventional rehabilitation treatment+KT | X-type+I-type+I-type | 6 w | ①② |
Xu et al.[18] |
Random number table method | 18/19 | Conventional treatment+electrical stimulation | Conventional treatment+electrical stimulation+KT | I-type+I-type | 50 d | ③④⑥ |
Li et al.[10] |
Not mentioned | 29/29 | Conventional treatment | Conventional treatment+KT | I-type | 22 d | ①④ |
Zhao et al.[11] |
Random number table method | 30/30 | Conventional treatment+control patch | Conventional treatment+KT | I-type+I-type | 4 w | ①② |
Note: ①FMA, ②AHI, ③VAS, ④MBI, ⑤PROM (flexure), ⑥apparent efficiency; (E): Experimental group and (C): Control group
Table 1: Basic Information Form
A funnel plot was made to evaluate the publication bias of the nine included papers. As the results are shown in fig. 3, the nine papers were not able to be distributed symmetrically on both sides, and therefore had a certain publication bias.
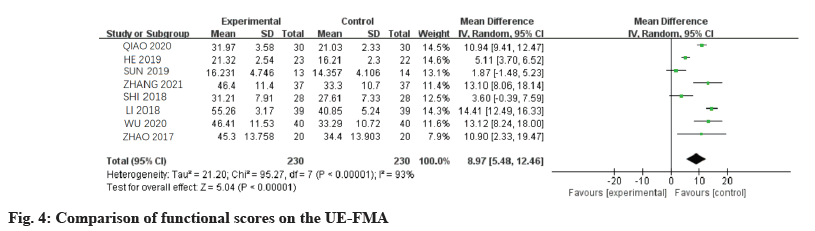
Eight of the nine included papers rated the scores of upper limb function in 460 individuals using the UEFMA[ 10-17], and the results are shown in fig. 4 (χ2=92.43, df=6, p<0.0001, I2=94 %, 95 % CI (5.48, 12.46)). The I2>50 % indicates that the results of the eight papers have a significant heterogeneity, therefore, the random effects model was chosen for the combined analysis. p<0.05 and the combined effects results did not intersect with the null line indicated that the results of the 8 RCTs were statistically different, which proved that the test group applying KT was more effective than the control group in the recovery of upper limb function in the GHS after stroke.
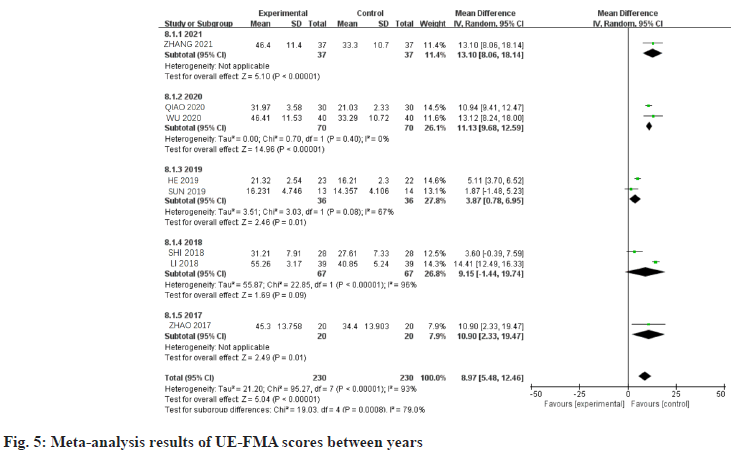
The heterogeneity of the 8 studies was high (I2=94 %), so the FMA scores in the 8 papers were analysed in subgroups. The high heterogeneity was considered likely to be due to differences in the year of publication and was therefore categorized into five subgroups; one paper published in 2021[17], two papers published in 2020[15,16], two papers published in 2019[13,14], two papers published in 2018[10,12], and one paper published in 2017[11]. The results of the analysis were shown in fig. 5. The results show that the heterogeneity does vary between years.
The significantly greater heterogeneity (I2=96 %) between the two data sets in 2018 suggests that it is the main cause of the high overall heterogeneity of UE-FMA scores[10,12]. The reason may be due to the large difference in the time of the study subjects in the two groups despite being published in the same year, the different taping protocols in the two test groups, or the different scale scoring criteria by the evaluators of the studies, but the specific reasons need to be analysed in further studies. Meanwhile, the difference between the two groups of data was not statistically significant (p>0.05).
One piece of literature was screened in each of the years 2021 and 2017, therefore descriptive analysis was performed. Zhao et al.[11] conducted hypothesis tests on UE-FMA scores before and after the treatment of the study participants, and the results showed that there was no significant difference in the UE-FMA scores before the treatment (p>0.05), and there was a significant difference after the treatment (p<0.05), which indicated that the study was statistically significant. In this study, the data of Zhao et al.[11] were analysed statistically (p=0.01, 95 % CI (2.33, 19.47)), and the results were consistent (p<0.05). Zhang et al.[17] conducted hypothesis tests on UEFMA scores of the study subjects after treatment, and the results showed that the upper extremity motor function scores of the experimental group were higher than those of the control group (p<0.05), which was statistically significant. In the present study, the data of Zhang et al. were statistically analysed (p<0.05, 95 % CI (8.06, 18.14)), and the results were consistent.
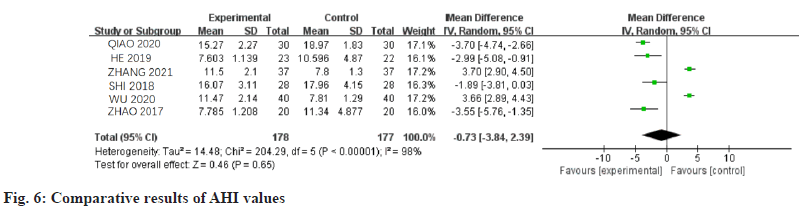
A total of six trials out of nine RCTs compared the value of shortest distance between the inferior border of the lateral end of acromion and the cephalic surface of the humerus in 356 individuals[11-13,15-17], and the results are shown in fig. 6 (χ2=204.29, df=5, I2=98 %, p=0.65, 95 % CI (-3.84, 2.39)). A randomeffects model was chosen with I2>50 % for the statistical analysis. Since p>0.05, 95 % CI (-3.84, 2.39), it could not be shown that the application of intramuscular patch in the experimental group was more effective than the control group in reducing the severity of GHS after stroke.
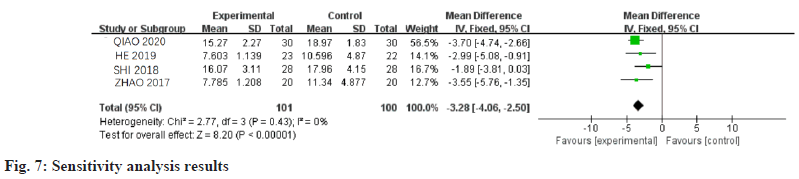
Comparing the post-treatment AHI values of the test and control groups in the 6 trials, it was found that only the control group of the 2 studies by Wu et al.[15] and Zhang et al.[17] had a higher AHI value than the treatment group, therefore, after a sensitivity analysis, it was found that the heterogeneity was significantly reduced by excluding the results of the studies. The results after exclusion are shown in fig. 7 (χ2=2.77, df=3, I2=0 %, p<0.05, 95 % CI (-4.06, -2.50)), therefore, the random effect model was chosen for the statistical analysis, and it also indicated that the application of KT in the experimental group was better than that in the control group in alleviating the severity of GHS after stroke. Therefore, the reason for the high heterogeneity consideration may be caused by the difference in the pre-treatment AHI values of the study subjects in the experimental and control groups or the difference in the therapist’s measurement method.
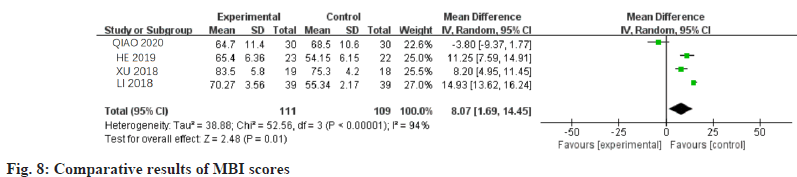
Four of the nine included papers evaluated the ability of 220 individuals to perform activities of daily living before and after treatment[10,13,16,18], and the results are shown in fig. 8 (χ2=52.56, df=3, I2=94 %, p=0.01, 95 % CI (1.69, 14.45)). Because of I2>50 %, there was obvious heterogeneity among the 4 papers, therefore, the random effect model was chosen for statistical analysis. p<0.05, 95 % CI (1.69, 14.45), indicating that the application of KT in the experimental group was better than the control group for the improvement of the ability to perform activities of daily living in GHS individuals after stroke.
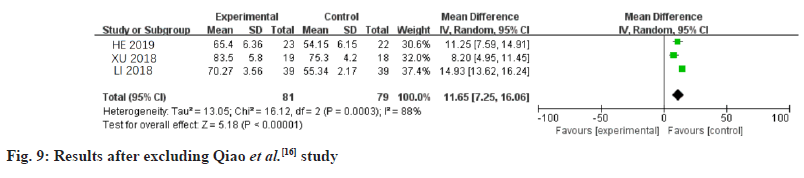
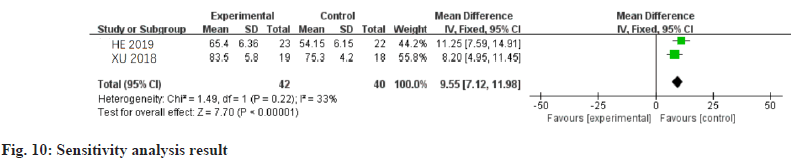
Comparison of the 4 sets of experimental data revealed that the difference between the results of Qiao et al.[16] MBI data was not statistically significant, and its exclusion was found to be effective in reducing the heterogeneity (fig. 9, I2=88 %), but still with I2>50 %. After sensitivity analysis, it was found that excluding Li et al.[10] and Qiao et al.[16] studies significantly reduced heterogeneity (fig. 10, I2=33 %). Therefore, it was considered that the high heterogeneity might be due to the different scale scoring criteria or measurement methods by the measurers in the two studies.
Fig. 9: Results after excluding Qiao et al.[16] study
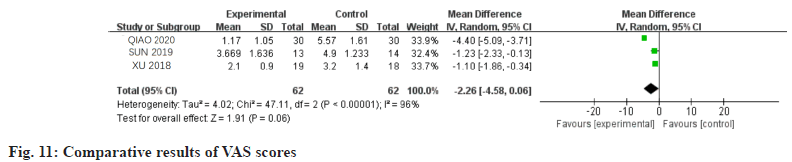
Three of the nine trials scored the pain level of the study subjects before and after the trials[14,16,18], and the results of the post-treatment scores are shown in fig. 11 ( χ2=4.02, df=2, I2=96 %, p=0.06, 95 % CI (-4.58, 0.06)). The I2=96 % showed that the results of these three trials were significantly heterogeneous, and therefore the randomized effect model was used for statistical analysis. p>0.05, 95 % CI (-4.58, 0.06), the difference in data was not statistically significant, therefore it was not possible to demonstrate the superiority of the application of KT in the test group in terms of its role in the treatment of glenohumeral joint pain. The reasons considered may be due to the differences in the three RCTs in which the subjects were the interventions or the small sample size in this study regarding the evaluation of glenohumeral joint pain.
Data from the three publications included in this study do not prove that KT can be applied to treat glenohumeral pain, but VAS scores before and after the three trial groups demonstrate that application of KT can assist in relieving glenohumeral pain. A recent meta-analysis evaluating KT for the treatment of hemiplegic shoulder pain concluded that KT was superior to sham, placebo, or no patch in reducing pain in both acute, subacute, and chronic stroke individuals[19].
The meta-analysis of this study showed that the application of KT combined with conventional rehabilitation therapy for post-stroke GHS can effectively reduce the inferior border of the external acromion-humeral head distance, assist in relieving shoulder pain, and significantly improve the individuals’ upper extremity motor function and ability to perform activities of daily living. The incidence of post-stroke GHS varies widely among different reports, and is higher in individuals with flaccid paralysis and significantly impaired motor function[20]. The pathogenesis of GHS after stroke may be triggered by overstretching of the shoulder capsule and the hypotonic supraspinatus and deltoid muscles due to gravity[21], or by the change of scapular direction due to the spasm of the pectoralis major and latissimus dorsi muscles and the tilting of the body to the hemiplegic side due to the poor control of the torso, resulting in the retraction and downward rotation of the scapula, which, together with the hypotonic supraspinatus and other flexors, ultimately leads to the detachment of the head of humerus from the articular glenoid[22]. The joint glenoid detachment, causing nerve entrapment pain and soft tissue damage. This negatively affects the individual’s daily activities and quality of life. Compared with traditional inelastic bandages, KT has the property of providing structural support but not restricting joint movement. By applying constant shear force to the skin for several days, the stress exerted on the skin improves the individual’s ability to improve the feedback of sensory input from the shoulder causing neural reflexes and thus improving proprioception[23,24], activates the recruitment of flexor muscles such as the supraspinatus and deltoid muscles during maximal contraction[25], slows down the degree of muscle wasting and spasticity during the recovery period in early stage stroke individuals[26], and it also generates transverse forces, thus stabilizing the fascial chain around the shoulder joint and the muscle tension to reduce gravity and the degree of spasm during recovery. It can also produce lateral force to stabilize the fascial chain and muscle tension around the shoulder joint to reduce the pull of gravity and other factors on the hypotonic muscle groups[27].
In this study, we believe that the reasons for the improvement of upper extremity motor function by KT may be to promote local circulation; to improve joint mobility[28]; to increase proprioception to promote muscle activation and improve control[29,30]; to relax the tense muscles to reduce pain and relieve the fear of the individuals[31]. After the improvement of upper limb motor function, the individuals’ ability of daily life activities also improved.
Only Chinese and English literature was included in this paper, and the possibility of omitting other relevant RCTs cannot be ruled out even after a comprehensive literature search; the total number of included studies and individuals was relatively small, and more samples are still needed for future exploration; some of the results were not labelled with the specific blinding method, and the results may be subject to a certain degree of bias.
On the topic of applying KT to treat stroke GHS, there is still a need for more high-quality RCTs including longer follow-up and large enough samples for systematic evaluation, which will help the research to analyse the optimal protocol of applying KT combined with basic rehabilitation therapy for stroke GHS. In addition, it is recommended that trials should apply more specific and reliable indicators or methods to assess individuals, which will make the analysis results more accurate and more conducive to subgroup analysis and sensitivity analysis.
Funding:
This study was supported by Shandong Geriatrics Society Fund Project (No: LKJGG2021Z018) and Shandong University of Traditional Chinese Medicine Scientific Research and Innovation Team Project (Approved No: 220316). The funders had no role in the design, execution, or writing of the study .
Conflict of interests:
The authors declared no conflict of interests.
References
- Arya KN, Pandian S, Vikas, Puri V. Rehabilitation methods for reducing shoulder subluxation in post-stroke hemiparesis: A systematic review. Top Stroke Rehabil 2018;25(1):68-81.
[Crossref] [Google Scholar] [PubMed]
- Ramirez JO, de la Cruz SP. Therapeutic effects of kinesio taping in children with cerebral palsy: A systematic review. Arch Argent Pediatr 2017;115(6):e356-61.
[Google Scholar] [PubMed]
- Mutlu EK, Mustafaoglu R, Birinci T, Ozdincler AR. Does Kinesio taping of the knee improve pain and functionality in patients with knee osteoarthritis?: A randomized controlled clinical trial. Am J Phys Med Rehabil 2017;96(1):25-33.
[Crossref] [Google Scholar] [PubMed]
- Liu K, Duan Z, Chen L, Wen Z, Zhu S, Qu Q, et al. Short-term effect of different taping methods on local skin temperature in healthy adults. Front Physiol 2020;11:488.
[Crossref] [Google Scholar] [PubMed]
- Chang WD, Chen FC, Lee CL, Lin HY, Lai PT. Effects of kinesio taping vs. McConnell taping for patellofemoral pain syndrome: A systematic review and meta-analysis. Evid Based Complement Alternat Med 2015;2015(1):471208.
[Crossref] [Google Scholar] [PubMed]
- Wang Y, Gu Y, Chen J, Luo W, He W, Han Z, et al. Kinesio taping is superior to other taping methods in ankle functional performance improvement: A systematic review and meta-analysis. Clin Rehabil 2018;32(11):1472-81.
[Crossref] [Google Scholar] [PubMed]
- Neurology Branch of Chinese Medical Association. 2016 Edition of Chinese Guidelines and Consensus for the Prevention and Treatment of Cerebrovascular Disease. Beijing: People's Health Press; 2016. p. 196-201.
- Nakayama H, Jorgensen HS, Raaschou HO. Recovery of upper extremity function in stroke individuals: The copenhagen stroke study. Arch Phys Med Rehabil 1994;73:51-3.
- Department of Medical Science, Ministry of Health, People's Republic of China. Chinese rehabilitation medicine diagnosis and treatment standard. Beijing: Huaxia Publishing House; 1999. p. 82-3.
- Li Y, Xiao G. Evaluation of the effect of intraosseous effect patch taping technique combined with rehabilitation therapy in the treatment of post-stroke shoulder subluxation. Contemporary medicine series. Contemp Med Symp 2018;16(20):84-6.
- Zhao SL, Wang WJ. Effect of kinesio taping on subluxation of shoulder in hemiplegic patients after stroke. Chin J Rehabil Theory Pract 2017;23(10):1200-2.
[Crossref] [Google Scholar] [PubMed]
- Sh B, Li K, Hu Y. Therapeutic effectiveness of Kinesio taping for relieving shoulder pain in stroke individuals with shoulder subluxation. Chin J Rehabil Med 2018;33(31):310-4.
- He Y, Cui R, Dong Y. Observation on the effect of rehabilitation training combined with intramuscular plaster on the subluxation of shoulder joint after cerebral apoplexy. J Baotou Med Coll 2019;35(10):10-9.
- Sun G, Zou C, Qi X. Analysis of the efficacy of intraosseous effect patch on shoulder pain of shoulder subluxation origin in stroke. Heilongjiang Pharm Sci 2019;42(3):8-12.
- Wu X, Yang M, Rao L. Effect of kinesio taping combined with conventional rehabilitation training in the treatment of shoulder subluxation in stroke individuals with hemiplegia and the influence of side upper limb motor function. China Mod Med 2020;27(16):59-62.
- Qiao L, Wang C. Effects of intramuscular effect patch combined with conventional rehabilitation training on shoulder subluxation and shoulder pain in hemiplegic individuals with stroke. Massage Rehabil Med 2020;11(2):39-42.
- Zhang Y. Effectiveness of intramuscular effect patch combined with conventional rehabilitation in the treatment of shoulder joint subluxation in hemiplegic individuals with stroke and its effect on the motor function of the affected upper limb. China Healthcare Nutr 2021;31(22):126.
- Xu L, Li X, Song B. The efficacy of intramuscular effect patch in the recovery of shoulder subluxation after stroke. Shanxi Med J 2018;47(14):1698-9.
- Deng P, Zhao Z, Zhang S, Xiao T, Li Y. Effect of kinesio taping on hemiplegic shoulder pain: A systematic review and meta-analysis of randomized controlled trials. Clin Rehabil 2021;35(3):317-31.
[Crossref] [Google Scholar] [PubMed]
- Stolzenberg D, Siu G, Cruz E. Current and future interventions for glenohumeral subluxation in hemiplegia secondary to stroke. Topic Stroke Rehabil 2012;19(5):444-56.
[Crossref] [Google Scholar] [PubMed]
- Lee JH, Baker LL, Johnson RE, Tilson JK. Effectiveness of neuromuscular electrical stimulation for management of shoulder subluxation post-stroke: A systematic review with meta-analysis. Clin Rehabil 2017;31(11):1431-44.
[Crossref] [Google Scholar] [PubMed]
- Arner JW, Peebles LA, Bradley JP, Provencher MT. Anterior shoulder instability management: Indications, techniques, and outcomes. Arthroscopy 2020;36(11):2791-3.
[Crossref] [Google Scholar] [PubMed]
- Santos GL, Souza MB, Desloovere K, Russo TL. Elastic tape improved shoulder joint position sense in chronic hemiparetic subjects: A randomized sham-controlled crossover study. PloS One 2017;12(1):e0170368.
[Crossref] [Google Scholar] [PubMed]
- Bischoff L, Babisch C, Babisch J, Layher F, Sander K, Matziolis G, et al. Effects on proprioception by Kinesio taping of the knee after anterior cruciate ligament rupture. Eur J Orthop Surg Traumatol 2018;28(6):1157-64.
[Crossref] [Google Scholar] [PubMed]
- Mendez-Rebolledo G, Ramirez-Campillo R, Guzman-Muñoz E, Gatica-Rojas V, Dabanch-Santis A, Diaz-Valenzuela F. Short-term effects of kinesio taping on muscle recruitment order during a vertical jump: A pilot study. J Sport Rehabil 2018;27(4):319-26.
[Crossref] [Google Scholar] [PubMed]
- Hsich HC, Liao RD, Yang TH. The clinical fleet of kinesio taping and modified constraint-induced movement therapy on upper extremity function and spasticity in individuals with stroke: A randomized controlled pilot study. Eur J Phys Rehabil Med 2021;57(4):511-9.
- Ortiz-Ramirez J, Cruz SP. Eficacy of the application of kinesio tape in individuals with stroke. Rev Neurol 2017;64(4):175-9.
- Yoshida A, Kahanov L. The effect of kinesio taping on lower trunk range of motions. Res Sports Med 2007;15(2):103-12.
[Crossref] [Google Scholar] [PubMed]
- Ozmen T, Aydogmus M, Dogan H, Acar D, Zoroglu T, Willems M. The effect of kinesio taping on muscle pain, sprint performance, and flexibility in recovery from squat exercise in young adult women. J Sport Rehabil 2016;25(1):7-12.
[Google Scholar] [PubMed]
- Chang HY, Chou KY, Lin JJ, Lin CF, Wang CH. Immediate effect of forearm kinesio taping on maximal grip strength and force sense in healthy collegiate athletes. Phys Ther Sport 2010;11(4):122-7.
[Crossref] [Google Scholar] [PubMed]
- Gonzalex-Iglesias J, Fernandex-de-Las-Penas C, Cleland JA. Short-term effects of cervical kinesio taping on pain and cervical range of motion in individuals with acute whiplash injury: A randomized clinical trial. J Orthop Sports Phys Ther 2009;39(7):515-21.
 ): Low risk of bias; (
): Low risk of bias; ( ): Unclear risk of bias and (
): Unclear risk of bias and ( ): High risk of bias
): High risk of bias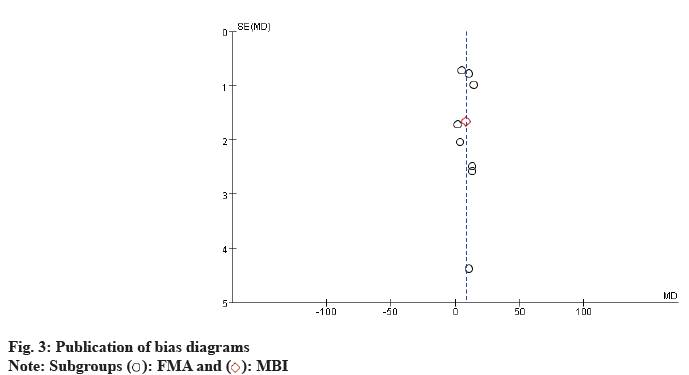
 ): FMA and (
): FMA and ( ): MBI
): MBI