- *Corresponding Author:
- Lu Wang
Nursing Department of Zuanshiwan Area, the Second Hospital of Dalian Medical University, Dalian, 116031, China
E-mail: byhulibu@126.com
| This article was originally published in a special issue, |
| "Clinical and Experimental Studies on Drug and Intervention Repurposing in China" |
| Indian J Pharm Sci 2019:81(4)spl issue1;165-168 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Nursing regimens were applied on patients with diabetes mellitus with tumors to improve medication compliance and the effects on medication compliance were observed and analyzed. A total of 160 patients diagnosed with diabetes mellitus and tumors treated at the Second Hospital of Dalian Medical University were enrolled. The patients were divided into the control group and the research group, with 80 patients in each group. Routine nursing care was provided to patients in the control group, while routine nursing care combined with medication compliance interfering nursing regimen was provided to patients in the research group. The nursing effects were compared between both groups. By comparing the medication compliance, fasting blood-glucose, 2-hour postprandial blood-glucose, levels of glycosylated hemoglobin and the overall nursing satisfaction, results showed that all indicators of the research group were significantly better than those of the control group (p<0.05). Application of medication compliance interfering nursing regimens to diabetic patients with tumor could significantly improve the medication compliance of patients.
Keywords
Diabetes mellitus complicated by tumour, medication compliance, nursing methods, nursing effects
Both diabetes mellitus and malignant tumour are lifethreatening diseases. Diabetes mellitus could cause disorders in protein metabolism, glucose metabolism and lipid metabolism, thus greatly up-regulating the incidence of malignant tumour[1-3]. As for the treatment of diabetic patients with tumour, the priority is to effectively control the blood glucose level. As longterm medication is required to control the blood glucose level, outcomes are dependent on patients’ medication compliance.
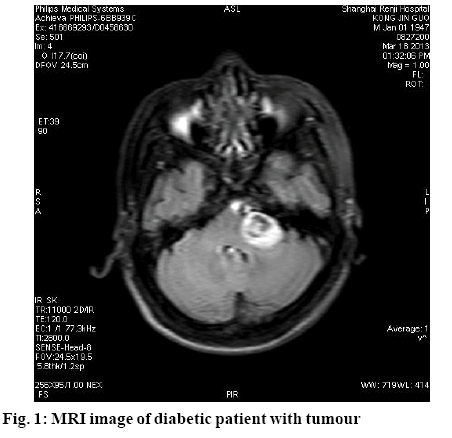
There are numerous factors contributing to diabetes, involving genetic and environment factors, with complicated clinical symptoms. As an abnormal metabolic syndrome, diabetics could lead to chronic progressive damage in multiple systems. Currently, patients suffering from both diabetes mellitus and tumour are increasing (fig. 1). Literature reports showed that there were various mechanisms underlying the occurrence of diabetes mellitus complicated by tumour. Patients were subjected to multiple therapeutic approaches and suffered from complicated emotions, thus leading to generally poor medication compliance. This study aims to observe and analyse the effects of nursing methods on the medication compliance of patients with diabetes mellitus and complicated by tumour, which is reported as follows.
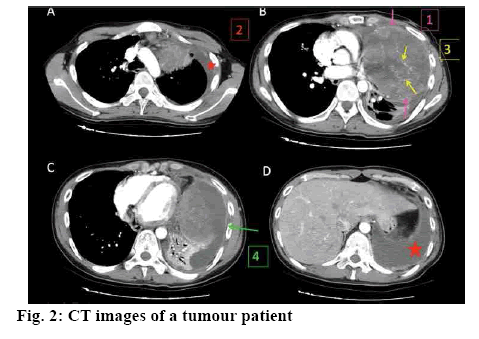
A total of 160 diabetic patients with tumour treated at the Second Hospital of Dalian Medical University from January 2015 to December 2017 were enrolled. CT image of a patient in this study were shown in fig. 2. All patients were definitely diagnosed by clinical examinations and presented with corresponding manifestations, such as polyuria, polydipsia, loss of weight, weakness, itchy skin, pain, ulcer, obstruction and anaemia. All patients were properly informed and the informed consents were signed. Patients were randomized into research group and control group, with 80 patients in each group. Of those, there were 48 male patients and 32 female patients in the research group, with an average age of 60.2±3.5 y. And there were 50 male patients and 30 female patients in the control group, with an average age of 62.0±4.0 y. Data obtained from both groups were comparable (p>0.05).
Routine nursing care was provided to the patients in the control group, including diet care, daily life care, complication care and health guidance. Routine nursing care combined with medication compliance interfering regimen was applied on patients in the research group, which included, psychology care. Diabetic patients with tumour may suffer from severe psychological burden and adverse emotions. Thus the nursing staff should build an active communication relationship with patients to understand their psychological status and dispel negative emotions (anxiety, nervous, depress, fear). For example, approaches like listening to music, reading books, playing chess, and taking a walk should be adopted to enhance patients’ faith, distract their attention and improve their values on medication therapy.
Health publicity was provided through holding a lecture, sending out health brochures, consulting and the like, as a part of health education on patients. Contents of health education included the causes of diabetes, therapeutic methods, knowledge and therapeutic regimens about tumour, types of hypoglycaemic agent, the importance of proper and regular medication, preservation of drugs and the consequences of poor compliance. Patients’ medication conditions were evaluated during health education. Patients were encouraged to follow doctors’ advice. Before each education, a simple quiz about the last lecture was conducted. A DVD, brochures for each lecture was provided to the patients, in case they wish to learn at home.
Experience sharing meetings were held once or twice every month, to provide a chance for patients to share their feelings and encourage each other, thus improving their compliance and promote recovery. Also, a certain theme was set for patients to learn. For example, members could discuss home-made recipe and exchange their tricks in cooking. Thus interactivity was enhanced and patients could remind each other to take drugs.
Daily patients medication situation was recorded in detail. Patients and their families were instructed to fill the medication record, aiming to remind them to take proper amount of medication on time, in case there was omission[4,5].
The medication compliance of both groups was measured by a medication compliance questionnaire designed by the hospital. The fasting blood glucose, 2-h postprandial blood glucose and levels of glycosylated haemoglobin were observed. The overall nursing satisfaction between both groups was compared.
Statistical analyses were performed using SPSS21.0. All quantitative data are expressed as mean±standard variance and comparisons were made with t-test. Enumeration data are expressed as natural number (n) and percentage (%) and comparisons were made with chi-square test. P<0.05 was considered statistically significant.
As shown in Table 1, fasting blood glucose, 2-h postprandial blood glucose and levels of glycosylated haemoglobin were compared after different interfering approaches. Results showed that all indicators were significantly lower in the research group compared with the control group (p<0.05). As shown in Table 2, the total medication compliance between both groups were observed and compared. Results showed that the total medication compliance of the research group was significantly greater than that of the control group (p<0.05). As shown in Table 3, the overall nursing satisfaction between both the groups were observed and compared. Results showed that the overall nursing satisfaction of the research group was significantly higher than that of the control group (p<0.05).
| Group | Fasting blood glucose (nM) | 2-h postprandial blood glucose (nM) | Glycosylated haemoglobin (%) |
|---|---|---|---|
| Control group (n=80) | 6.8±3.1 | 8.2±5.3 | 7.6±3.3 |
| Research group (n=80) | 4.8±0.9 | 5.0±1.5 | 4.9±0.8 |
| t | 6.32 | 4.27 | 4.56 |
| P | <0.05 | <0.05 | <0.05 |
Table 1: Comparison of Blood Glucose after Intervention
| Group | Cases | Complete compliance | Partial compliance | None compliance | Total medication compliance rate |
|---|---|---|---|---|---|
| Control group | 80 | 66 | 10 | 4 | 76(95.00) |
| Research group | 80 | 40 | 14 | 26 | 54(67.50) |
| X2 | 12.19 | ||||
| P | <0.05 |
Table 2: Comparison of Total Medication Compliance Rates
| Group | Cases | Very satisfactory | Satisfactory | Unsatisfactory | Overall nursing satisfaction |
|---|---|---|---|---|---|
| Control group | 80 | 60 | 19 | 1 | 79 (98.75) |
| Research group | 80 | 38 | 22 | 20 | 60 (75.00) |
| X2 | 7.60 | ||||
| P | <0.05 |
Table 3: Comparison of Overall Nursing Satisfaction
With improved living standards demands for medical service are also elevated. In the nursing respect, application of routine nursing care only is far from sufficing patients’ demands, which would also impede the development of nursing course. For those with diabetes mellitus and tumour, drug and therapeutic efficacy would be greatly hampered if they do not take medication properly, such as increasing or reducing dosage without permission, not taking medicine on time, which would fail to control the level of bloodglucose and lead to disease progression. Therefore, a scientific medication compliance nursing model could provide a more comprehensive, scientific and normative medication guides for patients. With humanization philosophy, we could provide a more comfortable and better nursing care for patients to improve medication compliance[6,7].
Patients with diabetes further complicated by tumour would suffer from both physical pain and psychologic stress, resulting in various negative emotions, such as panic, anxiety, unease, depression and agitation[8-13]. With poor psychological state, patients are often unwilling or even refuse to take medication. Therefore, there is a need to enhance communication with patients, understand their psychological status and provide effective guidance. Based on routine nursing care, medication compliance nursing model could help enhance patients’ willingness to take medication. The interfering nursing care includes psychological guidance, health publicity, daily supervision of medication and the like, which make the interfering regimen more planned, personalized and targeted[14-17]. This interfering regimen could help patient deeply understand that it is important to follow the doctors’ advice and promote their consciousness to take medication, thus leading to better efficacy.
Results from this study indicated that the medication compliance of the research group was greater than that of the control group (p<0.05); the fasting blood glucose, 2-h postprandial blood glucose and levels of glycosylated haemoglobin in the research group were significantly lower compared with the control group (p<0.05); the overall nursing satisfaction of the research group was significantly higher than that of the control group (p<0.05). Above findings fully indicate that medication compliance nursing model could apparently improve the quality of care and medication compliance, thus facilitating recovery.
In summary, application of medication compliance nursing model on diabetic patients with tumour could apparently improve their medication compliance and control the level of blood glucose, thus improving the quality of life.
References
- Shun-qun L, Jie Y, Guo-Yuan Y. Nursing methods for improving the medication compliance of diabetic patients with tumor. Chin J Clin Oncol 2015;22(08):632-5.
- Biao D, Wen H, Cheng-Ting Q, Xiao-Li H, Mei-Fang G. Analysis of patients’ medication compliance and influence factors after percutaneous coronary intervention. World Clin Medic 2017;38(03):174-9.
- Hong-Mei Y, Hui-Jun L. Effect of pharmaceutical intervention on drug compliance and drug adverse peactions in the patients with type 2 diabetes mellitus. China Modern Doctor 2017;55(18):95-8.
- Ofori-Kwakye K, Mfoafo KA, Kipo SL, Kuntworbe N, El Boakye-Gyasi M. Development and evaluation of natural gum-based extended release matrix tablets of two model drugs of different water solubilities by direct compression. Saudi Pharm J 2016;24(1):82-91.
- Attari Z, Bhandari A, Jagadish PC, Lewis S. Enhanced ex vivo intestinal absorption of olmesartanmedoxomilnano suspension: Preparation by combinative technology. Saudi Pharm J 2016;24(1):57-63.
- Xiao-Juan M, Wei Z, LI-Li D, Jing L, Hui-Qin C. Effect of personalize nursing care on type 2 diabetic patient with complications. Anhui Med J 2017;38(09):1211-3.
- Brogan RA, Malkin CJ, Batin PD, Simms AD, McLenachan JM, Gale CP. Risk stratification for ST segment elevation myocardial infarction in the era of primary percutaneous coronary intervention. World J Radiol 2014;6(08):865-72.
- Zhou H, He XY, Zhuang SW, Wang J, Lai Y, Qi WG, et al. Clinical and procedural predictors of no-ref low in patients with acute myocardial infarction after primary percutaneous coronary intervention. World J Emerg Med 2016;5(02):96-102.
- Ying-Mian L, Dong-Qing L, Xiu-Hua L, Song-Bo Z, Su-Min J, Zhi-Min L. Comprehensive nursing management of diabetic patients with tumor. Hebei Medicine 2016;38(16):2555-7.
- Abdel Moty SG, Hussein MA, Abdel Aziz SA, Abou-Salim MA. Design and synthesis of some substituted thiazolo [3, 2-a] pyrimidine derivatives of potential biological activities. Saudi Pharm J, 2016; 24(2):119-32.
- Ge S, Wang L, Ma J, Jiang S, Peng W. Biological Analysis On Extractives of Bayberry Fresh Flesh by Gc-Ms. Saudi J Biol Sci 2018;25(4):816-8.
- Gao W, Wang Y, Wang W, Shi L. The First Multiplication Atom-Bond Connectivity Index of Molecular Structures in Drugs. Saudi Pharm J 2017;25(4):548-55.
- Borgo M, Martini M, Bragazzi NL, Paluan F, Gorini I, Vecchio I, et al. Corpus Loquens: The Speaking Body and Abele De Blasio (1858-1945). Acta Medica Mediterr 2017;33(1):95-100.
- Pati NB, Gupta VRM, Mayasa V, Velivela SMD, Hussain A. Rethinking Chronic Pain Treatment with Opioids. Indian J Pharm Sci 2017;79(6):849-57.
- Şavluk ÖF, Kuşçu MA, Güzelmeriç F, Gürcü ME, Erkılınç A, Çevirme D, et al. Do Preoperative Oral Carbohydrates Improve Postoperative Outcomes in Patients Undergoing Coronary Artery Bypass Grafts? Turk J Med Sci 2017;47(6):1681-6.
- Khayyat SA, Sameeh MY. Bioactive Epoxides and Hydroperoxides Derived From Naturally Monoterpene Geranyl Acetate. Saudi Pharm J 2018; 26(1):14-19.
- Li W, Jia M, Wang J, Lu J, Deng J, Tang J. Association of Mmp9-1562C/T and Mmp13-77a/G Polymorphisms with Non-Small Cell Lung Cancer in Southern Chinese Population. Biomolecules 2019;9(3):107.