- *Corresponding Author:
- Bo Liu
Department of Critical Care Medicine, West China Hospital, Sichuan University
E-mail: liubojjfy@163.com
| This article was originally published in a special issue,“Role of Biomedicine in Pharmaceutical Sciences” |
| Indian J Pharm Sci 2023:85(2) Spl Issue “182-192” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the relationship between obstructive sleep apnea hypopnea syndrome complicated with various traditional Chinese medicine syndromes of hypertension and plasma homocysteine level, patients were divided into liver-fire excess syndrome, yin deficiency and yang excess syndrome, phlegm-blood stasis syndrome, yin deficiency and yang deficiency syndrome based on the traditional Chinese medicine syndrome type standard of hypertension complicated obstructive sleep apnea hypopnea syndrome. General data, body mass index values, apnea and hypopnea index, oxyhemoglobin saturation, Epworth sleepiness scale scores and homocysteine of patients were extracted and analyzed. The results revealed that the number of males was greater than that of females with a proportion of 1.5:1. The number of patients with body mass index ≥24.00 kg/m2 was obviously greater than that of patients with body mass index <24.00 kg/m2. The proportion of patients with body mass index >28.00 kg/m2 reached 59.18 %. In terms of the comparison of traditional Chinese medicine syndrome types, the proportion of patients suffering from phlegm-blood stasis syndrome was the highest, reaching 27.89 % and the proportion of patients suffering from yin deficiency and yang deficiency syndrome is the lowest, amounting to 22.45 %. In homocysteine examination, the homocysteine of syndrome was increased in order of yin deficiency and yang excess, phlegm-blood stasis, yin deficiency and yang deficiency and liver-fire excess. The results revealed that the syndrome type of phlegm-blood stasis was significant among patients with obstructive sleep apnea hypopnea syndrome in the distribution of traditional Chinese medicine syndrome types. This syndrome type showed significant statistical meaning in age, neck circumference, apnea and hypopnea index, average oxyhemoglobin saturation, triglyceride and overall difference in blood glucose fasting state. The severity of obstructive sleep apnea hypopnea syndrome was positively correlated with homocysteine and apnea, and hypopnea index was also positively correlated with homocysteine and was negatively correlated with lowest oxygen saturation. Lowest oxygen saturation was negatively correlated with homocysteine.
Keywords
Obstructive sleep apnea hypopnea syndrome, hypertension, traditional Chinese medicine, homocysteine, hypoxemia
Obstructive Sleep Apnea Hypopnea Syndrome (OSAHS) mainly refers to a disease in which although patients continue to breathe forcefully during sleep development, it causes repeated hypoxia of the oropharyngeal sinus wall, resulting in collapse of airway function and significant reduction or interruption of pulmonary airflow dynamics, which can lead to intermittent disturbances of air exchange (such as hypercapnia and hypoxemia) and sleep fragmentation[1-3]. OSAHS is one of the most common and harmful systemic diseases belonging to Sleep Apnea and Hypopnea Syndrome (SAHS) and its main symptoms are characterized by nocturnal snoring, apnea, early morning headache and dry mouth on clinicopathology[4-6]. According to statistics, the number of patients with complications of hypertension accompanied by severe spontaneous sleep breathing and spontaneous apnea is only about 30 %-50 % of the patients each year. Of the total number of hypertensive patients who died of previous OSAHS, the proportion of patients with previous cardiac organic hypertension syndrome is only about 50 %-60 % of the patients. In patients with resistant hypertension, the prevalence of OSAHS is high, up to 82 %[7-9].
Apnea and Hypopnea Index (AHI) is one of the important criteria for judging OSAHS and is usually used in combination with sleep respiratory testing for Oxyhemoglobin Saturation (SaO2) to determine the severity of OSAHS[10,11]. Some researchers point out that there is a positive correlation between Neck Circumference (NC) and the normal sleep respiratory hypopnea index AHI in patients with OSAHS. Similarly, to some extent, NC examination can be used as an important indicator for detecting OSAHS and even help predict the severity of OSAHS; while hypertensive patients or hypertensive patients with OSAHS are accompanied by an increase in AHI, a decrease in SaO2, an increase in Body Mass Index (BMI) and an increase in blood pressure[12-14]. With the increase of AHI level, the blood pressure variability of patients increases at night and the incidence of systemic damage severity and other symptoms of severe target organ damage will be correspondingly increased; other studies have reported that OSAHS level can directly increase the incidence of target organ vascular damage syndrome in elderly patients by aggravating plasma glucose and lipid metabolism disorders, so that the condition and serious harm of elderly patients are significantly relatively increased[15-17]. Therefore, dynamic comprehensive analysis and evaluation of early patients, early diagnosis, intervention and treatment are of great academic significance for evaluating the prognosis of early hypertension and cancer patients with other OSAHS lesions.
At present, there is no specific disease name and relatively uniform syndrome type standard for the two combined diseases in Traditional Chinese Medicine (TCM), and the “snoring, snoring sleep” and “vertigo, headache” recorded in the ancient books are mostly simple and intuitive generalizations of the symptoms of diseases by many ancient physicians[18-20]. For condition differentiation and therapy, modern doctors rely primarily on individual medical experience. They lack persuasion because they are sensitive to subjective concepts, such as the patient’s description of the ailment and objective environmental interference factors, which impacts TCM’s unique efficacy in the prevention and treatment of this disease. The unique “syndrome differentiation and treatment” in traditional medicine is the core of guiding clinical diagnosis and treatment. Only the correct “syndrome differentiation” can be more suitable for the nature of the disease and “treatment according to the syndrome”. Starting from the differentiation of disease syndrome types, relying on the existing detection indicators of modern medical laboratories, objective evidence is provided and a more standardized, unified and objective syndrome differentiation standard is established, which is more conducive to the implementation of the characteristic treatment of OSAHS with hypertension by TCM[21,22].
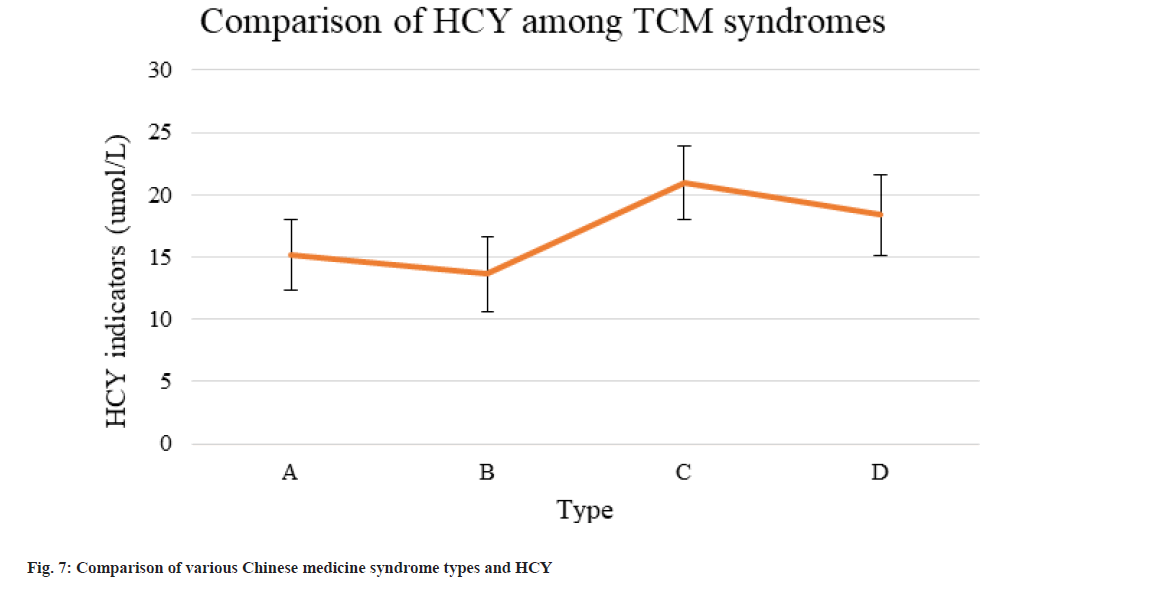
Homocysteine (HCY) is a type of intermediate amino acid generated when Methionine (Met) is converted to Cysteine (Cys). HCY in the human body can be routinely catabolized under physiological settings, hence the content has been kept low. With the gradual increase of serum HCY level, the risk of accidents after the onset of coronary heart disease, peripheral vascular disease and various cerebrovascular diseases has been greatly increased[23,24]. Complete experimental data can confirm that HCY is an independent risk factor for coronary artery, brain and peripheral atherosclerosis. The level of blood HCY in patients with OSAHS is still controversial. Some studies have observed a significant increase in blood HCY in patients with OSAHS, which may be a biomarker for cardiovascular disease and some believe blood HCY not increased[25]. It aims to collect medical history information from OSAHS patients with hypertension, combine it into data, and use cluster analysis to extract the characteristics of relevant TCM symptom types. The statistical relationship between TCM syndrome types of OSAHS combined with hypertension and plasma HCY was studied in order to give a foundation for diagnosing OSAHS combined with hypertension.
The paper’s organization paragraph is as follows; the materials and methods are presented in section 2. Section 3, discusses the experiments and results. Section 4 consists of the discussion section. Finally, in section 5, the research work is concluded.
Materials and Methods
Study subjects:
154 outpatients and inpatients with OSAHS complicated with hypertension were enrolled from open database from June 2021 to January 2022. Because some patients had problems such as missing data of plasma HCY or inability to cooperate with sleep monitoring, 7 patients dropped out and 147 patients finally met the criteria.
Diagnostic criteria for OSAHS[26]: Epworth Sleepiness Scale (ESS) was used and according to the clinical application treatment criteria of OSAHS in the Guidelines for the Diagnosis and Treatment of Obstructive Sleep Apnea-Hypopnea Syndrome (Basic Edition); the patient’s relevant medical history, signs, etc., and the evaluation results after clinical monitoring by multimode electric conductor sleep quality monitor. Irregular snoring and a jumbled sleep architecture, as well as respiratory arrest or frequent awakenings during the night and significant daytime drowsiness (ESS score >9 points), AHI ≥5 times/h; if the daytime ESS score was <9 points, but AHI ≥10 times/h (even AHI ≥5 times/h and one or more OSAHS combination diseases occurred in cognitive impairment, severe hypertensive symptoms, patients with coronary atherosclerotic heart disease, patients with chronic cerebrovascular disease, hyperglycemia, and insomnia), it was helpful to further confirm the diagnosis. AHI and the Lowest Arterial Oxygen Saturation (LSaO2) were used as the reference criteria as shown in Table 1.
| Severity | AHI | LSaO2 |
|---|---|---|
| Mild | 5-15 times/h | 85 %-90 % |
| Medium | 16-30 times/h | 80 %-84 % |
| Severe | >30 times/h | <80 % |
Table 1: Osahs Severity Grading Table
Diagnostic criteria for hypertension: The diagnosis and treatment specifications for hypertension refer to the 2018 edition of Chinese guidelines for the prevention and treatment of hypertension[27], and hypertension can be diagnosed if the following narrative conditions were met. In the absence of antihypertensive drugs, blood pressure was measured three times on different days and systolic blood pressure ≥140 mmHg and diastolic blood pressure ≥90 mmHg. The patient had a previous history of hypertension and was using antihypertensive drugs, although the blood pressure was less than 140/90 mmHg, hypertension could also be diagnosed. Hypertension grading criteria are shown in Table 2.
| Grading | Systolic blood pressure | Diastolic blood pressure |
|---|---|---|
| Grade 1 | 140-159 mmHg | 90-99 mmHg |
| Grade 2 | 160-179 mmHg | 100-109 mmHg |
| Grade 3 | ≥180 mmHg | ≥110 mmHg |
Table 2: Hypertension Grading Criteria Table
Chinese medicine syndrome type standard for hypertension complicated with OSAHS[28]: According to guidance on clinical research of TMC drugs (Trial) of ministry of health industry standard in 2002 and syndromes used in clinical diagnosis of modern Chinese medicine treatment of standard in 1997, patients with hypertension and complicated OSAHS syndrome were divided into liver-fire excess syndrome, yin deficiency and yang excess syndrome, phlegm-blood stasis syndrome and yin deficiency and yang deficiency syndrome combined with the relevant standard contents in the new version of blood stasis syndrome standard revised and confirmed by the former national traditional Chinese and western medicine integrated learning of blood stasis syndrome special committee.
Inclusion criteria: Patients with OSAHS and hypertension illnesses who fulfill the treatment specifications of traditional Chinese and western medicine; patients aged 20 y to 80 y old, male or female; patients who meet the national diagnosis and treatment specifications of TCM; patients who agreed and obeyed the arrangement.
Exclusion criteria: Patients not meeting the inclusion criteria; pregnant or lactating women; patients combined with mental illness; snoring patients with central nervous system injury and congenital deformity of the face and neck structure due to brain injury; recent use of drugs affecting sleep (such as sedative and hypnotic drugs) or use of TCM treatment in recent 2 w; patients with acute infection, chronic inflammatory disease, etc.
Dropout criteria: Patients not cooperating with information collection; patients unwilling to participate in the exploration halfway; patients lacking the detection values of laboratory indicators such as plasma HCY.
General information:
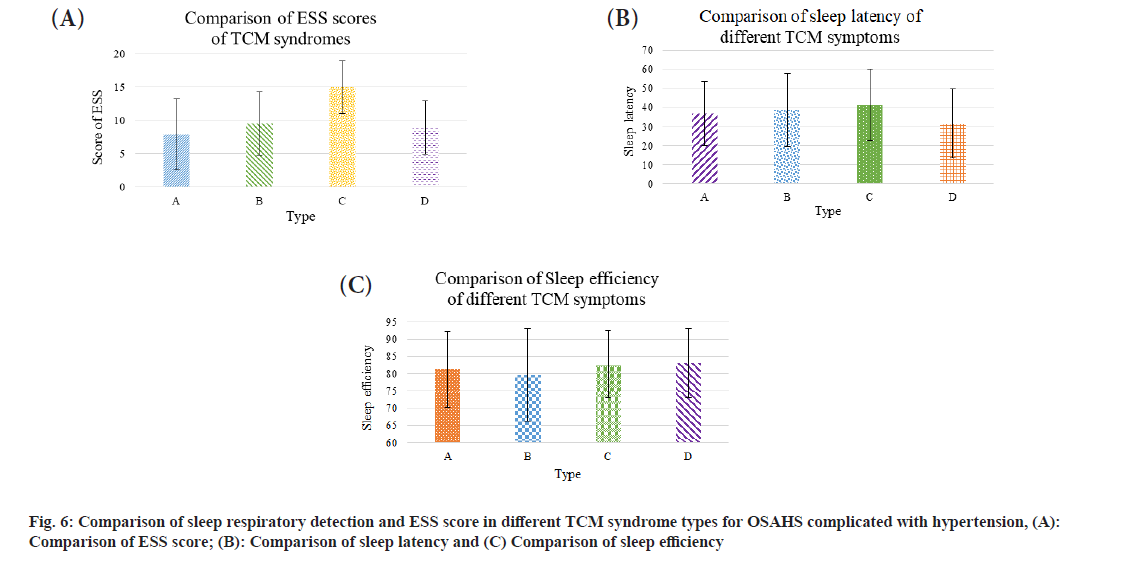
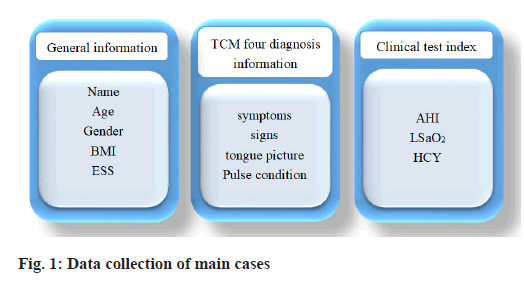
The general information of patients with OSAHS complicated with hypertension were collected, including gender, age, occupation, blood pressure, BMI, etc. After studying the literature and interviewing relevant specialists, the primary clinical symptoms, tongue coating, pulse and other details of OSAHS complicated with hypertension were determined. The OSAHS complex with hypertension data collection table was created. The information content is shown in fig. 1.
Indicator detection methods:
Measurement of height and weight: The next morning after monitoring sleep conditions, height and weight were measured by patients after defecation, removing shoes, socks and stand posture and patients maintained vertical standing position. Patients looked ahead with both eyes, the error was 3 mm. When weighing, clothes and shoes should be removed as far as possible. After the number was stable, it should be read and the weight of the remaining clothes should be subtracted, with an error of 0.5 kg.
BMI: BMI calculation equation is as follows;
BMI=Weight (kg)/height (m2)×(kg/m2) (1)
According to the adult weight determination criteria specified in 2013, adult BMI <18.5 kg/m2 is defined as lean, 18.5-23.9 kg/m2 as normal BMI, ≥24 kg/m2 as overweight and ≥28 kg/m2 as obese.
AHI, LSaO2: Patients were monitored by polysomnography (10-channel polysomnography SOMNOscreenTM plus by SOMNOmedics (Germany). In order to reduce the impact of environmental changes and mental factors on the sleep of the subjects, the subjects were arranged to perform polysomnography after 2 d of hospitalization. The subjects should not drink alcohol, tea, coffee, cola, chocolate and other caffeine-containing beverages 24 h before monitoring; in order to avoid the subjects from affecting the sleep quality at night due to lunch break, the subjects did not have lunch break on the day of monitoring; in order to facilitate the examination, the subjects wore detachable loose pajamas on the night of monitoring. The monitoring time was from 21:00 at night to 06:00 in the next morning. The monitoring time should not be less than 7 h. The monitoring results can only be used when the sleep onset time was more than 5 h. If the sleep onset time was not more than 5 h, the test should be repeated at another day. The original parameters monitored were automatically analyzed by sleep analysis software and then manually reviewed and corrected by a professional.
ESS score: The subjects were scored according to ESS by means of inquiry, which was recorded.
Plasma HCY:
Because alcohol, caffeine, a high-Met diet and other foods alter the synthesis and metabolism of plasma HCY, patients were requested to abstain from consuming these items the day before the test and fasting blood tests were performed the next morning after sleep monitoring. Plasma HCY was detected by the laboratory personnel using Beckman biochemical analyzer 2700 and the detection method was enzymatic detection. In order to reduce subjective errors, before collecting cases, the chief physician of TCM trained the investigator and the physician collecting the medical history, unified the standard of tongue vein and the investigator and another trained physician collected the four diagnostic information of the patients according to the four diagnostic information in the “OSAHS with hypertension case data collection form” by look, listen, question and feel the pulse.
Statistical analysis:
Statistical Package for the Social Sciences (SPSS) 23.0 software package was adopted for statistical data analysis. According to Shapiro-Wilk test, whether data conformed to normal distribution was verified. Measurement data between multiple groups conforming to normal distribution were compared by one-factor multi-sample mean. The data between two groups were analyzed by independent sample t test. Measurement data that didn’t conform to normal distribution were analyzed by rank sum test. Enumeration data were analyzed by Chi-square (χ2) test. p<0.05 indicated that the differences revealed statistical meaning.
Results and Discussion
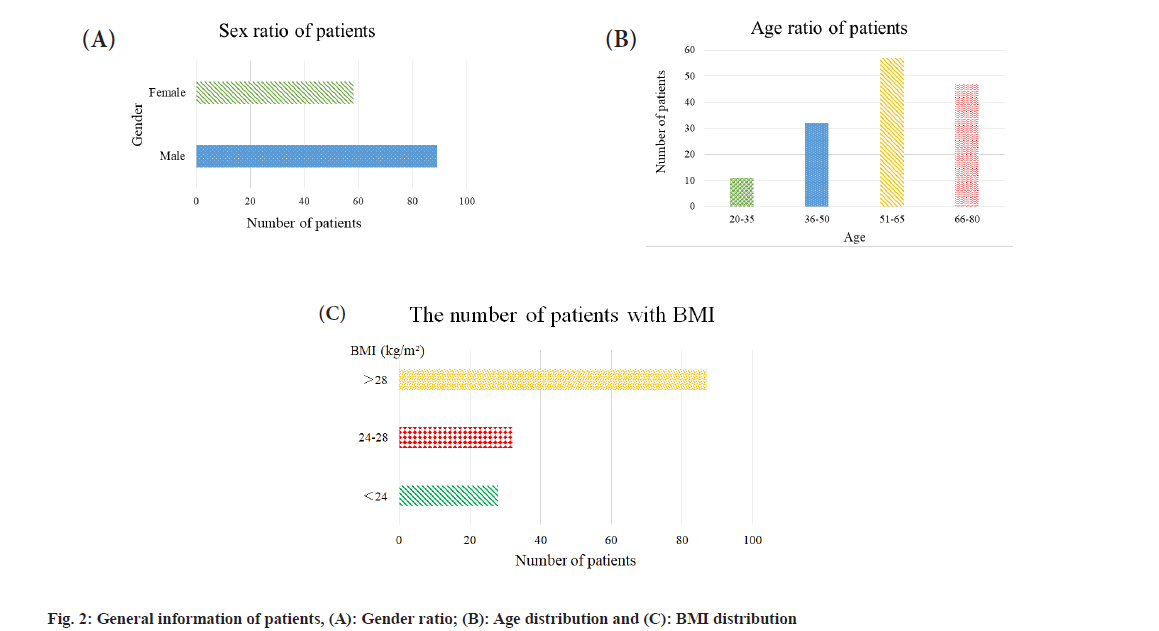
Finally, 147 patients were included, with a male-tofemale ratio of roughly 1.5, with 60.5 % males and 39.5 % females. The incidence of OSAHS with hypertension in males was more than that in females (fig. 2a). The oldest patient was 78 y old and the youngest was 21 y old, with an average age of 54.87±12.62 y. Patients with OSAHS and hypertension were mostly middle-aged and elderly (fig. 2b). Among the patients, 80.95 % had BMI ≥24.00 kg/m2 and 19.05 % had BMI <24 kg/m2. Patients with BMI ≥24.00 kg/m2 had significantly higher number of patients than those with BMI <24.00 kg/m2, of which 59.18 % had BMI >28.00 kg/m2 indicating that obesity may be closely related to OSAHS with hypertension as shown in fig. 2c.
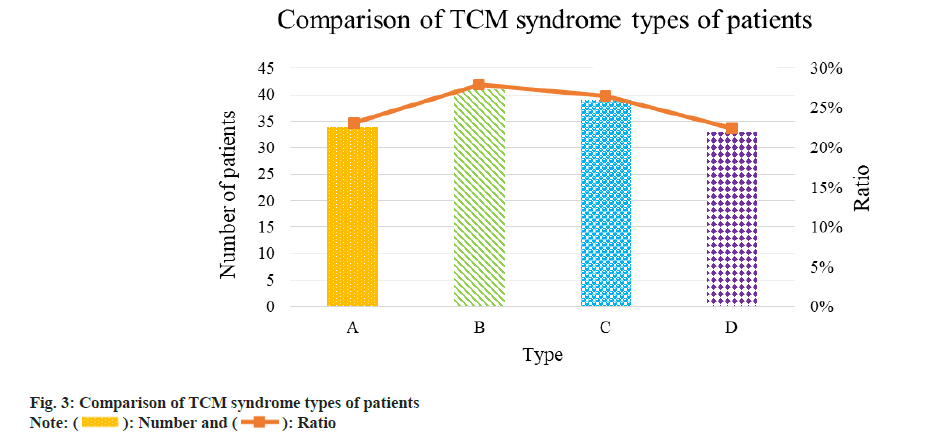
Studies have shown that in the comparison of TCM syndrome types in OSAHS patients with hypertension, phlegm-blood stasis syndrome accounted for the largest proportion and the percentage of each was as follows; 41 cases (27.89 %) of phlegm-blood stasis syndrome >39 cases (26.53 %) of yin deficiency and yang excess type >34 cases (23.13 %) of liver-fire excess type >33 cases (22.45 %) of deficiency of yin and yang syndrome, suggesting that phlegm-blood stasis syndrome may be the main type of OSAHS with hypertension. It was discovered that phlegm-blood stasis in the body may be a significant factor in OSAHS and hypertension (fig. 3). A, B, C and D are phlegmblood stasis, yin deficiency and yang excess, liver-fire excess and deficiency of yin and yang, respectively.
According to the hypertension grading criteria, OSAHS patients with hypertension were categorized into three grades. Patients with moderate to severe hypertension had the highest BMI index and the difference was statistically significant (p<0.05); in the rank correlation test of BMI and AHI, it was found that AHI was negatively correlated with BMI (R=0.439, p<0.05). The NC of OSAHS patients with hypertension was significantly better in severe patients than in mild and moderate patients (p<0.05); the rank correlation test of AHI and NC in OSAHS patients with hypertension revealed that AHI was significantly related to NC (R=0.392, p<0.05); the rank correlation test of MSaO2 in patients undergoing sleep respiratory monitoring showed that AHI was negatively correlated with MSaO2 in such patients (p<0.05); the rank correlation test of AHI and Triglyceride (TG) in biochemical blood lipids showed that R=0.387, p<0.05; the results showed that AHI was positively correlated with TG values; the conclusions stated above were statistically significant. Other indicators, such as Fasting Blood Glucose (FBG), glycation, Total Cholesterol (TC) and others, were not statistically significant. The BMI and NC indexes of patients with different severities of OSAHS are shown in fig. 4 and the relevant tests of AHI are shown in Table 3.
| Variable | R | p |
|---|---|---|
| BMI | 0.439 | <0.001 |
| Neck girth | 0.392 | <0.001 |
| MSaO2 | -0.421 | <0.050 |
| Fasting blood sugar (FBS) | 0.026 | 0.523 |
| Saccharify | 0.048 | 0.874 |
| TG | 0.387 | <0.050 |
| TC | -0.073 | 0.536 |
Table 3: Pearson Correlation Test Between Ahi and Each Index of Osahs Patients with Hypertension
Because AHI conformed to normal and the variance also conformed to single variance homogeneity, when oneway analysis of variance and calculation results were performed, the LSD method should generally be used to obtain the test results for the comparison of the two variances; although LSaO2 also conformed to normal distribution, because its variance was heterogeneous, the Games Howell method was used to test the comparison of the two variances. The main syndrome types of each stage were compared with other AHI and LSaO2 types by single factor analysis of variance and comparative experiments, and the results can also show that in the late stage of OSAHS syndrome or in patients with other acute hypertension, there was an important difference between the prognosis of AHI and LSaO2 types and the main clinical indications at each stage, and it also had significant clinical or statistical value and statistical significance of diagnosis (p<0.05). The MSaO2 readings were more substantially different between liver-fire excess and liver-fire and yin deficiency and yang excess than the other TCM condition kinds (p<0.05); the differences between yin and yang deficiency syndrome and phlegm-blood stasis and yin deficiency and yang excess were statistically significant (p<0.05); the remaining comparisons and differences were not statistically significant (p>0.05) (fig. 5). A, B, C and D are phlegm-blood stasis, yin deficiency and yang excess, liver-fire excess, and deficiency of yin and yang, respectively.
The results of sleep efficiency, sleep latency and ESS evaluation in the results of rank sum test of each syndrome type suggested OSAHS had more statistical significance than the differences in sleep efficiency, sleep latency and ESS evaluation among syndrome types of combined hypertension (p<0.05). ESS evaluation had certain statistical meaning in contrast with yin deficiency and yang excess, liver-fire excess and deficiency of yin and yang in terms of phlegmblood stasis (p<0.05) and the other differences had no statistical meaning. ESS evaluation was highest in deficiency of yin and yang, sleep latency was greatest in liver-fire excess, but sleep onset efficiency was poor in yin deficiency and yang excess (fig. 6). A, B, C and D are phlegm-blood stasis, yin deficiency and yang excess, liver-fire excess, and deficiency of yin and yang.
Since HCY was not normally distributed, the results after rank sum test suggested that the difference of HCY levels among syndrome types of OSAHS with hypertension had statistical value (p<0.05). The HCY levels among different syndrome types were compared in detail (fig. 7). A, B, C, and D are phlegm-blood stasis, yin deficiency and yang excess, liver-fire excess and deficiency of yin and yang. As a result of yin deficiency and yang excess, phlegm-blood stasis, yin and yang deficit and liver-fire excess syndrome, the HCY values of OSAHS patients with severe hypertension rose.
The symptoms of OSAHS are mainly reflected in the manifestations of mental collapse such as snoring at night or during sleep, or daytime lethargy, drowsiness and fatigue or poor physical fitness; therefore, the modern TCM community in China generally classifies insomnia as the TCM category of “snoring, snoring sleep” sleep syndrome according to its main symptoms. The main problem of the condition, according to Huang Wending, is airway stenosis or occlusion, and a rise in total BMI levels leads to a quick increase in the prevalence of OSAHS[29]. In conjunction with current TCM treatment standards, it is categorized into four categories; yin deficiency and yang excess, phlegmblood stasis, yin and yang deficiency and liver-fire excess. Based on considerable statistical research and data analysis, the results of this examination show that most patients with hypertension complicated with OSAHS suffer from phlegm-blood stasis syndrome. As the disease continues and progresses, deficiency syndromes such as deficiency of both qi and yin gradually become common. Besides, it is found out that age, AHI and hypotensive grading are also related to syndrome types. There are significant differences in AHI levels among different syndrome types during sleep. As a result, AHI levels of phlegm-blood stasis syndrome are syndrome of qi stagnation and blood stasis, and syndrome of deficiency of both qi and yin. OSAHS is a clinical syndrome characterized by snoring during sleep at night, resulting in diminished sleep quality, repeated nocturnal awakening states and daytime lassitude and fatigue. It is closely related to various risk factors such as weight, gender, NC and anatomical abnormalities of the upper airway; the rise in the overall level of weight indicators has led to a rapid increase in the prevalence of OSAHS[30]. The main pathogenesis of OSAHS in sleep is mainly summarized as follows. When a patient’s upper and lower airways feel stenosed or severely obstructed during long-term sleep activities, a large number of hypoxemia and a large number of blood and hypercapnia occur and a variety of chemical sensors from the peripheral central system and the central peripheral nervous system are continuously stimulated, until stimulation excites the parasympathetic nerve in the body, leading to sleep awakening at night[31]. The gold standard for the diagnosis of OSAHS is PSG (sleep respiratory testing), AHI (sleep respiratory index), which is currently used as an indicator for the diagnosis and evaluation of the severity of OSAHS and often used as the basis to grade the severity of the disease.
The research results demonstrated that the number of patients with complicated OSAHS and phlegm-blood stasis syndrome was the greatest among all patients with hypertension. There were 41 cases with phlegm-blood stasis syndrome (27.89 %), 39 cases with yin deficiency and yang excess syndrome (26.53 %), 34 cases with liver-fire excess syndrome (23.13 %) and 33 cases with yin deficiency and yang deficiency (22.45 %). To sum up, the distribution of hypertension complicated with OSAHS in Chinese medicine syndrome types was the result of the interaction among multiple reasons. According to the severity of AHI and OSAHS (mild, moderate and severe), patients with severe syndromes had a higher average BMI and BMI values than patients with light and moderate syndromes, indicating that a higher average weight reflected the worse disease. AHI level was clearly positively linked with BMI, according to the results of a Pearson correlation test on AHI level and BMI of individuals with hypertension exacerbated by OSAHS. Previous studies also showed that overweight or obesity was one of the independent risk factors causing sleep apnea hypopnea and hypopnea. This result indicated that the risk of suffering from the disease was greatly increased with the enhancement of BMI and the physical condition of patients with OSAHS might be exacerbated. Hence, patients with OSAHS must control their weight at all times. The research also suggested that the NC of patients with severe hypertension and OSAHS were larger than that of patients with mild and moderate hypertension and OSAHS. According to positive rank relationship test on AHI and NC of patients with hypertension and OSAHS, AHI was remarkably positively correlated with NC, which proved that NC could be viewed as an index of measuring the severity of OSAHS patients. Sleep apnea assay and mean nocturnal SaO2 were both negatively correlated with AHI and the differences had statistical values. The concentration of HCY in plasma affected the blood pressure levels of patients with OSAHS and severe hypertension. In addition, plasma HCY increased with the increase in AHI values of patients, suggesting that plasma HCY level in human body was the independent risk factor affecting the severity of OSAHS patients complicated with hypertension. The correlation between HCY and the severity of OSAHS among 147 patients was analyzed in the research, which revealed that the severity of OSAHS was positively correlated with plasma HCY level. The conclusion was highly consistent with the result of the present studies. As the disease progresses, patients HCY level rose. To conclude, HCY level is a key factor of suggesting complicated OSAHS disease among hypertension patients.
There are still some limitations in this research. More TCM syndrome types should be included in future studies. The differences in various indexes of patients and the changes in indexes corresponding to each syndrome type under specific Chinese medicine syndrome types need to be discussed to provide reference basis for future clinical diagnosis and treatment.
147 cases of OSAHS with hypertension were found to have a greater incidence in males than in females and the incidence was higher in those with excessive BMI and middle-aged and elderly people. In the distribution of TCM syndrome types in OSAHS patients with hypertension, phlegm-blood stasis syndrome accounted for a high proportion and the proportion was 41 cases (27.89 %) of phlegm-blood stasis syndrome >39 cases (26.53 %) of yin deficiency and yang excess syndrome >34 cases (23.13 %) of liver-fire excess syndrome >33 cases (22.45 %) of yin and yang deficiency syndrome. There were significant differences in age, NC, AHI, SaO2, TG and FBG among syndrome types in OSAHS patients with hypertension. OSAHS severity was positively correlated with HCY; AHI was positively correlated with HCY and negatively correlated with LSaO2; LSaO2 was negatively correlated with HCY.
Data availability:
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflict of interests:
The authors declared no conflict of interests.
References
- Yang X, Niu X, Xiao Y, Lin K, Chen X. MiRNA expression profiles in healthy OSAHS and OSAHS with arterial hypertension: Potential diagnostic and early warning markers. Respir Res 2018;19(1):194.
[Crossref] [Google Scholar] [PubMed]
- Zhang J, Ren J, Sun S, Zhang Z. A study to identify obstructive sleep apnea syndrome based on 24 h ambulatory blood pressure data. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi 2022;39(1):1-9.
[Crossref] [Google Scholar] [PubMed]
- Liu Y, Han J, Ning L, Chen L, Jiang X, Ke A, et al. Cognitive function and life quality of patients with moderate-to-severe obstructive sleep apnea-hypopnea syndrome in China. Expert Rev Respir Med 2021;15(3):435-40.
[Crossref] [Google Scholar] [PubMed]
- Jiang Q, Zhulepiya S, Chen Y, Zhou X, Zhang X, Xu X, et al. Influencing factors of renal function in hypertensive patients with obstructive sleep apnea-hypopnea syndrome. Zhejiang Da Xue Xue Bao Yi Xue Ban 2016;45(3):261-7.
[Google Scholar] [PubMed]
- Casas-Méndez F, Sánchez-de-la-Torre A, Valls J, Sánchez-de-la-Torre M, Abad J, Duran-Cantolla J, et al. Lung function impairment is not associated with the severity of acute coronary syndrome but is associated with a shorter stay in the coronary care unit. J Thorac Dis 2018;10(7):4220-9.
[Crossref] [Google Scholar] [PubMed]
- Meszaros M, Tarnoki AD, Tarnoki DL, Kovacs DT, Forgo B, Lee J, et al. Obstructive sleep apnea and hypertriglyceridaemia share common genetic background: Results of a twin study. J Sleep Res 2020;29(4):e12979.
[Crossref] [Google Scholar] [PubMed]
- Domínguez-Mayoral A, Sánchez-Gómez J, Guerrero P, Ferrer M, Gutiérrez C, Aguilar M, et al. High prevalence of obstructive sleep apnea syndrome in Spain’s Stroke Belt. J Int Med Res 2021;49(10):03000605211053090.
[Crossref] [Google Scholar] [PubMed]
- Bacci MR, Emboz JN, Alves BD, Veiga GL, Murad N, Meneghini A, et al. Obstructive sleep apnea syndrome and sleep quality in hypertensive patients. Rev Assoc Méd Bras 2017;63:1055-60.
[Crossref] [Google Scholar] [PubMed]
- Zhang XQ, Zhao X, Hong PW, Zhou J, Zeng P, Liu C, et al. Change in quality of life of OSAHS patients with minimally invasive surgery or CPAP therapy: A 2-year retrospective, single-center parallel-group study. Curr Mol Med 2020;20(3):231-9.
[Crossref] [Google Scholar] [PubMed]
- Du LN, Ren R, Tan L, Li TM, Lei F, Tang XD, et al. Association between daytime sleepiness and hypertension among patients with obstructive sleep apnea-hypopnea syndrome. Zhonghua Yi Xue Za Zhi 2016;96(42):3370-4.
[Crossref] [Google Scholar] [PubMed]
- Vicente-Herrero MT, Capdevila-García L, Bellido-Cambrón MC, de la Torre RI, Lladosa-Marco S. Blood pressure and sleep apnoea hypopnoea syndrome in workers. STOP-Bang test vs. Epworth test. Hipertension Riesgo Vasc 2017;35(1):15-23.
[Crossref] [Google Scholar] [PubMed]
- Zeng X, Ma D, Wu K, Yang Q, Zhang S, Luo Y, et al. Development and validation of a clinical model to predict hypertension in consecutive patients with obstructive sleep apnea hypopnea syndrome: A hospital-based study and monogram analysis. Am J Transl Res 2022;14(2):819.
[Google Scholar] [PubMed]
- Hao Z, Qin L, Tong J, Li N, Zhai Y, Zhao Y. The differences of carotid atherosclerosis among non-OSAHS and OSAHS patients of different severities: A cross-sectional study. Sleep Breath 2021;25(2):639-48.
[Crossref] [Google Scholar] [PubMed]
- Zeng YM, Hu AK, Su HZ, Ko CY. A review of the association between oral bacterial flora and obstructive sleep apnea–hypopnea syndrome comorbid with cardiovascular disease. Sleep Breath 2020;24(4):1261-6.
[Crossref] [Google Scholar] [PubMed]
- Wang HW, Liu HM, Zheng ZY, Jia YZ, Li HR. Effect of the obstructive sleep apnea hypopnea syndrome treatment on blood pressure in patients with resistant hypertension. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2017;52(1):49-52.
[Google Scholar] [PubMed]
- Zhou L, Ouyang R, Chen P, Luo H, Liu H, Liu G. A case of severe obstructive sleep apnea hypopnea syndrome with urinary and anal incontinence. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2018;43(3):333-6.
[Crossref] [Google Scholar] [PubMed]
- Friedlander AH, Boström KI, Tran HA, Chang TI, Polanco JC, Lee UK. Severe sleep apnea associated with increased systemic inflammation and decreased serum bilirubin. J Oral Maxillofac Surg 2019;77(11):2318-23.
[Crossref] [Google Scholar] [PubMed]
- Wu Y, Hu G, Pan F, Liu J, Mo X, Xie Y, et al. Obstructive sleep apnea hypopnea syndrome was a risk factor for uncontrolled hypertension in adult snorers in South China. Clin Exp Hypertens 2016;38(5):429-34.
[Crossref] [Google Scholar] [PubMed]
- Liu Y, Tu CL, Yao WF, Yu YF, Wang Z, Hu JR. Prevalence of obstructive sleep apnea hypopnea syndrome in professional drivers and the relationship with traffic accidents. Zhonghua Yi Xue Za Zhi 2016;96(48):3902-5.
[Google Scholar] [PubMed]
- Wang YY, Guang J, Yin SK. Screening of sleep apnea syndrome-A review of current situation. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2016;30(6):505-9.
[Crossref] [Google Scholar] [PubMed]
- Chen RK, Hong C, Zhou YM, Kuang AL, Zhang YT, Qing SM, et al. Severe obstructive sleep apnea-hypopnea syndrome with dilated cardiomyopathy leading to pulmonary hypertension: Case report and literature review. Zhonghua Jie He He Hu Xi Za Zhi 2017;40(1):46-51.
[Google Scholar] [PubMed]
- Jiang Z, Chen J, Chen J, Lei Z, Chen H, Wu J, et al. Anti-inflammatory effects of paeoniflorin caused by regulation of the hif1a/miR-210/caspase1/GSDMD signaling pathway in astrocytes: A novel strategy for hypoxia-induced brain injury in rats. Immunopharmacol Immunotoxicol 2021;43(4):410-8.
[Crossref] [Google Scholar] [PubMed]
- Klobu?níková K, Šiarnik P, Siváková M, Wágnerová H, Mucska I, Kollár B, et al. Carotid intima-media thickness is not associated with homocysteine and vitamin D levels in obstructive sleep apnea. Scand J Clin Lab Invest 2017;77(4):263-6.
[Crossref] [Google Scholar] [PubMed]
- Li J, Yu LQ, Jiang M, Wang L, Fang Q. Homocysteine level in patients with obstructive sleep apnea/hypopnea syndrome and the impact of continuous positive airway pressure treatment. Adv Clin Exp Med 2018;27(11):1549-54.
[Crossref] [Google Scholar] [PubMed]
- Wu H, Yuan X, Wang L, Sun J, Liu J, Wei Y. The relationship between obstructive sleep apnea hypopnea syndrome and inflammatory markers and quality of life in subjects with acute coronary syndrome. Respir Care 2016;61(9):1207-16.
[Crossref] [Google Scholar] [PubMed]
- Buysse DJ, Hall ML, Strollo PJ, Kamarck TW, Owens J, Lee L, et al. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS) and clinical/polysomnographic measures in a community sample. J Clin Sleep Med 2008;4(6):563-71.
[Google Scholar] [PubMed]
- Liu LS, Wu ZS, Wang JG, Wang W, Bao YJ, Cai J, et al. 2018 Chinese guidelines for prevention and treatment of hypertension-A report of the revision committee of Chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol 2019;16(3):182-245.
[Google Scholar] [PubMed]
- Zhang XY. Guiding Principle of Clinical Research on New Drugs of Traditional Chinese Medicine (Trial). ScienceOpen 2002;9(1):68-73.
- Zhang P, Guo WJ. The research progress of OSAHS and cardiovascular disease. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2016;30(6):442-5.
[Crossref] [Google Scholar] [PubMed]
- Yuan F, Zhang S, Liu X, Liu Y. Correlation between obstructive sleep apnea hypopnea syndrome and hypertension: A systematic review and meta-analysis. Ann Palliat Med 2021;10(12):12251-61.
[Crossref] [Google Scholar] [PubMed]
- Fei-jie ZU, Xiao-hua ZH, Tao RY, Hao-ming TI. Clinical characteristics of aldosterone producing adenoma and idiopathic hyperaldosteronism with obstructive sleep apnea hypopnea syndrome. Sichuan Da Xue Xue Bao Yi Xue Ban 2020;51(3):298-303.
[Crossref] [Google Scholar] [PubMed]
 ): Number and (
): Number and ( ): Ratio
): Ratio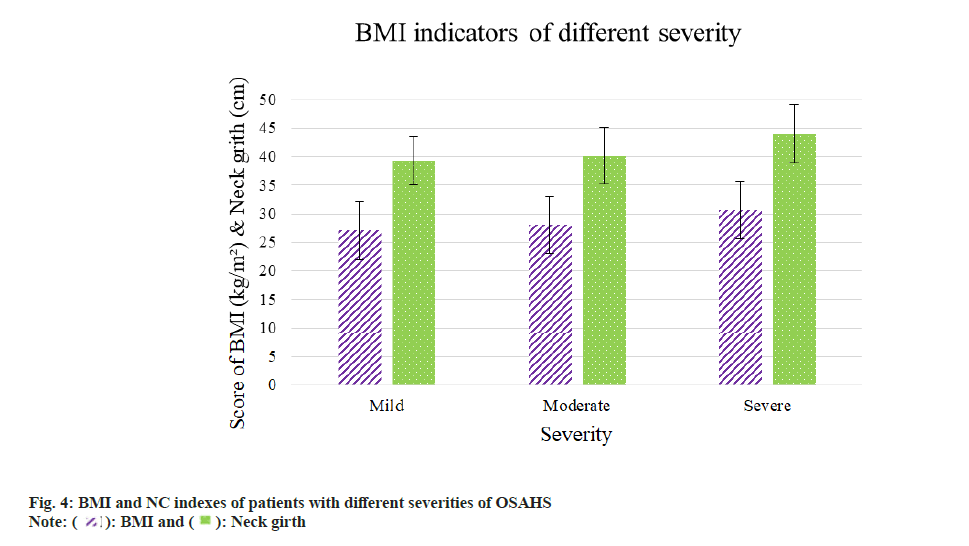
 ): BMI and (
): BMI and ( ): Neck girth
): Neck girth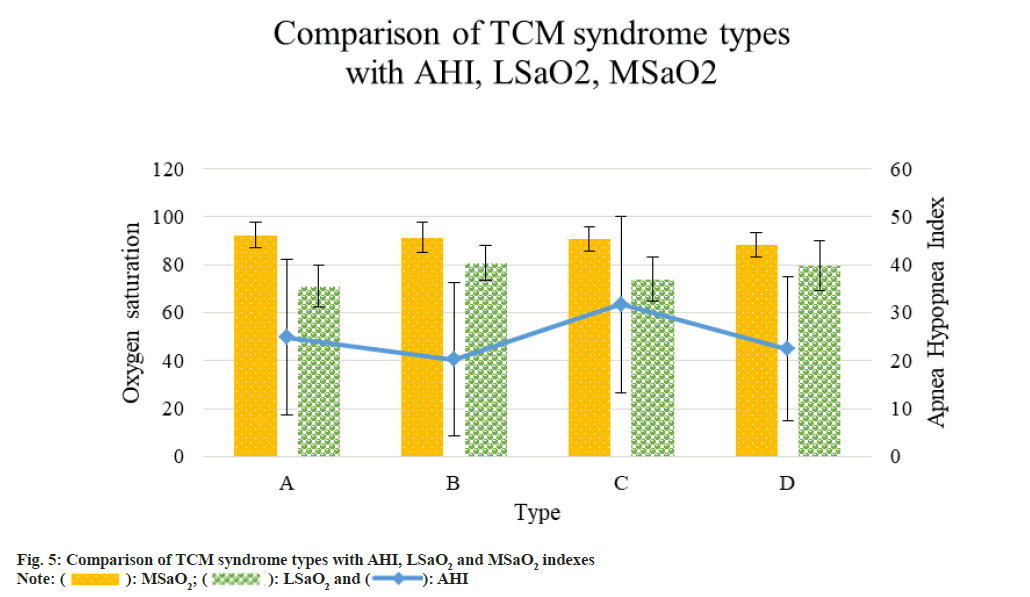
 ): LSaO2 and (
): LSaO2 and ( ): AHI
): AHI