- *Corresponding Author:
- Weihe Meng
Department of Proctology, Fengnan District Traditional Chinese Medicine Hospital, Tangshan 063000, China
E-mail: 18502261285@163.com
| This article was originally published in a special issue, “Transformative Discoveries in Biomedical and Pharmaceutical Research” |
| Indian J Pharm Sci 2023:85(4) Spl Issue “218-224” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Ulcerative colitis is a chronic inflammatory disease spreading to the colon and shows an increasing global prevalence. Its development is associated with intestinal dysbiosis, intestinal flora disorders and immune dysfunction. Recent evidence demonstrated potentially potent efficacy of traditional Chinese medicine management. The present study was undertaken to evaluate the safety and efficacy of Chaigui Ganjiang decoction plus rectal administration of Chinese herbal medicines in the treatment of ulcerative colitis. Between December 2018 and March 2021, 88 patients with ulcerative colitis diagnosed and treated in our hospital met the inclusion criteria and were recruited. They were assigned to receive mesalamine (control group) or Chaigui Ganjiang decoction plus rectal administration of Chinese herbal medicines (study group), with 44 cases in each group. Outcome measures included clinical efficacy, traditional Chinese medicine evidence score, serum inflammatory factor concentrations and adverse events. Traditional Chinese medicine interventions were associated with markedly higher treatment efficacy vs. mesalamine (p<0.05). Traditional Chinese medicine interventions provided more significant symptom remission for patients than mesalamine, as evinced by the lower traditional Chinese medicine evidence scores (p<0.05). Remarkably elevated serum interleukin-10 concentrations and reduced interleukin-17 and tumor necrosis factor-alpha concentrations in the study group suggested better inflammatory response mitigation of traditional Chinese medicine interventions than mesalamine (p<0.05). Chaigui Ganjiang decoction plus rectal administration of Chinese herbal medicines demonstrated a good safety profile vs. mesalamine by offering a lower incidence of adverse events (p<0.05). Chaigui Ganjiang decoction plus rectal administration of Chinese herbal medicines provides marked symptom remission in patients with ulcerative colitis, potentiates clinical efficacy, alleviates inflammatory responses and produces fewer adverse events.
Keywords
Chaigui Ganjiang decoction, rectal administration of Chinese herbal medicines, ulcerative colitis, inflammatory bowel disease
Ulcerative colitis is a chronic nonspecific inflammatory bowel disease[1], characterized by mucosal damage, erosions and ulcers caused by autoimmune diseases and rectal and sigmoid ulcers, and local bleeding may also be visible under endoscopy[2,3]. Ulcerative colitis lesions are mainly located in the mucosa and sub mucosa of the large intestine, with clinical manifestations such as diarrhea, purulent mucosal stools and abdominal pain[4]. The disease may occur across all age groups and is clinically characterized by a long disease course, high recurrence rate and susceptibility to carcinoma[5]. In recent years, the prevalence of ulcerative colitis has been escalating[6]. The main medications prescribed for the treatment of ulcerative colitis are amino salicylic acid, corticosteroids and immunosuppressive agents, which, however, are associated with frequent relapse, adverse effects and suboptimal efficacy[7,8]. Thus, there is an urgent need to identify better treatment methods. Compared to Western medicine, which shows stagnant development in the therapeutic efficacy of ulcerative colitis, Traditional Chinese Medicine (TCM) demonstrates marked therapeutic benefits[9], with stable efficacy and few side effects[10,11]. In TCM, ulcerative colitis is classified as "intestinal fetish", "dysentery", "stagnation", "intestinal wind" and "diarrhea", which necessitates the elimination of chill in the body and promotion of righteous Qi. Oral administration of TCM herbal decoction is the most frequent approach with established clinical efficiency[12]. In addition, Chinese herbal enema is one of the main practices in the clinical treatment of ulcerative colitis, which facilitates the absorption of drugs by the intestinal mucosa to achieve therapeutic effects. The combination of oral administration of herbal decoctions and Chinese medicine enema can regulate the internal organs, expel the external evils and realize the management of both symptoms and root causes. Thus, the present study was performed to evaluate the safety and efficacy of Chaigui Ganjiang decoction plus rectal administration of Chinese herbal medicines in the treatment of ulcerative colitis.
Materials and Methods
General information:
Between December 2018 and March 2021, 88 patients with ulcerative colitis diagnosed and treated in our hospital met the inclusion criteria and were recruited. They were assigned to receive mesalamine (control group) or Chaigui Ganjiang decoction plus rectal administration of Chinese herbal medicines (study group), with 44 cases in each group. The study was approved by the ethics committee of our hospital. All patients were treated in accordance with the Declaration of Helsinki and signed the informed consent forms.
Inclusion and exclusion criteria:
Inclusion criteria: Patients met the clinical diagnostic criteria for ulcerative colitis and were diagnosed by relevant imaging examinations; met the criteria of the TCM classification, cold-heat imbalance of Shaoyang Taiyin; all were between 18- 70 y of age and had complete clinical data.
Exclusion criteria: Patients with severe, fulminant ulcerative colitis; patients with cardiac, hepatic, or renal dysfunction; patients with allergies to the study drugs and patients who were pregnant or lactating.
Dropout criteria: Patients could not fully cooperate to complete the current study; rescinded their consent; participated in other studies, which affected the assessment of the results of the current study.
Treatment methods:
All patients received basic treatment upon admission. Patients in the control group swallowed 1 g of mesalamine enteric soluble tablets (Huidi, Guohua Zunzhi H19980148, Sunflower Pharmaceutical Group Jiamusi Luling Pharmaceutical Co., Ltd.) 1 h before meals, 4 times daily for 42 d.
The study group patients were given Chaigui Ganjiang decoction plus rectal administration of Chinese herbal medicines. The ingredients of the decoction included 30 g of radix Bupleuri, 10 g each of Scutellaria baicalensis (S. baicalensis), cassia twig, dried ginger, Pinelliae rhizoma, radix Glycyrrhizae preparata, radix Trichosanthis and fresh oyster. The herbs were decocted with water and administered once daily for 3 mo, with 1 mo as one treatment course.
The herbs of the rectal administration medicine included 20 g of lightyellow Sophora root, Phellodendri Chinensis cortex, 12 g of Bletilla hyacinthina reichb, 10 g of Chinese gall, 6 g of fructus chebulae, and 2 g of Panax notoginseng powder. The herbs were decocted with water to obtain 150 ml of filtrate, which was used for enema. The patients were instructed to empty the bowels 30 min before the enema. The filtrate was added to the disposable enemator, with the temperature maintained at 38°-39°. The patient's buttock was elevated 10 cm in the lateral position, the disposable catheter was inserted 15-20 cm into the anus and the medicine was slowly administered into the rectum and kept for 30 min.
Outcome measures:
Clinical efficacy: The clinical efficacy of patients after treatment was determined by clinical symptoms and Baron score and was divided into four grades; complete remission (main symptoms disappeared, colonic mucosa was normal, Baron score decreased by more than 95 %), markedly effective (main symptoms basically disappeared, colonic mucosa inflammation significantly reduced, Baron score decreased by 70 %-95 %), effective (main symptoms significantly were alleviated, mucosa showed mild inflammation, Baron score decreased by 30 %-70 %) and ineffective (no significant changes).
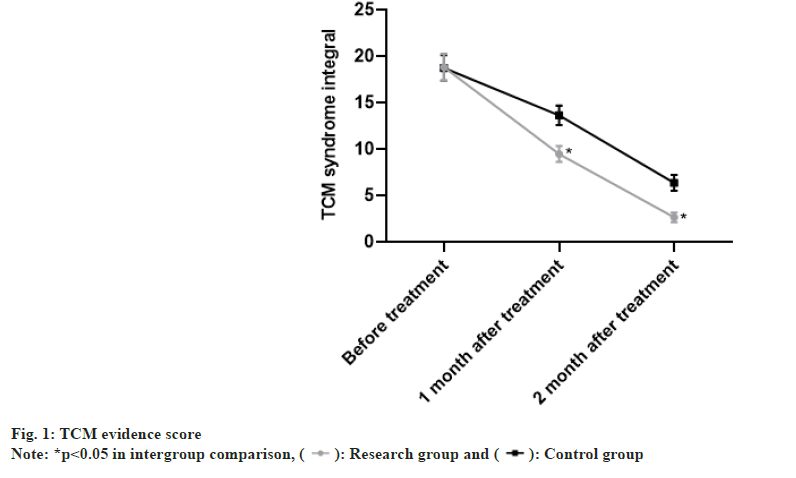
TCM evidence score: Patient’s symptoms such as diarrhea, pain, dyspnea, nausea and vomiting were scored according to the TCM efficacy assessment criteria on a scale of 1 to 4, with lower scores indicating less severe symptoms.
Inflammatory factors: Before and after treatment, 5 ml of fasting venous blood was collected from both groups and centrifuged at 3000 r/min for 15 min to isolate the serum. Serum concentrations of Interleukin (IL)-10, IL-17 and Tumor Necrosis Factor-alpha (TNF-α) were measured by enzymelinked immunosorbent assay.
Adverse events: The occurrence of adverse reactions, including acid reflux, nausea, abdominal pain, abdominal distension, rash, etc., was observed and recorded in both groups.
Statistical analysis:
Statistical Package for the Social Sciences (SPSS) 26.0 software was used to process the data, and image processing was performed using GraphPad Prism 8 software. Count data [n (%)] were examined using the chi-square test, and measurement data (x±s) were tested using the t-test. Statistical significance was indicated by p<0.05.
Results and Discussion
In the study group, there were 22 males and 22 females, aged 24-68 (38.94±7.23) y, 20 cases of E1 lesions, 18 cases of E2 lesions, 6 cases of E3 lesions, with a disease duration of 0.2 to 8 (2.25±1.07) y, 29 cases of mild disease, 15 cases of moderate disease, 14 cases of high school and below and 30 cases of undergraduate and above. In the control group, there were 23 males and 21 females, aged 23-65 (38.69±7.35) y, 22 cases of E1 lesions, 17 cases of E2 lesions, 5 cases of E3 lesions, with a disease duration of 0.2 to 8 (2.31±1.21) y, 27 cases of mild disease, 17 cases of moderate disease, 17 cases of high school and below and 27 cases of undergraduate and above. The two groups did not differ significantly in baseline patient profiles (p>0.05) as shown in Table 1.
| Study group (n=44) | Control group (n=44) | t | p | ||
|---|---|---|---|---|---|
| Sex | Male | 22 | 23 | ||
| Female | 22 | 21 | |||
| Age (year) | 24-68 | 23-65 | |||
| Mean | 38.94±7.23 | 38.69±7.35 | 0.161 | 0.925 | |
| Lesions | E1 | 20 | 22 | ||
| E2 | 18 | 17 | |||
| E3 | 6 | 5 | |||
| Disease duration | 0.2-8 | 0.2-8 | |||
| Mean | 2.25±1.07 | 2.31±1.21 | 0.246 | 0.841 | |
| Disease severity | Mild | 29 | 27 | ||
| Moderate | 15 | 17 | |||
| Education | High school and below | 14 | 17 | ||
| Undergraduate and above | 30 | 27 |
Table 1: Baseline Patient Profiles (x̄±s)
In the study group, there were 12 cases of complete remission, 20 cases of markedly effective, 11 cases of effective and 1 case of ineffective, with a total efficiency of 97.73 %. In the control group, there were 8 cases of complete remission, 10 cases of markedly effective, 15 cases of effective and 11 cases of ineffective, with a total efficiency of 75.00 %. TCM interventions were associated with markedly higher treatment efficacy vs. mesalamine (p<0.05) as shown in Table 2.
| Study group (n=44) | Control group (n=44) | t | p | |
|---|---|---|---|---|
| Complete remission | 12 | 8 | - | - |
| Markedly effective | 20 | 10 | - | - |
| Effective | 11 | 15 | - | - |
| Ineffective | 1 | 11 | - | - |
| Total efficiency | 97.73 | 75 | 9.649 | 0.001 |
Table 2: Clinical Efficacy (%)
The TCM evidence score of patients in the study group was (18.84±1.44) before treatment, (9.48±0.87) at 1 mo after treatment and (2.67±0.53) at 2 mo after treatment. The TCM evidence score of the control group before treatment was (18.77±1.39), at 1 mo after treatment (13.65±1.04) and at 2 mo after treatment (6.39±0.85). TCM interventions provided more significant symptom remission for patients than mesalamine, as evinced by the lower TCM evidence scores (p<0.05) as shown in fig. 1.
The pre-treatment IL-10 level in the study group was (24.41±5.41), IL-17 level was (56.85±8.58), TNF-α level was (57.89±9.11), the post-treatment IL-10 level was (38.54±6.78), IL-17 level was (24.16±3.41) and TNF-α level was (20.74±3.74). In the control group, the IL-10 level was (24.32±5.82), IL-17 level was (56.17±8.49), TNF-α level was (57.91±9.23) before treatment and the IL-10 level was (28.71±5.41), IL-17 level was (34.78±6.72) and TNF-α level was (28.01±5.01). Remarkably elevated serum IL-10 concentrations, reduced IL-17 and TNF-α concentrations in the study group suggested better inflammatory response mitigation of TCM interventions than mesalamine (p<0.05) as shown in fig. 2.
In the study group, there were 0 cases of acid reflux, 2 cases of nausea, 1 case of abdominal pain, 1 case of abdominal distension and 0 cases of skin rash with a total incidence of 9.09 %. In the control group, there were 3 cases of acid reflux, 4 cases of nausea, 2 cases of abdominal pain, 3 cases of abdominal distension and 1 case of skin rash, with a total incidence of 29.55 %. Chaigui Ganjiang decoction plus rectal administration of Chinese herbal medicines demonstrated a good safety profile vs. mesalamine by offering a lower incidence of adverse events (p<0.05) as shown in Table 3.
| Study group (n=44) | Control group (n=44) | t | p | |
|---|---|---|---|---|
| Acid reflux | 0 | 3 | - | - |
| Nausea | 2 | 4 | - | - |
| Abdominal pain | 1 | 2 | - | - |
| Abdominal distention | 1 | 3 | - | - |
| Skin rash | 0 | 1 | - | - |
| Total incidence | 9.09 | 29.55 | 5.905 | 0.017 |
Table 3: Adverse Events (%)
The pathogenesis of ulcerative colitis is unclear and has been shown to be potentially associated with abnormal immune function, psychological factors, infectious factors, oxygen-free radical damage and infections[6,13]. Western medicine uses adrenocorticosteroids and amino salicylic acid for disease management, among which mesalamine is considered the drug of choice for mild to moderate ulcerative colitis. Mesalamine is a first line amino salicylic acid drug[14], which has an intestinal coating that reduces absorption over the colon, increases the concentration of colonic drugs and effectively inhibits colitis reactions[15,16]. Nevertheless, mesalamine may elicit adverse reactions including headache, dizziness and gastrointestinal disorders, which compromise its efficacy. In TCM, ulcerative colitis is classified as "diarrhea", "intestinal obstruction" and "bloody stools". The disease is located in the intestinal tract and is closely related to liver, spleen and kidney dysfunction and its main pathogenesis is the weakness of the spleen and stomach, and damp-heat stagnation[17]. The main pathogenesis of ulcerative colitis is congenital and acquired spleen and stomach depletion, or lack of heat and cold regulation, or eating disorders or emotional disorders, resulting in spleen and stomach damage, functional transport disorders, large intestine conduction disorders and poor ventilation recovery. Moreover, the persistently produced damp heat, phlegm, stasis and toxicity during disease progression cause prolonged disease duration[18,19].
In the present study, the result showed that TCM interventions were associated with markedly higher treatment efficacy vs. mesalamine (p<0.05). The disease can be divided into active and remitting phases. The active phase is mainly characterized by heat and water accumulation in the intestine, Qi and blood imbalance, while the remitting phase is featured by positive deficiency and evil attachment and loss of health in transportation and transformation. In the Chaigui Ganjiang decoction used in this study, radix Bupleuri, S. baicalensis can alleviate the half-surface and half-ribs injury[20], dried ginger alleviates the bitterness and coldness of S. baicalensis and with radix Glycyrrhizae preparata warms the cold of Taiyin and prevents from entering Taiyin. Radix Trichosanthis moistens and quenches thirst, fresh oyster disperses micro-nodules in the chest and the combination of the two can relieve dryness in the viscera, promote water and remove dampness. Cassia twig and radix Glycyrrhizae preparata warm the channel of Qi. The joint use of the above multiple drugs relieves the liver and gallbladder, warms the cold and strengthens the yang, clears heat and removes blood stasis, thus providing a good outcome for ulcerative colitis. The symptom analysis shows that the pathogenesis of water-drink stagnation can be identified by "nodules in the chest and abdomen and unfavorable urination". Chaigui Ganjiang decoction is a potent formula for warming Yang and regulating the pivot. The whole formula is used to warm the middle jiao, nourish the upper and lower jiao to consolidate the root and unblock the qi of the three jiao, ultimately contributing to the treatment of chronic diseases. Zhang et al. modified the formula to achieve the purpose of dispelling dampness and stopping diarrhea and treating ulcerative colitis with clear efficacy. Thus, Chaigui Ganjiang decoction provides an excellent improvement in the signs and symptoms of ulcerative colitis.
The previous study adopted TCM sequential therapy, in which Chinese herbal decoctions were administered and Chinese herbal enemas were performed at different stages of the disease and the results showed superior clinical efficacy and better inflammatory response mitigation after TCM interventions vs. mesalamine. In the present study, remarkably elevated serum IL-10 concentrations, and reduced IL-17 and TNF-α concentrations in the study group suggested better inflammatory response mitigation of TCM interventions than mesalamine (p<0.05). Enema allows the drug to act directly on the lesion, with high absorption, high local concentration and long-lasting effect. Accurate rectal administration can avoid the stimulation of gastric mucosa and features the benefits of unobstructed defecation, heat removal and detoxification. Thus, it alleviates inflammation and pain, arrests bleeding, promotes ulcer healing, avoids damage to drugs by gastrointestinal enzymes and reduces the adverse reactions of oral drugs. Wang et al. observed 52 cases of ulcerative colitis with liver and spleen disharmony treated with Tongxia combined with rectal administration of Chinese herbal medicines by enema and the results showed that the total efficiency of the treatment group was significantly higher than that of the two control groups, which was consistent with the results of the present study. Hence, Chaigui Ganjiang decoction plus rectal administration of Chinese herbal medicines in the treatment of patients with ulcerative colitis can detoxify the liver and gallbladder, warm the cold, promote the circulation of Yang and disperse the nodules.
This study has the following limitations; the small sample size and short follow-up time may lead to bias. The classification method was insufficiently accurate, and the sample distribution lacked randomness and low reproducibility. Future studies with larger sample size and long-term follow-ups will be performed to validate the results of the current study.
Chaigui Ganjiang Decoction plus rectal administration of Chinese herbal medicines provides marked symptom remission in patients with ulcerative colitis, potentiates clinical efficacy, alleviates inflammatory responses, and produces fewer adverse events.
Acknowledgement:
Author confirms the final authorship for this manuscript. All listed authors have made a significant scientific contribution to the research in the manuscript, approved its claims and agreed to be an author.
Funding:
This work was supported by Project of Hebei Administration of Traditional Chinese medicine (No: 2021416).
Author contributions:
Xuemei Tang, Lianhua Ma and Liyan Zhang have contributed to the design and implementation of the research; Xiuhong Lv and Weihe Meng have contributed to the analysis of the results and to the writing of the manuscript.
Conflict of interests:
The authors declared no conflict of interests.
References
- Ordás I. Ulcerative colitis. Lancet 2012;380(9853);1606-19.
- Du L, Ha C. Epidemiology and pathogenesis of ulcerative colitis. Gastroenterol Clin North Am 2020;49(4):643-54.
[Crossref] [Google Scholar] [PubMed]
- Adams SM, Bornemann PH. Ulcerative colitis. Am Fam Phys 2013;87(10):699-705.
- Keshteli AH, Madsen KL, Dieleman LA. Diet in the pathogenesis and management of ulcerative colitis: A review of randomized controlled dietary interventions. Nutrients 2019;11(7):1498.
[Crossref] [Google Scholar] [PubMed]
- Kaenkumchorn T, Wahbeh G. Ulcerative colitis: Making the diagnosis. Gastroenterol Clin 2020;49(4):655-69.
[Crossref] [Google Scholar] [PubMed]
- Lee SD. Health maintenance in ulcerative colitis. Gastroenterol Clin 2020;49(4):15-6.
[Crossref] [Google Scholar] [PubMed]
- Segal JP, LeBlanc JF, Hart AL. Ulcerative colitis: An update. Clin Med 2021;21(2):135-9.
[Crossref] [Google Scholar] [PubMed]
- Eisenstein M. Ulcerative colitis: Towards remission. Nature 2018;563(7730):S33.
[Crossref] [Google Scholar] [PubMed]
- Kou FS, Shi L, Li JX, Wang ZB, Shi R, Mao TY, et al. Clinical evaluation of traditional Chinese medicine on mild active ulcerative colitis: A multi-center, randomized, double-blind, controlled trial. Medicine 2020;99(35):e21903.
[Crossref] [Google Scholar] [PubMed]
- Shen ZF, Wu HH, Zhu L, Zhou Q, Shen H. Traditional Chinese medicine for ulcerative colitis: Systematic reviews based on PRIO-harms. Zhongguo Zhong Yao Za Zhi 2020;45(3):674-82.
[Crossref] [Google Scholar] [PubMed]
- Lan YZ, Bai YL, Zhu XD. Integrated traditional Chinese and Western medicine for ulcerative colitis with diabetes: A protocol for systematic review and meta-analysis. Medicine 2021;100(4):e24444.
[Crossref] [Google Scholar] [PubMed]
- Luo S, Wen R, Wang Q, Zhao Z, Nong F, Fu Y, et al. Rhubarb Peony Decoction ameliorates ulcerative colitis in mice by regulating gut microbiota to restoring Th17/Treg balance. J Ethnopharmacol 2019;231:39-49.
[Crossref] [Google Scholar] [PubMed]
- Taku K, Britta S, Chen WS, Ferrante M, Shen B, Bernstein CN, et al. Ulcerative colitis. Nat Rev Dis Primers 2020;6(1):73.
- Le Berre C, Roda G, Nedeljkovic Protic M, Danese S, Peyrin-Biroulet L. Modern use of 5-aminosalicylic acid compounds for ulcerative colitis. Expert Opin Biol Ther 2020;20(4):363-78.
[Crossref] [Google Scholar] [PubMed]
- Kucharzik T, Koletzko S, Kannengiesser K, Dignass A. Ulcerative colitis—Diagnostic and therapeutic algorithms. Deutsch Ärztebl Int 2020;117(33-34):564-74.
[Crossref] [Google Scholar] [PubMed]
- Ko CW, Singh S, Feuerstein JD, Falck-Ytter C, Falck-Ytter Y, Cross RK, et al. AGA clinical practice guidelines on the management of mild-to-moderate ulcerative colitis. Gastroenterology 2019;156(3):748-64.
[Crossref] [Google Scholar] [PubMed]
- Xiong X, Cheng Z, Wu F, Hu M, Liu Z, Dong R, et al. Berberine in the treatment of ulcerative colitis: A possible pathway through Tuft cells. Biomed Pharmacother 2021;134:111129.
[Crossref] [Google Scholar] [PubMed]
- Zhang C, Jiang M, Lu A. Considerations of traditional Chinese medicine as adjunct therapy in the management of ulcerative colitis. Clin Rev Allergy Immunol 2013;44(3):274-83.
[Crossref] [Google Scholar] [PubMed]
- Wei YY, Fan YM, Ga Y, Zhang YN, Han JC, Hao ZH. Shaoyao decoction attenuates DSS-induced ulcerative colitis, macrophage and NLRP3 inflammasome activation through the MKP1/NF-κB pathway. Phytomedicine 2021;92:153743.
[Crossref] [Google Scholar] [PubMed]
- Cui L, Guan X, Ding W, Luo Y, Wang W, Bu W, et al. Scutellaria baicalensis Georgi polysaccharide ameliorates DSS-induced ulcerative colitis by improving intestinal barrier function and modulating gut microbiota. Int J Biol Macromol 2021;166:1035-45.
[Crossref] [Google Scholar] [PubMed]
 ): Research group and (
): Research group and ( ): Control group
): Control group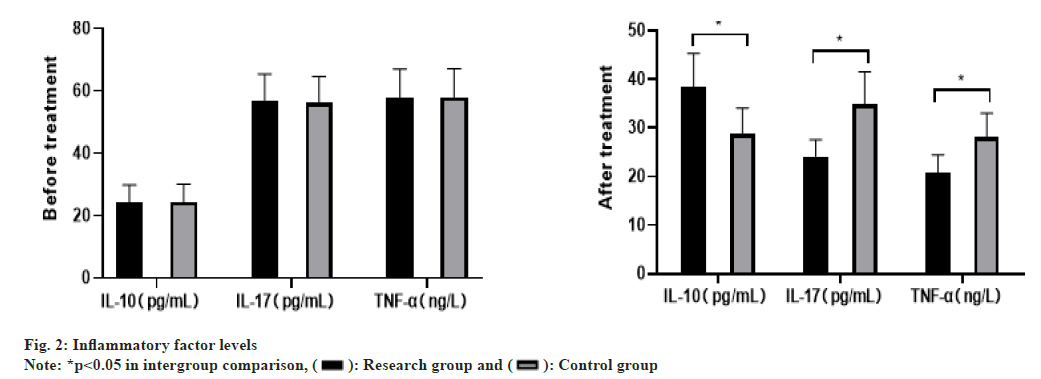
 ): Research group and (
): Research group and ( ): Control group
): Control group 



