- *Corresponding Author:
- Lingli Wang
Department of Cardiology, Heart Center, Three Gorges Hospital of Chongqing University, Chongqing 40000, China
E-mail: wanglingli0319@163.com
| This article was originally published in a special issue, “Transformative Discoveries in Biomedical and Pharmaceutical Research” |
| Indian J Pharm Sci 2023:85(4) Spl Issue “197-201” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
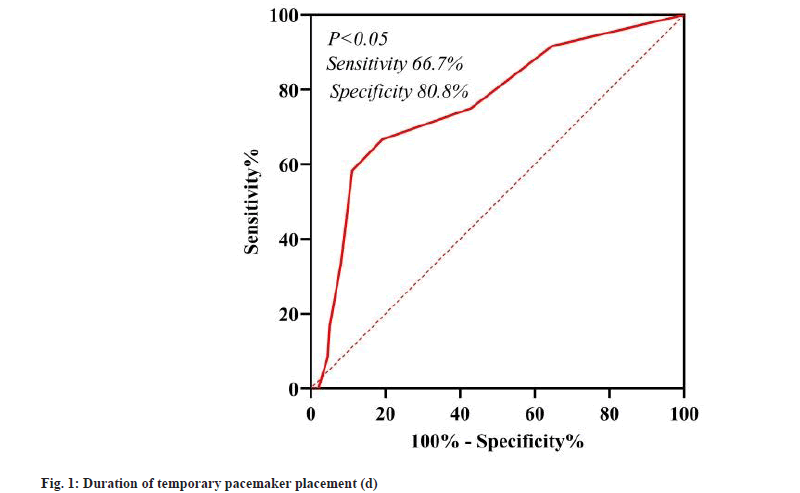
This study is to identify the high-risk factors for the occurrence of lower extremity venous thrombosis after temporary cardiac pacemaker via femoral vein. 210 patients who underwent temporary cardiac pacing via the femoral vein at Chongqing University Three Gorges Hospital from January 2017 to August 2022 were selected for the study. The patients were divided into non-thrombosis group (n=198) and thrombosis group (n=12) according to their lower extremity venous thrombosis. Baseline characteristics of the two groups were compared, and binary logistic regression was used to analyze the risk factors for developing lower extremity venous thrombosis after surgery. The proportion of combined diabetes and acute cerebral infarction was higher in the thrombosis group than in the non-thrombosis group, and the indwelling time of temporary pacing electrodes was longer in the thrombosis group than in the non-thrombosis group (p<0.05). Logistic regression presented that combined diabetes, acute cerebral infarction, and long placement time of temporary pacing electrodes were high risk factors for the development of lower extremity venous thrombosis after surgery (p<0.05). The placement duration (d) of temporary pacing electrodes had predictive value for the occurrence of lower extremity venous thrombosis after surgery, with the best predictive value of 3.5 d, sensitivity of 66.7 % and specificity of 80.8 % (p<0.05). Diabetes, acute cerebral infarction and prolonged placement of temporary pacing electrodes are high-risk factors for lower extremity venous thrombosis after temporary cardiac pacing through the femoral vein, and the indwelling time of the temporary pacing electrode (d) more than 3.5 d had a predictive significance for postoperative venous thrombosis of the lower extremity.
Keywords
Temporary pacemaker, femoral vein therapy, venous thrombosis
Temporary cardiac pacing is performed by implanting temporary electrodes in the right ventricle via intravenous route[1,2]. Temporary pacemakers are widely adapted clinically, not only for emergency pacing in diseases such as significant bradycardia, cardiac arrest or third-degree atrioventricular block, but also for perioperative protection in surgical procedures in patients with pathological sinus node syndrome, among others[2,3]. The femoral vein route is the fastest and most efficient way to perform emergency pacing electrode insertion, and it does increase the risk of venous thrombosis and pulmonary embolism compared to other sites[4]. Therefore, it is clinically important to identify the risk factors for venous thrombosis after temporary pacemaker through the femoral vein. Inclusion criteria include patients older than 15 y old with temporary pacemakers through the femoral vein at Chongqing University Three Gorges Hospital, between January 2017 and August 2022, were diagnosed and complete information on the duration of hospitalization is available. Exclusion criteria include patients who have been diagnosed with venous thrombosis before surgery; failure of temporary pacemaker placement and patients who did not cooperate with treatment and were not discharged as scheduled. After regular sterilization, the femoral vein was punctured by the Seldinger method and a 6F sheath (Cordis 11 cm) was placed. A St. Jude bipolar temporary pacing floating electrode is then delivered via sheath tube in the right ventricular apical region and connected to a temporary pacemaker (Medtronic). The decision to leave the sheath in place and the timing of indwelling is based on the condition. Directly by venous color Doppler, venous thrombosis of the lower extremities is found. Or based on the presence of extremity edema, cyanosis and pain, we suspect venous thrombosis, and also require venous color Doppler to confirm the diagnosis, and pulmonary embolism is confirmed by pulmonary computed tomography angiography. A total of 210 patients met the inclusion criteria between January 2017 and August 2022. Twelve of these patients developed lower extremity venous thrombosis, with a thrombotic incidence of 5.7 %. The gender, age, previous presence of hypertension and type 2 diabetes, Body Mass Index (BMI), etiology of temporary cardiac pacing, combined with acute cerebral infarction, malignancy, acute myocardial infarction, prophylactic anticoagulation with enoxaparin sodium, antiplatelet drugs, indwelling sheaths, and duration of temporary pacing electrode indwelling were collected from these 210 patients. The presence of swelling, redness, pain and other manifestations of venous thrombosis in the extremity to determine the lower extremity venous thrombosis, then further improve the lower extremity venous ultrasound to confirm the diagnosis, including intermuscular venous thrombosis and deep venous thrombosis. All statistical analyses were performed using Statistical Package for Social Sciences 25.0 statistical software. Means±standard deviations were used for measures obeying normal distribution, and medians (lower quartile~upper quartile) were used for measures not obeying normal distribution. The t-test or nonparametric test (Mann- Whitney U test) was used for comparison between groups for measurement data and the chi-square test was used for comparison between groups for count data. A multi-factorial logistic regression analysis was used to study the risk factors for venous thrombosis after temporary pacemaker through the femoral vein. p<0.05 was considered a statistically significant difference. The proportion of combined diabetes and acute cerebral infarction was higher in the thrombus group than in the non-thrombus group and the indwelling time of temporary pacing electrodes was longer in the thrombus group than in the non-thrombus group (p<0.05). The remaining clinical indicators were not statistically different (Table 1). Diabetes, acute phase cerebral infarction, indwelling sheath, and indwelling time were included as suspected influencing factors. Binary Logistic regression analysis was used. The conclusion suggested that combined diabetes, acute phase cerebral infarction, and postoperative indwelling of the puncture sheath were high risk factors for venous thrombosis after temporary pacemaker surgery; the longer the indwelling time of temporary pacemaker electrodes, the higher the risk of thrombosis. Table 2 shows the details. The area under the curve of the receiver operating characteristic curve for the placement time of temporary pacemaker electrodes (d) was 0.762 (95 % Confidence Interval (CI) 0.615 to 0.908). The best predictive threshold for the development of postoperative venous thrombosis was 3.5 d, with a sensitivity of 66.7 % and specificity of 80.8 %; p<0.05 (fig. 1). Temporary cardiac pacing via the femoral vein route is a quick, safe and effective method for cardiac emergencies, but the occurrence of venous thrombosis during pacing electrode placement remains a concern[5]. Venous thrombosis and subsequent pulmonary embolism are serious complications of temporary cardiac pacing using the femoral vein route[4]. The femoral vein route increases the risk of thrombosis compared to the internal jugular, subclavian and median elbow vein routes[3]. In this study, we reviewed previous cases and analyzed the risk factors for venous thrombosis in temporary cardiac pacing via the femoral vein route. There are some guidelines for clinical prevention of venous thrombosis. Previous studies have confirmed that the incidence of asymptomatic lower extremity deep vein thrombosis associated with temporary cardiac pacing via the femoral route is approximately 25 % to 34 %, and venous thrombosis is directly associated with femoral pacemakers[6-8]. Puncturing the femoral vein and leaving the sheath in place can damage the intima, which can activate platelets to release a variety of bioactive substances and initiate the endogenous coagulation system. This can cause platelet aggregation and adhesion, resulting in thrombosis. In addition, temporary cardiac pacing electrodes are passive electrodes, which are prone to electrode dislocation and require postoperative extremity braking and bed rest to avoid the occurrence of electrode dislocation[9]. The need for postoperative bed rest is an important factor in the occurrence of deep vein thrombosis and is associated with reduced venous blood return, inflammation and hypercoagulable state[10]. The present study suggested that prophylactic use of enoxaparin was not effective in reducing the risk of postoperative lower extremity venous thrombosis. Nolewajka et al.[4] found that venous thrombosis and subsequent pulmonary embolism were serious complications of temporary cardiac pacing via the femoral route despite the use of prophylactic low-dose heparin. This study suggested that the proportion of diabetes mellitus was higher in the thrombotic group than in the nonthrombotic group. The findings of the multifactorial study suggested that diabetes was a high risk factor for venous thrombosis after temporary cardiac pacing via the femoral vein route (Odds Ratio (OR)=5.749, 95 % CI 1.438 to 22.979), with p<0.05. A cohort study by Chung et al.[11] showed a 1.44-fold increased risk of venous thrombosis in patients with type 2 diabetes compared to controls. Impaired fibrinolysis, platelet and endothelial cell dysfunction in diabetic patients predispose to a hypercoagulable state, which increases the risk of deep vein thrombosis and pulmonary embolism[12,13]. This study suggested that acute cerebral infarction was a high risk factor for lower extremity venous thrombosis after temporary cardiac pacing via the femoral vein route (OR=10.47, 95 % CI 1.879-58.358), both in univariate and multifactorial analysis, with p<0.05. Patients with acute cerebral infarction are often temporarily immobilized due to bed rest or neurological deficits in the affected extremity. As a result, thrombosis secondary to venous thrombosis is more likely to occur[14,15]. The longer the duration (d) of temporary pacing electrode placement, the higher the occurrence of venous thrombosis after temporary cardiac pacing via the femoral vein route (OR=1.437, 95 % CI 1.143 to 1.805), with p<0.05. If temporary cardiac pacing is required, it should be kept as short as possible, a strategy that avoids or reduces the potential complications associated with temporary pacemaker implantation, including venous thrombosis[16]. Then, this study confirmed that temporary pacing electrodes left in place for more than 3.5 d (d) had diagnostic value for the occurrence of lower extremity venous thrombosis with a sensitivity of 66.7 % and specificity of 80.8 %, p<0.05. It is recommended that, therefore, temporary pacing electrodes be left in place for no more than 3.5 d (d). If the condition does not allow the removal of temporary pacing electrodes, antithrombotic measures are recommended to prevent thrombosis. Diabetes, acute cerebral infarction, and prolonged placement of temporary pacing electrodes were high-risk factors for lower extremity venous thrombosis after temporary cardiac pacing accessible through the femoral vein route, and the placement duration (d) of temporary pacing electrodes >3.5 (d) had predictive value for the occurrence of lower extremity venous thrombosis after surgery. To prevent lower extremity venous thrombosis, the focus should be on patients with diabetes and acute cerebral infarction in patients with temporary cardiac pacing via the femoral vein route. At the same time, temporary pacing electrodes should be removed as soon as the condition allows, avoiding indwelling for more than 3.5 (d).
| Group | non-thrombus group (n=198) | thrombus group (n=12) | χ2/Z | p | |
|---|---|---|---|---|---|
| Etiology of temporary pacemaker implantation | Acute myocardial infarction [cases,%] | 39 (19.7 %) | 3 (25 %) | 2.840a | 0.417 |
| Significant bradycardia or atrioventricular block [cases,%] | 117 (59.1 %) | 5 (41.7 %) | |||
| Intraoperative protection [cases,%] | 38 (19.2 %) | 3 (25 %) | |||
| Viral myocarditis [cases,%] | 4 (2 %) | 1 (8.3 %) | |||
| Gender | Male [cases,%] | 117 (59.1 %) | 5 (41.7 %) | 1.530a | 0.465 |
| Female [cases,%] | 81 (40.9 %) | 7 (58.3 %) | |||
| Age (y)# | 71 (61~77.5) | 74 (64.5~84.75) | -1.075 | 0.282 | |
| BMI≥28 [cases,%] | 14 (7.1 %) | 1 (8.03 %) | 0.027a | 0.869 | |
| Hypertension [cases,%] | 55 (27.8 %) | 5 (41.7 %) | 1.069a | 0.301 | |
| Diabetes [cases,%] | 25 (12.6 %) | 5 (41.7 %) | 7.793a | 0.005* | |
| Combined malignancy [cases,%] | 15 (7.6 %) | 0 (0 %) | 0.979a | 0.322 | |
| Combined acute phase cerebral infarction [cases,%] | 5 (2.5 %) | 3 (25 %) | 15.596a | <0.001* | |
| Acute myocardial infarction [cases,%] | 25 (12.6 %) | 2 (16.7 %) | 0.165a | 0.685 | |
| Prophylactic anticoagulation with enoxaparin [cases,%] | 52 (26.3 %) | 1 (8.3 %) | 1.928a | 0.165 | |
| Use of antiplatelet agents [cases,%] | 32(16.2 %) | 2(16.7 %) | 0.002a | 0.963 | |
| Indwelling sheaths [cases,%] | 19(9.6 %) | 2(16.7 %) | 0.629a | 0.428 | |
| Duration of temporary pacing electrode placement [d]# | 2 (1~3) | 5 (2.25~6) | 3.138 | 0.002* | |
Note: BMI = Body Mass Index; #: a non-normal distribution obtained by Shapiro-Wilk ormality test; *: indicates p<0.05
Table 1: Comparison of the Proportion of Diabetes and Acute Cerebral Infarction in the Thrombosis Group and Non-Thrombus Group
| B | Standard Error | Wald | Degrees of freedom | Significance | OR | 95% CI for OR | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower limit | Upper limit | ||||||||
| Diabetes | Yes | 1.75 | 0.707 | 6.121 | 1 | 0.013 | 5.75 | 1.438 | 22.979 |
| No | 0 | 1 | |||||||
| Combined acute phase cerebral infarction | Yes | 2.35 | 0.877 | 7.178 | 1 | 0.007 | 10.5 | 1.879 | 58.358 |
| No | 0 | 1 | |||||||
| Duration of indwelling of temporary pacing electrodes (d) | 0.36 | 0.117 | 9.662 | 1 | 0.002 | 1.44 | 1.143 | 1.805 | |
| Constant | -4.8 | 0.721 | 43.61 | 1 | 0 | 0.01 | |||
Table 2: Influencing Factors of Diabetes, Acute Phase Cerebral Infarction, Indwelling Sheath and Indwelling Time
Data sharing agreement:
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflict of interests:
The authors declared no potential conflicts of interest with respect to the research, author-ship, and/or publication of this article.
References
- Liu M, Han X. Bedside temporary transvenous cardiac pacemaker placement. Am J Emerg Med 2020;38(4):819-22.
[Crossref] [Google Scholar] [PubMed]
- He DH, Zhang ZG, Lin KM. Feasibility and safety of temporary pacemaker placement via median elbow vein. Chin J Hypertension 2022;30(4):382-6.
- Baloch F, Kabani AS, Naseem M, Khan AH. Perfecting temporary pacemakers in a developing country. Expert Rev Cardiovasc Ther 2021;19(2):177-80.
[Crossref] [Google Scholar] [PubMed]
- Nolewajka AJ, Goddard MD, Brown TC. Temporary transvenous pacing and femoral vein thrombosis. Circulation 1980;62(3):646-50.
[Crossref] [Google Scholar] [PubMed]
- Yu L, Yuan YQ, Liu HL. Subcutaneous injection of heparin to prevent temporary cardiac pacing electrode implantation in 22 thrombosis. J Zhengzhou Univ Med 2004;5(2):341-342.
- Weinstein J, Gnoj J, Mazzara JT, Ayres SM, Grace WJ. Temporary transvenous pacing via the percutaneous femoral vein approach: A prospective study of 100 cases. Am Heart J 1973;85(5):695-705.
[Crossref] [Google Scholar] [PubMed]
- Austin JL, Preis LK, Crampton RS, Beller GA, Martin RP. Analysis of pacemaker malfunction and complications of temporary pacing in the coronary care unit. Am J Cardiol 1982;49(2):301-6.
[Crossref] [Google Scholar] [PubMed]
- Sanders P, Farouque HO, Ashby DT, Mahar LJ, Young GD. Effect of anticoagulation on the occurrence of deep venous thrombosis associated with temporary transvenous femoral pacemakers. Am J Cardiol 2001;88(7):798-801.
[Crossref] [Google Scholar] [PubMed]
- Ayerbe JL, Sabaté RV, García CG, Leor OR, Pérez MG, Abadal AC, et al. Temporary pacemakers: Current use and complications. Rev Esp Cardiol 2004;57(11):1045-52.
[Crossref] [Google Scholar] [PubMed]
- Engbers MJ, Blom JW, Cushman M, Rosendaal FR, van Hylckama Vlieg A. The contribution of immobility risk factors to the incidence of venous thrombosis in an older population. J Thromb Haemost 2014;12(3):290-6.
[Crossref] [Google Scholar] [PubMed]
- Chung WS, Lin CL, Kao CH. Diabetes increases the risk of deep-vein thrombosis and pulmonary embolism. Thromb Haemost 2015;114(10):812-8.
[Crossref] [Google Scholar] [PubMed]
- Grant PJ. Diabetes mellitus as a prothrombotic condition[J]. J Intern Med, 2007,262(2):157-172. DOI: 10.1111/j.1365-2796.2007.01824.x. [Crossref] [Google Scholar] [PubMed]
- Avogaro A, Albiero M, Menegazzo L, de Kreutzenberg S, Fadini GP. Endothelial dysfunction in diabetes: the role of reparatory mechanisms. Diabetes Care 2011;34(Suppl 2):S285-90.
[Crossref] [Google Scholar] [PubMed]
- Rinde LB, Småbrekke B, Mathiesen EB, Løchen ML, Njølstad I, Hald EM, et al. Ischemic stroke and risk of venous thromboembolism in the general population: the Tromsø study. J Am Heart Assoc 2016;5(11):e004311.
[Crossref] [Google Scholar] [PubMed]
- Jin T, Jiang L, Zhang X. Influence of lower extremity deep venous thrombosis in cerebral infarction on coagulation index and thromboelastogram and its risk factors. J Healthc Eng 2022;2022:1-6.
[Crossref] [Google Scholar] [PubMed]
- Kossaify A. Temporary endocavitary pacemakers and their use and misuse: the least is better. Clini Med Insight Cardiol 2014;8:9-11.
[Crossref] [Google Scholar] [PubMed]