- *Corresponding Author:
- Zhilin Cui
Department of Traditional Chinese Medicine, The First Clinical Medical College of Heilongjiang University of Traditional Chinese Medicine, Haerbin 150500, China
E-mail: tongqingtang678@163.com
| This article was originally published in a special issue, “Exploring the Role of Biomedicine in Pharmaceutical Sciences” |
| Indian J Pharm Sci 2024:86(1) Spl Issue “124-130” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the effect of Renshen Yangrong decoction combined with conventional drugs in the treatment of dilated cardiomyopathy. 107 patients with dilated cardiomyopathy were divided into a Chinese medicine group (n=54) and a control group (n=53) using the random number table method. Control group received placebo combined with conventional medication and Chinese medicine group received Renshen Yangrong decoction combined with conventional medication. The clinical efficacy, cardiac function indexes, serological indexes, quality of life scores and adverse effects of the two groups were compared. The overall treatment efficiency of Chinese medicine group was higher than that of control group (p<0.05). After treatment, Chinese medicine group had higher left ventricular ejection fraction, blood volume, serum N-terminal pro-B-type natriuretic peptide, serum procollagen type I carboxy-terminal peptide, serum procollagen type III carboxy-terminal peptide and all Minnesota heart failure quality of life scale scores than control group (p<0.05) and the left ventricular end-diastolic diameter was lower than control group (p<0.05). No adverse events occurred in either group. Renshen Yangrong decoction combined with conventional drugs is safe and effective in the tr eatment of dilated cardiomyopathy.
Keywords
Dilated cardiomyopathy, Renshen Yangrong decoction, cardiac function, myocardial fibrosis, ventricular remodeling
Dilated Cardiomyopathy (DCM) is a myocardial disease in which the Left Ventricle (LV) is dilated and systolic, but without coronary artery disease or abnormal loading conditions proportional to the degree of LV damage[1,2]. The main feature is myocardial hypertrophy, which is associated with increased cardiomyocyte volume and expansion of the extracellular matrix due to interstitial and focal replacement fibrosis[3]. DCM is caused by a complex interaction of environmental and genetic factors and is predominantly in the middle-aged and elderly, with a male to female ratio of approximately 3:1[4,5]. DCM is a major cause of heart failure and is the most common indication for heart transplantation[6]. Currently, clinical treatment of DCM is based on improving ventricular remodeling, mostly with diuretics, beta-blockers and Angiotensin-Converting Enzyme (ACE) inhibitors, with no specific treatment available[7]. However, the prognosis of DCM has improved significantly with the current regimen, with an estimated 10 y survival rate of 85 % without death or heart transplantation[8,9]. Despite the success of the current treatment phase, studies have shown that some patients with DCM are still prone to sudden cardiac death and refractory heart failure, requiring heart transplantation or mechanical circulation[10]. There is therefore an urgent need to find more effective treatment options to improve the outcome of DCN.
Previous studies have shown that traditional Chinese Medicine (CM) has unique advantages in treating DCM from a holistic perspective, using a dialectical approach, which can help improve cardiac function, alleviate clinical symptoms and increase survival rates in DCM patients[11]. According to its clinical manifestations and characteristics, it belongs to the category of "palpitations, heart swelling, heart paralysis, chest paralysis, heartwater, phlegm, asthma and oedema" in CM[12]. The treatment is based on tonifying the deficiency and dispelling the evil, benefiting the Qi, invigorating the blood, strengthening the spleen and promoting water retention[13]. Yangrong decoction is from the "three causes and one disease evidence formula" written by Chen Wuzhe in the Southern Song Dynasty, and was later included again in the "Taiping Huimin Hodong Bureau Formula" and renamed as Ginseng Yangrong Tang. Renshen Yangrong decoction is composed of 12 herbs, including Ginseng, Astragalus and Atractylodes, and is mainly used for treating the symptoms of Yin-Yang exhaustion and deficiency of accumulated labor. Ginseng Nourishing Glory Tang has been proven to have an important role in the treatment of coronary angina[14] and malignant tumours[15]. However, the effect of its application in DCM has not been reported in studies. We hypothesized that the addition of Renshen Yangrong decoction to conventional Western medicine for the treatment of DCM would yield good results. Therefore, we conducted a randomized controlled trial to test our hypothesis, aiming to provide a more effective and diverse reference protocol for the clinical treatment of DCM.
Materials and Methods
Study design:
107 patients with DCM attending a hospital in China from January 2021 to December 2022 were randomly divided into a CM group (Group CM) (n=54) and a control group (Group C) (n=53) using a random number table. Group C received placebo combined with conventional medication and Group CM received Renshen Yangrong decoction combined with conventional medication. Patients in both groups signed an informed consent form. The hospital ethics committee supported the study.
Inclusion criteria: Confirmed diagnosis of DCM; age ≥18 y; New York Heart Association (NYHA) classification II-III and signed informed consent.
Exclusion criteria: Severe hepatic and renal dysfunction; malignant neoplasm; immune system disorders, infectious diseases; serious life-threatening diseases such as severe cardiac arrhythmias and cardiogenic shock; women in pregnancy or breastfeeding; pulmonary heart disease and pulmonary hypertension, and severe psychiatric disorders and poor compliance with treatment.
Treatment:
Group CM received Renshen Yangrong decoction combined with conventional medicine. Refer to the Chinese guidelines for the diagnosis and treatment of DCM[16], drugs includes B-blockers, ACE inhibitors, aldosterone antagonists, and diuretics. Renshen Yangrong decoction: Ginseng 10 g, Astragalus membranaceus 30 g, cultivated land 15 g, Atractylodes macrocephala 15 g, Poria cocos 15 g, Angelica sinensis 15 g, white peony root 15 g, Citrus reticulata blanco 15 g, cassia twig 10 g, Schisandra chinensis 5 g, ginger 5 g, Eupatorium 15 g, Lepidium seed 10 g, prepared licorice 5 g. Decoction in water, 1 dose daily, divided into morning and evening.
Group C received only conventional medication, which was administered in the same way as Group C. Placebo was also administered and the frequency of use was the same as Group CM with Renshen Yangrong decoction. Patients in both groups continued treatment for 12 w.
Primary outcomes:
Clinical efficacy: Referring to the diagnostic efficacy criteria for CM[17]; marked response cardiac function improved by 2 levels after treatment, major symptoms and signs improved significantly.
Moderate response: Cardiac function improved by 1 level after treatment, major symptoms and signs improved.
No response: Cardiac function did not improve after treatment, major symptoms and signs the number of symptoms and signs worsened or led to death.
Total effective rate=(Number of marked response+number of moderate response)/total×100 %
Cardiac function: Left Ventricular End-Diastolic Internal Diameter (LEVDD), Left Heart Ejection Fraction (LVEF) and Blood Volume per Beat (SV) were measured using color Doppler ultrasound before and after treatment.
Secondary outcomes:
Serological indicators: The levels of serum N-Terminal Pro-B-Type Natriuretic Peptide (N-proBNP), serum Procollagen Type I Carboxy Terminal Peptide (PICP), serum Procollagen Type III Carboxy-Terminal Peptide (PIIICP) were measured before and after treatment.
Quality of life: Quality of life was assessed in both groups before and after treatment using the Minnesota Living with Heart Failure Questionnaire (MLHFQ)[18] , which consists of 21 entries divided into 3 domains; physical (8 entries), emotional (5 entries), and other (8 entries), with a score range of 0 to 5 for each entry. Higher scores indicate poorer quality of life. Record the patient’s adverse reactions and calculate the incidence.
Statistical processing:
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) 21.0 statistical package for social sciences. Statistical information was expressed as n (%) and comparisons were made using the Chi-square (χ2) test. The Kolmogorov- Smirnov test was used to test the normality of the data, and non-normally distributed measures were expressed as median and quartiles, and the Mann-Whitney U test was used to compare between groups. Measures that conformed to the normal distribution were expressed as (X̄±S), and comparisons were made using the t-test, Analysis of Variance (ANOVA) and Least Significant Difference (LSD) test. Differences were indicated as statistically significant at p<0.05.
Results and Discussion
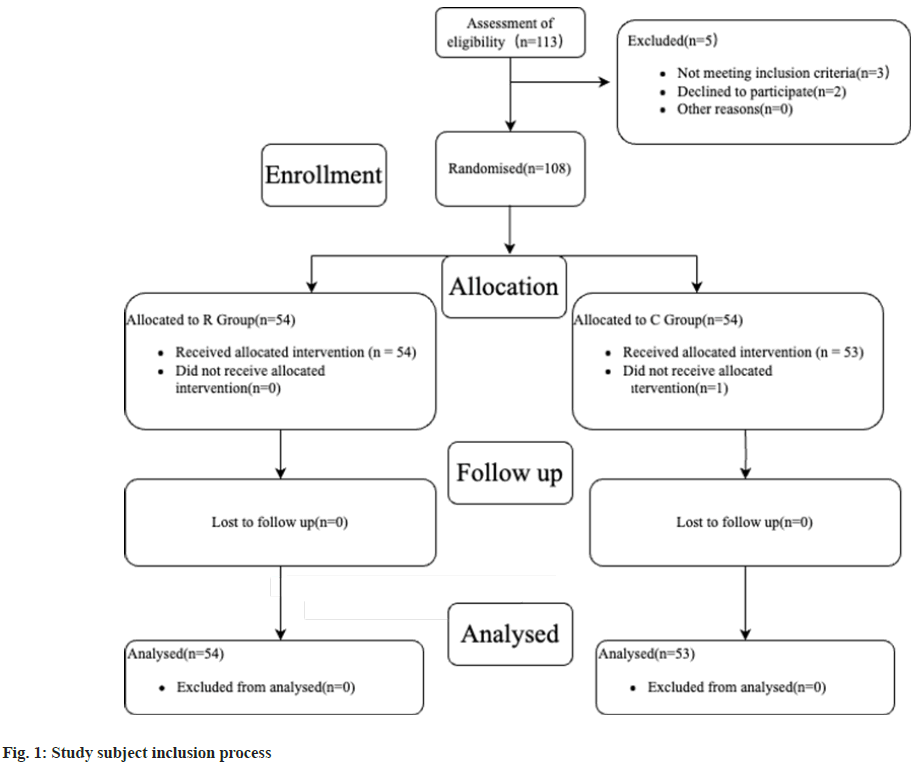
As shown in fig. 1, 113 patients were assessed for eligibility, 3 did not meet the inclusion criteria and 2 declined to participate. 108 patients were included and randomized, 54 were allocated to Group CM and 54 to Group C. Group C consisted of 1 patient who did not receive the intervention to which they were allocated. There was no loss to follow-up in either group. And the baseline information was well matched between the two groups as shown in Table 1. As shown in Table 2, the overall effectiveness of Group CM was higher than that of Group C (p<0.05).
| Characteristics | Group CM (n=54) | Group C (n=53) | χ2/t | p value |
|---|---|---|---|---|
| Demographics | ||||
| Age (years, mean±SD) | 53.43±4.39 | 54.04±4.28 | 0.728 | 0.469 |
| Male/female, n (%) | 35 (64.81)/19 (35.19) | 36 (67.92)/17 (32.08) | 0.116 | 0.734 |
| Medications at enrolment | ||||
| ACE inhibitor/ARB, n (%) | 54 (100.00) | 53 (100.00) | 0.000 | 1.000 |
| Beta-blocker, n (%) | 46 (85.19) | 45 (84.91) | 0.002 | 0.968 |
| MRA, n (%) | 24 (44.44) | 22 (41.51) | 0.094 | 0.759 |
| Loop diuretic, n (%) | 7 (12.96) | 6 (11.32) | 0.068 | 0.795 |
| Clinical characteristics at enrolment | ||||
| Heart rate (bpm, mean±SD) | 67.35±3.11 | 67.45±3.18 | 0.165 | 0.87 |
| Systolic blood pressure (mmHg, mean±SD) | 124.52±5.53 | 126.05±5.30 | 1.461 | 0.147 |
| Diastolic blood pressure (mmHg, mean±SD) | 73.57±4.36 | 74.89±4.78 | 1.493 | 0.139 |
| NYHA classification | 0.089 | 0.767 | ||
| II, n (%) | 28 (51.85) | 29 (54.72) | ||
| III, n (%) | 26 (48.15) | 24 (45.28) | ||
Note: Angiotensin Receptor Blocker (ARB) and Mineralocorticoid receptor antagonist (MRA)
Table 1: Baseline Characteristics of the Two Groups
| Group CM (n=54) | Group C (n=53) | χ2/t | p value | |
|---|---|---|---|---|
| Marked response | 28 (51.85) | 23 (43.40) | ||
| Moderate response | 23 (42.59) | 20 (37.74) | ||
| No response | 3 (5.56) | 10 (18.87) | ||
| Marked response+moderate response | 51 (94.44) | 43 (81.13) | 4.441 | 0.035 |
Table 2: The Overall Effectiveness [n (%)]
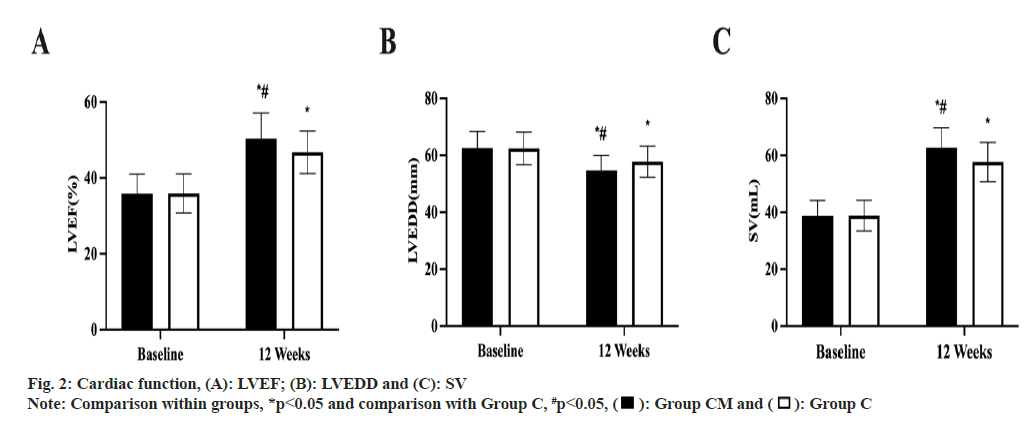
As shown in fig. 2, before treatment, there was no difference in LEVDD, LVEF and SV levels between the two groups (p>0.05). After treatment, LVEF and SV increased in both groups, and Group CM was higher than Group C (p<0.05); LEVDD decreased in both groups, and Group CM was lower than Group C (p<0.05).
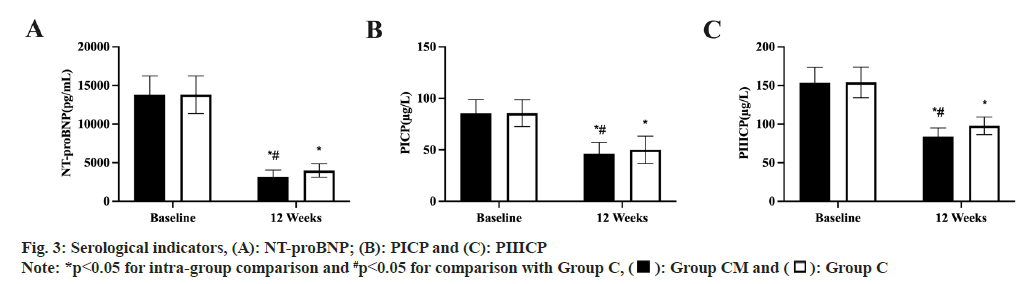
As shown in fig. 3, before treatment, there was no difference in serum NT-proBNP, PICP and PIIICP levels between the two groups (p>0.05). After treatment, serum N-Terminal Pro-B-Type Natriuretic Peptide (N-proBNP), PICP and PIIICP levels decreased in both groups, and Group CM was lower than Group C in both groups (p<0.05).
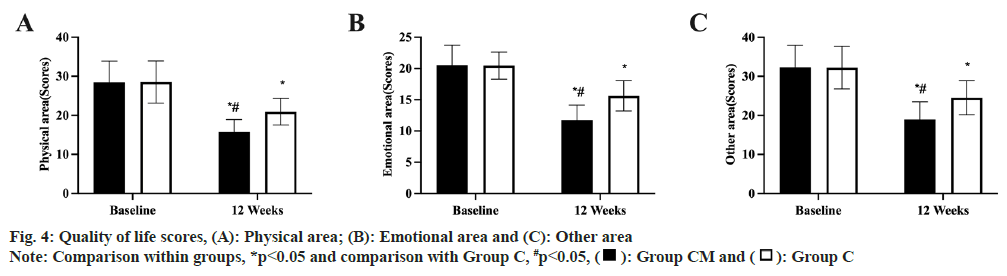
As shown in fig. 4, before treatment, there was no difference in all MLHFQ scores between the two groups (p<0.05). After treatment, all MLHFQ scores increased in both groups, with Group CM being higher than Group C (p<0.05).
In this study, patients with DCM were randomly divided into conventional drug-placebo and conventional drug-Renshen Yangrong decoction groups, and both groups received treatment for 12 w, during which time they were closely monitored. The results of the study showed that the addition of Renshen Yangrong decoction to conventional medication improved the therapeutic effect of DCM and was clinically beneficial.
The present study showed that the addition of Renshen Yangrong decoction to conventional medication had a significant synergistic effect between the two, increasing the overall efficiency of DCM treatment to 94.44 %, higher than that of 81.13 % when receiving conventional medication only, indicating that Ginseng Yangrong Tang combined with conventional medication was effective in treating DCM. The reason for this is presumed to be that the Ginseng in Renshen Yangrong decoction is a great tonic for the vital energy and warms the heart and yang, nourishing the qi to promote blood circulation and tranquilizing the mind and educating the mind. Atractylodes macrocephala and Poria cocos benefit the Qi, strengthen the spleen, calm the heart and induce diuresis. On this basis, Astragalus membranaceus is added to strengthen the spleen and nourish the lung to invigorate the blood, while white peony root nourishes the blood, softens the liver and astringes Yin to stop sweating; Angelica sinensis invigorates the blood and nourishes it, while cultivated land nourishes Yin and nourishes it. The three herbs are used together to nourish blood and promote the heart. This is complemented by Citrus reticulata blanco, which regulates Qi and transports the spleen, to prevent nourishment and greasiness from hindering the spleen; then combined with Schisandra chinensis to astringent the heart and tranquilize the mind, and Yuan Zhi to transport the heart and kidney. It also uses cassia twig to induce the fire to return to the source, guiding the herbs to encourage the growth of qi and blood in the Ying division, which helps to transform yang into qi. Prepared licorice benefits the qi and yang, restores the pulse and calms palpitations, nourishes the blood and nourishes the yin, and has the function of harmonizing all the medicines. The combination of these herbs achieves a mutual nourishing and glorifying effect on the five viscera and rules over the deficiencies. Combining the basic effects of conventional drugs can effectively improve DCM.
DCM has long been considered irreversible, but several studies in recent years have shown that nearly 40 % of patients with DCM develop significant left ventricular remodeling after drug therapy[9]. Left ventricular remodeling is one of the major determinants of prognosis in DCM, and therefore achieving left ventricular remodeling should be a major goal in the treatment of DCM patients. The process of left ventricular remodeling takes up to 2 y after DCM is diagnosed, and therefore patients with DCM need to receive long-term effective ongoing therapy[4]. Previous studies have shown that Ginseng Yang Rong Tang can inhibit pathological cardiomyocyte hypertrophy, prevent cardiac hypertrophy and improve ventricular remodeling[19], and the results of this study were also validated in this study. The results of this study showed that the LEVDD, LVEF and SV were significantly optimized, and the levels of NT-proBNP, PICP and PIIICP were reduced in patients with DCM treated with Renshen Yangrong decoction combined with conventional drugs, indicating that Renshen Yangrong decoction combined with conventional drugs could effectively delay the process of myocardial fibrosis and improve ventricular remodeling in patients with DCM. The abnormal proliferation of PICP and PIIICP can contribute to the remodeling of the myocardial collagen matrix, thus causing myocardial interstitial fibrosis[20]. Ginseng in Renshen Yangrong Decoction contains total ginsenosides that protect cardiomyocytes in experimental animals, improve myocardial metabolism, increase cardiac output per beat, and have bi-directional effects on cardiac function, blood vessels, blood pressure, and nerve centres[21]. Astragalus membranaceus contains a variety of active ingredients that regulate immune regulation, improve ventricular remodeling, anti-myocardial fibrosis and diuretic effects[22]. White peony root can increase serum erythrocyte and haemoglobin levels in mice with blood deficiency[23]. The combination of these drugs can effectively delay the process of myocardial fibrosis and ventricular remodeling in DCM and promote the improvement of cardiac function.
The quality of life and mental health of DCM patients are significantly limited[24]. Renshen Yangrong decoction can effectively promote the improvement of cardiac function. After treatment, the patient’s symptoms such as chest tightness, breathlessness and weakness are reduced, the patient’s activity endurance is increased and physical function is significantly improved. At the same time, negative emotions such as anxiety and irritability caused by limited physical function are alleviated, thus improving the emotional state. The optimization of the physical and emotional domains helps to facilitate other activities in daily life and work, thus improving the overall quality of life. In this study, patients with DCM who received Renshen Yangrong decoction in combination with conventional medication achieved better quality of life scores after treatment, suggesting that Renshen Yangrong decoction in combination with conventional western medicine helps improve the quality of life of patients with DCM.
In this study, no adverse reactions occurred in either group, indicating that the addition of Renshen Yangrong decoction to the conventional medicine was safe.
Firstly, the small number of study participants in this study may lead to a lack of credibility of the results and conclusions. Secondly, this study did not conduct a long follow-up of patients with DCM, and it is impossible to know the effect of the combination of Renshen Yangrong decoction with conventional drugs on the prognosis of patients with DCM. Finally, the dosage of conventional drugs was not recorded in the two groups in this study, and it is not possible to know whether the addition of Renshen Yangrong decoction would reduce the dosage of conventional drugs.
The combination of Renshen Yangrong decoction with conventional drugs is effective in the treatment of DCM and can effectively improve cardiac function. The mechanism of action may be related to delaying the process of myocardial fibrosis and ventricular remodeling, without increasing adverse effects and with high safety.
However, more clinical trial data are needed to verify whether this treatment protocol can be widely used and promoted in clinical practice.
Authors’ contribution:
Xiangyu Meng and Yue Du have contributed equally to this work.
Conflict of interests:
The authors declared no conflict of interests.
References
- Pinto YM, Elliott PM, Arbustini E, Adler Y, Anastasakis A, Böhm M, et al. Proposal for a revised definition of dilated cardiomyopathy, hypokinetic non-dilated cardiomyopathy, and its implications for clinical practice: A position statement of the ESC working group on myocardial and pericardial diseases. Eur heart J 2016;37(23):1850-8.
[Crossref] [Google Scholar] [PubMed]
- Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, et al. Classification of the cardiomyopathies: A position statement from the European society of cardiology working group on myocardial and pericardial diseases. Eur Heart J 2008;29(2):270-6.
[Crossref] [Google Scholar] [PubMed]
- Halliday BP, Prasad SK. The interstitium in the hypertrophied heart. JACC Cardiovasc Imaging 2019;12(11):2357-68.
[Crossref] [Google Scholar] [PubMed]
- Merlo M, Cannata A, Gobbo M, Stolfo D, Elliott PM, Sinagra G. Evolving concepts in dilated cardiomyopathy. Eur J Heart Fail 2018;20(2):228-39.
[Crossref] [Google Scholar] [PubMed]
- Yokokawa T, Sugano Y, Nakayama T, Nagai T, Matsuyama TA, Ohta-Ogo K, et al. Significance of myocardial tenascin-C expression in left ventricular remodelling and long-term outcome in patients with dilated cardiomyopathy. Eur J Heart Fail 2016;18(4):375-85.
[Crossref] [Google Scholar] [PubMed]
- Japp AG, Gulati A, Cook SA, Cowie MR, Prasad SK. The diagnosis and evaluation of dilated cardiomyopathy. J Am Coll Cardiol 2016;67(25):2996-3010.
[Crossref] [Google Scholar] [PubMed]
- Heart failure group of the cardiovascular disease branch of the Chinese medical association, heart failure committee of the Chinese physicians association, Chinese cardiovascular disease journal editorial committee. Heart failure specialty committee, Chinese cardiovascular disease journal editorial committee. Chinese heart failure diagnosis and treatment guidelines for diagnosis and treatment of heart failure in China, 2018. Chin J Cardiovasc Dis 2018;46(10):760.
- Merlo M, Pivetta A, Pinamonti B, Stolfo D, Zecchin M, Barbati G, et al. Long-term prognostic impact of therapeutic strategies in patients with idiopathic dilated cardiomyopathy: Changing mortality over the last 30 years. Eur J Heart Fail 2014;16(3):317-24.
[Crossref] [Google Scholar] [PubMed]
- Merlo M, Pyxaras SA, Pinamonti B, Barbati G, di Lenarda A, Sinagra G. Prevalence and prognostic significance of left ventricular reverse remodeling in dilated cardiomyopathy receiving tailored medical treatment. J Am Coll Cardiol 2011;57(13):1468-76.
[Crossref] [Google Scholar] [PubMed]
- Zecchin M, Merlo M, Pivetta A, Barbati G, Lutman C, Gregori D, et al. How can optimization of medical treatment avoid unnecessary implantable cardioverter-defibrillator implantations in patients with idiopathic dilated cardiomyopathy presenting with “SCD-HeFT criteria?” Am J Cardiol 2012;109(5):729-35.
[Crossref] [Google Scholar] [PubMed]
- Cao X, Liu H, Zhou M, Chen X, Long D. Comparative efficacy of five Chinese medicine injections for treating dilated cardiomyopathy with heart failure: A Bayesian network meta-analysis. J Ethnopharmacol 2022;282:114604.
[Crossref] [Google Scholar] [PubMed]
- Zhu YS, Li YL, Ju JQ, Du F, Zang YP, Wang XB, et al. Oral Chinese herbal medicine for treatment of dilated cardiomyopathy: A systematic review and meta-analysis. Evid Based Complement Alternat Med 2016;2016.
[Crossref] [Google Scholar] [PubMed]
- Zhang Q, Dong YJ. Clinical experience in the treatment of dilated cardiomyopathy with addition and subtraction of ginseng Yangrong Tang. J Integr Cardiovasc Cerebrovasc Dis Chin Western Med 2021;19(16):2862-4.
- Wang XJ, Yang K. Efficacy of ginseng Yangrong Tang combined with Tao Hong Siwu Tang in the treatment of angina pectoris in coronary heart disease (stasis blocking the arteries) and the effects on serum asprosin, NT-proBNP and Hcy. Sichuan Tradit Chin Med 2021;39(11):72-4.
- Pu XR, Feng Y, Wang MY. The use and research of ginseng Yangrong soup in the treatment of malignant tumors. Jilin Chin Med 2017;37(5):505-8.
- Chinese society of cardiovascular diseases, Chinese myocarditis cardiomyopathy collaborative group. Guidelines for the diagnosis and treatment of dilated cardiomyopathy in China. J Clin Cardiovasc Dis 2018;34(5):421-34.
- State administration of traditional Chinese medicine. Guidelines for clinical research on new Chinese medicines. Beijing: China Pharmaceutical Science and Technology Press; 2002. p. 74-7.
- Rector TS, Cohn JN. Minnesota Living with Heart Failure Questionnaire (MLHFQ): Assessing the quality of life in heart failure. Quality Life Res 1992;1(3):218-29.
- Tan JF, Wen W, Huang HC. Study on the role of TGF-β1/Smad signaling pathway in the inhibition of Ang II-induced cardiomyocyte hypertrophy by ginseng Yangrong Tang. China Pharm Guide 2020;18(15):1-3.
- Puntmann VO, Voigt T, Chen Z, Mayr M, Karim R, Rhode K, et al. Native T1 mapping in differentiation of normal myocardium from diffuse disease in hypertrophic and dilated cardiomyopathy. JACC Cardiovasc Imaging 2013;6(4):475-84.
[Crossref] [Google Scholar] [PubMed]
- Yu Z, Han SY, Li HX. Effects of ginseng and safflower extracts on cardiac hemodynamics in dogs with myocardial ischemia. Chin J Basic Chin Med 2012;18(7):777-82.
- Liu SY, Wang ZT. Research progress of Astragalus membranaceus in the treatment of dilated cardiomyopathy. Henan Tradit Chin Med 2017;37(6):993-6.
- Zhu YL, Zhang JJ, Huang YF. Comparative study on the tonic effect of white peony and red peony on blood deficiency in mice caused by cyclophosphamide and the effect on IL-3 and TNF-α. Chin J Tradit Chin Med 2014;29(4):1058-60.
- Steptoe A, Mohabir A, Mahon NG, McKenna WJ. Health related quality of life and psychological wellbeing in patients with dilated cardiomyopathy. Heart 2000;83(6):645-50.
[Crossref] [Google Scholar] [PubMed]
 : Group CM and
: Group CM and  : Group C
: Group C