- *Corresponding Author:
- Ning Deng
Department of Traditional Chinese Medicine, Xinjiang Medical University, Urumqi, Xinjiang 830011, China
E-mail: ningdeng_xj@163.com
| This article was originally published in a special issue,“Transformative Discoveries in Biomedical and Pharmaceutical Research” |
| Indian J Pharm Sci 2023:85(4) Spl Issue “164-168” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
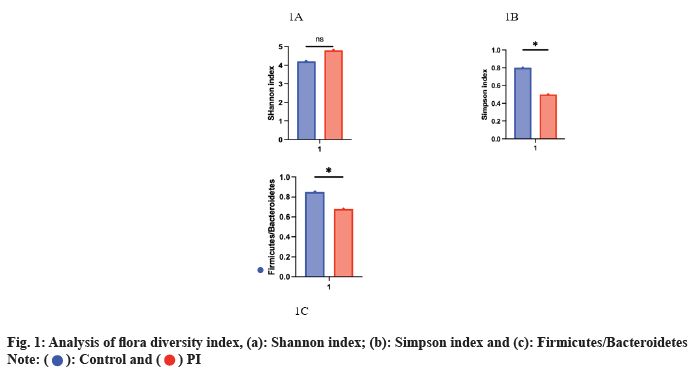
The study's objective is to investigate the correlation between gut microbiota and traditional Chinese medicine syndrome patterns in patients with chronic enteritis and insomnia. It also aims to assess the impact of antibiotic enema on the intestinal flora and traditional Chinese medicine syndrome types of patients with insomnia. Between January 2019 and December 2022, 60 patients with chronic insomnia (primary insomnia) were recruited from a hospital clinic based on exclusion and inclusion criteria. According to the standard of traditional Chinese medicine syndrome type, the intervention group received antibiotic enema treatment, while the control group received placebo enema treatment. The treatment period was 4 w. Statistical methods such as frequency and percentage were used to process the data to explore the correlation between chronic insomnia and traditional Chinese medicine syndrome types. The impact of antibiotic enema treatment on insomnia was evaluated. Initially, there was no significant difference in the Shannon and Simpson indices, which measure intestinal microbial diversity, between the two groups (p>0.05). However, beta-diversity analysis showed significant differences in intestinal microbial composition between the two groups (p<0.05). Specifically, the relative abundance of Firmicutes was lower in the intervention group, while the relative abundance of Bacteroidetes was higher. Post-intervention, the intestinal microbial composition of the intervention group demonstrated significant changes, characterized by a significant increase in the relative abundance of Bacteroidetes and a notable decrease in the Firmicutes/Bacteroidetes ratio (p<0.05). As for insomnia symptoms, sleep quality, sleep latency and sleep time in both groups were significantly improved after 4 w of treatment (p<0.05). However, the improvement in the intervention group was significantly higher than that in the control group (p<0.05). In addition, the proportion of patients with the syndrome of "liver qi stagnation and spleen deficiency" in the intervention group was significantly decreased, in contrast, the control group did not exhibit significant changes in their intestinal microbial composition (p<0.05). The findings of this study suggest a correlation between gut microbiota and traditional Chinese medicine syndrome patterns in patients with insomnia and chronic enteritis. Furthermore, antibiotic enema treatment was shown to significantly alleviate insomnia symptoms and enteritis.
Keywords
Insomnia, chronic enteritis, intestinal flora, traditional Chinese medicine, antibiotic
Insomnia is a common sleep disorder that affects many people around the world. Insomnia adversely affects both the physical and mental well-being of individuals. This can lead to symptoms such as mental stress, difficulty focusing, memory impairment and other related issues. Insomnia symptoms are associated with many lifestyle and environmental factors, but gut flora has also been suggested as a possible factor influencing insomnia[1-3]. Intestinal flora refers to the microbial community existing in the human gut, including bacteria, fungi, viruses and other microorganisms[4]. Intestinal flora is closely related to human immune system and metabolic function. In recent years, more and more studies have found that abnormal intestinal flora is related to the occurrence of various human diseases, such as obesity, diabetes, autoimmune diseases, etc.,[5-7]. Nevertheless, the association between atypical gut microbiota in patients with insomnia and Traditional Chinese Medicine (TCM) syndrome patterns remains poorly understood, warranting further investigation. TCM believes that the occurrence of insomnia is related to emotion, diet, rest and other factors, and treatment through syndrome differentiation can effectively improve the symptoms of insomnia. However, there is also a lack of in-depth research on the relationship between TCM syndrome types and intestinal flora abnormalities in insomnia patients[8-10]. Therefore, this study aimed to examine the potential link between gut microbiota and TCM syndrome patterns in patients with insomnia. And to evaluate the effect of antibiotic enema in the treatment of insomnia. Through the detection of intestinal flora and identification of TCM syndrome types in insomnia patients, we can understand the abnormal types of intestinal flora and characteristics of TCM syndrome types in insomnia patients, so as to explore the relationship between them. At the same time, we will also explore the role of antibiotic enema in the treatment of insomnia, in order to propose a more effective treatment plan. The study's findings hold immense significance in advancing our understanding of the underlying causes and treatment mechanisms of insomnia. If we can understand the abnormal types of intestinal flora and characteristics of TCM syndrome types of insomnia patients, and find appropriate treatment methods, the study's outcomes have the potential to enhance the overall well-being of individuals suffering from insomnia, thereby augmenting their quality of life. A total of 60 patients with chronic insomnia (Primary Insomnia (PI)) were recruited from a hospital clinic between January 2019 and December 2022. There were 34 males and 26 females, aged 37-78 y, with an average age of (35.14±20.16) y. All participants met the PI diagnostic criteria of the International Classification of Sleep Disorders and had reduced mental and physical activity. To eliminate the impact of medication, individuals who had used antibiotics during the first half of the study were excluded. Moreover, the study was carried out in compliance with the "Declaration of Helsinki" and received approval from the hospital's ethics committee. Before taking part, all individuals gave written agreement that they understood and agreed to participate. Randomization divided PI patients into two groups; an intervention group and a control group. The intervention group was treated with a metronidazole and levofloxacin antibiotic enema for 7 d, whereas the control group received a placebo enema. Both groups continued to receive regular treatment with PI during the study period. The study's primary objective was to evaluate alterations in gut microbiota by analyzing stool samples collected before and 1 w after the intervention. The secondary endpoints included changes in insomnia symptoms evaluated through the Pittsburgh Sleep Quality Index (PSQI) and alterations in TCM syndrome patterns, evaluated by licensed TCM practitioners. These assessments were conducted at the beginning of the study 1 w and 4 w after intervention. Subjective sleep quality score (0- 3) in the PSQI is a tool utilized to evaluate the subjective perception of sleep quality among individuals. The scores range from 0 to 3, with higher scores indicating poorer sleep quality and lower scores indicating better sleep quality. Sleep latency (0-3 points) refers to the time it takes to fall asleep. The score is 0-3 points. Sleep time (0-3 points) refers to the actual sleep time, the score is 0-3 points, 3 points means sleep time is very short, 0 points means sleep time is very long. Sleep efficiency (0-3 points) refers to the ratio of actual sleep time to sleep time, score is 0-3 points, 3 points indicates poor sleep efficiency and 0 points indicates high sleep efficiency. Sleep quality (0-3 points) refers to whether there are various sleep disorders during sleep, such as easy waking, night waking, nightmares, etc., score 0-3 points, 3 points indicates very poor sleep quality and 0 points indicates very good sleep quality. Primary sleep disorders (0-3 points) refers to various uncomfortable symptoms during sleep, such as apnea, cough, nasal congestion, etc. The score is 0-3 points, 3 points indicates serious sleep disorders and 0 points indicates no sleep disorders. Daytime dysfunction (0-3 points) refers to daytime fatigue, inattention, irritability and other symptoms, the score is 0-3 points, 3 points indicates serious daytime dysfunction and 0 points indicates no daytime dysfunction. The main manifestations of heart and liver restless insomnia are emotional instability, irritability, upset, insomnia, dreaminess, memory loss, headache, vertigo and other symptoms. Patients often feel palpitation, tachycardia or irregular heartbeat, and may be accompanied by dry mouth, bitter mouth, red tongue and other symptoms. The main manifestations of spleen and stomach weakness insomnia are loss of appetite, dyspepsia, diarrhea, abdominal distension, fatigue, insomnia and other symptoms. Patients often feel general weakness, heavy limbs, pale tongue and white moss. Insomnia symptoms in individuals with liver-spleen disharmony syndrome typically include chest tightness. Symptoms include burping, breast discomfort and pain, irritability, and sleep disturbance. Patients often feel chest tightness and pain, belching, dry mouth and bitter mouth, and tongue coating yellow and greasy. The main manifestations of insomnia are dizziness, tinnitus, waist and knee tenderness, mental fatigue, easy to catch a cold, insomnia and other symptoms. Patients often feel dizzy, tinnitus, waist and knees, cold hands and feet and so on. Red-tongue insomnia caused by heat disturbance is mainly manifested as dry mouth and thirst, bad breath, red tongue and yellow moss, insomnia and other symptoms. Patients often feel thirsty, dry mouth, yellow urine, constipation, bad breath, red tongue less moss or yellow greasy. Statistical Package for the Social Sciences (SPSS) version 26.0 was utilized for statistical analysis. Descriptive statistics are reported as mean±Standard Deviation (SD) of continuous variables, or median (quartile range), frequency and percentage of categorical variables. Post-test using Bonferroni correction. The significance level was set as p<0.05. In this study, 60 patients with PI were included and classified into five groups based on their TCM syndrome types; damp-heat intrinsic group, phlegmstasis interjection group, liver-qi stagnation group, liver-kidney Yin deficiency group, and spleen-kidney Yang deficiency group, labeled as group A, B, C, D and E, respectively. The baseline data analysis showed that there was no significant difference in gender, education level, age and duration of disease among the five groups (p>0.05) as shown in Table 1. No significant difference in gut microbiota diversity index (Shannon and Simpson indices) was observed between the two groups at baseline (p>0.05). However, Beta (β)-diversity analysis showed significant differences in intestinal microbial composition between the two groups (p<0.05). The study found that the intervention group had a lower relative abundance of Firmicutes compared to the control group. Additionally, the intervention group had a higher relative abundance of Bacteroidetes. This suggests that the intervention may have had an effect on the composition of the gut microbiome, specifically on the relative proportions of these two bacterial phyla. However, further research is needed to determine the potential health implications of these changes in gut microbiota composition. After the intervention, the intestinal microbial composition of the intervention group changed significantly and the relative abundance of Bacteroidetes increased significantly, while the ratio of Firmicutes/ Bacteroidetes decreased significantly (p<0.05) as shown in fig. 1. With respect to insomnia symptoms, sleep quality, sleep latency and sleep time were significantly improved in both groups after 4 w of treatment (p<0.05). However, the improvement in the intervention group was significantly higher than that in the control group (p<0.05). In addition, the proportion of patients with the syndrome of "liver qi stagnation and spleen deficiency", there was a significant decrease in the intervention group, whereas no noteworthy alteration was detected in the control group (p<0.05) as shown in Table 2. Insomnia is a common sleep disorder, and its pathogenesis is complex, involving many factors, including changes in gut microbiome. This study aims to explore the correlation between intestinal flora of insomnia patients and TCM syndrome types and evaluate the efficacy of antibiotic enema therapy on insomnia[11-14]. The results showed that the intestinal flora structure of insomnia patients had significant changes and the flora abundance and diversity decreased, and the proportion of dominant flora decreased. This is consistent with previous findings suggesting that insomnia symptoms are closely related to changes in gut flora. At the same time, this study also found that TCM syndrome types such as liver depression and qi stagnation, and heart and spleen disorder were prevalent in patients, which was consistent with concepts such as "heart and spleen are homologous" and "liver main drainage" in TCM theory[15-18]. These results suggest that the intestinal micro ecological environment and TCM syndromes of insomnia patients may interact with each other and participate in the occurrence and development of insomnia. In response to the above research results, this study conducted an antibiotic enema treatment experiment, and the results showed that the symptoms of insomnia and enteritis were significantly improved in the treatment group, while the treatment effect was not good in the control group. These results suggest that antibiotic enema therapy may be an effective way to improve insomnia symptoms. At the same time, this study also found that the proportion of patients with liver qi stagnation and spleen deficiency syndrome in the treatment group was significantly reduced. This further confirmed the correlation between intestinal micro ecological environment and TCM syndrome types. It should be noted that although antibiotic enema therapy can improve symptoms of insomnia and enteritis, it may have a negative impact on intestinal microbial community[19]. Therefore, its efficacy and safety need to be weighed in clinical application. In addition, only 60 patients with PI were included in this study as research objects, with a relatively small sample size, so it is necessary to further expand the sample size to further verify the reliability of the research results. Further studies are needed to confirm the conclusions of this study, as TCM syndrome typing is a traditional diagnosis method in TCM and there have been relatively few studies on the relationship between the gut microbiome and insomnia in modern medicine[20-23].
| TCM syndrome type | A | B | C | D | E | P |
|---|---|---|---|---|---|---|
| Gender | 15/10 (60 %) | 14/11 (56 %) | 12/13 (48 %) | 11/14 (44 %) | 14/11 (56 %) | 0.63 |
| Year | 59.4±6.2 | 61.1±5.3 | 60.3±4.9 | 59.7±6.1 | 60.8±5.2 | 0.42 |
| Course of disease | 8.5±3.2 | 8.1±2.8 | 9.2±3.1 | 8.9±2.9 | 8.4±2.6 | 0.27 |
| Educational level | 9/16 (36 %) | 10/15 (40 %) | 12/13 (48 %) | 13/12 (52 %) | 10/15 (40 %) | 0.18 |
Note: p>0.05, the difference was not statistically significant
Table 1: Comparison of Basic Data of Patients with Tcm Syndrome Types in Five Groups (X̅±S, N %)
| Treatment group/control group | Sleep quality (PSQI score) | Sleep latency (min) | Sleep time (h) |
|---|---|---|---|
| Pre-treatment | 12.3 | 37.5 | 5.9 |
| After treatment | 6.7 | 22.4 | 7.2 |
| Therapeutic effect change | -5.6 | -15.1 | 1.3 |
| Before control | 12.4 | 36.7 | 5.8 |
| After control | 10.1 | 30.2 | 6.1 |
| Control effect change | -2.3 | -6.5 | 0.3 |
Table 2: Comparison of Sleep Efficacy After Antibiotic Therapy
At the same time, the sample size of this study is small and the treatment time is short, so the longterm follow-up study needs to be further carried out[24-26]. In conclusion, this study suggests a correlation between gut microbiota and TCM syndrome types in patients with insomnia. The findings could help deepen our understanding of insomnia and provide new ideas for developing more effective treatments. At the same time, this study also reminds us that the TCM syndrome type and intestinal microbiome status of patients should be comprehensively considered in the clinical treatment process, so as to achieve a more individualized and targeted treatment plan.
Conflict of interests:
The authors declared no conflict of interests.
References
- Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun 2020;88:901-7.
- Tang Y, Gong M, Qin X, Su H, Wang Z, Dong H. The therapeutic effect of aromatherapy on insomnia: A meta-analysis. J Affect Disord 2021;288:1-9.
[Crossref] [Google Scholar] [PubMed]
- Mah J, Pitre T. Oral magnesium supplementation for insomnia in older adults: A systematic review and meta-analysis. BMC Complement Med Ther 2021;21(1):125.
[Crossref] [Google Scholar] [PubMed]
- Cénat JM, Blais-Rochette C, Kokou-Kpolou CK, Noorishad PG, Mukunzi JN, McIntee SE, et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res 2021;295:113599.
[Crossref] [Google Scholar] [PubMed]
- Sumsuzzman DM, Choi J, Jin Y, Hong Y. Neurocognitive effects of melatonin treatment in healthy adults and individuals with Alzheimer’s disease and insomnia: A systematic review and meta-analysis of randomized controlled trials. Neurosci Biobehav Rev 2021;127:459-73.
[Crossref] [Google Scholar] [PubMed]
- Choi K, Lee YJ, Park S, Je NK, Suh HS. Efficacy of melatonin for chronic insomnia: Systematic reviews and meta-analyses. Sleep Med Rev 2022;66:101692.
[Crossref] [Google Scholar] [PubMed]
- Shen Y, Wang YF. Chronic active Epstein–Barr virus enteritis: A literature review. J Dig Dis 2022;23(5-6):248-52.
[Crossref] [Google Scholar] [PubMed]
- Nunez P, Mateo SG, Quera R, Gomollón F. Inflammatory bowel disease and the risk of cardiovascular diseases. Gastroenterol Hepatol 2021;44(3):236-42.
- McAlindon ME. Cryptogenic multifocal ulcerating stenosing enteritis and other under-recognised small bowel inflammatory enteropathies. Curr Opin Gastroenterol 2022;38(3):279-84.
[Crossref] [Google Scholar] [PubMed]
- Ma Q, Li Y, Li P, Wang M, Wang J, Tang Z, et al. Research progress in the relationship between type 2 diabetes mellitus and intestinal flora. Biomed Pharmacother 2019;117:109138.
[Crossref] [Google Scholar] [PubMed]
- Guo X, Okpara ES, Hu W, Yan C, Wang Y, Liang Q, et al. Interactive relationships between intestinal Flora and Bile acids. Int J Mol Sci 2022;23(15):8343.
[Crossref] [Google Scholar] [PubMed]
- Huang Z, Chen Z, Li X, Tao J, Li Y, Zhu X, et al. The effect of intestinal flora intervention on bone development in children: A systematic review and meta-analysis. Complement Ther Clin Pract 2022;48:101591.
[Crossref] [Google Scholar] [PubMed]
- Ding Q, Hu Y, Fu Y, Qian L. Systematic review and meta-analysis of the correlation between intestinal flora and gestational diabetes mellitus. Ann Palliat Med 2021;10(9):9752-64.
[Crossref] [Google Scholar] [PubMed]
- Liu C, Guo X, Chang X. Intestinal flora balance therapy based on probiotic support improves cognitive function and symptoms in patients with Alzheimer’s disease: A systematic review and meta-analysis. Biomed Res Int 2022;2022:4806163.
[Crossref] [Google Scholar] [PubMed]
- Luo J, Xu Z, Noordam R, van Heemst D, Li-Gao R. Depression and inflammatory bowel disease: A bidirectional two-sample mendelian randomization study. J Crohn's Colitis 2022;16(4):633-42.
[Crossref] [Google Scholar] [PubMed]
- Ahmed W, Galati J, Kumar A, Christos PJ, Longman R, Lukin DJ, et al. Dual biologic or small molecule therapy for treatment of inflammatory bowel disease: A systematic review and meta-analysis. Clin Gastroenterol Hepatol 2022;20(3):e361-79.
[Crossref] [Google Scholar] [PubMed]
- Pan Y, Liu Y, Guo H, Jabir MS, Liu X, Cui W, et al. Associations between folate and vitamin B12 levels and inflammatory bowel disease: A meta-analysis. Nutrients 2017;9(4):382.
[Crossref] [Google Scholar] [PubMed]
- Carvalho AC, Souza GA, Marqui SV, Guiguer ÉL, Araújo AC, Rubira CJ, et al. Cannabis and canabidinoids on the inflammatory bowel diseases: Going beyond misuse. Int J Mol Sci 2020;21(8):2940.
[Crossref] [Google Scholar] [PubMed]
- Knowles SR, Graff LA, Wilding H, Hewitt C, Keefer L, Mikocka-Walus A. Quality of life in inflammatory bowel disease: A systematic review and meta-analyses—part I. Inflamm Bowel Dis 2018;24(4):742-51.
[Crossref] [Google Scholar] [PubMed]
- Wang T, Xu C, Pan K, Xiong H. Acupuncture and moxibustion for chronic fatigue syndrome in traditional Chinese medicine: A systematic review and meta-analysis. BMC Complement Altern Med 2017;17(1):1-1.
[Crossref] [Google Scholar] [PubMed]
- Qi H, Liu R, Zheng W, Zhang L, Ungvari GS, Ng CH, et al. Efficacy and safety of traditional Chinese medicine for Tourette's syndrome: A meta-analysis of randomized controlled trials. Asian J Psychiatr 2020;47:101853.
[Crossref] [Google Scholar] [PubMed]
- de Crescenzo F, D'Alò GL, Ostinelli EG, Ciabattini M, di Franco V, Watanabe N, et al. Comparative effects of pharmacological interventions for the acute and long-term management of insomnia disorder in adults: A systematic review and network meta-analysis. Lancet 2022;400(10347):170-84.
[Crossref] [Google Scholar] [PubMed]
- Zhang J, Zhang Z, Huang S, Qiu X, Lao L, Huang Y, et al. Acupuncture for cancer-related insomnia: A systematic review and meta-analysis. Phytomedicine 2022;102:154160.
[Crossref] [Google Scholar] [PubMed]
- Gebara MA, Siripong N, Dinapoli EA, Maree RD, Germain A, Reynolds CF, et al. Effect of insomnia treatments on depression: A systematic review and meta-analysis. Depress Anxiety 2018;35(8):717-31.
[Crossref] [Google Scholar] [PubMed]
- Kim SA, Lee SH, Kim JH, van Den Noort M, Bosch P, Won T, et al. Efficacy of acupuncture for insomnia: A systematic review and meta-analysis. Am J Chin Med 2021;49(5):1135-50.
[Crossref] [Google Scholar] [PubMed]
- Trauer JM, Qian MY, Doyle JS, Rajaratnam SM, Cunnington D. Cognitive behavioral therapy for chronic insomnia: A systematic review and meta-analysis. Ann Intern Med 2015;163(3):191-204.
[Crossref] [Google Scholar] [PubMed]
 ): Control and (
): Control and ( ) PI
) PI



