- *Corresponding Author:
- Huifang Yu
Critical Care Medicine Department Alpha, Renmin Hospital of Wuhan University (Hubei General Hospital), Wuhan, China
E-mail: 923318392@qq.com
|
This article was originally published in a special issue, "Therapeutic Perspectives in Biomedical research and Pharmaceutical Sciences and their nursing methods" |
| Indian J Pharm Sci 2021:83(4)Spl issue “34-39” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To explore the effect of programmed sedation and analgesia combined with nursing intervention on weaning and extubation of patients with tracheal intubation. 128 patients who underwent tracheal intubation in our hospital from January 2020 to March 2021 were randomly divided into two groups. The control group received routine intensive care intervention, used and adjusted analgesic and sedative drugs according to the doctor’s instructions. The intervention group was evaluated and monitored for programmed sedation and analgesia based on the control group. The mechanical ventilation, with tube and intensive care unit hospitalization time, delirium, unplanned extubation, ventilator-associated pneumonia and deep vein thrombosis were compared between the two groups. The incidence of adverse events, nursing satisfaction and the dosage of analgesic and sedative drugs were evaluated. The mechanical ventilation, with tube and intensive care unit hospitalization time were significantly shorter in intervention group (p<0.05). The incidence of adverse events such as delirium, unplanned extubation, ventilator-associated pneumonia and deep vein thrombosis in the intervention group was significantly lower than that in the control group (p<0.05), nursing satisfaction has also increased significantly. Program analgesia and sedation combined care for intensive care unit patients with tracheal intubation can improve the clinical efficacy, shorten the time of weaning extubation and intensive care unit stay, reduce the amount of sedatives, reduce the incidence of related adverse reactions and improve nursing satisfaction.
Keywords
Programmed analgesia and sedation, ventilator-associated pneumonia, extubation, analgesia, sedation
Tracheal intubation is the main treatment measure for patients with respiratory failure or decreased airway protection in intensive care unit (ICU) [1,2]. An ICU survey study collected from all hospitals in Scotland showed that the incidence of ICU intubation was as high as 70 % [3]. Compared with the anesthesiology department, the rate of adverse consequences and serious defects of ICU airway management is much higher [4,5]. In addition, ICU patients with tracheal intubation are mostly critically ill patients. The torture of the disease, various restraints, and invasive operations can easily cause anxiety and psychological trauma to patients with mechanical ventilation (MV) [6,7]. Analgesia and sedation, as the basic treatment for mechanically ventilated patients in ICU, can improve patient comfort, reduce anxiety, promote nursing and adapt to assisted ventilation [8]. However, inappropriate analgesia and sedation can prolong the patient’s MV time, increase the incidence of ventilator-associated pneumonia (VAP), deep vein thrombosis, accidental extubation and the patient’s painful memories during ICU treatment reaction [9-11].
Programmed sedation and analgesia (PSA) is based on analgesia and systematically adjusts the amount of sedatives according to the goal of sedation, which is conducive to grasping the balance between insufficient sedation and excessive sedation [12]. However, in actual work, there are still many problems in the implementation of PSA, such as ignoring pain and pain assessment, uncertain frequency of sedation assessment, insufficient sedation concept and few people with moderate sedation [13,14]. Therefore, the effective implementation of PSA depends on the close cooperation of medical and nursing care to improve the prognosis of patients [15].
Therefore in our study, the combined care of programmed analgesia and sedation for ICU patients with tracheal intubation aims to explore the impact on patients with weaning extubation and related complications, to provide reference for clinical treatment and nursing.
Materials and Methods
General data:
128 cases of tracheal patients in ICU of our hospital from January 2020 to March 2021 were selected as the study population. The inclusion criteria: Age >18 y; Complete clinical data; Obtain patients or the patient’s technical informed consent was approved by the ethics department of our hospital. Exclusion criteria: suffer from severe neurological and muscle diseases; use drugs and long-term opioids to relieve pain and cause dependence; patients with severe mental illness; patients who require deep sedation. The main diagnoses of the patient include: cerebral hemorrhage, type 2 diabetic ketoacidosis, gastrointestinal hemorrhage, respiratory failure, acute severe pancreatitis, cervical spinal cord injury, septic shock, lung infection and other diseases. Use random number table method to divide into intervention group and control group.
Methods:
Before sedation and analgesia treatment, both groups of patients removed reversible factors such as the ward environment, avoided unnecessary iatrogenic stimulation, corrected shock, hypoglycemia and other adverse reactions and assessed the patient’s disease itself that requires sedation and analgesia and whether there are any problems. Comfortable, unable to cooperate with treatment, risk of accidental extubation, etc. The patient’s analgesic drugs were fentanyl (loading dose 0.7-1.5 μg/kg, maintenance dose 0.2-1.8 μg/kg.h) or sufentanil (loading dose 0.15-0.25 μg/kg, maintenance dose 0.1-0.3 μg/kg.h); sedative drugs are dexmedetomidine (loading dose 1 μg/kg, maintenance dose 0.2-0.7 μg/kg); propofol (loading dose 1-2.5 mg/ kg, maintenance dose 0.5-4.0 mg/kg.h), midazolam (loading dose 2-3 mg, maintenance dose 0.05 mg/ kg.h). The control group received routine intensive care intervention and used and adjusted analgesia and sedative drugs according to doctor’s instructions. The intervention group received programmed sedation and analgesia evaluation and monitoring on the basis of the control group. Basic pain assessment: Use the intensive care pain observation tool (COPT) for basic pain assessment and evaluate the analgesic effect every hour. If necessary, increase the dose of analgesic drugs appropriately until COPT ≤3 min and then change to a 4 h evaluation [16]. If the dose of sedative drugs is not reached appropriately, increase. Evaluation of delirium: If the patient has acute changes or fluctuations in the state of consciousness, characteristics of attention disorder and changes in the level of consciousness, confusion, etc, perform a confusion assessment method for the intensive care unit (CAM-ICU) delirium assessment in a timely manner and report to the doctor to take necessary measures in time. Daily wake-up strategy: In order to avoid drug accumulation and prolong the drug effect [19], stop the sedative on the patient at 7:00 every day and pay close attention to the change of the patient’s vital signs and recovery of consciousness. Weaning care: Decrease the daily dose of sedatives by 10 %-25 %. Observe whether the patient has any adverse reactions after weaning, such as delirium, restlessness, irritability, etc., once found, notify the doctor immediately and began to implement sedation assessment. Basic assessment of sedation: Richmond agitation-sedation scale (RASS) are scored every hour, so that patients are between 0 and -2 points during the day and between -1 and +3 at night [17]. If the dose of sedative drugs is not reached appropriately, increase. Evaluation of delirium: If the patient has acute changes or fluctuations in the state of consciousness, characteristics of attention disorder, changes in the level of consciousness, confusion, etc., perform a CAM-ICU delirium assessment in a timely manner and report to the doctor to take necessary measures in time [18]. Daily wake-up strategy: In order to avoid drug accumulation and prolong the drug effect [19], stop the sedative on the patient at 7:00 every day and pay close attention to the change of the patient’s vital signs and recovery of consciousness. Weaning care: Decrease the daily dose of sedatives by 10 %-25 %. Observe whether the patient has any adverse reactions after weaning, such as delirium, restlessness, irritability, etc., once found and notify the doctor immediately. Psychological intervention: When the patient is awake, provide psychological care to eliminate the fear of mechanical ventilation, inform the patient of the safety of the environment in which the patient is located and the good treatment effect and other beneficial psychological hints, so as to reduce the painful memory of the patient during the treatment.
Outcome indicators:
We compared the MV time between the two groups, the length of stay in the ICU, the incidence of delirium, the incidence of unplanned extubation, the incidence of VAP and the amount of analgesic and sedative drugs and the nursing satisfaction the degree was evaluated.
Statistical method:
All analyses were performed using the statistical software EmpowerStats. Count data is expressed as n/%, with χ2 test, measurement data is expressed with x±s and t test, with p<0.05 as the difference is statistically significant. The p value of p<0.05 is considered to be statistically significant.
Results and Discussion
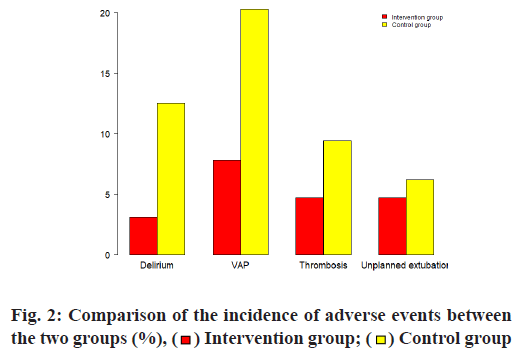
64 patients in the intervention group, aged from 29 to 80 y old, with an average age of 59 y old, 34 females. Acute Physiology and Chronic Health Score (APACEII) 34 points; 64 patients in the control group, aged between 31 and 82 y old, with an average age of 57 y, 35 female cases, APACEII score 32 points. The baseline information was similar in two groups. See for details Table 1. The MV, with tube and ICU stay time were significantly shorter in the intervention group (p<0.05). See Table 2 and fig. 1 for details.
| Intervention group (n=64) | Control group (n=64) | t/χ2 | P | |
|---|---|---|---|---|
| Age | 59.1±19.1 | 57.3±18.6 | 0.53 | 0.59 |
| Gender: (Female) | 34 (53.1 %) | 35 (54.7 %) | 0.03 | 0.85 |
| Type of disease | ||||
| Cerebral hemorrhage | 10 (15.6 %) | 11 (17.2 %) | 0.06 | 0.81 |
| Diabetic ketoacidosis | 2 (3.1 %) | 1 (1.6 %) | 0.34 | 0.55 |
| Gastrointestinal bleeding | 8 (12.5 %) | 6 (9.4 %) | 0.32 | 0.57 |
| Acute severe pancreatitis | 3 (4.7 %) | 2 (3.1 %) | 0.21 | 0.64 |
| Cervical spinal cord injury | 2(3.1 %) | 3 (4.7 %) | 0.41 | 0.60 |
| Septic shock | 20 (31.2 %) | 19 (29.7 %) | 0.04 | 0.84 |
| Lung infection | 19 (29.7 %) | 22 (34.4 %) | 0.32 | 0.50 |
| APACHEII | 32.1±15.4 | 34.1±16.6 | -0.70 | 0.48 |
Table 1: Baseline Data of the Two Groups
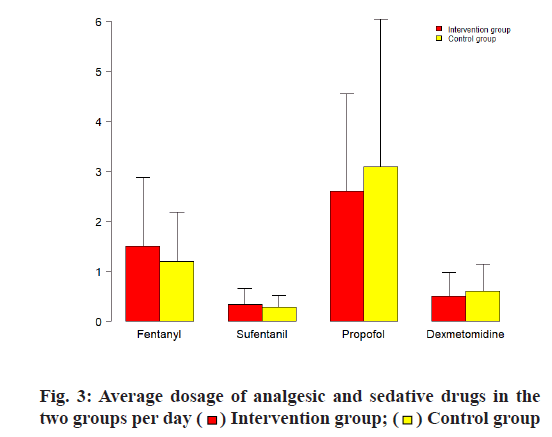
The incidence of delirium in the intervention group was 3.1 % and the incidence of VAP was 12.5 %, which were significantly lower than those in the control group (p<0.05); the incidence of deep vein thrombosis and unplanned extubation was not significant and difference between two groups (p>0.05), see Table 3, fig. 2 for details.
| Intervention group (n=64) | Control group (n=64) | t | P | |
|---|---|---|---|---|
| MV (d) | 3.5±1.7 | 4.2±2.0 | -2.13 | 0.03 |
| With tube time (d) | 3.8±1.8 | 4.5±2.0 | -2.03 | 0.03 |
| ICU stay (d) | 6.0±3.2 | 7.5±3.3 | -2.61 | 0.01 |
Table 2: Comparison of MV with Tube and ICU Stay Time Between the Two Groups
| Intervention group (n=64) | Control group (n=64) | χ2 | P | |
|---|---|---|---|---|
| Delirium | 2 (3.1 %) | 8 (12.5 %) | 3.91 | 0.04 |
| VAP | 5 (7.8 %) | 13 (20.3 %) | 4.14 | 0.04 |
| Thrombosis | 3 (4.7 %) | 6 (9.4 %) | 1.08 | 0.29 |
| Unplanned extubation | 3 (4.7 %) | 4 (6.2 %) | 0.69 | 0.15 |
Table 3: Comparison of the Incidence of Adverse Events Between the Two Groups
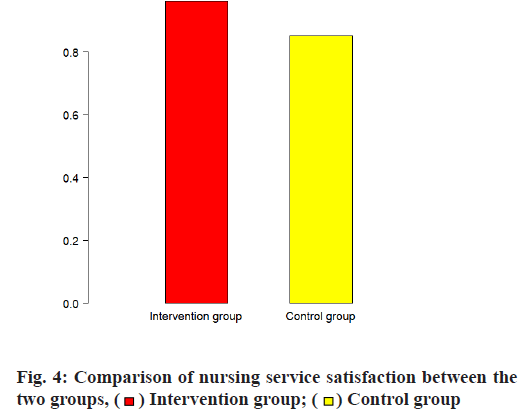
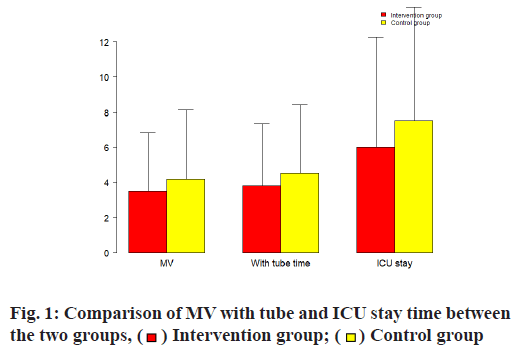
The sedative drugs were significantly lower in the intervention group, whether it was propofol or dexmedetomidine, while the analgesic drugs used more than the control group (p< 0.05), see Table 4, fig. 3 for details. The nursing satisfaction rate was significantly higher in the intervention group (p <0.05), see Table 5, fig. 4 for details.
| Intervention group (n=64) | Control group (n=64) | t | P | |
|---|---|---|---|---|
| Fentanyl (mg) | 1.5±0.7 | 1.2±0.5 | 2.73 | 0.05 |
| Sufentanil (mg) | 0.34±0.16 | 0.28±0.12 | 2.94 | 0.04 |
| Propofol (g) | 2.6±1.0 | 3.1±1.5 | -2.21 | 0.02 |
| Dexmedetomidine (mg) | 0.5±0.24 | 0.6±0.28 | -2.16 | 0.04 |
| Midazolam (mg) | 71±21.6 | 82±31.2 | -2.52 | 0.01 |
Table 4: The Average Dosage of Analgesic and Sedative Drugs in the Two Groups Per Day
| Very dissatisfied | Dissatisfied | Fair | Satisfied | Very satisfied | Total satisfaction rate | |
|---|---|---|---|---|---|---|
| Intervention group | 0 (0 %) | 1 (1.5 %) | 1 (1.5 %) | 30 (45 %) | 32 (50 %) | 62 (96.9 %) |
| Control group | 1 (1.5 %) | 2 (3.0 %) | 6 (9.0 %) | 29 (40.6 %) | 26 (71.8 %) | 55 (85.9 %) |
| χ2 | 4.87 | |||||
| p | 0.02 |
Table 5: Comparison of Nursing Service Satisfaction Between the Two Groups [n (%)]
Analgesia and sedation are part of the treatment of ICU patients with tracheal intubation. Excessive sedation and insufficient sedation can bring hidden dangers to the life safety of patients and increase unnecessary medical expenditures. In the past, in order to facilitate the management of ICU, the traditional sedation was mostly based on deep sedation [20]. With the development of medical technology and the advancement of mechanical ventilation, the disadvantages of deep sedation have become increasingly apparent [21]. A multicenter prospective cohort study conducted in 45 ICUs from Brazil showed that early deep sedation was associated with adverse outcomes and was an independent predictor of hospital mortality in mechanically ventilated patients [22]. In a multicenter prospective longitudinal cohort study of 11 hospitals in Malaysia, regardless of the sedative used, early deep sedation was independently associated with delayed extubation and high mortality [23]. Excessive sedation can also increase the length of stay in the ICU [24,25]. However, insufficient analgesia and sedation will not only increase the work intensity of the staff, but also increase the pain of the patient, increase the patient’s anxiety, restlessness and even endanger the patient’s life [26,27]. Studies have shown that most ICU survivors have pain and anxiety in their memories of ICU [28].
Therefore, to reduce individual differences in critically ill patients, it is necessary to implement PSA for ICU patients [29]. As one of the important personnel in the management of ICU patients, nurses are important assessors of analgesia and sedation status, as well as important implementers of sedation measures and play an important role in the implementation of PSA [24,30]. PSA joint care is a patient-centered nursing intervention model that requires planned and targeted completion of various nursing tasks, provides patients with individualized solutions and uses the smallest sedatives and maximum humane care to enable patients To achieve the optimal state of analgesia and sedation, while avoiding the related complications caused by insufficient and excessive analgesia and sedation and reducing the incidence of adverse events [31]. Our results also confirm the above view: PSA combined nursing intervention can significantly reduce the time of mechanical ventilation, ICU stay, the incidence of delirium, the incidence of VAP and avoid large-dose infusion of sedative drugs, which improves nursing satisfaction.
The PSA combined nursing intervention model can significantly improve the prognosis of patients and should become a template for the care of patients with ICU tracheal intubation for analgesia and sedation. However, since most of its studies are from nonrandomized controlled trials and the sample size is not large enough, the level of evidence is biased low [32]. A study showed that the implementation rate of the PSA program was only 43.7 % and there was a significant difference in the compliance rate between different hospitals [33]. A sample survey of medical staff in 101 ICUs across Belgium found that the effective rate was only 60 % and increasing the autonomy of nurses and assisting in the detection and management of sedatives can help optimize the goal of analgesia [34]. Most nurses encounter different challenges when using analgesia and sedation strategies. Therefore, it is necessary for nurses to make analgesia and analgesia strategies suitable for them.
This study has some limitations. Since our research population is mainly for Chinese people, it is necessary to be cautious to interpret this result to other populations; secondly, our research sample size is too small and it is not ruled out that some errors may be brought about in the research results [35-37].
The combined care of programmed analgesia and sedation for ICU patients with tracheal intubation can improve the clinical efficacy, shorten the event of weaning extubation and ICU admission, reduce the amount of sedatives and reduce the incidence of related adverse reactions, improve nursing satisfaction.
Conflicts of interest:
The authors declared no conflict of interest.
References
- Jiang J, Kang N, Li B, Wu AS, Xue FS. Comparison of adverse events between video and direct laryngoscopes for tracheal intubations in emergency department and ICU patients?a systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med 2020;28(1):10.
- Chen W, Chen J, Wang H, Chen Y. Application of bedside real-time tracheal ultrasonography for confirmation of emergency endotracheal intubation in patients in the intensive care unit. J Int Med Res 2020;48(4):0300060519894771.
- Simpson GD, Ross MJ, McKeown DW, Ray DC. Tracheal intubation in the critically ill: a multi-centre national study of practice and complications. Br J Anaesth 2012;108(5):792-9.
- Higgs A, McGrath BA, Goddard C, Rangasami J, Suntharalingam G, Gale R, et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth 2018;120(2):323-52.
- Mosier JM, Sakles JC, Law JA, Brown III CA, Brindley PG. Tracheal intubation in the critically ill. Where we came from and where we should go. Am J Respir Crit Care Med 2020;201(7):775-88.
- Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJ, Pandharipande PP, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility and sleep disruption in adult patients in the ICU. Crit Care Med 2018;46(9):e825-73.
- Correia MDL, Duran ECM. Conceptual and operational definitions of the components of the nursing diagnosis Acute Pain (00132). Rev Lat Am Enfermagem 2017;25:e2973.
- Egerod I, Jensen MB, Herling SF, Welling KL. Effect of an analgo-sedation protocol for neurointensive patients: a two-phase interventional non-randomized pilot study. Crit Care 2010;14(2):1-9.
- Neme D, Aweke Z, Micho H, Mola S, Jemal B, Regasa T. Evidence-Based Guideline for Adult Sedation, Pain Assessment, and Analgesia in a Low Resource Setting Intensive Care Unit. Int J Gen Med 2020;13:1445.
- Devlin JW, Skrobik Y, Rochwerg B, Nunnally ME, Needham DM, Gelinas C, et al. Methodologic innovation in creating clinical practice guidelines: insights from the 2018 society of critical care medicine pain, agitation/sedation, delirium, immobility and sleep disruption guideline effort. Crit Care Med 2018;46(9):1457-63.
- Kayir S, Ulusoy H, Dogan G. The effect of daily sedation-weaning application on morbidity and mortality in intensive care unit patients. Cureus 2018;10(1):e2062.
- Skrobik Y, Ahern S, Leblanc M, Marquis F, Awissi DK, Kavanagh BP. Protocolized intensive care unit management of analgesia, sedation, and delirium improves analgesia and subsyndromal delirium rates. Anesth Analg 2010;111(2):451- 63.
- Mukhopadhyay A, Tai BC, Remani D, Phua J, Cove ME, Kowitlawakul Y. Age related inverse dose relation of sedatives and analgesics in the intensive care unit. Plos one 2017;12(9):e0185212.
- Gill KV, Voils SA, Chenault GA, Brophy GM. Perceived versus actual sedation practices in adult intensive care unit patients receiving mechanical ventilation. Ann Pharmacother 2012;46(10):1331-9.
- Kydonaki K, Hanley J, Huby G, Antonelli J, Walsh TS. Challenges and barriers to optimising sedation in intensive care: a qualitative study in eight Scottish intensive care units. BMJ open 2019;9(5):e024549.
- Maatouk H, Al Tassi A, Fawaz MA, Itani MS. Nurses? evaluation of critical care pain observation tool (CPOT) implementation for mechanically ventilated intensive care patients. Data Brief 2019;25:103997.
- Jouan Y, Seegers V, Meziani F, Grelon F, Megarbane B, Anguel N, et al. Effects of mean arterial pressure on arousal in sedated ventilated patients with septic shock: a SEPSISPAM post hoc exploratory study. Ann Intensive Care 2019;9(1):54.
- Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med 2001;29(7):1370-9.
- Strøm T, Stylsvig M, Toft P. Psychological long-term effects of a no-sedation protocol in critically ill patients. Crit Care 2011;15(1):1-90.
- Gong Y, Yang H, Xie J, Liu J, Zhou J, Ma P. ICU Physicians? Perception of Patients? Tolerance Levels in Light Sedation Impacts Sedation Practice for Mechanically Ventilated Patients. Front Med 2019;6:226.
- Fuller BM, Roberts BW, Mohr NM, Pappal RD, Stephens RJ, Yan Y, et al. A study protocol for a multicentre, prospective, before-and-after trial evaluating the feasibility of implementing targeted SEDation after initiation of mechanical ventilation in the emergency department (The ED-SED Pilot Trial). BMJ open 2020;10(12):e041987.
- Tanaka LM, Azevedo LC, Park M, Schettino G, Nassar AP, Réa-Neto A, et al. Early sedation and clinical outcomes of mechanically ventilated patients: a prospective multicenter cohort study. Crit Care 2014;18(4):1-0.
- Shehabi Y, Chan L, Kadiman S, Alias A, Ismail WN, Tan MA, et al. Sedation depth and long-term mortality in mechanically ventilated critically ill adults: a prospective longitudinal multicentre cohort study. Intensive Care Med 2013;39(5):910- 8.
- Mehta S, Meade M, Burry L, Mallick R, Katsios C, Fergusson D, et al. Variation in diurnal sedation in mechanically ventilated patients who are managed with a sedation protocol alone or a sedation protocol and daily interruption. Crit Care 2016;20(1):1-7.
- Xie Y, Cao L, Qian Y, Zheng H, Liu K, Li X. Effect of Deep Sedation on Mechanical Power in Moderate to Severe Acute Respiratory Distress Syndrome: A Prospective Self-Control Study. BioMed Res Int 2020;2020.
- Hughes CG, Girard TD, Pandharipande PP. Daily sedation interruption versus targeted light sedation strategies in ICU patients. Crit Care Med 2013;41(9):S39-45.
- Rose L, Fitzgerald E, Cook D, Kim S, Steinberg M, Devlin JW, et al. Clinician perspectives on protocols designed to minimize sedation. J Crit Care 2015;30(2):348-52.
- Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013;41(1):263-306.
- Baron R, Binder A, Biniek R, Braune S, Buerkle H, Dall P, et al. Evidence and consensus based guideline for the management of delirium, analgesia and sedation in intensive care medicine. Revision 2015 (DAS-Guideline 2015)?short version. Ger Med Sci 2015;13.
- Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 2009;373(9678):1874-82.
- Fuller BM, Mohr NM, Roberts BW, Carpenter CR, Kollef MH, Avidan MS. Protocol for a multicentre, prospective cohort study of practice patterns and clinical outcomes associated with emergency department sedation for mechanically ventilated patients: the ED-SED study. BMJ open 2018;8(10):e023423.
- Jackson DL, Proudfoot CW, Cann KF, Walsh TS. The incidence of sub-optimal sedation in the ICU: a systematic review. Crit Care 2009;13(6):R204.
- Borkowska M, Labeau S, Schepens T, Vandijck D, Van de Vyver K, Christiaens D, et al. Nurses? sedation practices during weaning of adults from mechanical ventilation in an intensive care unit. Am J Crit Care 2018;27(1):32-42.
- Sneyers B, Laterre PF, Perreault MM, Wouters D, Spinewine A. Current practices and barriers impairing physicians? and nurses? adherence to analgo-sedation recommendations in the intensive care unit-a national survey. Crit Care 2014;18(6):1-2.
- Xie W, Zhong Z, Li G, Hou G, Huang K, Yu Z. A comparative study on clinical effects of dexmedetomidine and midazolam on patients with severe coronavirus disease 2019 on non-invasive ventilation. Zhonghua wei zhong bing ji jiu yi xue 2020;32(6):677- 80.
- Wang CY, Shang M, Feng LZ, Zhou CL, Zhou QS, Hu K. Correlation between APACHE III score and sleep quality in ICU patients. J Int Med Res 2019;47(8):3670-80.
- Yang XH, Hu B, Shang Y, Liu J, Zhong M, Shang XL, et al. Expert consensus on management of analgesia and sedation for patients with severe coronavirus disease 2019. Chin Med J 2020;133(18):2186-8.
 Intervention group;
Intervention group; Control group
Control group