- *Corresponding Author:
- J. Dong
Internal medicine, Department of East Medical District, Linyi People’s Hospital, 233 Fenghuang Street, Hedong District, Linyi City, 276000, China
E-mail: dongjiedj_1984@126.com
| This article was originally published in Special issue on “Trends in therapeutic Management of Various Conditions” |
| J Pharm Sci 2020:82(3) spl issue 6;101-105 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
In order to explore the harm caused by Escherichia coli infection to puerperium, and to propose effective and feasible treatment plan, 68 women who are born in hospital and have Escherichia coli infection during puerperium are selected as research objects. According to different treatment methods, they are divided into observation group and experimental group, with 34 cases in each group. The observation group is treated with levofloxacin hydrochloride. The experimental group is treated with cefazolin and levofloxacin hydrochloride. The time of disappearance, adverse reactions and clinical efficacy are compared between the two groups. Studies have found that women infected with Escherichia coli during puerperal period can cause uterine tenderness, anal pain, abnormal lochia, breast tenderness, etc., and timely anti-infective treatment is needed. The total effective rate of maternal treatment in the experimental group is 94.1%, and the total effective rate of maternal treatment in the observation group is 70.6%. The difference between the two groups is statistically significant (P < 0.05). The disappearance time of lower abdominal pain, anal pain and abnormal lochia in the experimental group is shorter than that in the observation group, and the difference is statistically significant (P < 0.05). The incidence of adverse reactions in the experimental group is 8.8%, which is significantly lower than that in the control group (35.3%). The difference is statistically significant (P < 0.05). The effect of cefazolin combined with levofloxacin hydrochloride on the maternal treatment of Escherichia coli in the puerperium period is significant. The clinical symptoms of the patients are obviously improved, and the adverse reactions are less, which is worthy of clinical application.
Keywords
Escherichia coli, puerperium, infection, cefazolin, levofloxacin oxyacid
The 6-8 weeks postpartum period is called the puerperium period. During this period, the whole-body condition of the mother is restored, and the organs are gradually functioning normally. Therefore, it is especially important for the nursing and rehabilitation of maternal puerperium. Otherwise, it will increase the risk of infection and related adverse reactions and pose a serious threat to the quality of life and even life safety of women[1-3]. According to statistics, the probability of infection in the puerperium is about 1.3% to 7%. After childbirth, due to the decline of estrogen and progesterone levels, low estrogenemia occurs, and the milk begins to secrete. The secretion of maternal milk is greatly affected by infant sucking and breast stimulation[4]. Puerperal infection means that during the period of before maternal production, the production process, and the recovery of the body after production, because of factors such as decreased autoimmunity or trauma during childbirth, maternal reproductive tract is vulnerable to pathogens, which may cause local or systemic inflammatory reactions. In severe cases, it may cause sepsis, toxic shock, and even threaten the lives of women[5]. Therefore, prevention of puerperal infection has become a problem that obstetricians pay more attention to now. After investigation and statistics, the strains of maternal puerperal infection are mainly Escherichia coli, Staphylococcus aureus, Enterococcus faecalis and Staphylococcus epidermidis. It is necessary to select targeted antibacterial drugs according to the results of drug-sensitive culture. The Escherichia coli strain referred to in this study is commonly known as Escherichia coli, and is the most important pathogen of infection in puerperal women, accounting for 30% to 40% of all pathogenic bacteria. Escherichia coli is a normal habitat in the gut of humans and animals, and is also an indispensable group of bacteria that maintains the homeostasis of the body[6]. After childbirth, due to the decline of body resistance and immunity, the normal flora is dysfunctional, the vaginal defense ability and self-purification ability are reduced, and the possibility of bacterial infection is significantly increased[7-8]. In summary, although there are studies on the treatment options for Escherichia coli infection, there are few analyses of the hazards and related risk factors caused by Escherichia coli infection in women during puerperium, and there is a lack of more targeted and effective treatment options[9]. Therefore, the symptoms, signs and adverse reactions of women with Escherichia coli during puerperium are closely observed, and relevant treatment is given to analyze the therapeutic effect of drugs on the maternal infection of Escherichia coli and its effect on maternal prognosis. A reliable reference is provided for future clinical treatment. The specific results are reported below. Sixty-eight women with fetuses with Escherichia coli infection who are born in our hospital from January 2014 to July 2018 are randomly selected as the observation group and the experimental group, with 34 cases in each group. In the observation group, the age ranges from 21 to 36 years old, with an average age of (27.40±3.53) years old. The pre-prenatal weight is 54.25-72.10kg, the average body weight is (62.30±9.52) kg, the course of disease is 3-7 d, and the average disease duration is (6.23±2.32) d. In the experimental group, the age ranges from 21 to 35 years old, with an average age of (28.02±3.47) years old. The pre-partum weight is 53.55-71.30kg, the average body weight is (61.85±9.32) kg, the course of disease is 3-7 d, and the average disease duration is (6.15±2.28) d. The general data of the two groups are compared, and the difference is not statistically significant (P>0.05), which is comparable. The informed consent signed by the patients or their family members was obtained and this study was approved by the medical ethics committee of Linyi Women’s and Children’s Hospital. Inclusion criteria: Full-term primipara has one fetus, gestational week is 38-40 weeks are selected, the pathogen of infection is a pathogen of Escherichia coli, there is no other adverse reactions of pregnancy and childbirth, there is no heart, brain, kidney and other organ dysfunction, and neonatal indicators are not abnormal and in good health. Exclusion criteria: Primiparas with two or more pathogenic bacteria infection, with mental disorders or unable to cooperate with treatment, with underlying diseases, and with congenital diseases of newborns are excluded.
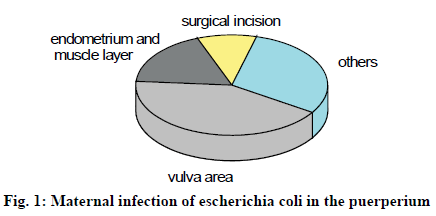
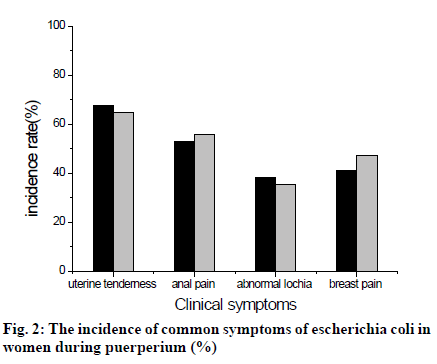
The vital signs, symptoms and adverse reactions of all parturients are closely observed. All parturients are placed in a semi-recumbent position to prevent retrograde inflammation and infection. At the same time, adequate nutritional support is provided through intravenous access to correct anemia and electrolyte disturbance and enhance immunity. If vulvovaginal infection occurs, debridement and drainage should be performed immediately. If the puerpera has abdominal incision infection, the incision drainage should be carried out immediately. If the puerpera has pelvic abscess, the remnants of uterine cavity should be removed and drained through posterior fornix incision. If the puerpera’ s suppurative thrombosis continues to spread, the ligation of ovarian vein, internal iliac vein, etc., or the incision of diseased vein can be considered for direct thrombectomy. Levofloxacin hydrochloride (manufacturer: Jiangsu Ruinian Advance Pharmaceutical Co., Ltd.; production batch number: national medicine quasi-word H20060994; specification: 0.2g) is intravenously injected into the women in observation group, with 200mg per time and twice a d. On the basis of the anti-infective treatment of levofloxacin hydrochloride in the observation group, cefazolin (manufacturer: Shenzhen Huarun Jiu Xin Pharmaceutical Co., Ltd.; production batch number: national medicine quasi-word H20060601; specification: 1.5g) is intramuscularly injected into the study group, once 0.5g, 2 times a d. Both groups of women were treated for 3 d according to the above protocol. Firstly, the clinical outcomes of the two groups of women are compared. Evaluation criteria: markedly, the Escherichia coli pathogen test results are negative, the symptoms disappear, and the vital signs return to normal; the effective Escherichia coli pathogen test results are negative, the symptoms improve and the vital signs improve. Invalidation is positive for Escherichia coli pathogen test and symptoms are not improved. Secondly, the time to disappear from infection symptoms is compared between the two groups, including uterine tenderness, abnormal lochia, anal pain and breast tenderness. Thirdly, the incidence of maternal adverse reactions is compared between the two groups, including urticaria, abnormal liver function, nausea and vomiting, and diarrhea. In this study, SPSS20.0 statistical software is used to analyze the data. The count data is expressed in n/%. The χ2 is used to test. The measurement data is expressed as x±s. t is used to test. P<0.05 is considered statistically significant. In this study, it is found that Escherichia coli is the most common pathogen of infection in women during puerperium. The most common part involved is the genital area, accounting for 42.0% of the total, followed by infection of the endometrium and myometrium, which accounts for 18.0% of the total. It can also be seen in surgical wound infections (10.0%) and infections in other areas (30.0%). As can be seen from fig. 1, in women with puerperal infection, cervicitis, acute vulvitis and vulvovaginitis are more common. If the urinary system, respiratory system or digestive system is involved, the corresponding inflammation manifests. In recent years, anti-infective treatment during maternal puerperium has become a key issue of clinical concern. All women infected with Escherichia coli will have different degrees of uterine tenderness, anal pain, abnormal lochia, breast tenderness and other symptoms, of which the highest probability of uterine tenderness, followed by anal pain. There is no significant difference in the maternal symptoms between the two groups (P>0.05), as shown in fig. 2. At present, the clinician will give corresponding antibiotic treatment according to the specific infection situation of the mother, and the application of the single antibacterial drug will produce certain resistance to the more serious pregnant women, which may delay the disease and lead to further deterioration of the disease. Levofloxacin hydrochloride is a widely used broad-spectrum antibacterial drug in clinical practice. It belongs to the third-generation fluoroquinolone drug. It has a long half-life and strong antibacterial effect. It can effectively inhibit the activity of bacterial DNA helicase, which can be used against mycoplasma and chlamydia. It has a powerful killing effect and has been widely used in anti-infective treatment[10]. Cefazolin belongs to the first generation of cephalosporins and can kill various bacteria such as Escherichia coli, Streptococcus pneumoniae and Enterobacter aerogenes. It is often used to treat respiratory and urinary diseases caused by sensitive bacteria. At the same time, there is also a significant therapeutic effect on endocarditis. Cefazolin has a strong promoting effect on the binding of penicillin and protein in the cell membrane. The drug absorption is fast, which can effectively inhibit the growth and reproduction of bacteria. At the same time, the bacteria can be dissolved and killed, and the anti-infection effect is very remarkable[11-13]. However, due to the continuous updating of clinical drugs, the use of certain antibacterial drugs is easy to produce endogenous drugs, and the therapeutic effect is not satisfactory. Based on this, this study combines the two drugs into the maternal infection of Escherichia coli in the puerperal period. It is found that the combined treatment effect is obvious, and the synergy of drugs is enhanced [14-16].
After treatment in the observation group, 10 cases are markedly effective and 14 cases are effective. The total effective rate is 70.6%. After the maternal treatment in the experimental group, 12 cases are markedly effective and 20 cases are effective. The total effective rate is 94.1%. The total effective rate of the two groups is statistically significant (P<0.05), as shown in Table 1. After treatment, lower abdominal pain, anal pain, lochia abnormality and breast swelling pain in both groups are significantly improved compared with those before treatment, and the disappearance time of symptoms in the experimental group is significantly shorter than that in the control group. The difference between the two groups is statistically significant (P < 0.05), as shown in Table 2. In the observation group, 3 parturients have urticaria symptoms, 2 parturients have abnormal liver function, 4 parturients have nausea and vomiting symptoms, and 3 parturients have diarrhea symptoms. The total incidence of adverse reactions is 35.3%. In the experimental group, 2 parturients have urticaria and 1 parturient has abnormal liver function. The incidence of adverse reactions is 8.8%. The incidence of adverse reactions in the study group is significantly lower than that in the control group (x2 = 22.1452, P < 0.05). With the progress of medical treatment level and the increasing attention to health, although the management of maternal perinatal period is constantly strengthened, the infection rate in puerperium has been significantly reduced, and the incidence of adverse reactions is also decreasing year by year. However, in some local hospitals where medical technology is not well developed, the incidence of infection among puerperal women still exists, and when the situation is serious, it will also pose a great threat to the safety of maternal life. This also suggests that medical staff should strengthen the nursing of the vulnerable parts of puerperal women, strictly sterile operation, prevent infection, strictly grasp the indications of perineal lateral incision during the delivery and perineal lateral incision, and pay attention to the cleaning and disinfection of perineum, so as to reduce the risk of puerperal infection. sDuring the puerperium period, if the mother is infected with Escherichia coli, it will cause symptoms such as uterine tenderness, anal pain, abnormal lochia, and breast tenderness. The hospital should do preventive and management work in a targeted manner. If Escherichia coli infection occurs during maternal puerperium, anti-infective treatment is needed. The treatment with levofloxacin hydrochloride and cefuroxime hydrochloride can effectively improve the clinical symptoms of the mother and improve the therapeutic effect, and the adverse reactions caused by the combination are less, which is worthy of clinical application. Although antibiotics are still in the stage of continuous replacement, this study has confirmed the curative effect of levofloxacin hydrochloride combined with cefuroxime in the treatment of Escherichia coli. However, there is still the possibility of drug resistance in women with severe symptoms. Based on this, the application of antibiotics is the focus of future clinical needs.
| Group | Markedly effective | Effective | Invalid | Total effective rate |
|---|---|---|---|---|
| Observation group | 10/29.4 | 14/42.2 | 10/29.4 | 70.6 |
| Experimental group | 12/35.3 | 20/58.8 | 2/5.88 | 94.1 |
| χ2 | - | - | - | 7.421 |
| P | - | - | - | <0.05 |
Table 1: Comparison of Clinical Efficacy Between the Two Groups (N = 34, %)
| Group | Lower abdominal pain | Anal pain | Lochia abnormality | Breast swelling pain |
|---|---|---|---|---|
| Observation group | 7.43±0.28 | 7.90±0.65 | 9.12±1.34 | 8.35±0.78 |
| Experimental group | 3.12±0.25 | 3.95±0.48 | 5.02±1.18 | 4.27±0.58 |
| t | 27.6354 | 26.4273 | 27.1543 | 26.9350 |
| p | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
Table 2: Comparisons of the Disappearance Time of Clinical Symptoms Between the Two Groups (X ± S, D)
References
- Kobayashi N, Ahmed S, Sumi A. Collaborative Research on Puerperal Infections in Bangladesh. Nihonseigaku Zasshi 2017; 72(2) : 106-111.
- Dubuc J. Short communication: Diagnostic performance of on-farm bacteriological culture systems for identification of uterine Escherichia coli in postpartum dairy cows. Journal of Dairy Science, 2017; 100(4): 3079-82.
- Ellis S, Tyrrel S, O'Leary E. Proportion of sewage sludge to soil influences the survival of Salmonella Dublin and Escherichia coli. Clean Soil Air Water 2018; 46(4): pp. 1800042.
- Kulkarni SR, Peerapur BV, Sailesh KS. Isolation and Antibiotic Susceptibility Pattern of Escherichia coli from Urinary Tract Infections in a Tertiary Care Hospital of North Eastern Karnataka. J Nat Sci Biol Med 2017; 8(2):176-180.
- Tirumalai MR, Karouia F, Tran Q. The adaptation of Escherichia coli cells grown in simulated microgravity for an extended period is both phenotypic and genomic. Npj Microgravity 2017; 3(15): 15.
- Abdi-Hachesoo B, Asasi K, Sharifiyazdi H. Farm-level evaluation of enrofloxacin resistance in Escherichia coli isolated from broiler chickens during a rearing period. Comparative Clini Pathol 2017; 26(2): 471-6.
- Helldal L, Karami N, Welinderolsson C. Evaluation of MLVA for epidemiological typing and outbreak detection of ESBL-producing Escherichia coli in Sweden. Bmc Microbiology 2017; 17(1): 8.
- Bellizzi S, Bassat Q, Ali MM. Effect of Puerperal Infections on Early Neonatal Mortality: A Secondary Analysis of Six Demographic and Health Surveys. Plos One 2017; 12(1): e0170856.
- Kaiser JE, Bakian AV, Silver RM. Clinical Variables Associated With Adverse Maternal Outcomes in Puerperal Group A Streptococci Infection. Obstet Gynecol 2018; 132(1): 1.
- Mbchb RG, Fracr LAM, Fracr CBM. Sonographic findings in acute puerperal endometritis: The hypoechoic rim sign and endomyometrial junction indistinctness. J Ultrasound Med 2017; 20(3): 123-8.
- Mashwal FA, Safi SHE, George SK. Incidence and molecular characterization of the extended spectrum beta lactamase-producing Escherichia coli isolated from urinary tract infections in Eastern Saudi Arabia. Saudi Med J 2017; 38(8): 811-15.
- Jin YK, Olinares PDB, Chen J. Structural basis of transcription arrest by coliphage HK022 Nun in an Escherichia coli RNA polymerase elongation complex. Elife 2017; 6.
- Kim SY, Lee Y, Seo SJ. Effects of Escherichia Coli-derived Recombinant Human Bone Morphogenetic Protein-2 Loaded Porous Hydroxyaptite-based Ceramics on Calvarial Defect in Rabbits. J Bone Metabol 2017; 24(1): 23-30.
- Rehman MU, Hui Z, Iqbal MK. Antibiotic resistance, serogroups, virulence genes, and phylogenetic groups ofEscherichia coliisolated from yaks with diarrhea in Qinghai Plateau, China. Gut Pathogens 2017; 9(1): 24.
- Tolen TN, Ruengvisesh S, Taylor TM. Application of Surfactant Micelle-Entrapped Eugenol for Prevention of Growth of the Shiga Toxin-Producing Escherichia coli in Ground Beef. Foods 2017; 6(8): 69.
- Shofty B, Gonen L, Avraham S. Postoperative cerebrospinal fluid rhinorrhea in puerperal women following transcranial resection of tuberculum sella meningiomas. J Neurosurg Sci 2017.