- *Corresponding Author:
- V. Nallasamy
Department of Pharmacy Practice, J. K. K. Nattraja College of Pharmacy, Kumarapalayam, Tamil Nadu 638183, India
E-mail: nvmurthi@gmail.com
| Date of Received | 17 April 2021 |
| Date of Revision | 19 May 2023 |
| Date of Acceptance | 22 July 2023 |
| Indian J Pharm Sci 2023;85(4):1137-1143 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
The objective of this work was to assess the pharmacist provided telephonic patient educational interventions, designed to improve the management of lipid levels and reduce the non-compliance of lipid-lowering medications. This work was a prospective study. The participants were 60 adults (intervention group with 30 and control group with 30) with cardiovascular disease prescribed lipid-lowering drugs to manage dyslipidemia. Patients in the intervention group were advised regarding lipid management and compliance with therapy by a pharmacist through regular face-to-face counseling and telephonic counseling. Control group patients were received standard medical care. The primary outcome measure was the percentage of patients who achieved a goal low-density lipoprotein below 100 mg/dl±5 % and improvement in adherence to the prescribed medications after 2 mo. In the intervention group, a significant difference was observed in the low-density lipoprotein levels and improvement in adherence after 2 mo of pharmacist intervention. The study demonstrated that pharmacists’ individualized telephonic counseling had positive impacts on the management of lipid levels, including improved medication compliance.
Keywords
Counseling, pharmacists, hyperlipidemia, cardiovascular disease, nonadherence
Cholesterol is a vital lipid molecule in our body, but too much cholesterol in our body can cause many problems. Cholesterol disorders are clinically significant due to an increase in the risk of cardiovascular diseases and stroke. Hypercholesterolemia causes 2.6 million deaths (4.5 % of the total) per year. The control of Total Cholesterol (TC) is one of the key public health campaigns worldwide. According to the World Health Organization report, reducing 10 % of serum cholesterol in men aged 40 has been reported to reduce 50 % of cardiovascular diseases within 5 y. A similar serum cholesterol level decrease in men aged 70 y can result in an average 20 % decrease in cardiovascular disease rate in the next 5 y[1].
The pharmacologic treatment of hyperlipidemia is generally used to prevent heart diseases. Recent developments in the treatment of dyslipidemia are mostly based on different clinical trials. Currently, many safe and effective drugs are available for the treatment of hyperlipidemia. Several studies have reported that Low-Density Lipoprotein (LDL) values are above the recommended target levels in most patients[2]. This is an important issue. There are several reasons for poor control of cholesterol levels. Among the many factors, poor adherence to the prescribed medication is one of the key reasons for poor control of cholesterol levels[3].
A study conducted exposed that 47.5 % of newly- treated patients are not followed the initial statin therapy[4]. Similarly, a meta-analysis reported that 60 % of patients discontinue their statins within 6 mo of treatment commencement[5]. A cohort study recently noted that the discontinuation rates in the primary care settings were higher than those in clinical trials, signifying that non-compliance is one of the key issues in controlling cholesterol levels[6].
Efforts to reduce non-compliance are necessary, especially in lipid-lowering therapy. Studies have been published on the impact of counselling provided by pharmacists in the management of cholesterol levels[7,8]. Pharmacists have a crucial role in reducing nonadherence in patients by providing advice on medications. But the effective management of this system requires long-term face-to-face counseling, which may not be feasible for large numbers of patients or those living in remote areas. An alternate approach to improve compliance and treatment outcomes is telephone follow-up in addition to regular face-to-face counseling. A similar study was conducted by Ma et al.[9]. In their study, pharmacists delivered an intervention on lipid-lowering medication adherence were studied among 689 patients with coronary heart disease in a developed country. The aim of our study has been designed to assess the impact of personalized telephone follow- up on the management of LDL and non-compliance among cardiovascular disease patients receiving lipid-lowering drug therapy. This study was expected to understand pharmacists' impact on providing telephonic intervention in a developing country like India.
Materials and Methods
The study was conducted after the institution ethics committee approval (JKKNCP/PP/Ethics/4525818). In this study, Cardiovascular Disease (CVD) patients were defined according to World health organization criteria[10]. Patients were recruited from the outpatient department of tertiary care hospital, Erode, Tamilnadu, India. Patients included in the study if he/she was aged between 30 and 85 y with cardiovascular disease, taking at least aspirin or other therapies (ticlopidine, clopidogrel, and warfarin, etc.) and patients received refill lipid-lowering drugs (niacin, β-Hydroxy β-methylglutaryl-CoA reductase inhibitors, fibrates, or bile acid sequestrants, etc.) past 6 mo period. Patients having baseline fasting LDL above 130 mg/dl were included in the study. Patients who were able to understand and speak Tamil and had a telephone/mobile phone in their homes were selected for the study. Written informed consent was obtained from each study participant. The key endpoints of the study were the percentage of patients at goal LDL below 100 mg/dl±5 % (excluding patients with Triglyceride (TG)>400 mg/ dl), (A goal LDL below 105 mg/dl was selected based on±5 % laboratory assay margin of error).
Intervention:
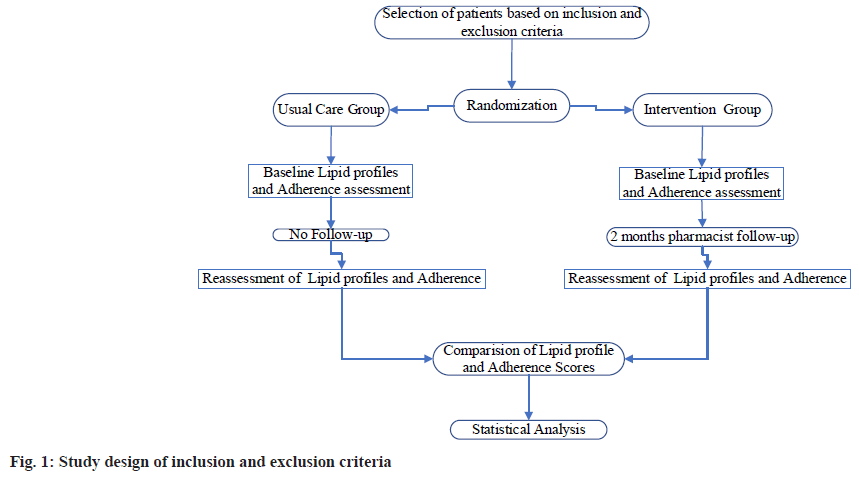
A total of 60 patients were selected for the study based on inclusion and exclusion criteria. Patients were randomized to the intervention group and control group (usual care) based on the inclusion criteria and informed consent. A randomization schedule was used with the help of a computer to create a list of random numbers. Patients randomized in the intervention group were followed by the pharmacist after physician consultation, as described below. Control group (usual care) patients were informed of their lipid levels and also informed to contact the physician for further follow-up (fig. 1).
Outcomes:
Lipid profiles were recorded at baseline and end of the study period (2 mo). Patients enrolled in the intervention group were provided face-to-face counseling after physician consultation. Each patient was extensively counseled/explained on the proper use of the drugs after the regular physician consultation. In addition to that, every week, the pharmacist regularly telephoned intervention group patients for 2 mo. During telephonic communication, more importance was placed on drug therapy's necessity in reducing the risk of cardiovascular events. Patients were questioned about possible side effects, general well-being, and specific reasons for nonadherence if necessary. The counseling includes providing information about the use of drugs, dose, and frequency of prescribed drugs. Dietary advice was also briefly provided. By using the data collection questionnaire, information regarding patient demographics, sex, age, education, medical history, and co-morbidities was collected. Adherence assessment was obtained through the 8-item self- report Morisky Medication Adherence Scale (MMAS)[11]. Based on the score of MMAS, adherence was valued as follows; high adherence (=8), medium adherence (6 to 8), and low adherence (<6). Patients who had a low or moderate rate of adherence were considered nonadherent.
Statistical analysis:
Data were analyzed in Statistical Package for the Social Sciences/16 using Fisher’s exact test and paired t-test. The threshold for statistical significance was set at p< 0.05.
Results and Discussion
Hyperlipidemia increases the risk of cardiovascular diseases, and control is essential for preventing cardiovascular complications. Nonadherence to the prescribed medication is one of the key factors of treatment failure[12]. In this study, an attempt has been made to improve compliance and treatment outcomes by telephonic follow-up in addition to regular face-to-face counseling. A total of 60 patients were included in this study based on inclusion and exclusion criteria. 30 patients were enrolled in each group of the study, and none of the patients were lost to follow-up in the study period. Baseline parameters were similar in both groups. No statistically significant differences were found (Table 1).
| Gender | Intervention (n=30) | Usual Care (n=30) | p value |
|---|---|---|---|
| Gender wise distribution of patients (n=60) | |||
| Male (41) | 22 (73.3 %) | 19 (63.3 %) | 0.58 |
| Female (19) | 08 (26.7 %) | 11 (36.7 %) | |
| Age wise distribution of patients (n=60) | |||
| <50 y old | 02 (6.7 %) | 04(13.3 %) | 0.67 |
| ≥50 y old | 28 (9.3 %) | 26 (86.7 %) | |
| Risk factor distribution in the participants (n=60) | |||
| 0 risk factors | 2(6.7 %) | 2(6.7 %) | 0.28 |
| 1 risk factor | 6(20 %) | 5(16.7 %) | 0.39 |
| 2+ risk factors | 22(73.3 %) | 23(76.7 %) | 0.34 |
Table 1: Baseline Patient Demographics
Both gender, and sex differences have been reported in the diagnosis, pathophysiology, and treatment of dyslipidemia[13,14]. Lipid profiles are similar in both genders until childhood, but after puberty, lipid levels physiologically vary. LDL levels commonly increase from young adulthood to 60 y of age in men and 70 y in women. After that LDL levels generally decrease[15]. In our study, a high prevalence rate of dyslipidemia in the male population was observed. This difference in prevalence may be due to female sex hormones, mainly estrogen, which offers a protective effect against the increase of lipid or TG levels, such a protective role of estrogen has been previously reported[16]. The higher prevalence rate in males may be because of metabolic changes, sedentary lifestyles, and work pressure coupled with a lack of physical inactivity[17].
In this study, the distribution of risk factors that contributed to elevated lipid levels in both groups was found to be hypertension, diabetes, HDL<40 mg/ dl, and smoking (Table 2). No statistically significant differences were found in the risk factors.
| Risk factors | Intervention (n=30) | Usual Care (n=30) | p-value |
|---|---|---|---|
| Hypertension | 26 (29.2 %) | 28(26.2 %) | 0.35 |
| Diabetes | 21(23.6 %) | 25(23.4 %) | 0.41 |
| HDL<40 mg/dl | 16(18.0 %) | 19(17.8 %) | 0.37 |
| Smoking | 08 (9.0 %) | 13(12.1 %) | 0.39 |
Note: p value stands for calculated probability of findings observed; *p<0.05 significant
Table 2: Distribution of Risk Factors Contributed to Increased Lipid Level
Lipid profiles were recorded at baseline, at the end of the study period (2 mo). In 2 mo, the study period, every week pharmacist regularly telephoned to intervention group patients and provided information as specified previously. In the pharmacist intervention group, the baseline TC value was 240±36.5 mg/dl. After 2 mo of pharmacist intervention, it was reduced to 180±32.5 mg/dl, and the average change was about -60±36.2 mg/dl. Similarly, in the pharmacist intervention group, the baseline LDL was 159±31.8 mg/dl. It was reduced to 89±27.6 mg/dl after 2 mo of pharmacist intervention, and the average change is about -70±31 mg/dl. TC and LDL reduction were found to be statistically significant (p<0.05).
In the pharmacist intervention group, the baseline TG value was 172±94.2 mg/dl. After 2 mo of pharmacist intervention, it was reduced to 171±83.9 mg/dl, and the average change was about -1±103.4 mg/dl. Similarly, in the pharmacist intervention group, the baseline HDL was 42±07.8 mg/dl. After 2 mo of pharmacist intervention, it was changed to 43±6.10 mg/dl, and the average change is about +1±06.80 mg/dl. TG and HDL reduction was found to be statistically nonsignificant (p>0.05) (Table 3).
| Lipid Level (mg/dl) | Baseline (mg/dl) | Final (mg/dl) | Average change | p-value (Within group) |
|---|---|---|---|---|
| Distribution of lipid levels among usual care group | ||||
| TC | 227±32.7 | 202±34.6 | -25±39.8 | 0.028 |
| TG | 156±65.8 | 144±61.9 | -12±60.2 | 0.073 |
| LDL | 149±35.4 | 114±27.9 | -35±28.3 | 0.019 |
| HDL | 44±12.9 | 47±11.7 | +3±9.1 | 0.214 |
| Distribution of lipid levels among intervention group | ||||
| TC | 240±36.5 | 180±32.5 | -60±36.2 | 0.031 |
| TG | 172±94.2 | 171±83.9 | -1±103.4 | 0.117 |
| LDL | 159±31.8 | 89±27.6 | -70±31.4 | 0.038 |
| HDL | 42±07.8 | 43±6.10 | +1±06.80 | 0.396 |
Note: TC=Total Cholesterol; TG=Triglycerides; LDL=Low-Density Lipoprotein; HDL=High-Density Lipoprotein; p value stands for calculated probability of findings observed; *p<0.05 significant
Table 3: Distribution of Lipid Levels
In the usual care group, the baseline TC value was 227±32.7 mg/dl. After 2 mo, it was reduced to 202±34.6 mg/dl, and the average change was about 25±39.8. Similarly, in the usual care group, the baseline LDL was 149±35.4 mg/dl. After 2 mo, it was reduced into 114±27.9 mg/dl, the average change is about -35±28.3. TC and LDL reduction were found to be statistically significant (p<0.05).
In the usual care group, the baseline TG value was 156±65.8 mg/dl. After 2 mo, it was reduced to 144±61.9 mg/dl, and the average change was about -12±60.2 mg/dl. Similarly, in the usual care group, the baseline HDL was 44±12.9 mg/dl. It was changed to 47±11.7 mg/dl after 2 mo, and the average change is about +3±9.1 mg/dl. TG and HDL reduction was found to be statistically nonsignificant (p>0.05). In the intervention group, the number of patients who had baseline LDL<105 mg/dl was nil. After 2 mo of pharmacist intervention, the number of patients who had LDL<105 mg/dl was 14. The number of patients who had baseline LDL between 105-130 mg/dl was 6. After 2 mo of pharmacist intervention, the number of patients who had LDL between 105-130 mg/dl was 9. Similarly, the number of patients who had baseline LDL between 131-160 mg/dl was 13. After 2 mo of pharmacist intervention, the number of patients had LDL between 131-160 mg/dl was 6. The number of patients who had baseline LDL>160 mg/dl was 11. After 2 mo of pharmacist intervention, the number of patients who had LDL between 160 mg/dl was 1 (Table 4). This result demonstrated a significant improvement in LDL control through a pharmacist- provided telephonic intervention. The pharmacist intervention resulted in statistically significant increases (p<0.05) in achieving the goal LDL.
| LDL level (mg/dl) | Number of patients (n=30) Baseline | Number of patients (n=30) Final |
|---|---|---|
| Impact of pharmacist counseling on LDL goals | ||
| <105 | 0 (0 %) | 14(46.66 %) |
| 105-130 | 6(20.0 %) | 9(30.0 %) |
| 131-160 | 13(43.33 %) | 6(20.0 %) |
| >160 | 11(36.66 %) | 1(3.33 %) |
| LDL goals of the usual care group | ||
| <105 | 0(0 %) | 9(30.00 %) |
| 105-130 | 8(26.66 %) | 7(23.33 %) |
| 131-160 | 12(40.00 %) | 10(33.33 %) |
| >160 | 10(33.33 %) | 4(13.33 %) |
Table 4: Distribution of Low-Density Lipoprotein Level
Similarly, in the usual care group, the number of patients who had baseline LDL<105 mg/dl was nil. After 2 mo, the number of patients who had LDL<105 mg/dl was 9. The number of patients who had baseline LDL between 105-130 mg/dl was 8. After 2 mo, the number of patients who had LDL between 105-130 mg/dl was 7. Similarly, the number of patients who had baseline LDL between 131-160 mg/dl was 12. After 2 mo, the number of patients who had LDL between 131-160 mg/dl was 10. The number of patients who had baseline LDL>160 mg/dl was 10. After 2 mo, the number of patients who had LDL between 160 mg/dl was 4. This result demonstrated a significant improvement in LDL control without pharmacist intervention (p<0.05). The differences in LDL and TC control between the pharmacist intervention group and the usual care group were statistically significant (p<0.05). Significant reduction in lipid management was observed in the control group also but the percentage of reduction of lipid level was more in the intervention group. Similar results were obtained by a study conducted by Till et al. In their study, out of 88 patients, in the pharmacist group, the average reduction in LDL levels was 30.1 mg/ dl (an average decrease of 18.5 %)[18]. The average LDL decrease in the usual care group was 16.8 mg/ dl, (an average decrease of 6.5 %). The results were statistically significant (p<0.05). And in a similar study conducted by Nola et al. stated that LDL was reduced in the pharmacist intervention group, compared with an increase in the control group[19].
In this study, among 30 patients in the intervention group, 7 (23.3 %) patients had an MMAS score of less than 6, and 23 (76.6 %) patients' scores ranged in the medium or high range between 6-8. But, in the usual group, among 30 participants, 5 (16.6 %) patients had MMAS scores less than 6, and 25 (83.3 %) patients ranged in the medium or high range between 6-8. After 2 mo of telephonic counseling, in the intervention group, one patient was found an MMAS score of less than 6 (MMAS mean score 5.5). But, in the usual group, the baseline of 5 patients was nonadherent (MMAS mean score 7.2), and after 2 mo, seven patients were found to be nonadherent (MMAS mean score 7.6) (Table 5). This study observed a significant improvement in non-adherence in lipid management through a pharmacist-provided telephonic intervention.
| Medication Adherence | Baseline | After 2 mo | p-value |
|---|---|---|---|
| Changes in Medication Adherence MMAS Mean scores of intervention group after 2 mo telephonic counselling (N=30) | |||
| Total number of Patients having MMAS Score<6 | 7 (23.33 %) | 1 (3.33 %) | - |
| MMAS Mean Score (N=30) | 7.2 | 5.5 | 0.028 |
| Changes in Medication Adherence MMAS mean scores of usual care group after 2 mo telephonic counselling (N=30) | |||
| Total number of Patients having MMAS Score<6 | 5 (16.66 %) | 7 (23.33 %) | - |
| MMAS Mean Score (N=30) | 7.2 | 7.6 | 0.117 |
Table 5: Impact of Telephonic Counselling on Medication Adherence
Similarly, Ma et al. conducted a 1 y randomized trial to evaluate the pharmacist delivered an intervention on lipid-lowering medication adherence among 689 patients with coronary heart disease[9]. At the end of the study period, the authors observed that approximately two-thirds of subjects reached their LDL goal, and high adherence rates were also observed for beta-blocker and angiotensin- converting enzyme inhibitor medications. There are some limitations to this study. This study was designed with a small sample size. Despite the small convenience sample, we were able to show an association between pharmacist intervention and lipid management. Further confirmation of these findings, a larger sample may provide insight into the pharmacist’s impact on lipid management. Also, we did not assess if the LDL reduction was due to factors other than the profession of the individual providing care, such as brands of drugs prescribed and patient knowledge of a diet.
Although regular medical care can be effective in increasing compliance with therapy[20,21], they are not easily accessible for people located in remote area and also patients have to come regularly for face-to-face counseling. An alternative is telephone follow-up by a pharmacist, which can help patients to maintain compliance with therapy, and know about laboratory tests and physician appointments. This study exposed the pharmacist’s contribution to improving the effectiveness of cholesterol management in patients with dyslipidemia.
In conclusion, this study confirms that the healthcare team includes pharmacists in lipid management, providing better lipid level reductions. And also, pharmacist-provided information reduces the nonadherence level in patients. The impact of pharmacist intervention in lipid management may reduce long-term cardiovascular complications. The telephonic follow-up model may reduce the cost associated with face-to-face counseling and help implement it in people residing in remote areas. Further studies are required to analyze the cost difference.
Conflict of interests:
The authors declared no conflict of interests.
References
- Global Health Observatory: Raised cholesterol. Geneva: World Health Organization; 2019.
- Reiner Ž, de Backer G, Fras Z, Kotseva K, Tokgözoglu L, Wood D, et al. Euroaspire investigators. Lipid lowering drug therapy in patients with coronary heart disease from 24 European countries--findings from the EUROASPIRE IV survey. Atherosclerosis. 2016;246:243-50.
[Crossref] [Google Scholar] [PubMed]
- Senior V, Marteau TM, Weinman J, Genetic Risk Assessment for FH Trial (GRAFT) Study Group. Self-reported adherence to cholesterol-lowering medication in patients with familial hypercholesterolaemia: The role of illness perceptions. Cardiovasc Drug Ther 2004;18:475-81.
[Crossref] [Google Scholar] [PubMed]
- Corrao G, Conti V, Merlino L, Catapano AL, Mancia G. Results of a retrospective database analysis of adherence to statin therapy and risk of nonfatal ischemic heart disease in daily clinical practice in Italy. Clin Ther 2010;32(2):300-10.
[Crossref] [Google Scholar] [PubMed]
- Liberopoulos EN, Florentin M, Mikhailidis DP, Elisaf MS. Compliance with lipid-lowering therapy and its impact on cardiovascular morbidity and mortality. Expert Opinion Drug Safety 2008;7(6):717-25.
[Crossref] [Google Scholar] [PubMed]
- Andrade SE, Walker AM, Gottlieb LK, Hollenberg NK, Testa MA, Saperia GM, et al. Discontinuation of antihyperlipidemic drugs—do rates reported in clinical trials reflect rates in primary care settings? New Engl J Med 1995;332(17):1125-31.
[Crossref] [Google Scholar] [PubMed]
- Taitel M, Jiang J, Rudkin K, Ewing S, Duncan I. The impact of pharmacist face-to-face counseling to improve medication adherence among patients initiating statin therapy. Patient Prefer Adherence 2012;6:323-9.
[Crossref] [Google Scholar] [PubMed]
- Bluml BM, McKenney JM, Cziraky MJ. Pharmaceutical Care Services And Results In Project Impact: Hyperlipidemia. J Am Pharm Assoc 2000;40(2):157-65.
[Crossref] [Google Scholar] [PubMed]
- Ma Y, Ockene IS, Rosal MC, Merriam PA, Ockene JK, Gandhi PJ. Randomized trial of a pharmacist-delivered intervention for improving lipid-lowering medication adherence among patients with coronary heart disease. Cholesterol 2010;2010:383281.
- WHO. Cardiovascular diseases (CVDs). 2017.
- Morisky DE, Ang A, Krousel‐Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens 2008;10(5):348-54.
[Crossref] [Google Scholar] [PubMed]
- Cheng CW, Woo KS, Chan JC, Tomlinson B, You JH. Assessing adherence to statin therapy using patient report, pill count, and an electronic monitoring device. Am J Health Syst Pharm 2005;62:411-15.
[Crossref] [Google Scholar] [PubMed]
- McNamara JR, Campos H, Ordovas JM, Peterson J, Wilson PW, Schaefer EJ. Effect of gender, age, and lipid status on low density lipoprotein subfraction distribution. Results from the Framingham Offspring Study. Arteriosclerosis 1987;7(5):483-90.
- Krauss RM, Burke DJ. Identification of multiple subclasses of plasma low density lipoproteins in normal humans. J Lipid Res 1982;23(1):97-104.
[Crossref] [Google Scholar] [PubMed]
- Schaefer EJ, Lamon-Fava S, Cohn SD, Schaefer MM, Ordovas JM, Castelli WP, et al. Effects of age, gender, and menopausal status on plasma low density lipoprotein cholesterol and apolipoprotein B levels in the Framingham Offspring Study. J Lipid Res 1994;35(5):779-92.
[Crossref] [Google Scholar] [PubMed]
- Kavanagh K, Davis MA, Zhang L, Wilson MD, Register TC, Adams MR, et al. Estrogen decreases atherosclerosis in part by reducing hepatic acyl-CoA: cholesterol acyltransferase 2 (ACAT2) in monkeys. Arterioscler Thromb Vasc Biol 2009;29(10):1471-7.
[Crossref] [Google Scholar] [PubMed]
- Qi L, Ding X, Tang W, Li Q, Mao D, Wang Y. Prevalence and risk factors associated with dyslipidemia in Chongqing, China. Int J Environ Res Public Health 2015;12(10):13455-65.
[Crossref] [Google Scholar] [PubMed]
- Till TL, Voris JC, Horst JB. Assessment of clinical pharmacist management of lipid-lowering therapy in a primary care setting. J Manage Care Pharm 2003;9(3):269-73.
[Google Scholar] [PubMed]
- Nola KM, Gourley DR, Portner TS, Gourley GK, Solomon DK, Elam M, et al. Clinical and humanistic outcomes of a lipid management program in the community pharmacy setting. J Am Pharm Assoc 2000;40(2):166-73.
[Crossref] [Google Scholar] [PubMed]
- Bramlet DA, Helen King RN BS, Lanette Young MS, Witt JR. Management of hypercholesterolemia: practice patterns for primary care providers and cardiologists. Am J Cardiol 1997;80(8):39H-44H.
[Crossref] [Google Scholar] [PubMed]
- Shaffer J, Wexler LF. Reducing low-density lipoprotein cholesterol levels in an ambulatory care system: Results of a multidisciplinary collaborative practice lipid clinic compared with traditional physician-based care. Arch Intern Med 1995;155(21):2330-5.
[Crossref] [Google Scholar] [PubMed]