- *Corresponding Author:
- B. Guo
Department of Traditional Chinese Medicine, Key Laboratory of Ningxia Minority Medicine Modernization, Yinchuan, Ningxia 750021, China
E-mail: Guo12200055@163.com
| This article was originally published in a special issue, “Drug Discovery and Repositioning Studies in Biopharmaceutical Sciences” |
| Indian J Pharm Sci 2024:86(4) Spl Issue “252-265” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
The objective of this study is to systematically evaluate the clinical efficacy and safety of acupuncture combined with other therapies in the treatment of bronchial asthma, further providing effective evidence-based support for clinical application. Chinese databases such as China National Knowledge Infrastructure, Virus Protein domain Database information resource system, Chinese biomedical literature database and WanFang data including international databases like PubMed, Cochrane library, Web of Science and Excerpta Medica Database were searched comprehensively up to August 2023 for studies related to acupuncture combined with other therapies against bronchial asthma. Literature was screened out, extracted the data using excel spreadsheets, assessed the quality of included studies according to the Cochrane Handbook for Systematic Reviews of Interventions; further, we conducted heterogeneity tests, meta-analysis, sensitivity analysis and hypothesis testing using RevMan 5.4 software for clinical overall effective rate, pulmonary function tests such as forced expiratory volume in the first second, peak expiratory flow, forced expiratory volume in the first second/forced vital capacity, etc. Forest plots were constructed and analyzed; funnel plots were used for publication bias analysis to systematically evaluate the clinical efficacy and safety of acupuncture combined with other therapies in the treatment of bronchial asthma. The clinical efficacy of acupuncture combined with other therapies in the treatment of bronchial asthma is significant, justifying its widespread clinical application. However, the included studies have limitations, with an overall low-quality level and certain risk of bias, affecting the reliability of the meta-analysis. It is expected that in the future, high-quality, large-sample, and multicenter scientifically rigorous studies will be conducted to continuously improve and update systematic evaluations to verify the clinical efficacy of acupuncture combined with other therapies in the treatment of bronchial asthma.
Keywords
Acupuncture, bronchial asthma, beta-agonists, inflammation, Western medicine
Bronchial asthma occurs by chronic airway inflammation, recurrent attacks and protracted course[1-3], which can lead to acute episodes characterized by breathing difficulties, airway spasms and even suffocation, with some cases progressing to heart failure[4,5]. Chronic phase which is persistent is a significant stage, manifesting as varying degrees of symptoms occurring weekly (but less than daily), impacting comfort, immune function and lung health[6]. Despite medical advancements, bronchial asthma remains as a prevalent global health concern, with epidemiological data indicating a notable rise in its incidence over recent decades[7,8]. Management primarily relies on the medication for symptom relief, posing substantial burdens on patients, families and society due to its chronic and exacerbation-prone nature. Statistics suggest that approximately 262 million individuals are affected by asthma worldwide.
In clinical practice, Western medicine primarily addresses asthma treatment through anti-inflammatory measures and symptomatic relief based on specific syndrome patterns, with medications categorized as controllers and relievers[9]. Common medications for bronchial asthma treatment include β (beta)-agonists, glucocorticoids, anticholinergic drugs and theophylline drugs. Despite extensive domestic and international research, asthma remains incurable[10]. Consequently, long-term medication use escalates the economic burden on patients, reduces compliance, leading to associated complications. Hence, even in urban areas, the overall asthma control rate is merely 28.5 %[11].
In bronchial asthma treatment, Traditional Chinese Medicine (TCM) adopts a holistic approach, yielding notable advantages and substantial therapeutic effects[12]. TCM categorizes asthma as wheezing[13], with its pathogenesis involving kidney qi deficiency, airway obstruction and lung function impairment[14]. Treatment with TCM aims to soothe liver, regulate qi, promote blood circulation and eliminate blood stasis[15]. Acupuncture which is a traditional therapy effectively alleviates asthma symptoms with high safety and efficacy[16-19]. It not only addresses acute attacks but also improves the symptoms of lung function during chronic asthma remission[20].
Currently, the number of clinical trials on acupuncture for bronchial asthma in China is rising, along with its related literature. However, these studies often feature outdated literature and limited research methodologies. This study aims to systematically review recent research to enhance the treatment approaches, such as combining acupuncture with moxibustion, herbal plasters and cupping techniques. The objective is to assess the clinical efficacy of acupuncture in treating bronchial asthma. Through qualitative and quantitative analysis via systematic literature and meta-analysis, this study seeks to determine the effectiveness of acupuncture as a primary treatment for bronchial asthma, aiming to improve the clinical outcomes.
Materials and Methods
Data collection:
Computerized search was conducted by utilizing databases such as China National Knowledge Infrastructure (CNKI), VIrus Protein domain DataBase (VIP DB) information resource system, China Biology Medicine (CBM) disc, WanFang data, PubMed, Cochrane Library, Web of Science and Excerpta Medica Database (EMBASE) for randomized controlled trials on TCM acupuncture treatment for bronchial asthma, with language restrictions to Chinese and English, covering the period from the inception of the databases to August 2023; keywords such as acupuncture or acupuncture therapy or acupuncture points or electroacupuncture and (bronchial asthma or asthma) and (randomized controlled trial) were used to search the literature in English.
Inclusion criteria: 1021 individuals of age between (5-81) y and patients having no statistical difference in the base line data such as age, gender, etc., indicating baseline comparability (p>0.05) were included in the study.
Exclusion criteria: Studies involving patients receiving treatment for other diseases concurrently with the intervention measures; literature that has been published repetitively; literature from which valid data cannot be extracted; studies from which the original authors does not yield the data and literature which is neither in Chinese nor in English were excluded from the study.
Treatment method:
The experimental group received combination treatment of acupuncture with TCM and acupuncture combined with Western medicine while the control group received conventional Western medicine treatment or moxibustion interposed with ginger. Both the groups should have balanced baseline data and consistent treatment durations.
The main outcome indicators include overall clinical efficacy rate, lung function which comprises of Forced Expiratory Volume in the 1st second (FEV1), Peak Expiratory Flow (PEF) and FEV1/ Forced Vital Capacity (FVC), etc.
Literature screening and data extraction was independently conducted by three evaluators and was cross-checked; during differing opinions, discussions were held to seek an agreement. If a consensus could not be reached, a 3rd evaluator was consulted for a joint decision. Data extraction for the included literature was based on a predefined data extraction form, which included title, authors, publication date, sample size, patient gender, patient age, intervention measures and duration of treatment, etc.
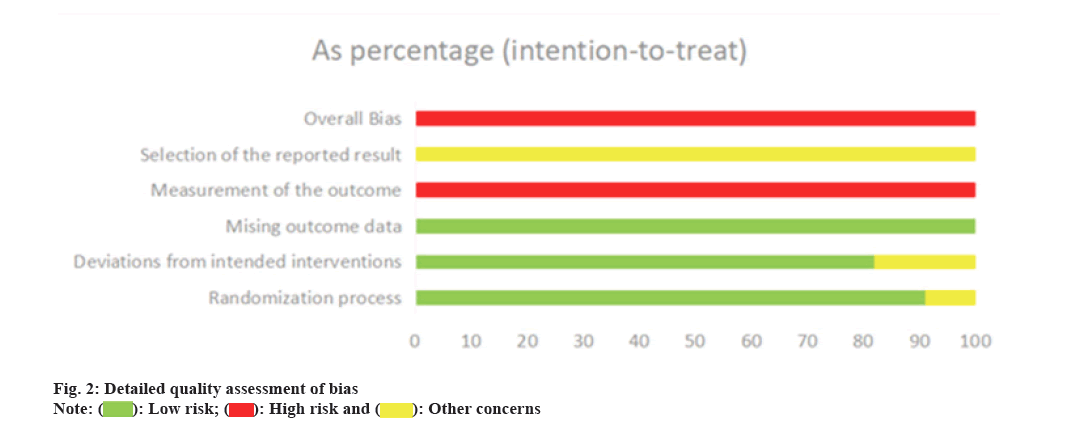
Cochrane Risk of Bias 2 (ROB2) tool was used to assess the quality of the study, covering 5 domains namely; bias arising from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in the measurement of the outcome and bias in selection of the reported result. Each domain's assessment results included high and low risk. A comprehensive evaluation across all domains produced an overall assessment outcome.
Statistical analysis:
Statistical analysis was performed using RevMan 5.4 statistical software. For a given outcome indicator, if at least two studies reported on it, a meta-analysis was conducted. Q-test, in conjunction with heterogeneity Index (I²), was used to assess the heterogeneity among studies. Random-effects model was employed if I²≥50 % (p≤0.01); otherwise, fixed-effects model was used. The outcome of this study was a dichotomous variable where Odds Ratio (OR) was used as an effect indicator. Mean Difference (MD) and 95 % Confidence Interval (CI) were used as effect statistics for the outcome indicators measured by the same scale. If a study had multiple measurement time points, only data from the last time point was included in the analysis. If the required data was not reported in the study, the data was converted based on the information provided in the text. For the data that could not be subjected to meta-analysis, textual description was used for induction and p<0.05 was considered to be statistically significant.
Results and Discussion
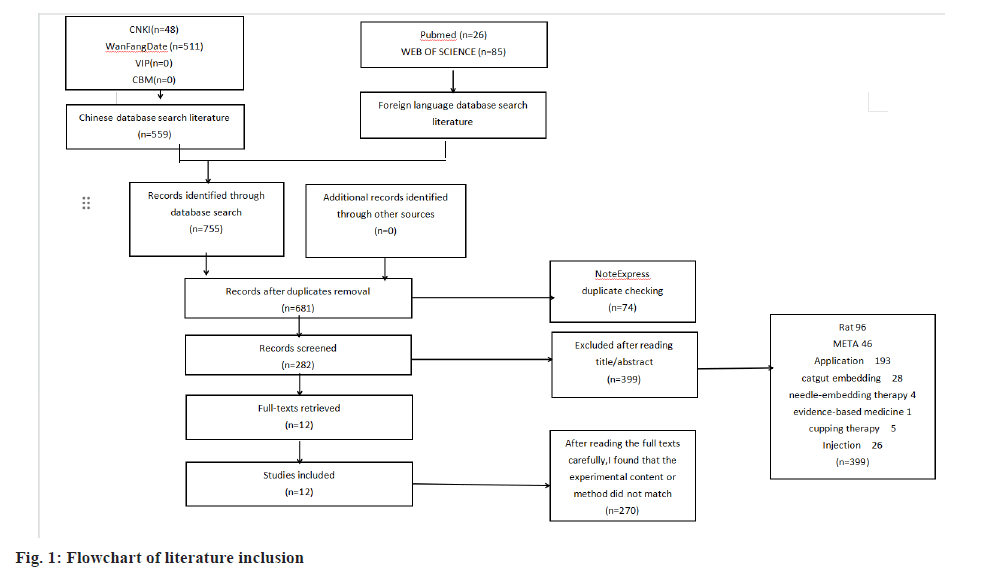
A total of 755 articles were retrieved, among which 559 articles were from Chinese databases and 196 were from English databases. After removing 74 duplicate articles using NoteExpress software; 399 articles were excluded after reading titles and abstracts and 270 articles were excluded after carefully analyzing the full text. Finally, 12 studies meeting the inclusion criteria were identified. The flowchart of literature inclusion is presented in fig. 1. This includes experimental design, researchers, intervention measures and outcome measurement indicators (Table 1). Here, in Table 1, the clinical outcomes correspond to their respective score. The outcomes compared different aspects of the study between the two groups before and after treatment. 1: Clinical efficacy; 2: FVC; 3: PEF; 4: FEV1;5: FEV1/FVC; 6: Interleukin (IL)-6; 7: Tumor Necrosis Factor-Alpha (TNF-α); 8: high sensitivity C-Reactive Protein (hs-CRP); 9: Disappearance time of symptoms; 10: Safety; 11: IgE levels; 12: Eos levels; 13: Generic Quality of Life Inventory (GQOLI)-74 score; 14: Adverse reaction rates; 15: Forced Expiratory Flow (FEF) 25; 16: FEF50; 17: FEF75; 18: Maximal Mid Expiratory Flow (MMEF); 19: Symptom scores; 20: CD3+ levels; 21: CD4+ levels; 22: CD8+ levels; 23: CD19+ levels; 24: CD4+/CD8+ levels; 25: FVC % Pred; 26: PEF % Pred; 27: Pre/post-treatment FEV1/FVC; 28: Pre/post-treatment T Helper type 1 (Th1) levels; 29: Pre/post-treatment Th2 levels; 30: Pre/post-treatment Th17 levels; 31: Pre/post-treatment Regulatory T (Treg) cell levels; 32: Pre/post-treatment Th1/Th2 levels; 33: Pre/post-treatment Th17/Treg levels; 34: Sputum symptom scores; 35: Dyspnea symptom scores; 36: Cough symptom scores; 37: Pre/post-treatment Peak Expiratory Flow Rate (PEFR); 38: Pre/post-treatment PEFR; 39: Pre/post-treatment IL-17; 40: Pre/post-treatment Matrix Metalloproteinase-9 (MMP-9); 41: Pre/post-treatment CRP; 42: Pre/post-treatment TNF-α; 43: Recurrence; 44: Wheezing symptom; 45: Pre/post-treatment Asthma Quality of Life Questionnaire (AQLQ) efficacy scores.
| Type of disease | Sample size | Age | Intervention method | Outcome | |||
|---|---|---|---|---|---|---|---|
| Gender (male/female) | Intervention arm (male/female) | Control arm | Intervention arm | Control arm | Intervention arm | ||
| Chronic persistent phase of bronchial asthma | 50 (34/16) | 50 (46/4) | 18~53 | 18~51 | Oral transfer factor capsules (Western medicine) | Chinese herbal medicine (Tonifying kidney anti-asthma decoction)+acupuncture | 1-10[21] |
| Acute exacerbation of bronchial asthma | 45 (37/8) | 45 (43/2) | 67.89±5.42 | 67.82±5.39 | Western medicine | Western medicine+Chinese herbal medicine (Anti-asthma formula)+acupuncture | 1,4,5,11-14[22] |
| Chronic persistent phase of bronchial asthma | 59 (49/10) | 59 (57/2) | 47.30±3.51 | 47.29±3.60 | Western medicine | Western medicine+Chinese herbal medicine (Xiao Qinglong decoction)+acupuncture+acupuncture | 1,4,5,38-42[23] |
| Chronic persistent phase of bronchial asthma | 35 (27/8) | 35 (32/3) | 8±2 | 7±2 | Western medicine | Western medicine+(External application)+acupuncture | 1,11,15-24,28-33[24] |
| Chronic persistent phase of bronchial asthma | 48 (41/7) | 48 (47/1) | 34.5.±4.1 | 34.3±4.5 | Western medicine | Acupuncture+Chinese herbal medicine (Sanao decoction+anti-cough dispersing formula) | 1,11,12[25] |
| Non-acute exacerbation phase bronchial asthma (Phlegm-dampness and kidney deficiency type) | 34 (23/11) | 36 (32/4) | 21~65 | 20~64 | Western medicine | Acupuncture+traditional Chinese herbal decoction | 1-4,11[26] |
| Chronic persistent phase of bronchial asthma | 49 (37/12) | 49 (47/2) | 19~70 | 18~70 | Western medicine | Western medicine+acupuncture | 1,42[27] |
| Chronic persistent phase of bronchial asthma | 50 (42/8) | 50 (49/1) | 9~66 | 10~67 | Western medicine | Acupuncture+Tuina massage | 1[28] |
| Chronic persistent phase of bronchial asthma | 40 (29/11) | 40 (37/3) | 68.49±4.83 | 67.91±5.38 | Western medicine | Western medicine+acupuncture | 1,5,14,20-22,24-27,34-37[29] |
| Chronic persistent phase of bronchial asthma | 21 (15/6) | 21 (20/1) | 16~73 | 15~72 | Ginger moxibustion therapy | Embedded thread at acupoints+ginger moxibustion therapy+electroacupuncture | 1[30] |
| Chronic persistent phase of bronchial asthma | 34 (26/8) | 33 (29/4) | 48.74±10.986 | 47.61±12.021 | Western medicine | Acupuncture+ginger moxibustion therapy | 1,3,5,19, 32,34,36,37,44,45[31] |
| Chronic persistent phase of bronchial asthma | 45 (34/11) | 45 (42/3) | 60~81 | 60~81 | Western medicine | Western medicine+Chinese herbal medicine (oral administration)+acupuncture | 1[32] |
Table 1: Characteristics of included studies.
Design and intervention measures of included studies were studied. All the included studies were conducted in China[21-32], covering various regions such as Gansu Province (1 study)[32], Henan Province (2 studies)[22,23], Guangdong Province (2 studies)[21,27], Beijing (1 study)[24], Shaanxi Province (1 study)[29], Jiangsu Province (1 study)[25], Ningxia Hui Autonomous Region (1 study)[30], Liaoning Province (1 study)[28], Fujian Province (1 study)[31], and Hebei Province (1 study)[26]. The number of individuals included ranged from 31-100, total in 1021 individuals. In studies where acupuncture was the main intervention, there were 2 studies[21,26] using acupuncture combined with Chinese medicine, 1 study[23] using acupuncture combined with Western and Chinese medicine, 1 study[24] using acupuncture combined with Western, Chinese medicine, and herbal patch, and 1 study[31] using acupuncture combined with moxibustion. The control measures mainly involved Western medicine or conventional medical therapy. In studies where acupuncture and moxibustion were used as the main interventions, there was 1 study using acupuncture combined with Chinese medicine[25], 1 study using acupuncture combined with massage[28], 2 studies using acupuncture combined with Western medicine[27,29], and 2 studies using acupuncture combined with Western medicine and Chinese medicine[22,32]. The control measures mainly involved Western medicine or conventional medical therapy. In studies where electroacupuncture was the main intervention, there was 1 study using electroacupuncture combined with acupoint embedding and ginger-separated moxibustion[30], with ginger-separated moxibustion as the control measure. The methodology of included studies is presented in Table 2 while specific intervention therapies were described in Table 3.
| Randomization process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported result | Overall bias | References |
|---|---|---|---|---|---|---|
| Low risk of bias | Low risk of bias | Significant difference in intervention methods, impossible to blind; high risk of bias | All participants completed the experiment. | Uncertain risk of bias | High risk of bias | [21] |
| Low risk of bias | ||||||
| Low risk of bias | Low risk of bias | Significant difference in intervention methods, impossible to blind; high risk of bias | All participants completed the experiment | Uncertain risk of bias | High risk of bias | [22] |
| Low risk of bias | ||||||
| Low risk of bias | Low risk of bias | Significant difference in intervention methods, impossible to blind; high risk of bias | All participants completed the experiment. | Uncertain risk of bias | High risk of bias | [23] |
| Low risk of bias | ||||||
| Low risk of bias | Low risk of bias | Significant difference in intervention methods, impossible to blind; high risk of bias | All participants completed the experiment | Uncertain risk of bias | High risk of bias | [24] |
| Low risk of bias | ||||||
| Uncertain random allocation bias risk | Low risk of bias | Significant difference in intervention methods, impossible to blind; high risk of bias | All participants completed the experiment | Uncertain risk of bias | High risk of bias | [25] |
| Low risk of bias | ||||||
| Low risk of bias | Low risk of bias | Significant difference in intervention methods, impossible to blind; high risk of bias | All participants completed the experiment. | Uncertain risk of bias | High risk of bias | [26] |
| Low risk of bias | ||||||
| Low risk of bias | Low risk of bias | Significant difference in intervention methods, impossible to blind; high risk of bias | All participants completed the experiment | Uncertain risk of bias | High risk of bias | [27] |
| Low risk of bias | ||||||
| Coin toss randomization method. Low risk of bias | Low risk of bias | Significant difference in intervention methods, impossible to blind; high risk of bias | All participants completed the experiment. | Uncertain risk of bias | High risk of bias | [28] |
| Low risk of bias | ||||||
| Uncertain random allocation bias risk | Low risk of bias | Significant difference in intervention methods, impossible to blind; high risk of bias | All participants completed the experiment | Uncertain risk of bias | High risk of bias | [29] |
| Low risk of bias | ||||||
| Computer-generated random numbers Low risk of bias |
Low risk of bias | Significant difference in intervention methods, impossible to blind; high risk of bias | All participants completed the experiment | Uncertain risk of bias | High risk of bias | [30] |
| Low risk of bias | ||||||
| Low risk of bias | Both the experimental and control groups had dropouts and unequal numbers | Significant difference in intervention methods, impossible to blind; high risk of bias | Dropouts accounted for 8.3 % in experimental group and 5.6 % in control group | Uncertain risk of bias | High risk of bias | [31] |
| High risk of bias | Low risk of bias | |||||
| Random selection and average distribution; uncertain bias risk | Low risk of bias | Significant difference in intervention methods, impossible to blind; high risk of bias | All participants completed the experiment. | Uncertain risk of bias | High risk of bias | [32] |
| Low risk of bias |
Table 2: Research method characteristics included in the study.
| S.no | Intervention method | Acupoint selection | Intervention frequency | Measurement time | Number of loss | References |
|---|---|---|---|---|---|---|
| 1 | Acupuncture treatment combined with oral Chinese herbal decoction | RN22, EX-B1, BL23, ST36, DU14, ST40, BL13, BL20 and BL17 | Dosage of medicine included twice/day for 30 d with acupuncture once every 2 d for 30 d | Before treatment and 30 d after treatment | 0,0 | [21] |
| 2 | Aminophylline injection+acupuncture therapy and oral administration of Xiao decoction | EX-B1, BL13, ST40, LI11, LU10, LU7, ST36, PC6, KI3 and SP6 | 14 d of intravenous injection along with acupuncture for 28 d once/day with Chinese herbal medicine, for 14 d twice/day | Before and after 28 d of treatment | 0,0 | [23] |
| 3 | Acupuncture+oral administration of Sanao decoction and Zhisou powder for treating cough | DU14, BL13 and LU6 | Acupuncture was followed for 2 w once/day along with medication for 2 w, one dose/day | Before and after 2 w of treatment | 0,0 | [25] |
| 4 | Acupuncture+oral Chinese herbal decoction entails | EX-B1, BL13, BL17, BL23 and ST40 | 20 sessions of acupuncture once/day with medication for 28 d, twice/day | Before treatment and 28 d after treatment | 0,0 | [26] |
| 5 | Acupuncture+Western medicine | BL23, BL13, BL43, KI3, LU9, BL26, DU4, ST36, RN6, ST40, LU7, EX-B, RN22, LU5, ST44, LI4, BL12 and GB20 | Each acupuncture session lasts for 5 min with 6 needle insertions | 6 mo after treatment | 0,0 | [27] |
| 6 | Acupuncture+massage therapy | Acupuncture: LU7, BL13, BL12, LU5, DU14, RN17, ST40, LU6, LI4, EX-B1, BL2, BL13, BL43, LU9. Tuina massage: EX-B1, BL23, BL13 and EX-HN14 |
1 needle insertion (Acupuncture) for every 5 min along with Tuina massage for 1-2 min/per acupoint | 1 y after treatment | 0,0 | [28] |
| 7 | Conventional treatment+oral asthma-relieving and anti-asthmatic formula | BL13, EX-B1, RN17, LU9 and LU7 | 14 d of Chinese herbal medicine, twice/day with 14 d of acupuncture, once/day | Before and after 14 d of treatment | 0,0 | [29] |
| 8 | Acupuncture+embedded thread at acupoints and seasonal moxibustion therapy | Seasonal moxibustion therapy at acupoints, EX-B1, DU14, BL13, BL12 and BL15, and acupuncture with moxibustion and thread embedding therapy at EX-B1, DU14, BL13, BL12, BL15, ST36 and RN22 acupoints | Seasonal moxibustion therapy was followed once for every 15 d for 6 mo | 6 mo after treatment | 0,0 | [30] |
| 9 | Acupuncture+moxibustion using separated ginger slices | Acupuncture: DU14, EX-B1, BL43, BL17, DU14 Ginger moxibustion therapy: BeiYu |
Ginger moxibustion therapy once/day for a total of 3 mo with acupuncture for 3 mo once/day | Before treatment and 90 d after treatment | 2,3 | [31] |
| 10 | Conventional Western medicine treatment, oral Chinese herbal medicine+acupuncture+massage therapy | Acupuncture: BL23, BL26, KI3, ST36, EX-B1. Cupping therapy with acupuncture: RN6, LI11 and BL13 |
- | 1 y after treatment | 0,0 | [32] |
Table 3: Characteristics of intervention therapies.
Measurement of outcome indicators of all the included studies was evaluated. In terms of outcome indicators, a total of 12 articles evaluated the efficacy primarily using the total clinical effective rate[23-34]; 6 articles evaluated treatment effects based on improvements in lung function parameters (FEV1, PEF, FEV1/FVC, etc.)[21-23,26,29,31]; 4 studies evaluated treatment efficacy based on improvements in blood indicators such as Immunoglobin E (IgE)[21,24-26]; 3 studies assessed improvements in symptom scores[24,29,31]; and 2 studies compared the Percentage (%) of cellular subgroup levels of Cluster of Differentiation (CD)3+, CD4+, CD8+, CD19+ and CD4+/CD8+ as evaluation indicators[24,29].
Quality assessment and risk of bias evaluation was studied. 12 included studies mentioned randomization, with 7 studies using computer-generated random number tables for grouping[21-24,26,27,31], 1 study using coin tossing for grouping[28], 3 studies mentioning random patient selection for grouping[25,29,32] and 1 study mentioning the use of computer-generated random numbers for grouping[30]. None of the 12 articles exhibited selective reporting bias or other sources of bias. The assessment of publication bias is shown in fig. 2.
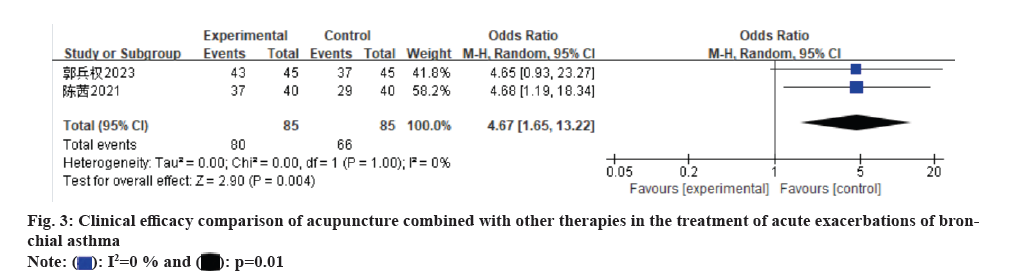
Meta-analysis results of acupuncture combined with other therapies for bronchial asthma have been discussed. Due to good similarity among the included studies, a meta-analysis was conducted. Primarily the clinical efficacy of acupuncture combined with other therapies for acute bronchial asthma was studied. In the included clinical studies, 2 studies compared the clinical efficacy of acupuncture combined with other therapies[22,29]. Total sample size was 170 and there was no heterogeneity among the studies, using a random-effects model (I²=0 % and p=1.00). Meta-analysis results showed that acupuncture treatment for acute bronchial asthma was more clinically effective than other measures (OR=4.67 and 95 % CI: 1.65-13.22) (fig. 3).
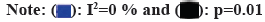
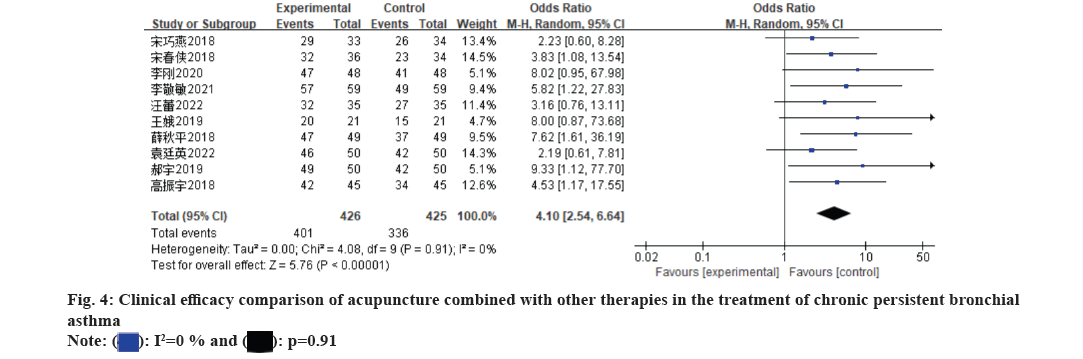
Acupuncture combined with other therapies for chronic persistent bronchial asthma was also evaluated. In the included literature, 10 studies analyzed acupuncture combined with other therapies compared to other therapies, with a total sample size of 851[21-28,30-32]. There was no significant heterogeneity among the studies (I2=0 % and p=0.91) and random-effects model was used. Meta-analysis results showed that acupuncture combined with other measures was more clinically effective than the control group for treating chronic persistent bronchial asthma (OR=4.10 and 95 % CI: 2.54-6.44) (fig. 4).
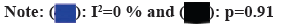
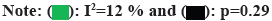
FEV1 % predicted value was assessed for the treatment of acupuncture combined with other therapies for acute bronchial asthma. In the included clinical studies, 2 studies compared the FEV1 % predicted of acupuncture combined with other therapies with other therapies[22,29]. The total sample size was 170 where we found slight heterogeneity among the studies (I²=12 % and p=0.29), using a random-effects model. Meta-analysis results showed that the FEV1 % Pred of acupuncture treatment for acute bronchial asthma was superior to other measures (OR=4.93 and 95 % CI: 2.22-7.64) (fig. 5).
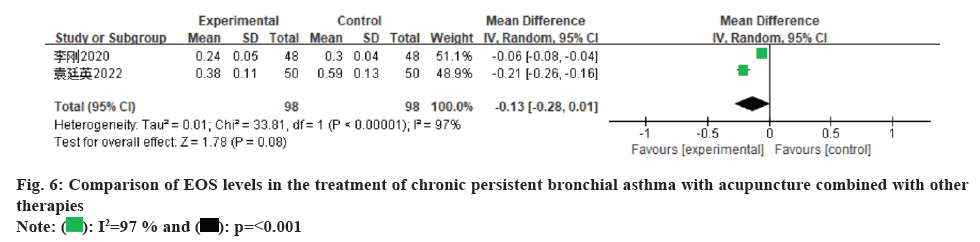
Eosinophil (EOS) level after undergoing treatment with acupuncture combined with other therapies for chronic persistent bronchial asthma was studied. 2 studies analyzed acupuncture combined with other therapies compared to other therapies[21,25]. The total sample size was 196 and there was significant heterogeneity among the studies (I2=97 % and p<0.00001), using a random-effects model. Meta-analysis results showed that the EOS level in acupuncture combined with other measures for treating chronic persistent bronchial asthma was not significantly different from that in the control group (MD was -0.13 and 95 % CI: -0.28 to 0.01) (fig. 6).
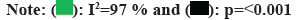
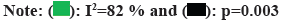
FEV1 level was evaluated after undergoing treatment with acupuncture combined with other therapies for chronic persistent bronchial asthma was evaluated. 3 studies analyzed acupuncture combined with other therapies compared to other therapies[21,23,26]. The total sample size was 288 and there was significant heterogeneity among the studies (I2=82 % and p=0.003), using a random-effects model. Meta-analysis results showed that the FEV1 level in acupuncture combined with other measures for treating chronic persistent bronchial asthma was not significantly different from that in the control group (MD was 0.45 and 95 % CI: 0.16-0.74) (fig. 7).
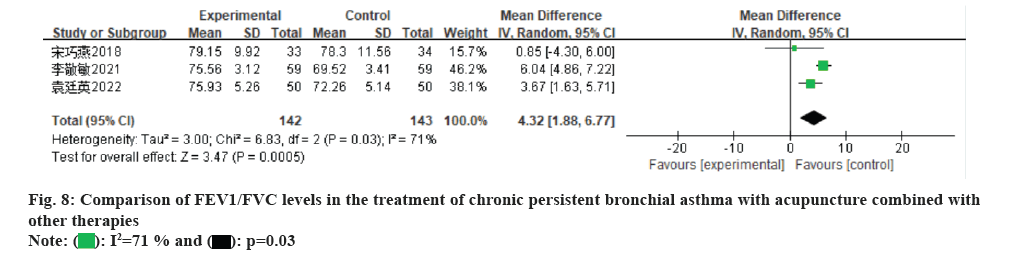
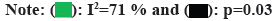
Acupuncture combined with other therapies for chronic persistent bronchial asthma was studied. 3 studies analyzed acupuncture combined with other therapies compared to other therapies[21,23,31]. The total sample size was 285 and there was significant heterogeneity among the studies (I²=71 % and p=0.03), using a random-effects model. Meta-analysis results showed that the FEV/FVC level in acupuncture combined with other measures for treating chronic persistent bronchial asthma was superior to that in the control group (MD was 4.32 and 95 % CI: 1.88-6.77) (fig. 8).
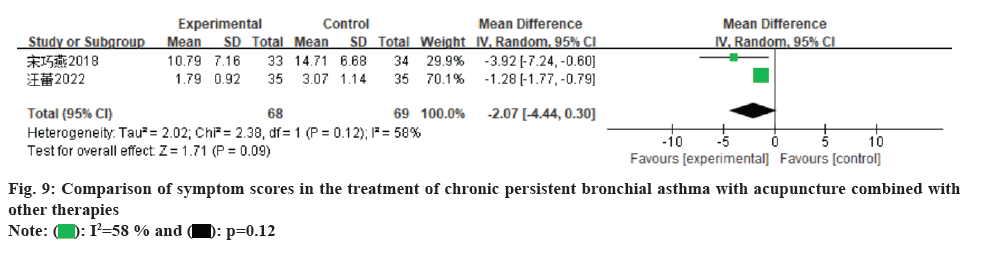
Further, symptom scores were compared after undergoing acupuncture combined with other therapies for chronic persistent bronchial asthma. 2 studies analyzed acupuncture combined with other therapies compared to other therapies[24,31]. The total sample size was 137 and there was moderate heterogeneity among the studies (I²=58 % and p=0.12), using a random-effects model. Meta-analysis results showed that the symptom score comparison in acupuncture combined with other measures for treating chronic persistent bronchial asthma was not significantly different from that in the control group (MD was -2.07 and 95 % CI: -4.44 to 0.30) (fig. 9).
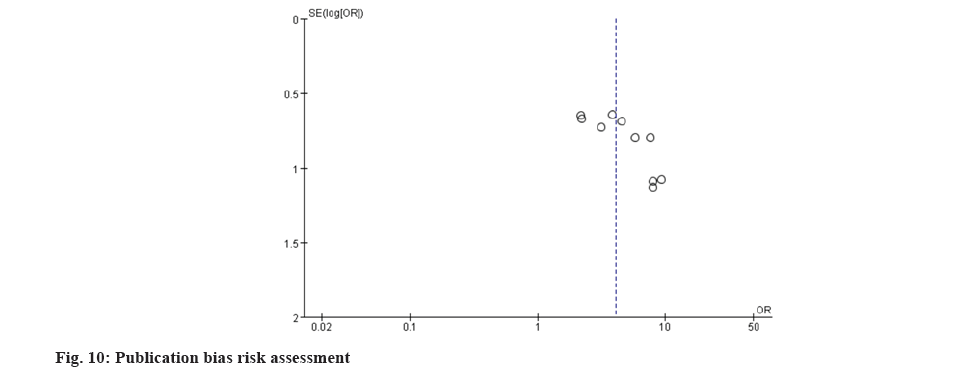
Subsequently, publication bias assessment was evaluated. 10 studies analyzed funnel plot asymmetry for the clinical efficacy of acupuncture combined with other therapies compared to other therapies for chronic persistent bronchial asthma[21,23-28,30-32]. The results showed that the funnel plot was generally symmetrical and within the confidence interval range, indicating a low likelihood of publication bias (fig. 10).
A meta-analysis of 12 studies[21-32] revealed that combining acupuncture with other therapies in treating bronchial asthma yields diverse approaches and significantly enhances clinical outcomes compared to Western or TCM alone; multiple prognostic indicators demonstrated superior efficacy.
Throughout the history, TCM practitioners have proposed various understandings regarding the etiology and pathogenesis of asthma. This encompasses the theories like phlegm-dampness pathogenesis, the complex interplay of cold and heat, dietary influences, external pathogens and underlying root causes[33]. Treatment emphasizes nourishing the lung, spleen and kidney, eliminating phlegm sources, and dispelling phlegm and stasis to address recurrent bronchial asthma attacks. During the acute phase, when righteousness is deficient and pathogenic factors are excessive, treatment involves descending qi, transforming phlegm, halting coughing, relieving asthma and strengthening the body while enhancing blood circulation. In the chronic remission phase, the focus shifts to nourishing the spleen and lung, warming the kidney, absorbing qi, transforming phlegm and promoting blood circulation[34].
Previous literature displays a diverse range of acupuncture styles paired with various therapies. This study's literature encompasses the techniques such as supplementing and draining method, treating winter diseases in summer, twisting and supplementing-draining method, mid-day midnight flow acupuncture method with even supplementing and draining method being predominant. Different perspectives, practitioners and texts attribute varying meanings to this method. Despite its widespread use in contemporary practice and research, ancient and modern literature diverges in describing its attributes, concepts, connotations and techniques. In ancient times, ping bu ping xie (mild tonifying and attenuating) wasn't an independent acupuncture technique but was a generalized approach for tonifying and reducing[35]. Modern ping bu ping xie techniques differ significantly from those described in ancient texts and it focuses on balanced techniques of lifting, thrusting and twisting, suitable for conditions of neither deficiency nor excess, maintaining tonification-reducing principles and clinical indications[36,37]. Other therapies combined with acupuncture encompass cupping, moxibustion with sliced ginger, massage, seasonal needling techniques, embedding acupuncture needles, applying herbal patches and oral herbal medicine administration. Herbal formulas include Yishen Huoxue Pingchuan decoction, combination of Zhenwu with Xiao Qinglong decoction, combination of Cansu Wenzhe with Sanzi Yangqin decoction and combination of San'ao with Zhisuo San decoction.
According to 12 studies that have been summarized, the most commonly used acupoints are Dingchuan, Shenshu, Feishu, Zusanli, Fenglong and Dazhui. 9 studies used Dingchuan and Feishu, while 4 used Feishu and Dazhui concurrently, consistent with Zhang Jiaxun's description[38]. Feishu and Dingchuan are local acupoint pairs that enhance the local meridian circulation synergistically. The combination of Feishu and Dingchuan dispels wind, expels the heat and regulates lung qi to relieve asthma; it is often used for acute exacerbations and chronic persistent asthma, potentially substituting β2 agonists to prevent adverse reactions like palpitations and anxiety[39]. From the location and meridian of the acupoint, Feishu is located 1.5 cun beside the spinous process of the third thoracic vertebra on both sides, which is a specific acupoint where the qi of the lung is transmitted to the back[40]. Its location is close to the lung, making it the most frequently used acupoint in acupuncture treatment for asthma[41,42]. Dingchuan is an extraordinary acupoint which lies 0.5 cun beside the midline below the spinous process of the 7th cervical vertebra. It's empirically effective for asthma treatment, serving as a primary acupoint for addressing asthma and coughing[43]. A review of domestic and international literature on acupuncture for asthma revealed that the Dingchuan acupoint is the 2nd most commonly used point for asthma treatment, following only the Feishu acupoint[44].
With advancing research, modern medicine classifies bronchial asthma as a heterogeneous disease, categorized into acute exacerbation, chronic persistence and clinical remission periods based on clinical manifestations[45].
Predominant TCM syndrome classification for asthma which is outlined as per the guiding principles for clinical research of new Chinese medicines, categorizes the acute exacerbation phase into cold, heat and phlegm-wind asthma. Meanwhile, the remission phase primarily involves syndromes of lung qi, spleen qi and kidney qi deficiency[46]. Wang[47] explained that the TCM syndrome clustering during the chronic persistent period comprises three types, yang deficiency with hidden fluid retention syndrome, mixed syndrome of cold and heat and yin deficiency with phlegm-heat syndrome. Recent literature analysis reveals that compared to previous systematic reviews, TCM provides a broader array of treatment options for bronchial asthma. The concurrent application of acupuncture alongside other therapies demonstrates notable efficacy in asthma treatment, suggesting a promising clinical utility of combining acupuncture with other modalities for managing bronchial asthma.
All the literature included in this study originates from China, potentially introducing regional bias. Some studies merely mention random without specifying the randomization method. Many studies lack adequate allocation concealment and blinding, potentially compromising the quality of research evidence. Given acupuncture's unique nature, it is challenging to patients and researchers, but technique of blinding should be applied in data collection, efficacy assessment and statistical analysis. This study encompasses relatively small number of trials, potentially impacting the robustness of conclusions drawn. Further high-quality evidence is required to enhance these findings.
In summary, this study indicates that acupuncture, whether used alone or as an adjunct therapy, is safe and efficacious for treating bronchial asthma, surpassing Western medicine. It holds particular clinical advantages in ameliorating symptoms and can serve as a complementary treatment alongside Western medicine without increasing the risk of adverse reactions.
Author’s contributions:
Fei Wang, Chunxue Meng and Zi’an Zhou are the co-first authors.
Funding:
This study was supported by the Key Research and Development Plan of Ningxia Hui Autonomous Region (Approval No: 2022BEG02040); National Natural Science Foundation of China (Approval No: 82260967); Natural Science Foundation of Ningxia Hui Autonomous Region (Approval No: 2022AAC05030); Key Research and Development Plan of Ningxia Hui Autonomous Region (Approval No: 2021BEB04023); School-level project of Ningxia Medical University (Approval No: XZ2021004) and the Natural Science Foundation of Ningxia (Approval No: 2022AAC02070).
Conflict of interests:
The authors declared no conflict of interests.
References
- Huo H, Yang Y, Dong J, Mao Z, Hu P, Song F. Development of a personalized pharmacologic treatment repository for bronchial asthma based on the 2018 guideline for the diagnosis and management of bronchial asthma in primary care (practice edition). Chin Gen Pract 2022;25(10):1181.
- Zhang J, Liu C, Mu J, Sha L, Li S, Song X. Long-term trajectories of lung function and risk factors in children with bronchial asthma. Chin J Appl Clin Pediatr 2022;1458-63.
- Deng Z, Lu SH, Zhang QL. Research progress on the application of quantitative proteomics in biomarkers of bronchial asthma. Chin Med J 2022;102(34):2711-15.
- Rathod A, Zhang H, Arshad SH, Ewart S, Relton CL, Karmaus W, et al. DNA methylation and asthma acquisition during adolescence and post-adolescence, an epigenome-wide longitudinal study. J Pers Med 2022;12(2):1-18.
[Crossref] [Google Scholar] [PubMed]
- Lin SC, Shi LS, Ye YL. Advanced molecular knowledge of therapeutic drugs and natural products focusing on inflammatory cytokines in asthma. Cells 2019;8(7):1-24.
[Crossref] [Google Scholar] [PubMed]
- Padem N, Saltoun C. Classification of asthma. Allergy Asthma Proc 2019;40(6):385-8.
[Crossref] [Google Scholar] [PubMed]
- Trikamjee T, Comberiati P, Peter J. Pediatric asthma in developing countries: Challenges and future directions. Curr Opin Allergy Clin Immunol 2022;22(2):80-5.
[Crossref] [Google Scholar] [PubMed]
- Wang E, Zahid S, Moudgal AN, Demaestri S, Wamboldt FS. Intimate partner violence and asthma in pediatric and adult populations. Ann Allergy Asthma Immunol 2022;128(4):361-78.
[Crossref] [Google Scholar] [PubMed]
- Shi ZH H, Shi ZH F. The research progress of bronchial asthma. J Med Pharm Chin Minor 2014;20(11):62-5.
- Zhang JL. Overview of the mechanisms of drug therapy for bronchial asthma. Chin J Clin Med 2017;4(85):16812-3.
- Zhong JW, He JY, Xie JD. Study on the medication rules of traditional Chinese medicine compound prescriptions for the treatment of asthma based on the patent database. Mod Med Lab 2023;51(5):575-82.
- Liu Y L, Wang Q. A brief analysis of Shegan Mahuang decoction in the treatment of acute outbreaks of bronchial asthma. J Chin Clin Med 2023;15(27):27-30.
- Zang XL, Wang PY. Discussion on the perennial roots of asthma. Chin Med Mod Distance Educ 2024;22(5):35-7.
- Wu FM, Su SHCH, Li H. The Relationship between phenotypes of airway inflammation during acute asthma attacks and traditional Chinese medicine syndrome differentiation. Chin J Integr Med 2020;30(5):426-8.
- Liu L, Shen YT, Zhang AI H. Clinical analysis of traditional Chinese medicine Shu Gan Jie You in treating bronchial asthma. J Tradit Chin Med 2023;42(5):58-9.
- Zhang J, Shao SJ, Ren ZH. Multi-central clinical research on asthma with clod fluid retained in lung treated with ‘Three acupoints and five needles therapy’. Chin J Integr Med 2018;33(2):797-800.
- Liang XX, Deng M, Chen JY. Clinical study of filiform-fire needle in the treatment of acute attack of bronchial asthma. Chin Pharm J 2021;11(13):50-3.
- Zhang YQ. The effect of acupuncture treatment on pulmonary function in patients with acute asthma attacks. Chin J Clin Med 2020;7(10): 63-4.
- Tang Y B,Qin L H, Effects of acupuncture lung and large intestine network on bronchial asthma patients. J Hubei Univ Chin Med 2014;16(1):90-2.
- Li CX, Li ZX, Wang D, Zhang RY, Wang YH, Zeng Y, et al. Advances in the clinical research on acupuncture in treatment of respiratory diseases. Zhen Ci Yan Jiu Acupunct Res 2020;45(2):169-72.
- Yuan YY, Zhong FX, Liu T. Clinical efficacy and safety of Yishen Pingchuan decoction combined with acupuncture in treating bronchial asthma. Chin J Clin Ration Drug Use 2022;15(15):61-3.
- Guo BQ, Huang HN, Wang YM. Clinical observation of the treatment of acute attacks of bronchial asthma in elderly patients with Zhi Xiao Ping Chuan formula combined with Ziwu flow injection acupuncture. Tradit Chin Med 2023;39(3):518-20.
- Li JM. The Effect of acupuncture combined with Xiao Qing long decoction on pulmonary function and serum inflammatory factors in the treatment of bronchial asthma. Tradit Chin Med 2021;37(7):1170-2.
- Wang L, Zhao J, Zhao Y. Clinical study of acupuncture combined with Chinese medicinal acupoint sticking for bronchial asthma in children. Shanghai J Acupunct 2022;41(2):174-9.
- Li G. The Impact of acupuncture combined with Sanao decoction and modified Zhisou San in treating 48 cases of bronchial asthma on the body's immune function. J Clin Aesthet Dermatol 2020;29(9):113-5.
- Song CHX, Yv YY, Sun N. Clinical study of acupuncture and herbal medicine combination therapy for non-acute exacerbations of phlegm-dampness and kidney deficiency type bronchial asthma. J Tradit Chin Med 2018;33(4):52-4.
- Xue QP, Cai TT, Jiang QY. Clinical observation on treatment of bronchial asthma with acupuncture and moxibustion. Contemp Med 2018;24(33):42-4.
- Hao Y. Clinical observation of acupuncture, moxibustion, and tuina therapy in the treatment of bronchial asthma. Chin Med J 2019;17(18):173-4.
- Chen Q, Wang W, Liu YL. Clinical study of Zhixiao Pingchuan prescription combined with Ziwu Liuzhu acupuncture in the treatment of the acute attack period of elderly bronchial asthma. Prog Mod Biomed 2021;21(19):3760-4.
- Wang E, Wang ZHW. The efficacy of acupuncture, acupoint embedding, and seasonal acupoint therapy combined with moxibustion in treating bronchial asthma. China Health Care Nutr 2019;29(35):288-9.
- Song QY. Prevention and treatment on asthma in chronic persistent period with acupuncture and moxibustion therapy: An observation on patients with summer treatment for the winter diseases. Fujian Univ Tradit Chin Med 2018;11:312-5.
- Gao ZHY. Clinical study of traditional Chinese medicine diagnosis and treatment for elderly patients with chronic bronchial asthma. Psychological Res 2018;24(23):176-7.
- Liu H. Clinical observation of stopping aerosol in treating bronchial asthma. J Tradit Chin Med 2013;35(10):39-40.
- Zhu JF. Research on the diagnostic and therapeutic thinking and methods of traditional Chinese medicine for bronchial asthma. J Tradit Chin Med 2016;22(2):284-6.
- Shi WX, Chen XL, Yan HY. Origin and evolution of even reinforcing-reducing acupuncture method. J Tradit Chin Med 2023;39(6):91-6.
- Lou BC, Lou XH. On the acupuncture method of even reinforcing-reducing method. J Tradit Chin Med 1982(4):46-8.
- Shu Y, Yuan Q. Discussion on mild reinforcing and mild reducing in ancient time and present time. J Acupunct Meridian Stud 2022;38(7):94-7.
- Zhang JX. On selection and compatibility of acupuncture treatment of asthma based on data mining (periodical literature). Changchun Univ Chin Med 2020;12:224-6.
- Qiao Y, Liang Y, Zhuo S, Yang X, Liang T, Ling X, et al. Effect and mechanism of acupuncture on airway smooth muscle relaxation during acute asthma attack in rats. J Clin Acupunct 2024;44(3):295-302.
- Chen MJ, ZHong YL, Chen XY. Psychological communication needs and nursing strategies for children receiving lung yu acupoint injections in special clinics. J Emerg Med 2023;28(5):507-9.
- Zhang GS, Qiu RR, Pan J, Zhang J, Zhang C, Wang CX. Commonality and pattern analysis of acupoint selection in moxibustion treatment of asthma. J Acupunct Tuina Sci 2019;17(6):451-6.
- Zheng HZ, Qi QI, Xiong J, Jun CH, Guan LC. Moxibustion pre-treatment inhibits RhoA/ROCK signaling to prevent lung inflammation in asthmatic rats: Moxibustion pre-treatment reduces RhoA/ROCK signal expression and prevents pneumonia in asthmatic rats. World J Tradit Chin Med 2022;32(3):230-6.
- Li Tie, Jing W, Zuo XW. Clinical observation of acupuncture combined with cupping therapy at dingchuan acupoint in treating bronchial asthma. Biotech World 2016;(4):201-3.
- Li MY. Clinical observation on combination of acupuncture and moxibustion at single point and acupoint for bronchial asthma. Changchun Univ Chin Med 2020;6:129-132.
- Diagnostic criteria, clinical staging, and severity classification of bronchial asthma. Chin J Difficult Compl Cases 2006;3:180-6.
- Meng Q, Kong N, Zhang J. Progress in herbal medicine treatment for bronchial asthma. J Tradit Chin Med 2019;37(6):100-1.
- Wang ZX. Correlation between clinical staging of bronchial asthma and TCM syndromes. Yunnan Univ Chin Med 2019;26:113-7.
 .
.
 .
.
 .
.
 .
.
 .
.
 .
.
 .
.
 .
.