- *Corresponding Author:
- Xiao Rong Chen
Department of Anesthesia, University-Town Hospital of Chongqing Medical University, No. 55 middle Road of University-Town, Gaoxin district, Chongqing 401331, China
E-mail: ccbb662661@163.com
| This article was originally published in a special issue, “Clinical Research in Pharmaceutical and Biomedical Sciences” |
| Indian J Pharm Sci 2021:83(1)Spl issue1;18-22 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
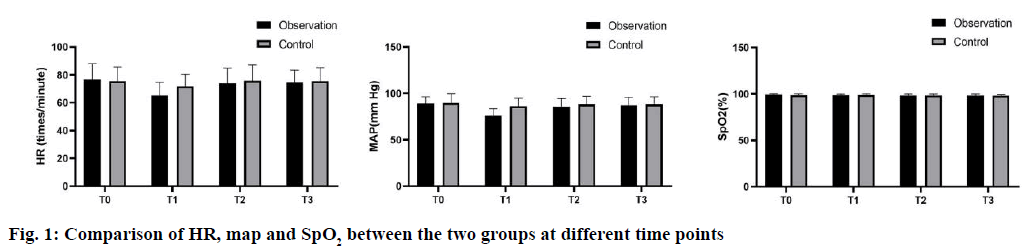
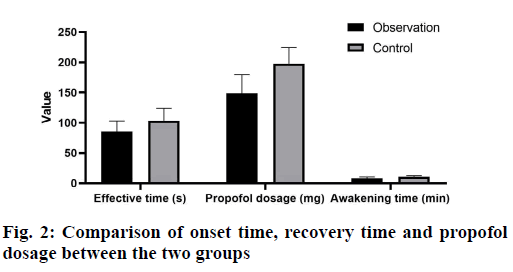
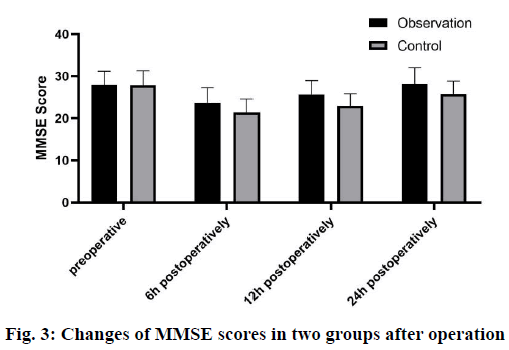
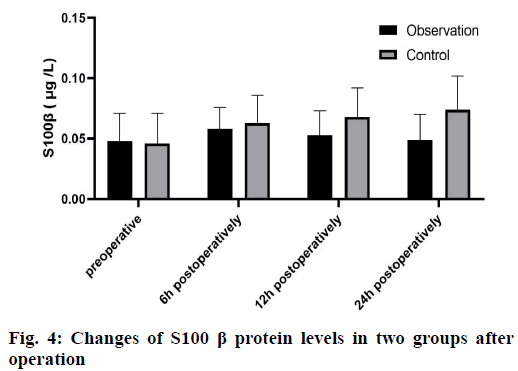
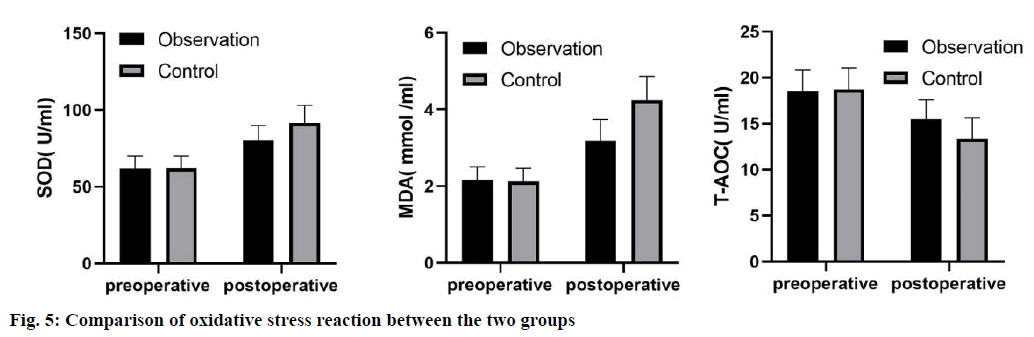
To investigate the analgesic effect and safety of Dexmedetomidine compounded with propofol in laparoscopic cholecystectomy patients. 136 patients who underwent elective laparoscopic cholecystectomy from June 2018 to June 2020 in our hospital were selected, and all patients were classified into Class I~II according to the American Society of Anesthesiologists classification, and were divided into control group and observation group according to the random number table method, with 68 patients in each group. The patients in the observation group were first injected with Dexmedetomidine hydrochloride 1 μg/kg intravenously and then propofol 2 mg/kg intravenously for about 10 min. the patients in the control group were treated with placebo, i.e. 5 ml of 0.9 % saline intravenously followed by propofol 2 mg/kg intravenously. The postoperative recovery of the 2 groups was compared; a simple mental status scale score to evaluate the postoperative cognitive function changes; S100 calcium-binding protein B and oxidative stress indexes were measured in patients before and after surgery. The differences in heart rate, mean arterial pressure and blood oxygen saturation between the two groups at T0 were not statistically significant (p>0.05); at T1, heart rate and mean arterial pressure of the two groups were significantly lower than those at T0 (p<0.05), and the differences in heart rate and mean arterial pressure between the observation group and the control group at T1 were statistically significant. Significance (p<0.05). However, there was no statistically significant difference in blood oxygen saturation between the two groups at different time points (p>0.05). After the administration of blood oxygen saturation, the mean onset of effect time, time of awakening and the dosage of propofol in the observation group were significantly less than that in the control group (p<0.05). The simple mental status scale scores were significantly higher in the observation group than in the control group at 6 h, 12 h and 24 h after surgery, and the difference was statistically significant (p<0.05); S100 calcium-binding protein B was significantly lower in the observation group than in the control group at 24 h after surgery, and the difference was statistically significant (p<0.05); postoperative superoxide dismutase, malondialdehyde, and malondialdehyde were significantly higher in the observation group than in the control group (p<0.05). The total antioxidant capacity was significantly increased, and the total antioxidant capacity was significantly decreased (p<0.05); the postoperative superoxide dismutase and malondialdehyde were significantly lower than those of the control group, and the total antioxidant capacity was significantly higher than that of the control group, and the difference was statistically significant (p<0.05). Laparoscopic cholecystectomy using propofol compounded with Dexmedetomidine can significantly reduce oxidative stress, reduce brain tissue damage, and protect patients’ cognitive function, with satisfactory resultsy.
Keywords
laparoscopic cholecystectomy, analgesia, Dexmedetomidine, propofol
Laparoscopic cholecystectomy, as a kind of laparoscopic surgery, has the advantages of small trauma, quick recovery and less complications, and is widely used in surgery[1,2]. In the process of laparoscopic surgery, tracheal intubation, extubation and other operations can make patients produce strong stress response, affect perioperative hemodynamic balance, and may cause postoperative cognitive dysfunction[3]. Relevant studies have shown that improper use of narcotic drugs will increase the risk of adverse reactions[4]. For laparoscopic surgery, it is particularly important to choose suitable anesthetic drugs and increase the accuracy and standardization of operation to ensure the safety of patients. The aim of this study was to investigate the analgesic effect and safety of dexmedetomidine combined with propofol in painless gastrointestinal endoscopy. A total of 136 patients undergoing laparoscopic cholecystectomy in our hospital from June 2018 to June 2020 were selected. All patients were divided into grade I~II according to the American Society of Anesthesiology (ASA), and randomly divided into observation group and control group, 68 cases in each group. The patients in the observation group included 42 males and 26 females, with an average age of (55.26±6.31) y old (32-75 y old), weight (67.09±4.20) kg, height (168.20±7.35) cm, 3 cases with hypertension and 5 cases with diabetes mellitus. The control group consisted of 43 males and 25 females, aged 34-73 y (mean 54.75±5.80) y, weight (67.23 ±3.19 kg), height (167.76±7.20) cm, 2 cases with hypertension and 6 cases with diabetes mellitus. There was no significant difference in gender, age, weight, height, hypertension and diabetes between the two groups (p>0.05). The study was approved by the hospital ethics committee; all participants agreed and signed informed consent. Exclusion criteria: Women in menstruation, lactation and pregnancy; Patients with severe hypertension and coronary heart disease; Conversion to laparotomy in laparoscopic surgery; Simple mental status scale (MMSE) score <23; Sedative and analgesic drug use history within 30 d or previous drug allergy history. All patients were given routine fasting before operation, and the vital signs such as pulse, blood pressure and heart rate were detected before operation; in addition, venous access was established and oxygen was given through nasal catheter with oxygen flow of 4 l/min. Patients in the observation group were given Dexmedetomidine hydrochloride injection 1 μg/kg, and propofol injection 2 mg/kg was injected intravenously about 10 min later. The control group was treated with placebo, i.e. intravenous injection of 5 ml 0.9 % normal saline, and then 2 mg/kg propofol injection. Laparoscopic surgery was performed after the disappearance of eyelash reflex in the two groups. If body movement reaction occurred during the operation, intermittent operation and additional injection of propofol were required. After the operation, the patient is sent to the observation room and can move freely until he is fully awake. When the patient has no adverse reactions such as dizziness, nausea and vomiting, and the vital signs such as heart rate and blood pressure are stable, the patient can leave the observation room. Observation index: Heart rate (HR) was observed at the following 4 time points: 5 min before administration (T0), at the beginning of operation (T1), at 5 min after operation (T2) and 5 min after operation (T3); as well as mean arterial pressure (map) and blood oxygen saturation (SpO2); The onset time of anesthesia, the dosage of propofol, the recovery time and the time of leaving hospital were observed. The recovery time refers to the time from the end of gastroscope operation to the first eye opening, and the time of leaving the hospital refers to the time from waking up to leaving the monitoring room; MMSE score was used to evaluate cognitive function and serum S100 calcium-binding protein B (S100 β) protein level was detected by double antibody sandwich method at 6, 12, 24 h before and after the operation; Before and after operation (after extubation), the levels of superoxide dismutase (SOD) and malondialdehyde (MDA) were measured by xanthine oxidase method, MDA level by thiobarbituric acid chemical colorimetry and the level of total antioxidant capacity (T-AOC) was measured by total antioxidant capacity kit. SPSS 20.0 statistical software was used to analyze the data. The measurement data were expressed by x±s and t test. p<0.05 was considered to be statistically significant. There was no significant difference in HR, map and SpO2 between the two groups at T0 (p>0.05); HR and map of the two groups at T1 were significantly lower than those at T0 (p<0.05), and the differences of HR and map between the observation group and the control group at T1 were statistically significant (p<0.05). However, there was no significant difference in SpO2 between the two groups at different time points (p>0.05), as shown in fig. 1. After administration, the average onset time, recovery time and propofol dosage of the observation group were significantly shorter than those of the control group (p<0.05), and the difference in the average dosage of propofol between the two groups was statistically significant (p<0.05), as shown in fig. 2. The MMSE score and S100 β protein of the two groups were significantly changed (p<0.05); the MMSE score of the observation group was significantly higher than that of the control group at 6 h, 12 h and 24 h after operation (p<0.05); the S100 β protein in the observation group was significantly lower than that in the control group at 24 h after operation (p<0.05), as shown in fig. 3 and fig. 4. There was no significant difference in SOD, T-AOC and MDA between the two groups before operation (p>0.05); after operation, SOD and MDA in the two groups were significantly increased, and T-AOC was significantly decreased (p<0.05); after operation, SOD and MDA in the observation group were significantly lower than those in the control group, and T-AOC was significantly higher than that in the control group (p<0.05), as shown in fig. 5. Postoperative cognitive dysfunction refers to the patients’ cognitive ability, memory, orientation, sleep, consciousness and other acute disorder syndrome within a few days after surgery, which has the characteristics of volatility and reversibility[5]. Clinical research results show that the imbalance of cerebral oxygen metabolism during perioperative period is closely related to postoperative cognitive function[6]. Propofol can improve the function of gamma-aminobutyric acid (GABA) receptor and inhibit the long term effect of hippocampus. Some studies have found that general anesthesia combined with dexmedetomidine in laparoscopic surgery can effectively improve the anesthetic effect and help to maintain hemodynamic stability[7]. Dexmedetomidine, as an α2-adrenoceptor agonist, has the effects of sedation, analgesia and anti-anxiety, can reduce sympathetic nerve excitation and maintain hemodynamic stability[8]. Meanwhile, Dexmedetomidine has a certain protective effect on brain tissue, and will not affect the patient’s perioperative spontaneous respiratory function[9]. Our results showed that the eye opening time, extubation time and orientation recovery time in the observation group were significantly lower than those in the control group, indicating that the recovery time of patients after propofol combined with dexmedetomidine anesthesia was significantly shorter. The possible reason is that the concentration of propofol in the blood and tissues of patients is low, and the elimination rate is high after operation, which helps to shorten the recovery time of patients[10]. MMSE score is one of the important methods to evaluate cognitive function, which has good reliability and effectiveness[11]. The results of present study showed that MMSE scores at 6 and 12 h after operation in both groups were significantly lower than those before operation, indicating that the cognitive function of patients after laparoscopic cholecystectomy would be decreased by the two anesthesia methods; while the MMSE scores of the observation group at 6, 12 and 24 h after operation were significantly higher than those of the control group, indicating that propofol can maintain the postoperative mental state of patients better. The possible reason is that propofol can significantly improve the neuroelectrophysiological response caused by glucose free hypoxia, and the hippocampus is the most sensitive part of hypoxia, which is closely related to cognitive function. Through the hippocampus and, The hippocampal activity is required for forming and reconstructing relational memory, propofol can effectively reduce the brain tissue damage caused by oxidative stress reaction and alleviate the decrease of cognitive function of which is certainly a beneficial property[12]. S100 β protein is a protein substance secreted by glial cells and plays a role in learning and memory. It is often used to evaluate nervous system injury in clinic, and its expression level is positively correlated with nervous system injury[13]. Our results suggest that the level of S100 β protein in the observation group is significantly lower than that in the control group at 24 h after operation, which indicates that propofol has less nerve damage during the perioperative period and is helpful to protect brain tissue. Oxidative stress reaction can reflect the degree of brain tissue damage in surgical patients, among which SOD belongs to oxygen free radical scavenging enzyme, which can reflect the overall antioxidant capacity of the body; while MDA is a kind of damage toxic product produced by the body during stress reaction, which can reflect the degree of brain tissue free radical damage[14,15]. The results of this study showed that the levels of SOD and MDA were significantly increased and the level of T-AOC was significantly decreased in the two groups after operation, which indicated that both anesthesia methods could cause oxidative stress reaction to a certain extent after operation, and affect the hemodynamic level, resulting in the increase of oxidative stress products and the decrease of antioxidative ability. We confirmed that the level of SOD and MDA in the observation group was significantly lower than that in the control group after operation, and the level of T-AOC was significantly higher than that in the control group, indicating that the degree of oxidative stress in the observation group was significantly lighter than that in the control group, and the postoperative antioxidant capacity was significantly better than that in the control group, indicating that the protective effect of propofol on brain tissue and oxygen free radical scavenging capacity were significantly better. In conclusion, propofol combined with Dexmedetomidine in laparoscopic cholecystectomy can significantly reduce oxidative stress reaction, reduce brain tissue damage and protect cognitive function of patients.
Conflicts of interest:
The authors report no conflicts of interest.
Acknowledgements:
This work was supported by The First Affiliated Hospital of Hainan Medical College and University- Town Hospital of Chongqing Medical University, Xue Fei Lu and Xiu Yu Cai contributed equally to this work.
References
- Khare A, Sharma SP, Deganwa ML, Sharma M, Gill N. Effects of dexmedetomidine on intraoperative hemodynamics and propofol requirement in patients undergoing laparoscopic cholecystectomy. Anesth Essays Res 2017;11:1040.
- Sharma P, Gombar S, Ahuja V, Jain A, Dalal U. Sevoflurane sparing effect of dexmedetomidine in patients undergoing laparoscopic cholecystectomy: A randomized controlled trial. J Anaesthesiol Clin Pharmacol 2017;33:496.
- Subasi H, Ozdemir KI, Duger C, Kaygusuz K, Isbir AC, Gursoy S, et al. Dexmedetomidine and remifentanil as adjuncts to total intravenous anesthesia with propofol. Anaesth Pain & Intensive Care 2017;21:328-34.
- Bhutia MP, Rai A. Attenuation of Haemodynamic parameters in response to pneumoperitoneum during laparoscopic cholecystectomy: a randomized controlled trial comparing infusions of propofol and dexmedetomidine. J Clin Diagn Res 2017;11:UC01.
- Bhagat N, Yunus M, Karim HM, Hajong R, Bhattacharyya P, Singh M. Dexmedetomidine in attenuation of haemodynamic response and dose sparing effect on opioid and anaesthetic agents in patients undergoing laparoscopic cholecystectomy-A randomized study. J Clin Diagn Res 2016;10:UC01.
- Yang X, Xie J, Liu J, Wang T. Effects of dexmedetomidine on the deformability of erythrocyte in patients with laparoscopic cholecystectomy. Pak J Pharm Sci 2016;29.
- Park HY, Kim JY, Cho SH, Lee D, Kwak HJ. The effect of low-dose dexmedetomidine on hemodynamics and anesthetic requirement during bis-spectral index-guided total intravenous anesthesia. J Clin Monit Comput 2016;30:429-35.
- Bakan M, Umutoglu T, Topuz U, Uysal H, Bayram M, Kadioglu H, et al. Opioid-free total intravenous anesthesia with propofol, dexmedetomidine and lidocaine infusions for laparoscopic cholecystectomy: a prospective, randomized, double-blinded study. Rev Bras Anestesiol 2015;65:191-9.
- Bakan M, Umutoglu T, Topuz U, Uysal H, Bayram M, Kadioglu H, et al. Anestesia venosa total livre de opioides, com infusões de propofol, dexmedetomidina e lidocaína para colecistectomia laparoscópica: Estudo prospectivo, randomizado e duplo-cego. Rev Bras Anestesiol 2015;65:191-9.
- Anjum N, Tabish H, Debdas S, Bani HP, Rajat C, Basu GD. Effects of dexmedetomidine and clonidine as propofol adjuvants on intra-operative hemodynamics and recovery profiles in patients undergoing laparoscopic cholecystectomy: A prospective randomized comparative study. Avicenna J Med 2015;5:67.
- Srivastava VK, Nagle V, Agrawal S, Kumar D, Verma A, Kedia S. Comparative evaluation of dexmedetomidine and esmolol on hemodynamic responses during laparoscopic cholecystectomy. J Clin Diagn Res 2015;9:UC01.
- Li N, Xiong L, Wu YH, Chen XJ, Meng YZ, Li SF, et al. Effects of dexmedetomidine on cognitive function in elderly patients after laparoscopic cholecystectomy: A protocol for systematic review and meta-analysis. Medicine 2020;99:e20177.
- Zoroufchi BH, Zangian H, Abdollahpour A. Examination of the sedative and analgesic effects of gabapentin and dexmedetomidine in patients undergoing laparoscopic cholecystectomy surgery: A randomized controlled trial. J Family Med Prim Care 2020;9:1042.
- Naemi AR, Kashanitabar V, Kamali A, Shiva A. Comparison of the Effects of Haloperidol, Metoclopramide, Dexmedetomidine and Ginger on Postoperative Nausea and Vomiting After Laparoscopic Cholecystectomy. J Med Life 2020;13:206.
- Chilkoti GT, Karthik G, Rautela R. Evaluation of postoperative analgesic efficacy and perioperative hemodynamic changes with low dose intravenous dexmedetomidine infusion in patients undergoing laparoscopic cholecystectomy?A randomised, double-blinded, placebo-controlled trial. J Anaesthesiol Clin Pharmacol 2020;36:72.