- *Corresponding Author:
- Yanling Hong
Department of Cardiology, Luzhou People’s Hospital, Luzhou, Sichuan Province 646000, China
E-mail: heaven19842023@163.com
| This article was originally published in a special issue, “Innovations in Biomedical Research and Drug Development” |
| Indian J Pharm Sci 2023:85(3) Spl Issue “128-133” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
A total of 110 patients with obstructive sleep apnea hypoventilation syndrome were selected from January 2017 to December 2018, including 76 cases of men and 34 females, aged 40-50 y and according to the apnea hyponea index, patients were classified into 3 groups of moderate to moderate and 5 apnea hyponea index 20 was divided into group A (36 cases), the 40 of 20 to apnea hyponea index is divided into group B (45 cases) and apnea hyponea index the 40 of 20 to 40 is divided into group B (45 cases) and apnea hyponea index to 40 is divided into group C (29 cases). In the same period in the health check-up center to extract 40 cases without obstructive sleep apnea hypopnea syndrome, arrhythmia and other medical history of health check-up objects. 24 h Holter-monitoring and polysomography monitoring of 4 groups of people, observed and recorded heart rate variability indicators for each group, including all standard deviations for sinus cardiac arrest, standard deviation per 5 min sinus cardiac interstitial period, the average root mean square of successive differences of the total sinus intercardial period difference is divided by the number of individuals of the sinus cardiac interstitial period of 50 ms the average root mean square of successive differences of the total sinus intercardial period difference is divided by the number of individuals of the sinus cardiac inner struggle period of 50 ms divided by the percentage of the total sinus cardiac inner struggle period (proportion of NN50), low frequency and high frequency. Standard deviation of all sinus beats, standard deviation of the mean value of sinus, root mean square of successive differences, proportion of NN50, low frequency and high frequency were lower than those in the control group (p<0.05) in patients with obstructive sleep apnea hypopnea syndrome. The proportion of NN50 and high frequency in group C were lower than A and B (p<0.05) and the low frequency was higher than the proportion of NN50 and high frequency in group C were lower than A and B (p<0.05) and the low frequency was higher than group A, group B and control group (p<0.05). Holter-monitoring is a non-invasive test, the price is not high and it can be a regular test for testing the autonomic nervous function in patients with obstructive sleep apnea hypopnea syndrome.
Keywords
Heart rate variability, Holter, autonomic nervous system, obstructive sleep apnea hypopnea syndrome
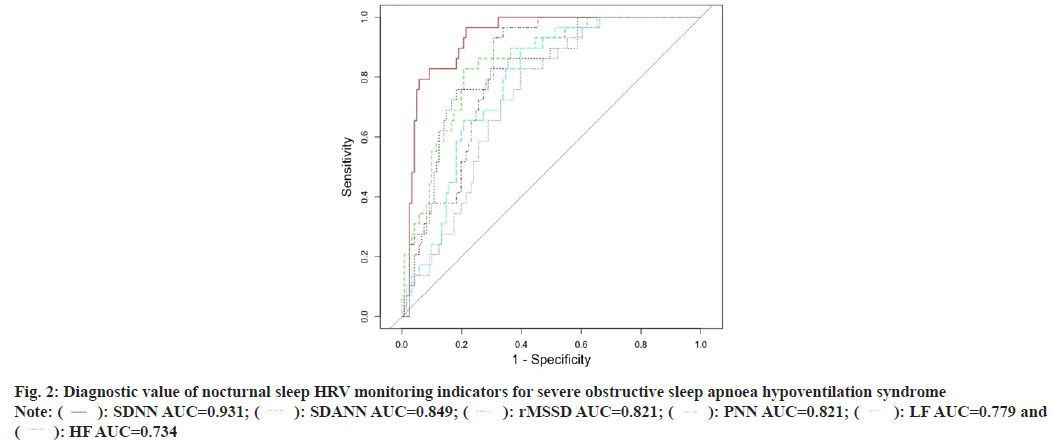
Obstructive Sleep Apnea Hypopnea Syndrome (OSAHS) is characterized by snoring during sleep with apnea and superficial breathing, recurrent nighttime hypoxemia, hypercapnia and sleep architecture disorders, resulting in daytime sleepiness, cardiovascular and cerebrovascular complications and multi-organ damage, which severely affects the quality of life and survival of patients[1]. Some epidemiological studies have found that OSAHS has a high prevalence, especially in older patients and is potentially dangerous, especially in combination with cardiovascular disease, with respiratory sleep-related cardiovascular disease accounting for approximately 0.12 % of deaths from OSAHS in the United States (US) each year[2]. In recent years, studies in China have shown that the prevalence of OSAHS is about 2 %-5 %, while with the progression of the disease can lead to pulmonary hypertension with pulmonary heart disease, hypertension, coronary heart disease and a series of cardiovascular and cerebrovascular diseases, which seriously threaten people’s life and health and must be given attention[3,4]. The aim of this paper is to analyses the changes of Heart Rate Variability (HRV) indexes through ambulatory electrocardiography to provide clinicians with indicators to evaluate the autonomic function of patients with OSAHS and to adjust the treatment plan according to the changes of indexes in time to provide safer and more reasonable treatment for patients, as well as to improve their own treatment methods. A total of 110 patients with obstructive sleep apnea hypoventilation syndrome, including 76 males and 34 females, with an average age between 51.2±3.3 y, who attended our hospital from January 2017 to December 2018 were selected. The patients were divided into three groups according to the number of apnoea plus hypopnoea per hour of sleep (Apnea Hyponea Index (AHI)) 5≤AHI<20 for group A (36 patients), 20≤AHI<40 for group B (45 patients) and AHI≥40 for group C (29 patients). Another 40 normal healthy volunteers (selected from the case pool of our health screening department, without history of OSAHS or arrhythmia, 18 males and 22 females, mean age 48±2.3 y) were selected as the control group. All patients signed an informed consent form and the study was approved by the medical ethics committee of the hospital. Diagnostic criteria for OSAHS refer to the obstructive sleep apnea hypoventilation syndrome diagnostic and treatment guidelines (2011 Revision)[5], with clinical symptoms such as nocturnal snoring with apnea, daytime sleepiness (Epworth Sleepiness Scale (ESS) score ≥9), inattention, upper narrowing and obstruction of any part of the airway, signs of AHI ≥5 times/h. The diagnosis of OSAHS can be confirmed by the presence of one or more OSAHS comorbidities such as cognitive dysfunction, hypertension, coronary artery disease, cerebrovascular disease, diabetes mellitus and insomnia in those with insignificant daytime sleepiness (ESS score <9), AHI ≥10 beats/h or AHI ≥5 beats/h. Exclusion criteria for OSAHS exclusion of atrial fibrillation, atrioventricular block of degree II or greater, sinus atrial block, pathological sinus node syndrome and arrhythmias affecting HRV such as frequent premature beats and pulmonary disease. A 12 lead Electrocardiogram (ECG) recorder from Briggs and Stratton, and the system analysis software were used to record and analyses the data. The skin was first tested with alcohol and then treated with specific sandpaper at the electrode application site to remove foreign bodies from the skin surface and subjects with hairy chests were shaved with a razor blade to reduce ECG interference. The data obtained were processed by the ECG analysis system to obtain data on the various HRV indicators, including the Standard Deviation of all Sinus Beats (SDNN), which mainly reflects the magnitude of sympathetic and vagal tone and is used as an overall indicator to assess the damage and recovery of the autonomic nervous system; the standard deviation of the mean value of sinus beat intervals every 5 min in the whole recording Standard Deviation of the Mean Value of Sinus (SDANN) intervals per 5 min period (SDANN) mainly reflects the slow changes in HRV, i.e. the magnitude of sympathetic tone, including the SDNN Index, which mainly represents the magnitude of short duration sympathetic or vagal tone; root Mean Square of Sinus Interval Difference (rMSSD) reflects the fast changes in HRV, i.e. a sensitive indicator of parasympathetic tone; the number of sinus intervals with a difference of ≥50 ms divided by the number of sinus intervals as a whole percentage (%) of sinus interval difference ≥50 ms divided by the number of sinus intervals. Like rMSSD, Proportion of NN50 (PNN50) reflects fast changes in HRV and is a sensitive indicator of parasympathetic tone[6]. Frequency domain indicators these include High Frequency (HF) and Low Frequency (LF) and the ratio of the two (LF/HF). The statistical software Statistical Package for the Social Sciences (SPSS) 20.0 was used for statistical description and inference. Count data were expressed as frequencies and percentages, measurement data were expressed as means and standard deviations, the Chi-square (χ2) test was used for group comparisons of count data, one-way Analysis of Variance (ANOVA) was used for group comparisons of measurement data, and Least Significance of Difference (LSD) was used for two-way comparisons between groups. LSD was used to compare two groups. Alpha (α)=the area under the Receiver Operating Characteristic (ROC) curve, was used to compare the diagnostic value of each indicator for severe obstructive sleep apnoea hypoventilation syndrome, where the AUC is a value between [0,1] and the closer the value is to 1, the higher the diagnostic predictive value of the indicator. The results of the one-way ANOVA showed that the differences in the 24 h sleep HRV monitoring results were statistically significant in all groups, with SDNN, SDANN, rMSSD, PNN50, LF and HF being lower in groups A, B and C than in the control group, and the differences were statistically significant (p<0.05); in OSAHS patients, the more severe the condition, the lower the SDNN, SDANN rMSSD, PNN50, LF and HF were lower in OSAHS patients with more severe disease (p<0.05) and the differences were statistically significant between the two groups as shown in Table 1. The results of the one-way ANOVA showed that the differences in the results of nocturnal sleep HRV monitoring were statistically significant in all groups, with SDNN, SDANN, rMSSD, PNN50, LF and HF in groups A, B and C being lower than those in the control group, and the differences were statistically significant (p<0.05); in OSAHS patients, the more severe the condition, the lower the SDNN, SDANN, rMSSD, PNN50, LF and HF were lower in OSAHS patients with more severe disease (p<0.05) and the differences were statistically significant between the two groups as shown in Table 2. The area under the ROC curve for each indicator was obtained as follows; the diagnostic value of 24 h HRV monitoring indicators were SDN>SDANN>rMSSD>LF>HF>PNN; the diagnostic value of nighttime HRV monitoring indicators were SDNN>SDANN>PNN>rMSSD>LF>HF as shown in Table 3 and Table 4, fig. 1 and fig. 2. Epidemiological studies in China have found that at least 30 % of hypertensive patients have OSAHS, while about 50 % of OSAHS patients have hypertension in combination, suggesting that OSAHS is a cause of hypertension independent of risk factors for hypertension such as age, smoking and obesity[7]. The current gold standard for the diagnosis of the disease is the overnight Polysomnograph (PSG), but screening for sleep apnoea syndrome using a single indicator of periodic changes in heart rate can be missed, and combining this with heart rate improves the accuracy of screening for OSAHS, particularly in patients with no significant changes in heart rate during apnoea. In recent years, the use of ECG in combination with PSG for primary screening of OSAHS has become increasingly important due to its relative ease of access, low cost and good compliance, and its accuracy is improving, making the use of ECG in patients with OSAHS increasingly popular[8-10]. HRV analysis is a sensitive, noninvasive, quantitative method for detecting the regulation of cardiac vegetative function. It is a method for examining the variability of the heart’s sinus interval and an indicator of sympathetic and vagal tone and its homeostasis[11]. It has been found that HRV can be used to evaluate cardiac autonomic function in patients with acute stroke. A decrease in HRV indicates increased sympathetic tone, which is often associated with serious cardiovascular events and is a valuable predictor of sudden cardiac death and arrhythmias[12,13]. The SDNN reflects the total sympathetic and vagal tone, and is a useful indicator of autonomic deficits. SDANN mainly reflects sympathetic tone and is negatively correlated with sympathetic function[14,15]. rMSSD, PNN50 are indicators of vagal tone and a decrease in this indicates to a certain extent a decrease in vagal excitability. Several studies have found that HF, an index of frequency domain analysis, is mainly indicative of vagal activity, particularly respiratory sinus arrhythmia and the resulting respiratorysynchronous heart rate fluctuations; LF, an efferent nerve of the autonomic nervous system, is influenced by both sympathetic and vagal nerves, with sympathetic nerves playing a major role[16-18]; HRV reflects subtle temporal changes from one cardiac cycle to the next and occurs based on autonomic regulation of heart rate. HRV reflects the subtle temporal variations of each cardiac cycle and is based on the autonomic regulation of heart rate, which is associated with a variety of diseases[19]. In this study, SDNN, SDANN, rMSSD, PNN50, LF and HF were found to be lower in patients in groups A, B and C than in the control group, suggesting that the autonomic function of patients was impaired and the severity was positively correlated with the degree of the condition. The SDNN, SDANN, rMSSD, PNN50 and HF of the patients in groups A, B and C were lower than those of the control group during sleep (p<0.05), the PNN50 and HF of group C were lower than those of groups A and B (p<0.05) and the LF was higher than those of groups A, B and the control group (p<0.05), suggesting that vagal tone decreased at night, and the decrease was more pronounced in groups B and C, while sympathetic nerves enhanced, leading to increased cardiac stress and an increased risk of sudden death, a change that needs to be taken seriously. Dynamic ECG is a method that can continuously record and analyses changes in human cardiac activity for a long period of time and is currently one of the important means of non-invasive cardiac examination in the clinical cardiovascular field, with the characteristics of high efficiency, noninvasive, safety, accuracy and repeatability, the instrument is easy to carry, non-invasive to install, the examination cost is not high, and the cost is reimbursable by medical insurance, it helps to assess the cardiac autonomic function of people suffering from OSAHS and is useful for predicting. It has a preventive significance in predicting the occurrence of cardiac events in patients and its indices have an important guiding role in the treatment and prognosis of patients, and can be used clinically as one of the tests for routine screening of patients with OSAHS.
| Group | SDNN (ms) | SDANN (ms) | rMSSD (ms) | PNN50 | LF | HF |
|---|---|---|---|---|---|---|
| Group A | 108.47±4.55* | 98.55±4.01* | 28.33±1.05* | 3.46±1.74* | 412.36±408.51* | 401.22±387.14* |
| Group B | 92.22±0.74*# | 85.25±0.65*# | 27.41±1.22*# | 2.33±0.47*# | 354.64±312.99*# | 340.84±335.25*# |
| Group C | 65.14±1.33*#& | 51.85±1.24* #& | 9.16±0.74* #& | 2.65±1.24* #& | 326.47±308.56* #& | 320.51±318.94* #& |
| Control | 126.71±4.83 | 121.63±4.52 | 39.48±4.95 | 8.98±1.47* | 524.21±478.53 | 504.95±501.25 |
| F | 39.181 | 39.968 | 26.618 | 228.653 | 30.909 | 22.888 |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Note: *p<0.05 compared to control; #p<0.05 compared to group A and &p<0.05 compared to group B
Table 1: Results of 24 H HRV Monitoring In Patients With OSAHS
| Group | SDNN (ms) | SDANN (ms) | rMSSD (ms) | PNN50 | LF | HF |
|---|---|---|---|---|---|---|
| Group A | 99.21±3.65* | 90.54±2.76* | 29.14±1.21* | 3.78±1.65*# | 454.65±423.27*# | 448.24±438.69*# |
| Group B | 74.57±1.56* | 73.13±1.21* | 24.86±1.01* | 3.01±1.44*# | 435.02±429.15*# | 438.55±421.67*# |
| Group C | 65.23±1.08* | 55.84±0.47* | 10.35±0.89* | 2.41±0.95* | 489.65±457.02*# | 405.36±389.14* |
| Control | 121.48±4.35 | 110.52±4.21 | 36.47±3.98 | 9.04±1.63 | 474.36±428.14 | 466.87±453.24 |
| F | 54.857 | 48.047 | 24.522 | 98.06 | 19.629 | 19.638 |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Note: *p<0.05 comparison with control group and #p<0.05 comparison with group C
Table 2: Nocturnal Sleep HRV Monitoring Results in Patients with OSAHS
| Indicators | Threshold values | AUC | Sensitivity | Specificity |
|---|---|---|---|---|
| SDNN | 84.344 | 0.917 | 0.966 | 0.785 |
| SDANN | 68.446 | 0.89 | 0.759 | 0.917 |
| rMSSD | 25.649 | 0.834 | 0.862 | 0.793 |
| PNN | 3.854 | 0.697 | 1.000 | 0.446 |
| LF | 353.309 | 0.759 | 0.793 | 0.719 |
| HF | 408.401 | 0.736 | 0.966 | 0.463 |
Table 3: Diagnostic Value of 24 H Sleep HRV Monitoring Indicators for Severe Obstructive Sleep Apnoea Hypoventilation Syndrome
| Indicators | Threshold values | AUC | Sensitivity | Specificity |
|---|---|---|---|---|
| SDNN | 79.053 | 0.931 | 0.966 | 0.785 |
| SDANN | 71.081 | 0.849 | 0.828 | 0.793 |
| rMSSD | 22.208 | 0.82 | 0.759 | 0.818 |
| PNN | 4.256 | 0.821 | 0.966 | 0.661 |
| LF | 495.583 | 0.779 | 0.897 | 0.603 |
| HF | 498.76 | 0.734 | 0.828 | 0.603 |
Table 4: Diagnostic Value of Nocturnal Sleep HRV Monitoring Indicators for Severe Obstructive Sleep Apnoea Hypoventilation Syndrome
Conflict of interests:
The authors declared no conflict of interests.
References
- Lin SH, Wu YP. Correlation analysis of sleep breathing monitoring with heart rate variability by ambulatory electrocardiography. J Prac Cardiol 2017;26(4):271-4.
- Zhang N, Zhong N. The relationship between obstructive sleep apnea hypoventilation syndrome and cardiovascular disease. Chin J Tuberculosis Respir Dis 2003;9(26):513.
- Chen Qi. Research progress of obstructive sleep apnea hypoventilation syndrome and related diseases. China Mod Doctor 2017;11(55):165-8.
- He S. Clinical evaluation of left ventricular Tei index in patients with obstructive sleep apnea syndrome. Hebei Med 2017;39(18):2830-2.
- Sleep apnea disorders group of the Chinese medical association respiratory diseases branch. Guidelines for the diagnosis and treatment of obstructive sleep apnea hypoventilation syndrome (2011 revised edition). Chin J Tuberculosis Respir Dis 2012;35(1):9-12.
- Chinese journal of cardiovascular diseases editorial committee task force on heart rate variability countermeasures. Recommendations for the clinical application of heart rate variability monitoring. Chin J Cardiovasc Dis 1998;26(4):252-5.
- Lanza GA, Cianflone D, Rebuzzi AG, Angeloni G, Sestito A, Ciriello G, et al. Prognostic value of ventricular arrhythmias and heart rate variability in patients with unstable angina. Heart 2006;92(8):1055-63.
[Crossref] [Google Scholar] [PubMed]
- Liu FG, Zhang XZ. The relationship between obstructive sleep apnea hypoventilation syndrome and cardiovascular disease. Chin J Tuberculosis Respir Dis 2003;9(26):515.
- Liu X, Chen S, Fang Y. Correlation study of heart rate variability and heart rate deceleration force in patients with OSAHS. J Integr Med Cardiovasc Dis 2017;15(22):2801-4.
- Lin J, Can C, Liu, Mei Y. Advances in primary screening of sleep apnea syndrome by ambulatory electrocardiography. Chin Med J 2017;97(1):76-8.
- Shang Y, Yang N, Zhu Y, Song X. Application of artificial neural network in HRV analysis. Comput Technol Dev 2018;27(9):141-9.
- Li X, An L, Yao S. Clinical value of dynamic electrocardiographic heart rate variability index to evaluate cardiac autonomic function in acute stroke patients. Chin J Gerontol 2017;37(5):1145-6.
- Xiong M. Research on the application of heart rate variability in sleep and biofeedback systems. Univ Chin Acad Sci 2014:1-87.
- Katz-Leurer M, Zohar N, Boum A, Keren O. Monitoring changes in heart rate, as an indicator of the cardiovascular autonomic nervous function, among patients at the sub-acute phase post-brain damage during a physiotherapy session: A preliminary investigation. Brain Inj 2014;28(1):127-31.
[Crossref] [Google Scholar] [PubMed]
- Li J. Study on the correlation between circadian rhythm and heart rate variability of blood pressure and TCM evidence in elderly hypertension. China Acad Tradit Chin Med 2014:1-60.
- Zhang Y, Zhou Y. Heart rate variability in patients with coronary heart disease with different anxiety and/or depressive disorders and the effect of sertraline application. Guangdong Med 2017;38(14):2219-23.
- Zhang Y, Lin P, Wang N. Research progress on factors influencing heart rate variability in patients with coronary artery disease. Mod Clin Nurs 2019;18(3):64-8.
- Zhao LQ, Leng YQ, Lu JJ. Characterization of heart rate variability in patients with coronary artery disease and coronary artery disease combined with hypertension. Chin J Clin Phys 2019;47(3):287-9.
- Zhang QY, Tang GM. Heart rate variability in ventricular arrhythmias in coronary artery disease. Cardiol Circ 2019;38(1):52-60.
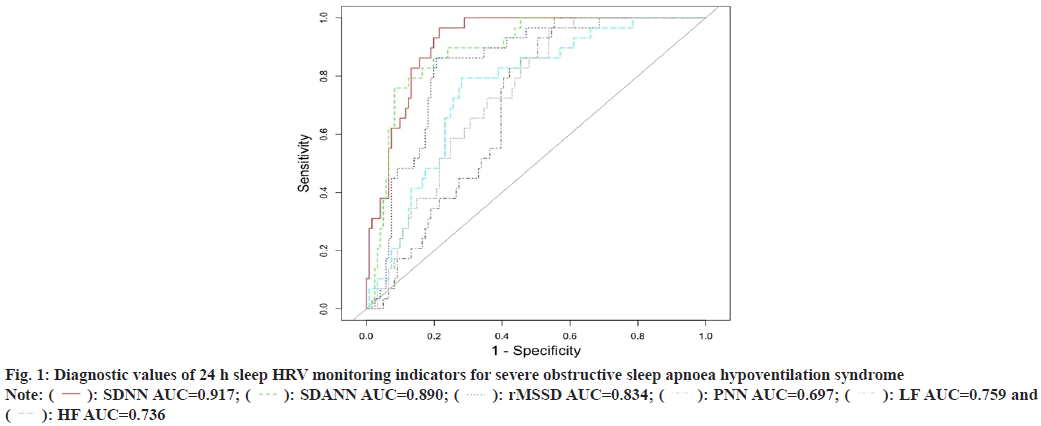
 : SDNN AUC=0.917;
: SDNN AUC=0.917;  : SDANN AUC=0.890;
: SDANN AUC=0.890;  : rMSSD AUC=0.834;
: rMSSD AUC=0.834;  : PNN AUC=0.697;
: PNN AUC=0.697;  : LF AUC=0.759 and
: LF AUC=0.759 and  : HF AUC=0.736
: HF AUC=0.736