- *Corresponding Author:
- J. J. Kirubakaran
Department of Pharmacy Practice, Vikas Institute of Pharmaceutical Sciences, Rajahmundry, Andhra Pradesh 533103, India
E-mail: john.mpharm@gmail.com
| Date of Received | 24 July 2021 |
| Date of Revision | 29 March 2022 |
| Date of Acceptance | 13 May 2022 |
| Indian J Pharm Sci 2022;84(3):598-603 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
The exact frequency of poisoning is unclear, although it is the most prevalent cause of emergency room visits. It is a critical domain for emergency medicine practitioners, who are the first to see people who have been exposed to toxic substances. As a result, they must be aware of how to manage the poisoning. So, a survey was designed to identify their knowledge on antidotes for common poisonings, along with queries on antidotes and decontamination measures available within each hospital. A total of 232 people replied to the poll (77.33 % response rate). In general, data of antidotes are not found higher but differed based upon the antidote. Physicians who work in tertiary hospitals and more bedded hospitals appreciably served well. Merely 42.24 % of the 16 antidotes are accessible at each reporting hospitals on average; 18.1 % could acquire them from adjacent hospitals and 20.26 % could acquire them from a local distributor. Only 19.4 % of people can acquire an antidote within 2 h. The most common decontamination therapy is gastric lavage, while extracorporeal decontamination procedures 42.24 % and 36.64 % respectively are available in varying degrees. Knowledge of specific antidotes was shown to be connected to the size, type and location of the hospital in the East Godavari district, rather than individual physician characteristics. In roughly half of the hospitals assessed, significant antidotes are still unavailable or available within 2 h, even though all key acute decontamination therapies and procedures appear to be widely used.
Keywords
Antidotes, emergency department, extracorporeal decontamination, poisoning
The true incidence of poisoning is unknown, but it is the most common cause of Emergency Department (ED) visits. This creates the challenge for the emergency medicine expertise. It is an essential domain for the emergency medicine practitioners, who are the first line people to see the people who are exposed to the toxic substances. So, its mandatory for them to know how to manage the poisoning[1]. A report from American Association of Poison Control Centers (AAPCC) and National Poison Data System (NPDS) states that above 2.1 million human poison incidences and almost 2500 poisoning-linked deaths in 2013 (7.9 deaths/million). The pattern of suicide differs in various population and culture[2]. India stands at 10th position in the world rank with an average suicidal rate of 9.74/lakh population[3]. The most common mode of suicide is by using agrochemicals, it also depends on the availability, motivation and intent[4]. In India 15 suicides took place every 1 h during the year 2015 and more than 1 lakh persons (133 623) have committed suicide[5]. According to National Crime Records Bureau, Ministry of Home Affairs Government of India, 2018 about 134 516 people committee suicide in India in the year 2018 which is 10.2 incidence of suicides per one lakh (100 000) of population[6].
Pre determining the clinical indices as earlier can help in providing appropriate supportive care which will favour in the patient outcome[7]. In any ED the first review is done using Airway, Breathing, Circulation, Disability/Dextrose (ABCD), assessment. It’s mostly helpful in the assessment of poisoning[8]. The main issue in assessment is “how much the ED physician knows about the antidote?” In India less than 1 % of the hospitals have drug information centres[9]. There are very limited studies which evaluate the knowledge of physicians for antidotes in poisoning and the availability of the necessary resources to treat poisoning cases.
Materials and Methods
We personally delivered a written survey to the physicians in East Godavari district hospitals in Andhra Pradesh, India. The hospital names and addresses, hospital level, hospital characteristics including bed capacity, teaching hospital or not and its location category (urban/rural) were abstracted from the system. The survey had been accomplished by one of the physicians and collected personally. They were entailed to deliver their basic personal records and specialty, experience, seniority, the way they attained their toxicology info and the place they are occupied in. To intensify the retort percentage, researchers communicated relevant staff by telephone, beforehand and afterward the survey.
The survey was created with instructions for the proposal and handling of self-administered surveys for clinicians[10]. Subsequently when literature review had been inclusive, a local expert panel group aided in item generation, pretesting and reduction. A pilot study with 10 hospitals to authorize ease of use, comprehensibility and precise description were structured. The survey exercised a fill in the blank structure and comprised of three parts. The first part survey contains question based on info of antidotes to 16 kinds of universally perceived poisonings, encompassing two kinds of pesticides: Organophosphates and rodenticides; two classes of toxins: Datura and snake bites; seven chemicals: Carbon monoxide, methanol, fluoride, cyanide, nitrite, iron and lead; five medicines: Acetaminophen, opiates, tricyclic antidepressants, benzodiazepines and digoxin. Each time they bestowed the right antidote reply to the poisoning, they got 1 point to their total score (with a peak score of 16). At the end of questionnaire, the answerers were needed to list the top 3 substances used for suicide which they confront in their ED very recurrently. The second part of the survey is about the availability of antidotes in their ED of numerous antidotes and if unobtainable, they can get them from their local distributors or any other neighbouring hospital and how much time they think it would take to procure. The third part of the study examined the types of treatment methods offered in the hospital, encompassing cathartic, whole bowel irrigation, lavage, charcoal, haemodialysis, hemofiltration and/or hemoperfusion.
Results and Discussion
The questionnaire was distributed to 300 physicians and a total of 232 filled questionnaires was received, in this 24.14 % was from the age group of 36-45 y of age, followed by 46-55 y, 122.84 %; 56-64 y, 20.69 %; 26-35 y, 15.09 %; 66-75 y, 14.66 % and >75 y are 2.59 %. The survey was answered by postgraduates 62.50 %, general physician 36.21 % have also contributed for this study. The score-based analysis has been shown in Table 1.
| Category | Result | Total score (out of 16) | p |
|---|---|---|---|
| Gender | 0.117 | ||
| Male | 155 | 11.48±3.16 | |
| Female | 77 | 11.05±3.50 | |
| Type of hospital | 0.091 | ||
| Teaching hospital | 94 | 12.39±3.12 | |
| Tertiary care hospital | 65 | 11.26±3.26 | |
| Private clinics | 50 | 9.80±2.81 | |
| Rural hospital | 23 | 10.61±3.5 | |
| Bed capacity | 0.007 | ||
| <150 | 81 | 12.57±3 | |
| 150-300 | 32 | 10.94±3.44 | |
| 300-500 | 14 | 11.43±3.06 | |
| 500-1000 | 11 | 9.45±1.51 | |
| >1000 | 94 | 10.63±3.33 | |
| Emergency speciality | <0.001 | ||
| Yes | 55 | 14.95±0.97 | |
| No | 177 | 10.22±2.91 | |
| Location of the hospital | 0.097 | ||
| Urban | 141 | 11.13±3.35 | |
| Rural | 91 | 11.67±3.14 | |
| Experience of physicians | <0.001 | ||
| <5 | 15 | 14.87±0.92 | |
| 6-10 | 40 | 13.55±2.56 | |
| 11-15 | 28 | 12.39±3.44 | |
| 16-20 | 18 | 12.56±2.62 | |
| 21-25 | 36 | 9.64±2.86 | |
| 26-30 | 21 | 11.19±3.63 | |
| 31-35 | 22 | 10.32±2.9 | |
| 36-40 | 18 | 9.94±2.9 | |
| >40 | 34 | 8.97±1.85 |
Table 1: Responders and their corresponding scores
The participants of the survey who work in teaching hospitals were 40.52 %, tertiary care hospitals are 28.02 % each and hospitals which are in rural area are 9.91 %. From the analysed data, many physicians are from <150 bedded hospitals 34.91 %, 13.79 % are from 150- 300 bedded hospitals, 6.03 % from 300-500 bedded hospitals. One hospital which lies under 500-1000 beds where 4.74 % doctors participated. Teaching hospital physicians 40.52 % involved in the survey which had a capacity of >1000 beds. It was identified that 60.78 % are from urban located hospitals and other 39.22 % are from rural settings. Out of 232 physicians who participated in the study, 23.71 % have the specialized in ED, all others 76.29 % are from other specialities.
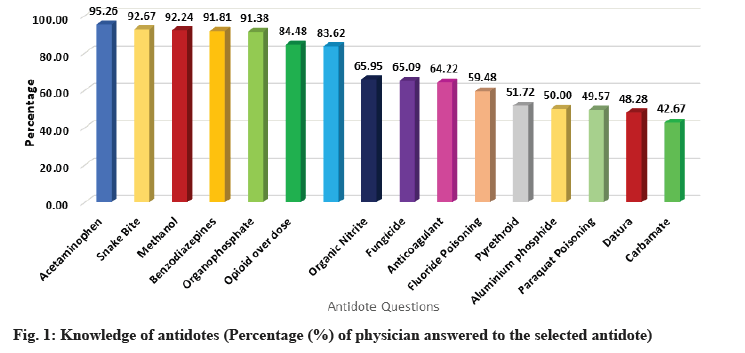
It is identified that the physicians have a better knowledge in treating acetaminophen 95.26 %, benzodiazepines 91.81 and opiates 84.48 % when compared with other medications like tricyclic antidepressants 83.62 %. Only 42.67 % of them have correctly identified the antidote for carbamate 28.45 %.
The physicians who participated in the study have a good knowledge in treating organophosphate poisoning 91.38 % and snake bite 92.67 %, methanol’s antidote was identified by 92.24 % of the physicians. For the other questions only <40 % of them has correctly answered. A bar diagram shows the score obtained by 232 physicians in fig. 1.
In this we see that organophosphates are leading with 80.6 % followed by tricyclic antidepressants 85.34 %. This pattern was followed in our study also. The notable and other poisoning is acetaminophen 43.53 %, snakebite 48.71 % and herbicide or plant poisons 40.95 %.
The decontamination procedures which are readily available in the hospital where the participated physicians are working are listed below. Gastric lavage 92.76 %, activated cathartic 75.43 %, charcoal 62.93 % and whole bowel irrigation 41.81 %.
This result illustrates closely the accessibility of extracorporeal decontamination procedures in the hospital where the participated physicians are working are listed below; haemodialysis 42.24 %, hemofiltration 36.64 %, hemoperfusion 34.48 % and not available 54.74 %.
This question is placed in the questionnaire to know the source used by the physicians to treat the poisoned patient when they are unaware about the antidote to be used. Under such circumstances what will be their preferred mode for searching or to improve the knowledge. 49.14 % of the physicians preferred to check the old literatures, 21.98 % have answered as they have enough knowledge from their medical school. 16.38 % say that they are interested to continue learning and 12.5 % takes helps from the experts or the seniors.
The availability of antidotes is very essential but only 42.24 % doctors said that it is readily available. 18.1 % can avail from the nearby hospitals and 20.26 % can buy from local distributors, this hospital has a close access to the distributors. The hospitals in rural setup 19.4 % can avail the antidotes in 2 h. The correlation between availability of antidote with location of hospital and type of hospital shows statistically significant (Table 2).
|
|
Location of the hospital | Type of hospital | ||||
|---|---|---|---|---|---|---|
| Availability of antidote | Urban | Rural | Teaching hospital | Tertiary care hospital | Private clinics | Rural hospital |
| Readily available | 23.28 | 18.97a | 20.26 | 14.66 | 3.88 | 3.45b |
| From nearby hospitals | 9.48 | 8.62a | 6.9 | 5.6 | 4.31 | 1.29b |
| Local distributors | 12.07 | 8.19a | 8.62 | 3.88 | 6.03 | 1.72b |
| Antidotes in 2 h | 15.95 | 3.45a | 4.74 | 3.88 | 7.33 | 3.45b |
Note: ap<0.01: Rural compared to urban and bp<0.01: Non-tertiary hospitals compared to tertiary hospitals
Table 2: Availability of the antidotes
The foremost outcomes of this investigation were presented below: Organophosphates, tricyclic antidepressants and snakebite were the top three primary kinds of poisoning documented in our survey. Antidote knowledge was not high, dependent on the antidote usage and the hospital of the medical practitioner. There were insufficient antidotes available at responding hospitals. Gastric lavage was the utmost extensively expended decontamination process and in comparison, to the others in Asia there are no inferior extracorporeal decontamination procedures[11,12].
Antidotes must be properly understood to treat intoxicated patients successfully. Antidotes, specialized decontamination procedures and extracorporeal decontamination techniques, on the other hand, are all critical to properly treat patients. In India, there are currently no widely accepted precise criteria that determine an ED’s preparation for the care of acute hazardous exposures and poisonings[13].
This investigation established that, on the whole, physicians who participated in the survey had specific experience upon the usage of numerous antidotes, depending on the antidote and their expertise, and their expertise differed. Organophosphates, sedatives and snakebite were the most common forms of poisonings by many responding physicians in this poll, albeit the results may be subjected to personal bias.
Organophosphates get the highest score with 80.60 % of respondents naming them as one of the top three contaminants. This finding is consistent with the findings from India, Sri Lanka and a few African nations[13-16]. According to official data from 2005, self-poisoning with pesticides accounted for 19.6 % of India’s suicides[17]. According to Sri Lankan national mortality figures from the same year, 54 % of suicides were caused by pesticide intake[18]. Taking something toxic close at hand is the simplest method to commit suicide. Organophosphate pesticides were the topmost repeatedly consumed pesticide in rural regions and sedatives were frequently utilised in urban zones, resulting in widespread availability.
Antidotes are important in the treatment of poisoned or overdosed people. Totally, antidotes necessitated promptly (within 30 min) ought to be stored at all hospitals, according to World Health Organization (WHO) guidelines for poison control centers[19]. Opioids, tricyclic antidepressants and acetaminophen are three of the upmost four single categories of poisonings linked with the highest sum of fatalities in the United States and all three have antidotes[20]. Similarly, there are antidotes for all three of the most common poisonings in our study. The proportion of physicians who know the right antidotes for organophosphates, tricyclic antidepressants and snakebite are 91.38 %, 82.76 % and 90.95 %, respectively according to our findings.
When we analysed the survey’s overall findings, it was discovered that the mediocre test points were 10 out of 16 (62.5 %) right. The outcomes of the respondent’s tests did not differ substantially contingent on their medical speciality, years of practice or how they learned toxicology. However, it varied greatly across tertiary and non-tertiary hospital physicians, as well as across hospitals with varying bed counts. Our subsequent statistical research revealed that the sum of hospital beds did not appear to be an autonomous contributing factor. These findings imply that in the East Godavari area, a physician’s toxicological expertise is influenced more by the type of hospital in which they work, than by their personal history.
Individuals in Indians go to the largest hospital first if they have a condition, resulting in patients being crammed into bigger hospitals and departing only a limited patients in smaller hospitals, according to published studies[21]. The findings of this investigation back up this popular belief. Given the gap in patient numbers, one plausible source of this imbalance might be a "self-fulfilling prophesy". Physicians who work in larger hospitals will have greater expertise treating a wider spectrum of poisonings than those at smaller institutions.
Physicians in both rural and urban hospitals had no remarkable modifications in their over-all ratings when compared by hospital location. Physicians in urban hospitals outperformed when related to the physicians in rural areas on only three of the 16 antidote questions. Similarly, there were no substantial variances in total points between physicians at teaching hospitals and non-teaching hospitals. Physicians at teaching hospitals fared better on just 5 of the 16 antidote questions.
In our poll, physicians of varying seniority fared substantially differently on 7 out of 16 antidote items. Surprisingly, the groups with the best results were not usually those with the topmost seniority (i.e. having more than 10 y of experience), although those having “only” 3-5 y or 5-10 y of work experience. This might be since emergency medicine was rationally a new profession in India, having only a 20 y history. East Godavari’s toxicological development is considerably slow. Most emergency medicine doctors are former internal medicine doctors with only a rudimentary understanding of emergency medicine. Only in the last 10 y there has been formal emergency medical training. Finally, there is currently no regular clinical toxicological training for emergency medicine trainees in East Godavari.
Is it important how physicians acquire toxicological knowledge? Only 5 out of 16 antidote questions exhibited significant differences in performance amongst physicians with different means of obtaining knowledge, according to our findings. Aside from physician knowledge, the antidote stocking status at the ED was also questioned in 3 out of 5 of the five physicians who received their toxicological expertise from reading the literature. As we had expected, the results were embarrassingly dismal[13]. Only 42.24 % of the needed antidotes were accessible in all the hospitals assessed. Furthermore, only 18.1 % could obtain antidotes from neighbouring hospitals and only 20.26 % from local wholesalers. Only 19.4 % can receive a required antidote within 2 h, even if they have access to a local supply. Because organophosphate poisoning is so prevalent, the antidotes for organophosphate poisoning, pralidoxime and atropine were easily obtainable at all the reporting hospitals. In rural locations and nontertiary hospitals, the stocking situation is significantly worse. Some antidotes ought to be accessible for instant dispensation upon a patient’s entry, which necessitates provision in the ED at many hospitals; other antidotes must be obtainable within 60 min and could be supplied in the hospital pharmacy if swift distribution to the ED is ensured.
Decontamination techniques might transmute a possibly life-threatening intoxication into a lessthreatening condition when a poisoned patient gets to the emergency room. Aside from irrigation, food and fresh air, the most used procedures were gastric lavage, activated charcoal, cathartics, emetics and whole bowel irrigation. According to our findings, 92.76 % can perform gastric lavage, 75.43 % can perform cathartics, 62.93 % have charcoal and 41.81 % might perform whole bowel irrigation. In the United States, activated charcoal is the utmost common decontamination method, pursued by cathartics, gastric lavage and whole bowel irrigation[22]. Nevertheless, according to a finding from Palestine[19], gastric lavage appears to be the most common decontamination procedure in India[23].
Extracorporeal decontamination treatments for instance hemoperfusion and hemodialysis might be required in several cases of acute poisoning and our data revealed that 36.64 %-42.24 % of respondents have hemodialysis and hemofiltration accessible, and 34.48 % can perform hemoperfusion for patients. However, 54.74 % of them did not have access to extracorporeal procedures. These figures are lower than those from Malaysia[11] and Palestine[19].
As we mentioned at the beginning, approximately 33.77 % of doctors did not complete the survey, with non-responders being further communal in smaller, rural hospitals, which presented littler knowledge in this assessment and registered fewer antidotes, unique decontamination techniques and extracorporeal decontamination procedures are available. As a result, the real condition might be far poorer than what had been discovered.
In conclusion, clinically serious poisonings are common in East Godavari. The size, kind and location of the hospital in East Godavari had a stronger correlation with antidote knowledge than individual physician characteristics. In the hospitals assessed, significant antidotes are still unavailable or available within 2 h, in addition even all key acute decontamination therapies and procedures appear to be unavailable. More antidotes should be stored and physicians working in EDs in the East Godavari area should get more targeted education regarding antidotes to common poisons.
Acknowledgements:
Authors would like to acknowledge Principal and authorities of Vikas Institute of Pharmaceutical Sciences and Godavari Institute of Engineering and Technology (GIET) School of Pharmacy, Rajahmundry, Andhra Pradesh.
Conflict of interests:
The authors declared no conflict of interest.
References
- Liu Y, Zhu H, Walline J, Wang M, Xu Q, Li Y, et al. The mastery of antidotes. Hum Exp Toxicol 2016;35(5):462-71.
[Crossref] [Google Scholar] [PubMed]
- Kirubakaran JJ, Jena SK, Rao MB, Dhanaraju MD. A study on pattern and outcome of poisoning cases in a tertiary care hospital in Andhra Pradesh, India. Indian J Public Health Res Dev 2019;10(8):575-80.
- Kanchan T, Menezes RG. Suicidal poisoning in Southern India: Gender differences. J Forensic Leg Med 2008;15(1):7-14.
[Crossref] [Google Scholar] [PubMed]
- Kirubakaran JJ, Rao MB, Dhanaraju MD. A study of treatment pattern on envenom in two tertiary care teaching hospital in South India. Int J Pharm Res 2019;11(1):131-8.
- National Crimes Record Bureau. Accidents in India 2015-Statistics. Ministry of Home Affairs, Government of India, New Delhi; 2015. p. 1-20.
- National Crimes Record Bureau. Accidental deaths and suicides in India 2018. Ministry of Home Affairs, Government of India, New Delhi; 2018. p. 1-277.
- Churi S, Ramesh M, Bhakta K, Chris J. Prospective assessment of patterns, severity and clinical outcome of Indian poisoning incidents. Chem Pharm Bull 2012;60(7):859-64.
[Crossref] [Google Scholar] [PubMed]
- Kirubakaran JJ, Dhanaraju MD. “Toxidrome” A Review. Saudi J Med Pharm Sci 2019;5(3):206-12.
- Sundaram R, Ur R, Pulari V. Poison information resources: Its role in prevention and management of poisoning. Am J PharmTech Res 2014;4(5):1-11.
- Burns KE, Duffett M, Kho ME, Meade MO, Adhikari NK, Sinuff T, et al. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ 2008;179(3):245-52.
[Crossref] [Google Scholar] [PubMed]
- Al-Sohaim SI, Awang R, Zyoud SE, Rashid SM, Hashim S. Evaluate the impact of hospital types on the availability of antidotes for the management of acute toxic exposures and poisonings in Malaysia. Hum Exp Toxicol 2012;31(3):274-81.
[Crossref] [Google Scholar] [PubMed]
- Gunnell D, Eddleston M. Suicide by intentional ingestion of pesticides: A continuing tragedy in developing countries. Int J Epidemiol 2003;32(6):902-9.
- Blanchard J, Feltes M, Kim JY, Pousson A, Douglass K. Experience of Indian emergency physicians in management of acute poisonings. Toxicol Commun 2019;3(1):54-60.
- Kinyanda E, Hjelmeland H, Musisi S. Deliberate self-harm as seen in Kampala, Uganda. Soc Psychiatry Psychiatr Epidemiol 2004;39(4):318-25.
[Crossref] [Google Scholar] [PubMed]
- Abebe M. Organophosphate pesticide poisoning in 50 Ethiopian patients. Ethiop Med J 1991;29(3):109-18.
[Google Scholar] [PubMed]
- Eddleston M, Karalliedde L, Buckley N, Fernando R, Hutchinson G, Isbister G, et al. Pesticide poisoning in the developing world-a minimum pesticides list. Lancet 2002;360(9340):1163-7.
[Crossref] [Google Scholar] [PubMed]
- National Crimes Record Bureau. Suicides in India. Ministry of Home Affairs, Government of India, New Delhi; 2015.
- van Der Hoek W, Konradsen F, Athukorala K, Wanigadewa T. Pesticide poisoning: A major health problem in Sri Lanka. Soc Sci Med 1998;46(4):495-504.
[Crossref] [Google Scholar] [PubMed]
- Zyoud SE, Al-Jabi SW, Bali YI, Al-Sayed AM, Sweileh WM, Awang R. Availability of treatment resources for the management of acute toxic exposures and poisonings in emergency departments among various types of hospitals in Palestine: A cross-sectional study. Scand J Trauma Resusc Emerg Med 2014;22(1):1-9.
[Crossref] [Google Scholar] [PubMed]
- Mowry JB, Spyker DA, Cantilena Jr LR, McMillan N, Ford M. 2013 annual report of the American association of poison control centers’ National poison data system (NPDS): 31st annual report. Clin Toxicol 2014;52(10):1032-283.
[Crossref] [Google Scholar] [PubMed]
- Chauhan C. Most Indians prefer private healthcare services over govt hospitals. Hindustan Times; 2015.
- Lavergne V, Nolin TD, Hoffman RS, Roberts D, Gosselin S, Goldfarb DS, et al. The EXTRIP (extracorporeal treatments in poisoning) workgroup: Guideline methodology. Clin Toxicol 2012;50(5):403-13.
[Crossref] [Google Scholar] [PubMed]
- Chandran J, Krishna B. Initial management of poisoned patient. Indian J Crit Care Med 2019;23(4):234.
[Crossref] [Google Scholar] [PubMed]