- *Corresponding Author:
- Zhou Yuanzhong
School of Public Health, Zunyi Medical University, Zunyi, Guizhou 563000, China
E-mail: zhouyuanzhongabc@sina.com
| Date of Received | 07 December 2024 |
| Date of Revision | 20 February 2025 |
| Date of Accepted | 30 April 2025 |
| Indian J Pharm Sci 2025;87(2):66-72 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To evaluate the impact of a novel surgical technique involving the use of carboprost tromethamine suppositories, in conjunction with folding and suturing the lower uterine segment at the site of a previous cesarean section scar, on the incidence of early postoperative scar defects in subsequent cesarean sections. Between March 2019 and June 2022, 133 patients who received the intervention formed the study group, while a control group of 130 patients received standard care. Both cohorts underwent cesarean section via the transverse incision of the lower uterine segment. The study group additionally received carboprost tromethamine suppositories postoperatively. Data on maternal demographics, operative details, and postoperative outcomes were collected and followed up for 6 to 12 mo. Statistical analysis was performed using statistical package for the social sciences 18.0, with a p value of less than 0.05 indicating significance. The study group demonstrated no significant differences from the control group in maternal age, gestational age, delivery time, body mass index, or new-born birth weight. Operative time was modestly extended in the study group due to the intervention. Postoperatively, there were no significant differences in intraoperative blood loss, intestinal exhaust time, hospital stay duration, or postoperative lochia bleeding. The study group exhibited a reduced rate of abnormal vaginal bleeding (8.27 % vs. 18.46 %) and a lower incidence of diverticulum formation (3.01 % vs. 11.54 %). Notably, the thickness of the lower uterine muscle layer was significantly greater in the study group at both 42 d and 6 mo post-surgery, with no cases of diverticulum formation observed at 6 mo in the study group, compared to 5.50 % in the control group. The integration of carboprost tromethamine suppositories with the surgical technique of folding and suturing during a second cesarean section significantly lowered the rate of scar diverticulum formation and enhanced patient outcomes. This approach presents a promising advancement in the prevention of postcesarean section complications, warranting further investigation and potential clinical adoption.
Keywords
Folding stitching, cesarean section, uterine scar, pharmaceutical intervention, prophylactic antibiotics, anti-inflammatory drugs, clinical application, carboprost tromethamine suppositories
Cesarean section is a vital delivery method that significantly reduces maternal and neonatal mortality rates. It mitigates the adverse effects of certain factors during natural childbirth and alleviates the pain associated with labor, thereby smoothing the delivery process and enhancing the birthing experience for mothers[1]. However, as an invasive surgical procedure, cesarean section can cause substantial harm to the mother and is susceptible to postpartum complications[2]. The uterus, post cesarean section or myomectomy, becomes a scarred organ. Pregnant women with a scarred uterus are at an increased risk of uterine rupture, abnormal placentation, and placenta previa due to the compromised contractility and blood supply of the thin tissue, posing a serious threat to the life safety of both mother and child[3]. The conventional suturing method for a scarred uterus involves the removal of some thin tissue followed by continued suturing, which is prone to complications such as postpartum hemorrhage and impaired wound healing. In contrast, the continuous longitudinal folding suture technique for the lower uterine segment is straightforward to perform and beneficial in reducing intraoperative bleeding, poor wound healing, and infection, showing promise for clinical application.
Peng [4] conducted a retrospective analysis of the efficacy of hysteroscopy combined with laparoscopic surgery in 24 patients with Cesarean Scar Diverticulum (CSD), revealing that both the "folding suture method" and the "muscle flap filling suture method" are effective, with no significant difference in improving menstrual patterns, uterine thickness, and overall efficacy, indicating both are safe and effective for CSD repair. Donnez O posits that with the rising cesarean section rates, CSD should be considered in cases presenting with symptoms like spotting and dysmenorrhea. CSD can be visualized using various tools such as hysterosalpingography and transvaginal ultrasound, emphasizing the importance of understanding the status of cesarean scars for CSD diagnosis. Kulshrestha et al.[5] describe the uterine niche as a complication arising from cesarean section due to defects in tissue healing, leading to deficiencies in the uterine muscle layer. The symptoms are varied, encompassing abnormal bleeding, spotting, and infertility. A range of diagnostic methods exists, and prevention hinges on proper surgical techniques. Treatment options span medical or surgical correction, with management needing to consider risk factors comprehensively. Shen et al. suggest that the incidence of postoperative vaginal bleeding abnormalities and the severity of diverticulum formation are lower with folding combined suturing compared to conventional surgery, demonstrating its potential to significantly reduce the occurrence or severity of postcesarean section diverticulum[6].
The presence of Postcesarean Section Diverticulum (PCSD) was first identified in 1995 in patients who had undergone cesarean section, with its existence linked to abnormal vaginal bleeding[7]. Tsuji et al.[8] believe the incidence rate correlates with the number of cesarean sections, involving pathological changes such as fibrosis and adenomyosis, impacting fertility. While laparoscopy, hysteroscopy, and transvaginal surgery are effective treatment methods, treatment strategies lack standardization, and a unified definition is necessary for future in-depth research into the etiology, pathology, and optimization of treatment strategies for CSD. Shi et al.[9] identify menstrual irregularities, the number of cesarean sections, and uterine location as independent risk factors for the formation of uterine scar diverticulum. Patients with a posterior uterus and a history of multiple cesarean sections are more likely to develop diverticula, with the depth of the diverticula positively correlating with menstrual irregularities, aiding in the prediction and intervention of uterine diverticulum occurrence.
This study aims to assess the impact of folding and suturing the lower uterine segment at the site of the original cesarean section scar on the formation of PCSD during a second cesarean section. A total of 263 women were selected for the study, with 133 undergoing the folding and suturing procedure for the lower uterine segment, forming the study group. A control group of 130 women received routine surgery. The continuous folding and suturing technique applied during cesarean section for women with a scarred uterus can significantly reduce maternal harm, decrease the formation of scar diverticulum, and diminish postpartum complications such as bleeding, incision infection, and postpartum infection, thereby improving prognosis.
Materials and Methods
Study participants and groups:
We conducted a study at our institution from March 2019 to June 2022, enrolling women who were undergoing their second cesarean section and had provided informed consent[10]. Eligible participants exhibited regular menstrual cycles prior to the current pregnancy, had a history of a transverse incision during their first cesarean section, and were undergoing a repeat procedure. Exclusions applied to women under 18 or over 50 y of age, those with a history of massive hemorrhage, chronic illnesses, mental disorders, an inability to cooperate, or endometrial and cervical issues. The control group comprised 130 women enrolled from March 2019 to December 2020, while the study group included 133 women enrolled from January 2022 to June 2022. The study protocol was approved by our hospital's ethics committee.
Surgical methods:
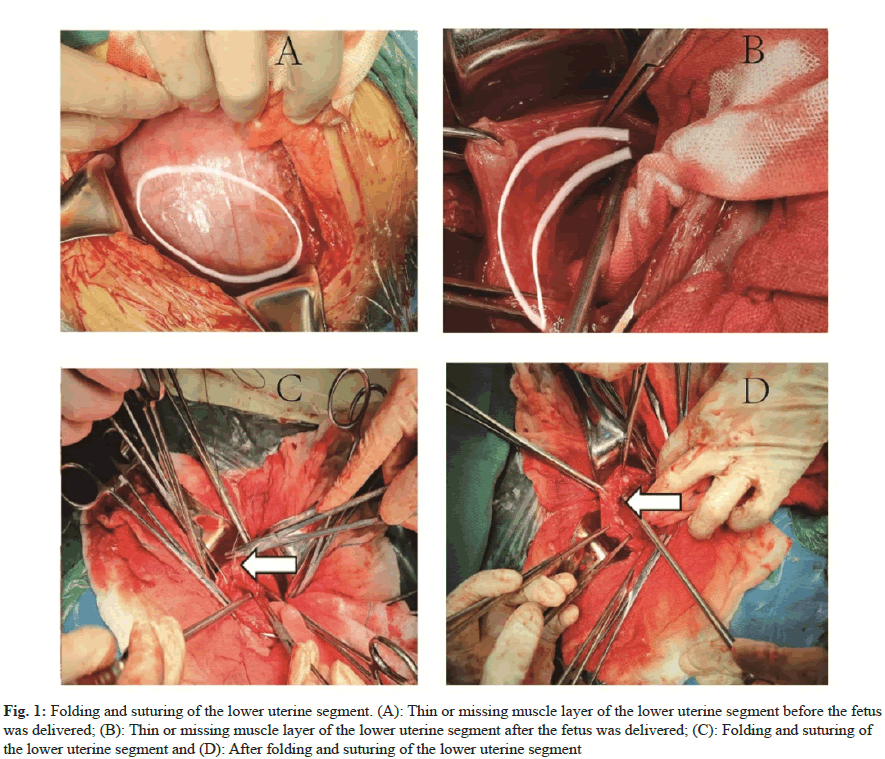
Both study and control groups underwent cesarean section via a transverse incision of the lower uterine segment. In the study group, the incision was strategically placed 1.0-2.0 cm above the previous scar to circumvent the weakened area. This approach facilitated the extraction of the fetus and placenta (fig. 1A). The study group also received a novel intervention: An exploratory examination of the muscle layer and a subsequent folding suture technique (fig. 1B-fig. 1D), aimed at reinforcing the uterine wall and re-establishing its anatomy. This method involved a meticulous two-layer suturing process. In contrast, the control group’s uterine incisions were closed with a standard double-layer continuous suture, ensuring optimal tension to prevent blood supply compromise. Both groups were under the care of senior attending physicians and received spinal anaesthesia. The only procedural difference was the application of the folding suture technique in the study group.
Fig. 1: Folding and suturing of the lower uterine segment. (A): Thin or missing muscle layer of the lower uterine segment before the fetus was delivered; (B): Thin or missing muscle layer of the lower uterine segment after the fetus was delivered; (C): Folding and suturing of the lower uterine segment and (D): After folding and suturing of the lower uterine segment
Observational indicators:
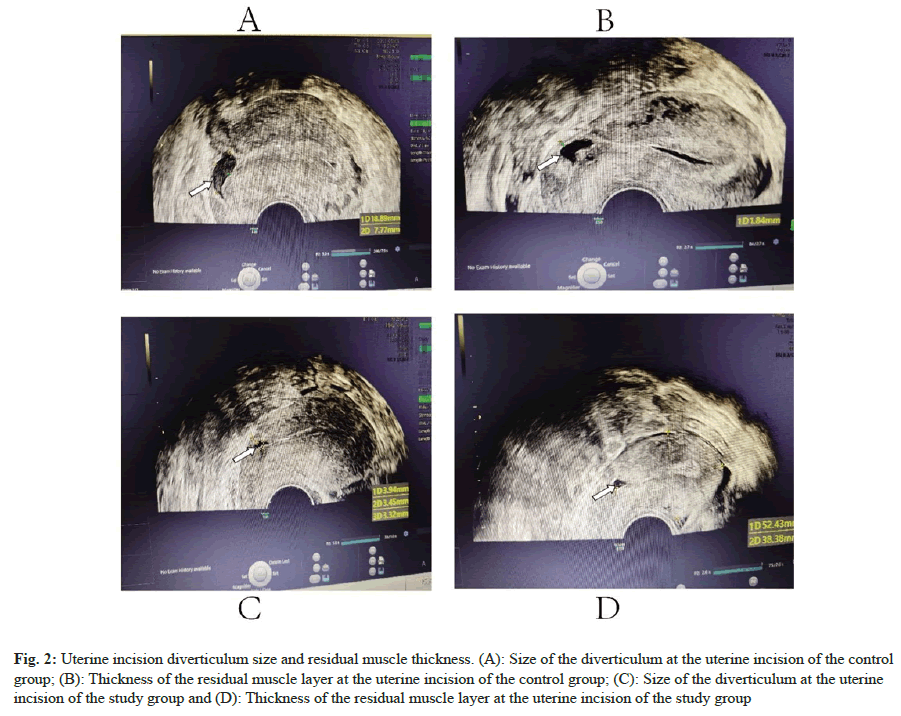
Demographic and clinical data, including maternal age, gestational age, parity, Body Mass Index (BMI), and new-born weight, were documented alongside intraoperative and postoperative metrics such as operative time and blood loss. Postoperative recovery indicators included intestinal exhaust time, hospital stay, and lochia bleeding duration. Follow-up assessments at 6 mo to 12 mo post-surgery involved vaginal color ultrasound to monitor for complications like abnormal vaginal bleeding and to evaluate the integrity of the uterine incision, the presence of PCSD, and the thickness of the residual muscle layer (fig. 2).
Fig. 2: Uterine incision diverticulum size and residual muscle thickness. (A): Size of the diverticulum at the uterine incision of the control group; (B): Thickness of the residual muscle layer at the uterine incision of the control group; (C): Size of the diverticulum at the uterine incision of the study group and (D): Thickness of the residual muscle layer at the uterine incision of the study group
Statistical Methods:
Data analysis was performed using Statistical Package for the Social Sciences (SPSS) 18.0. Quantitative data are presented as means with standard deviations (x̄ ±s), and group comparisons were made using t-tests. Categorical data are reported as percentages, with intergroup comparisons conducted using the chi-square (χ²) test. Statistical significance was set at a p-value of less than 0.05.
Results and Discussion
Our analysis showed equivalence in maternal age, gestational period, delivery timing, BMI, and newborn weight across both study and control groups, with no statistically significant differences observed (p>0.05), as shown in Table 1. The study group had a slightly extended operative time, which reached statistical significance (p<0.05). However, the two groups were comparable in terms of intraoperative blood loss, intestinal recovery time, hospital stay, and postoperative bleeding duration, with no significant differences (p>0.05), as depicted in Table 2. Significantly fewer cases of abnormal vaginal bleeding were recorded in the study group (8.27%) compared to the control group (18.46%). The occurrence of uterine scar diverticulum (PCSD) was also markedly reduced in the study group, affecting only 3.01% of participants, vs. 11.54% in the control group (p<0.05), as detailed in Table 3. The study group exhibited a substantial increase in the thickness of the lower uterine muscle layer at 42 d and 6 mo post-surgery, with a corresponding decrease in the rate of uterine scar diverticulum formation at these intervals and at 1 y post-surgery. These differences were statistically significant (all p<0.05), as shown in Table 4.
| General information | Study group (n=133) | Control group (n=130) | t | p |
|---|---|---|---|---|
| Age (years) | 31.80±4.46 | 32.56±4.26 | 1.421 | 0.157 |
| Gestational week | 38.60±1.29 | 38.70±0.93 | -.723 | 0.47 |
| Number of births (times) | 2.21±0.54 | 2.52±3.13 | -1.133 | 0.267 |
| BMI (kg/m2) | 27.84±3.96 | 27.30±4.21 | -1.079 | 0.282 |
| Birth weight (g) | 3225.26±450.31 | 3248.03±403.05 | 0.432 | 0.667 |
Table 1: Comparison of General Maternal Data between the Two Groups
| Perioperative information | Study group (n=133) | Control group (n=130) | t | p |
|---|---|---|---|---|
| Operative time (min) | 70.36±12.99 | 65.78±11.35 | -3.044 | 0.003 |
| Intraoperative blood loss (ml) | 553.38±214.19 | 539.15±175.61 | -0.588 | 0.557 |
| Postoperative lochia duration (days) | 32.69±6.92 | 39.48±41.37 | 1.865 | 0.063 |
| Intestinal exhaust time (h) | 33.67±11.41 | 33.27±11.31 | -0.307 | 0.759 |
| Length of hospital stay (days) | 5.23±0.71 | 5.28±1.09 | 0.450 | 0.653 |
Table 2: Comparison of the Perioperative Conditions of Cesarean Section between the Two Groups
| Abnormal vaginal bleeding and PCSD formation | Study group (n=133) | Control group (n=130) | χ2 | p |
|---|---|---|---|---|
| Abnormal vaginal bleeding | ||||
| Yes (%) | 8.27 (11/133) | 18.46 (24/130) | 4.421 | 0.036 |
| No (%) | 91.73 (122/133) | 81.54 (106/130) | ||
| PCSD formation | ||||
| Yes (%) | 3.01 (4/133) | 11.54 (15/130) | 5.838 | 0.016 |
| No (%) | 96.99 (129/133) | 88.46 (115/130) | ||
Table 3: Comparison of Abnormal Vaginal Bleeding and Incisional Scar Diverticulum Formation After the Second Cesarean Section Between the Two Groups
| Group | Number of cases | 42 d after surgery | 6 mo after surgery | Uterine scar formation 1 y after surgery (case/%) | ||
|---|---|---|---|---|---|---|
| Thickness of lower uterine muscle layer (mm) | Formation of uterine scar diverticulum (case/%) | Thickness of lower uterine muscle layer (mm) | Formation of uterine scar diverticulum (case/%) | |||
| Control | 130 | 3.03±0.37 | 0 (0.00) | 3.14± 0.17# | 6 (5.50) | 8 (7.34) |
| Research | 133 | 3.72±0.26 | 0 (0.00) | 3.83±026# | 0 (0.00) | 1 (0.92) |
| T value | 15.93 | 0.000 | 23.190 | 4.285 | 4.172 | |
| P value | p<0.05 | p>0.05 | p<0.05 | p<0.05 | p<0.05 | |
Table 4: Comparison of Thickness of Lower Uterine Muscle Layer and Formation of Scar Diverticulum
The statistical assessment at 42 d post-surgery yielded a T-value of 15.930 for uterine muscle layer thickness, signifying a significant disparity between the study and control groups (p<0.05). With no instances of diverticulum formation in either group at this stage, the lack of a t-test and a non- significant P-value confirmed the group’s similarity. At the 6 mo follow-up, the T-values for muscle layer thickness and diverticulum formation were 23.190 and 4.285, respectively (both p<0.05), denoting clear distinctions between the groups. By 1 y, the T-value for diverticulum formation was 4.172 (p<0.05), reinforcing the observed group differences.
The increasing awareness of uterine scar diverticula among clinicians, driven by the two-child and three- child policies and a focus on enhancing women’s quality of life, has led to a rise in diagnosis. These diverticula, resulting from cesarean sections, can lead to menstrual irregularities, discomfort, and decreased quality of life, including impacts on sexual activity. More seriously, they are associated with secondary infertility, repeated implantation failures in assisted reproduction, uterine scar pregnancies, and late pregnancy complications such as uterine rupture, posing significant risks to women’s reproductive health and safety.
Our study’s findings indicate that the technique of folding and suturing the lower uterine segment during a second cesarean section effectively restores anatomy, increases the thickness of the uterine muscle layer, and reduces postoperative abnormal vaginal bleeding. Despite a slightly longer operative time in the study group, there was no increase in surgical damage as measured by intraoperative bleeding, postoperative recovery, hospital stay, or postoperative bleeding time.
The study’s ample sample size and the consistent application of surgical techniques by experienced physicians lend reliability to our findings. We observed no significant differences in maternal characteristics between groups, but a significant reduction in the abnormal vaginal bleeding rate and diverticulum incidence in the study group compared to the control group.
Uterine diverticulum post-cesarean section is a complication characterized by poor uterine incision healing, leading to a diverticular-like protrusion that can cause abnormal bleeding and pain, and contribute to secondary infertility. Our results show that the novel suturing technique not only increases muscle layer thickness but also improves uterine incision blood flow and resistance to contraction forces, facilitating healing and reducing postpartum complications.
Furthermore, the potential integration of pharmaceutical interventions, such as prophylactic antibiotics and anti-inflammatory drugs, presents an opportunity to further optimize surgical outcomes. These medications could mitigate postoperative inflammation and infection, supporting the healing process and potentially decreasing the risk of diverticulum formation. The combination of surgical innovation and pharmacological therapy represents a promising approach to improving patient outcomes in cesarean section recovery.
Conclusion:
In summary, the "folding and suturing of the lower segment of the uterus" performed during the second cesarean section can effectively prevent uterine scar diverticulum formation. The technique is worth promoting clinically due to its efficacy in improving anatomical structure and reducing abnormal vaginal bleeding and diverticulum formation. Furthermore, integrating pharmaceutical strategies such as the use of prophylactic antibiotics and anti-inflammatory drugs can potentially reduce complications and enhance postoperative outcomes, thereby improving the prognosis for patients undergoing cesarean sections. The combination of surgical techniques and medication provides a comprehensive approach to optimizing patient care and recovery.
Funding:
Science and Technology Program of Guizhou Province (QKHPTRC-GCC (2022) 039-1, QKHPTRC-CXTD (2022) 014).
Data Availability:
All data collected and analysed during this study are included in this article. Further inquires can be directed to the corresponding author.
Conflict of interests:
The authors declared no conflict of interests.
References
- Vijayasree M. Efficacy of prophylactic B-Lynch suture during lower segment caesarian section in high risk patients for atonic postpartum Haemorrhage. Kathmandu Univ Med J 2016;53(1):9-12.
[Google Scholar] [PubMed]
- Zhang NN, Wang GW, Zuo N, Yang Q. Novel laparoscopic surgery for the repair of cesarean scar defect without processing scar resection. BMC Pregnancy Childbirth 2021;21:1-7.
[Crossref] [Google Scholar] [PubMed]
- Kaya C, Aslan Ö, Tetik M. Hysteroscopy-guided natural orifice repair of isthmocele. Gynecol Minim Invasive Ther 2022;11(2):116-8.
[Crossref] [Google Scholar] [PubMed]
- Peng C, Huang Y, Lu Y, Zhou Y. Comparison of the efficacy of two laparoscopic surgical procedures combined with hysteroscopic incision in the treatment of cesarean scar diverticulum. J Invest Surg 2022;35(1):225-30.
[Crossref] [Google Scholar] [PubMed]
- Kulshrestha V, Agarwal N, Kachhawa G. Post-caesarean niche (isthmocele) in uterine scar: An update. J Obstetr Gynecol India 2020;70(6):440-6.
[Crossref] [Google Scholar] [PubMed]
- Huang J, Li Q, Yuan X, Liu Q, Zhang W, Li P. Intrauterine infusion of clinically graded human umbilical cord-derived mesenchymal stem cells for the treatment of poor healing after uterine injury: A phase I clinical trial. Stem Cell Res Ther 2022;13(1):85.
[Crossref] [Google Scholar] [PubMed]
- de Vasconcelos Gaspar A, Brandao A. Isthmocele, a rising pathology. Clin Case Rep 2022;10(4):e05727.
[Crossref] [Google Scholar] [PubMed]
- Tsuji S, Nobuta Y, Hanada T, Takebayashi A, Inatomi A, Takahashi A, et al. Prevalence, definition, and etiology of cesarean scar defect and treatment of cesarean scar disorder: A narrative review. Reproduct Med Biol 2023;22(1):e12532.
[Crossref] [Google Scholar] [PubMed]
- Shi L, Du K. Prediction of scar myometrium thickness and previous cesarean scar defect using the three‐dimensional vaginal ultrasound. Contrast Med Mol Imag 2022;2022(1):3584572.
[Crossref] [Google Scholar] [PubMed]
- Wang J, Shi X, Li Y, Li Z, Chen Y, Zhou J. Prophylactic intraoperative uterine or internal iliac artery embolization in planned cesarean for pernicious placenta previa in the third trimester of pregnancy: An observational study (STROBE compliant). Medicine 2019;98(44):e17767.
[Crossref] [Google Scholar] [PubMed]