- *Corresponding Author:
- W. H. Zhang
Department of Spinal surgery, Affiliated Hospital of Jining Medical University, No.79, Guhuai Road Jining, Shandong 272029, China
E-mail: zwh100213@163.com
| This article was originally published in a special issue, “Clinical Research in Pharmaceutical and Biomedical Sciences” |
| Indian J Pharm Sci 2021:83(1)Spl issue1;62-69 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the therapeutic effect of percutaneous endoscopic bilateral decompression via unilateral interlaminar approach in the treatment of degenerative lumbar spinal stenosis is the main objective. One hundred and thirty-eight patients with degenerative lumbar spinal stenosis admitted to our hospital from March 2018 to July 2020 were selected and divided into a control group and a trial group according to a randomized double-blind method, with 69 cases in each group. The control group was treated with laminectomy and decompression, while the trial group was treated with percutaneous endoscopic bilateral decompression via unilateral interlaminar approach. The Visual analogue scale score and Oswestry Disability Index were assessed before, on the first day after surgery and at the last postoperative follow-up (3 mo after surgery), and the patients were analyzed for postoperative complications, surgical indicators and overall efficacy using the modified MacNab criteria. In addition, the intervertebral space height index and the cross-sectional area of the spinal canal were measured pre and postoperatively in the operated segment and in the adjacent segment superior to the operated segment. The results showed that the operation time, bleeding volume, incision length and hospital stay of the study group were lower than those of the control group, and the differences were statistically significant (p<0.05, respectively. And the excellent rate of the study group was higher than that of the control group, and the difference was significant (p<0.05). In addition, there was no significant difference in Visual Analogue Scale score and Oswestry Disability Index between the two groups before operation. After operation, the Visual Analogue Scale score and Oswestry Disability Index of the two groups were both significantly improved, and the Visual Analogue scale score and Oswestry Disability Index of the study group were lower than those of the control group, and the differences were significant (p<0.05, respectively). What’s more, the incidence of complications in the study group was lower than that in the control group (p<0.05). The results also indicated that at the last follow-up, there were no significant differences in intervertebral height index before and after operation in the both operated segment and the superior adjacent segment (p>0.05). In addition, at the last follow-up, the cross-sectional area of the spinal canal of the operated segment was significantly increased, and the improvement was more obvious in the study group than the control group, and the difference was statistically significant (p<0.05). However, there was no significant increase in the superior adjacent segment compared with that before operation (p>0.05). Percutaneous endoscopic bilateral decompression via unilateral interlaminar approach has the advantages of minimal trauma, precise decompression and rapid recovery in improving degenerative lumbar spinal stenosis, with good recent results.
Keywords
Degenerative lumbar spinal stenosis, unilateral interlaminar approach, bilateral decompression, percutaneous spinal endoscopic technique
Degenerative lumbar spinal stenosis (LSS) is a common fatigue type lumbar disease in the middleaged and elderly[1], which can significantly affect the quality of life and daily activities of patients, and lead to progressive disability[2-4]. Conservative treatments such as physical therapy and acupuncture are the first choices for most LSS patients[5], which can relieve pain, but the effect is general, and the pain attacks repeatedly[1]. If conservative treatment fails, nerve decompression should be considered. Conventional laminectomy has the disadvantages of chronic low back pain and iatrogenic instability[6]. And lumbar fusion surgery has the disadvantages of large trauma, high cost and easy to cause many complications, which is a challenge to the elderly, especially the elderly patients with osteoporosis[7,8].
In recent years, with the continuous development of minimally invasive technology, percutaneous total spinal endoscopic technology, which combines the advantages of traditional open surgery and endoscopic technology, can effectively reduce the pressure through small incision, and effectively separate, bite and clamp the diseased tissues such as herniated intervertebral disc and hypertrophic ligament under the endoscopic system, so as to fully remove them. However, for the osseous and ligament structures that do not cause compression, percutaneous total spinal endoscopic technology can retain as appropriate. Moreover, in the process of this operation, there is no need to peel off more related tissues such as paravertebral muscles and target segment facets. On the premise of ensuring decompression, it can reduce the damage to the physiological structure of the spine, reduce the damage to the stability of the spine, and is conducive to postoperative recovery. For the elderly patients with high perioperative risk, it is an effective and accurate decompression method for choosing. This study was to investigate the clinical efficacy and safety of percutaneous endoscopic bilateral decompression via unilateral interlaminar approach in the treatment of LSS, so as to provide reference for the further promotion and application of this surgical method in clinical practice in the future.
Clinical characteristics and Methods
General information:
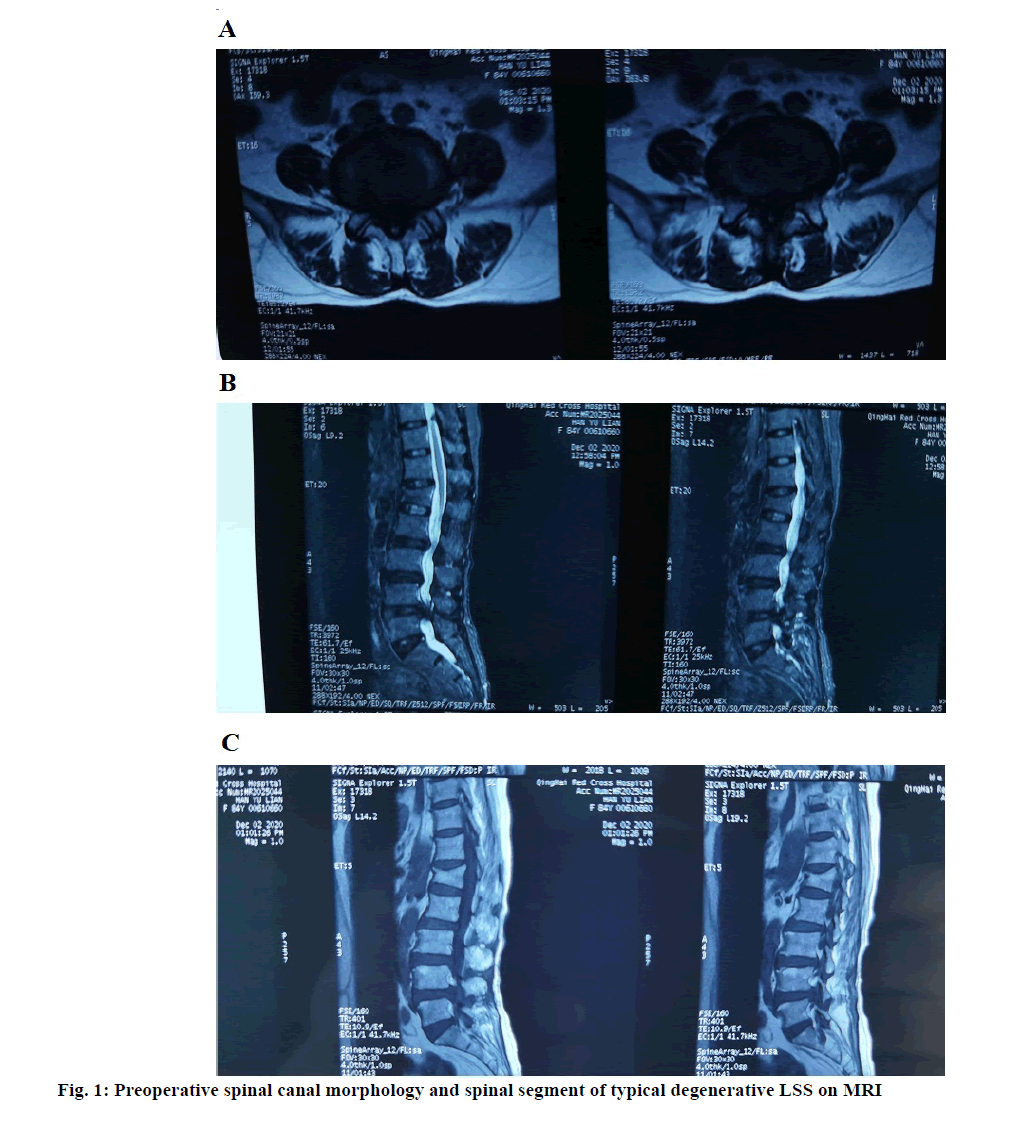
A total of 138 patients with degenerative LSS admitted to our hospital from March 2018 to July 2020 were selected. Inclusion criteria: Imaging examination showed single segment central type and lateral recess type LSS; the patients had typical intermittent claudication symptoms, accompanied with bilateral buttock and/or lower limb pain, and mainly with buttock and lower limb pain. The visual analogue scale (VAS) of low back pain was less than 3; there was no improvement after conservative treatment for more than 3 mo; there were complete (X-radiation (X-ray), Magnetic resonance imaging (MRI)) imaging data in our hospital before and after operation; there were indications for operation. Exclusion criteria:Patients with simple disc herniation; lumbar segmental instability, degenerative lumbar spondylolisthesis, meyerding grade II or above; Patients with a history of surgery at the same segment of the lumbar spine, isthmus, severe deformity, spinal infection and tumor; Patients with serious medical diseases who cannot tolerate local anesthesia; the follow-up information was incomplete or lost. Preoperative X-ray showed obvious degeneration of lumbar spine, Computed tomography (CT) showed obvious stenosis of lumbar spinal canal, hyperplasia and hypertrophy of articular process and ligamentum flavum, and the shape of spinal canal was clover; MRI showed degeneration and protrusion of intervertebral disc with spinal canal stenosis, nerve compression, unclear cauda equina nerve, and disappearance of fat outside dural sac (fig. 1A). The patients were randomly divided into the control group and the study group, with 69 cases in each group. In the control group, there were 41 males and 28 females, aged 55-82 (64.35±3.15) y, and the course of disease was 1-4 (2.72±1.14) y. There were 37 males and 31 females in the study group, aged 58-84 (65.76±4.05) y, and the course of disease was 2-6 (3.29±1.21) y. There was no significant difference in clinical data between the two groups (p>0.05).
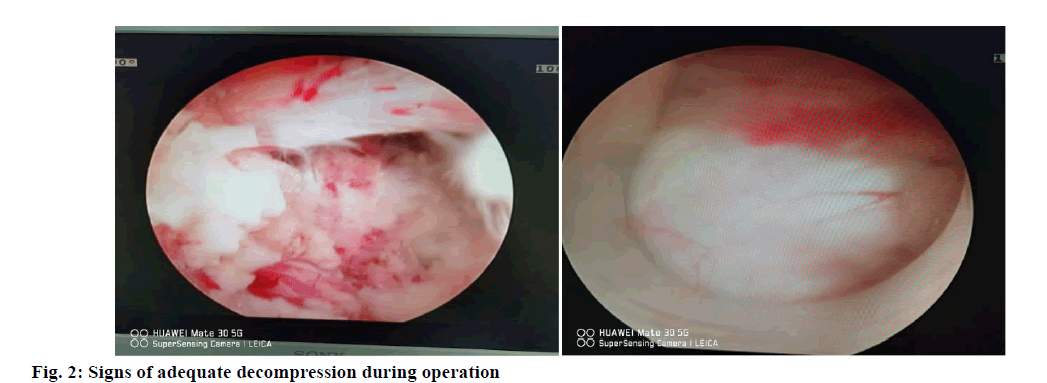
Methods: The control group was treated with laminectomy and decompression. A longitudinal incision was made at the center of decompression segment. The skin, subcutaneous and fascial tissues were removed at the edge of the supraspinous ligament. The sacrospinalis muscle was stripped off to expose the lamina. The upper and lower lamina was excised. Hemostasis was performed with bone wax. The spinous process complex was preserved. The articular process and ligamentum flavum adjacent to the bone window were excised. The lateral recess was enlarged and the nerve roots were exposed and pulled out. Osteophyte on the posterior margin of the body was decompressed along the nerve root until there was no compression in the nerve running area. The study group was treated with percutaneous endoscopic bilateral decompression via unilateral approach between lamina. After continuous epidural anesthesia, the patient was placed in prone position with abdomen suspended. The operating table was adjusted to make the lumbar spine moderately forward flexion, increase the laminar space and tension the ligamentum flavum. According to the lumbar X-ray and body surface marks, the responsible laminar space was initially located and marked. After the sterile sheet was laid after routine disinfection, the puncture needle was used to locate the lesion side of the lamina space again, and the positioning point was located at the middle point of the lower edge of the upper vertebral lamina. After localization, a 7 mm long incision was made at 0.5-1 cm beside the spinous process Through longitudinal skin incision (incision of skin, subcutaneous tissue and deep fascia), the pencil head expands the muscle and soft tissue, puts the working channel along the pencil head, pulls out the pencil head, confirms the satisfactory position of the working channel under fluoroscopy, then connects and puts it into the spinal endoscope. Under the microscope, after cleaning the fibrous adipose tissue on the surface of the ligamentum flavum, the ligamentum flavum, articular process and vertebral lamina can be seen, and the high-speed grinding drill with protective sheath is used to polish bone. The order is: the medial edge of the lower and upper facets of the operated side; the attachment of the lamina to the ligamentum flavum of the operated side; the root of the spinous process; the ventral side of the contralateral lamina; the ventral side of the contralateral upper and lower facets of the operated side. Then the nerve was dissected and the ligamentum flavum and dural sac were separated to prevent adhesion. The hypertrophic ligamentum flavum was removed along the attachment point of ligamentum flavum with blue forceps and gun forceps. The superior and inferior articular processes of the operative side and the contralateral side were further treated, and when the dural sac and bilateral nerve roots were fully released, the radiofrequency scalpel was able to stop bleeding completely. Decompression completion sign: the range of decompression reached the lower edge of the upper vertebral body at the proximal end, the upper part of the bony lateral recess at the distal end, and 3-5 mm at the dorsal side of the nerve and dural sac. The dural sac filled well and recovered to normal pulsation; the nerve root returned to normal shape, and there was clear and sufficient space around the dural sac and nerve root, as shown in fig. 2. Withdraw the working cannula, suture the incision, apply aseptic dressing, cover and bandage.
Observed indexes:
The following clinical indicators were evaluated before operation, 1 d after operation and the last follow-up (3 mo after operation): VAS was used to evaluate low back pain and lower limb pain; lumbar function was evaluated by Oswestry disability index (ODI); the incidence of surgical complications.
At the last follow-up, the modified MacNab standard was used to evaluate the overall efficacy. Excellent: the symptoms disappear completely, and the original work and life are restored; Good: there are slight symptoms, and the activity is slightly limited, which has no effect on the work and life; Fair: the symptoms are relieved, and the activity is limited, which affects the normal work and life; Poor: there is no difference before and after treatment, or even worse. The total excellent rate=(excellent+good)/total×100 %.
The operation time, bleeding volume, incision length and hospital stay were compared between the two groups.
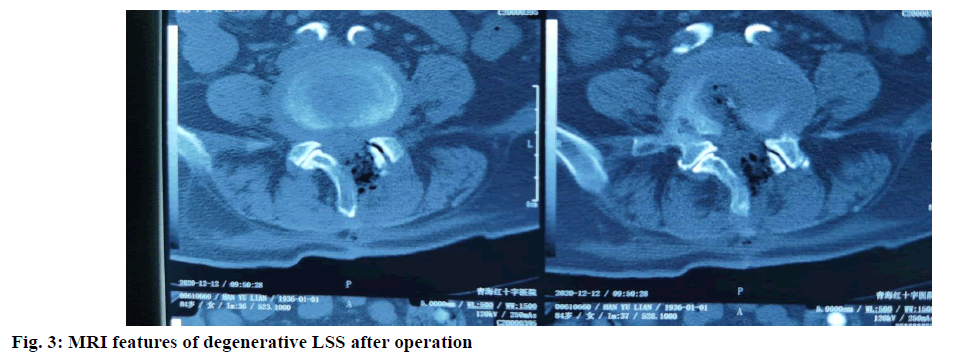
The intervertebral height index (IHI) and cross-sectional area of the spinal canal (CASC) of the surgical segment and the upper adjacent segment (the upper segment of the operative segment) were measured. CASC: The cross section of the middle layer was selected from the cross section of the diseased intervertebral body in MRI scanning, and the measurement area was the area between the facet joint and the lamina, as shown in fig. 3. IHI: We measured the IHI as previous[9,10]. IHI=(anterior intervertebral space height+posterior intervertebral height)/(width of upper vertebral endplate in intervertebral space+width of upper end plate of lower vertebral body in intervertebral space), that is (a+b)/(c+d). The morphology was shown in fig. 1B and fig. 1C.
Statistical analysis:
All the collected data were checked, numbered and sorted out. The database was established by Excel. Statistical Package for the Social Sciences (SPSS) 20.0 was used for statistical analysis. All the results were expressed as (x±s). All preoperative and postoperative measurements were compared by paired t-test. p<0.05 meant the difference was significant.
Results and Discussion
The results showed that the operation time, bleeding volume, incision length and hospital stay of the study group were lower than those of the control group, and the differences were statistically significant (p<0.05, respectively), as shown in Table 1.
| Groups | N | Operation time (min) | Bleeding volume (ml) | Incision length (mm) | Hospital stay (d) |
|---|---|---|---|---|---|
| Control group | 69 | 69.78±10.25 | 361.60±24.10 | 7.58±1.46 | 9.82±0.67 |
| Study group | 69 | 51.40±9.68 | 235.85±28.95 | 11.92±1.69 | 7.24±0.88 |
| t | 5.371 | 6.047 | 4.468 | 4.883 | |
| p | 0.001 | 0.001 | 0.001 | 0.001 |
Table 1: Comparison of Operation Related Indexes between the Two Groups
The results showed that the excellent rate of the study group was higher than that of the control group, and the difference was significant (p<0.05), as shown in Table 2.
| Clinical efficacy | ||||||
|---|---|---|---|---|---|---|
| Groups | N | Excellent | Good | Fair | Poor | Excellent rate |
| Control group | 69 | 46 | 20 | 2 | 1 | 66 (95.65) |
| Study group | 69 | 35 | 23 | 8 | 3 | 58 (84.06) |
| t | 5.531 |
|||||
| p | 0.001 |
|||||
Table 2: Comparison of Surgical Treatment Effect between the Two Groups
The results showed that there was no significant difference in VAS and ODI between the two groups before operation. After operation, the VAS and ODI of the two groups were both significantly improved, and the VAS and ODI of the study group were lower than those of the control group, and the differences were significant (p<0.05, respectively), as shown in Table 3.
| Group | Control group | Study group | t | p | |
|---|---|---|---|---|---|
| VAS | Before operation | 7.27±0.58 | 7.36±0.62 | 0.943 | 0.721 |
| 1 d after operation | 4.60±0.47 | 2.26±0.43 | 4.315 | 0.001 | |
| Last follow-up | 2.33±0.21 | 1.82±0.17 | 2.058 | 0.024 | |
| t | 5.473 | 6.553 | |||
| p | 0.001 | 0.001 | |||
| ODI | Before operation | 77.21±5.51 | 78.82±4.93 | 1.026 | 0.619 |
| 1 d after operation | 57.33±4.14 | 43.39±4.08 | 4.157 | 0.001 | |
| Last follow-up | 37.73±2.09 | 28.44±2.27 | 5.052 | 0.001 | |
| t | 4.343 | 6.217 | |||
| p | 0.001 | 0.001 | |||
Table 3: Comparison of Vas and Odi Between the Two Groups
The results showed that the incidence of complications in the study group was lower than that in the control group (p<0.05), as shown in Table 4.
| Group | Control group | Study group | t | p |
|---|---|---|---|---|
| N | 69 | 69 | ||
| Incision infection | 2 (2.90 %) | 1 (1.45 %) | ||
| Ischemic necrosis of incision | 1 (1.45 %) | 0 (0.00 %) | ||
| Dural sac tear | 2 (2.90 %) | 0 (0.00 %) | ||
| Gastrointestinal dysfunction | 3 (4.35 %) | 1 (1.45 %) | ||
| Incidence of complications | 8 (11.59 %) | 2 (2.90 %) | 4.105 | 0.001 |
Table 4: Comparison of Complications between the Two Groups
The results indicated that at the last follow-up, there were no significant differences in IHI index before and after operation in the both operated segment and the superior adjacent segment (p>0.05). In addition, at the last follow-up, the CASC of the operated segment was significantly increased, and the improvement was more obvious in the study group than the control group, and the difference was statistically significant (p<0.05). However, there was no significant increase in the superior adjacent segment compared with that before operation (p>0.05), as shown in Table 5.
| Group | Before operation | After operation | t | p | ||
|---|---|---|---|---|---|---|
| CASC | Operated segment | Control group | 117.18±42.31 | 159.42±38.81 | 5.332 | 0.001 |
| Study group | 116.36±44.89 | 183.17±64.57 | 7.192 | 0.001 | ||
| The superior adjacent segment | Control group | 130.25±40.46 | 133.78±39.60 | 1.467 | 0.539 | |
| Study group | 131.09±41.25 | 135.24±44.30 | 1.787 | 0.231 | ||
| IHI | Operated segment | Control group | 36.76±6.03 | 34.89±5.64 | 3.064 | 0.031 |
| Study group | 36.58±6.22 | 33.96±5.31 | 4.642 | 0.001 | ||
| The superior adjacent segment | Control group | 34.68±5.11 | 34.56±5.27 | 0.993 | 0.715 | |
| Study group | 34.72±4.98 | 34.37±4.38 | 1.124 | 0.609 | ||
Table 5: Comparison of Casc and Ihi Indexes Before and After Operation between the Two Groups
Due to the rapid development of society and the change of people’s lifestyle, the incidence rate of degenerative LSS is increasing. And degenerative LSS is also the most common kind of LSS[4,5]. With the increase of age and weight, the degenerative degree of lumbar bone and soft tissue increases, such as intervertebral disc protrusion, intervertebral joint hypertrophy, hypertrophy and calcification of ligamentum flavum, etc., which will lead to stenosis of lumbar spinal canal and intervertebral foramen, and then compress cauda equina nerve, nerve root and corresponding blood vessels, causing corresponding clinical symptoms including lumbocrural pain. Therefore, it is of great clinical significance to select the appropriate surgical treatment according to the patient’s condition[11].
At present, non-surgical treatment is still the first choice for the treatment of LSS[12]. Physical therapy for lumbar spinal stenosis usually involves some combination of core strengthening, flexibility training, and stability exercises. The evidence of benefit from physical therapy alone is not clear. Common physical therapy includes bed rest, massage, proper exercise, braking, etc. The most commonly used drugs are non-steroidal anti-inflammatory drugs, among which cyclooxygenase-2 (COX-2) inhibitors are the first choice due to their small side effects on gastrointestinal tract[13]. When non-surgical treatment is ineffective, decompression is often used. Traditional decompression operations include total laminectomy, semi laminectomy, interlaminar fenestration and other laminectomy. Simple fenestration decompression or partial laminectomy can reduce the pressure of pathological factors, so as to achieve good clinical effect; however, when the decompression range is too large and the facet resection is too much, there is a risk of aggravating lumbar instability. Although the above-mentioned traditional decompression is effective in a short period of time, its disadvantages such as large amount of bleeding, more soft tissue damage, long recovery time after operation, high risk of infection and anesthesia also follow. However, bilateral decompression through unilateral percutaneous interlaminar approach for degenerative LSS does not need to damage the patient’s lamina tissue, paravertebral muscle and ligament tissue, which has less impact on the stability of the spine after operation and can reduce the occurrence of postoperative adhesion and scar. And under endoscopy, surgeons can deal with the nerve roots of patients under direct vision, which can clearly observe the pathological tissue[14]. The operation only needs local anesthesia, and can communicate with the operator in time to reduce the injury of nerve and blood vessel. There is almost no bleeding during the operation, so the operator’s vision is clearer, thus reducing the risk of misjudgment and misoperation. In addition, the operation has less damage to the body tissue of the patients, so the patients can carry out underground activities early after the operation to reduce the pain symptoms. And because of the small incision, the incidence of incision infection decreases. In this study, the operation time, bleeding volume, incision length and hospital stay of the study group were lower than those of the control group, and the differences were statistically significant. And the incidence of complications in the study group was lower than that in the control group. Therefore, percutaneous endoscopic bilateral decompression through unilateral interlaminar approach has a good clinical effect in the treatment of degenerative LSS, which can reduce the incidence of postoperative complications, and is conducive to the rapid recovery of patients. Post operatively, it has been observed that quality of life and the over aII satisfaction percentage of the patients has been drasticaIIy improved.
In this study, MRI and X-ray were used to measure the follow-up patients. At present, MRI has become one of the most accurate methods in the diagnosis of LSS. Eum et al.[15] evaluated the diagnostic value of CT and MRI for LSS, and found that the diagnostic value of the two imaging methods was similar. Torudom et al.[16] also suggested that LSS patients should receive routine lumbar MRI examination before surgery. They found that patients with severe or single segment stenosis of the central canal, moderate or multi segment stenosis on lumbar MRI had better postoperative satisfaction. The advantages of MRI in qualitative and quantitative evaluation of spinal decompression are as follows: firstly, MRI has more advantages than CT in displaying nerve root or lumbar spinal canal compression, because it can better display various soft tissues, such as ligamentum flavum, foraminal ligament and herniated intervertebral disc[17-20]. Second, due to the combination of high quality, high soft tissue contrast and high resolution, MRI can evaluate the condition of intervertebral disc, nerve root, posterior longitudinal zone and intervertebral foramen in multiple directions and sequences. In this study, we used MRI to quantitatively measure the CASC and IHI of lumbar intervertebral disc. The results indicated that at the last follow-up, there were no significant differences in IHI index before and after operation in the both operated segment and the superior adjacent segment. In addition, at the last follow-up, the CASC of the operated segment was significantly increased, and the improvement was more obvious in the study group than the control group, and the difference was statistically significant. However, there was no significant increase in the superior adjacent segment compared with that before operation. The improvement of the mean CASC indicates that the stenosis in the center of lumbar spinal canal has been fully reduced.
To sum up, percutaneous endoscopic bilateral decompression via unilateral interlaminar approach for degenerative LSS has the advantages of small trauma, accurate decompression and rapid recovery, and has good short-term effect.
Acknowledgements
This work was supported by the Qinghai Red Cross Hospital and the Affiliated Hospital of Jining Medical University.
Conflict of interests
The authors declared no conflict of interest.
References
- Katz JN, Harris MB. Lumbar spinal stenosis. N Engl J Med 2008;358:818-25.
- De Graaf I, Prak A, Bierma-Zeinstra S, Thomas S, Peul W, Koes B. Diagnosis of lumbar spinal stenosis: a systematic review of the accuracy of diagnostic tests. Spine 2006;31:1168-76.
- Kreiner DS, Shaffer WO, Baisden JL, Gilbert TJ, Summers JT, Toton JF, et al. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J 2013;13:734-43.
- Epstein NE, Maldonado VC, Cusick JF. Symptomatic lumbar spinal stenosis. Surg Neurol 1998;50:3-10.
- Armon C, Argoff CE, Samuels J, Backonja MM. Assessment: use of epidural steroid injections to treat radicular lumbosacral pain: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 2007;68:723-9.
- Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Blood E, Hanscom B, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med 2008;358:794-810.
- Bresnahan LE, Smith JS, Ogden AT, Quinn S, Cybulski GR, Simonian N, et al. Assessment of paraspinal muscle cross-sectional area after lumbar decompression: minimally invasive versus open approaches. Clin Spine Surg 2017;30:E162-8.
- Amundsen T, Weber H, Nordal HJ, Magnaes B, Abdelnoor M, Lilleas F. Lumbar spinal stenosis: conservative or surgical management?: A prospective 10-year study. Spine 2000;25:1424-36.
- Lonne G, Odegard B, Johnsen LG, Solberg TK, Kvistad KA, Nygaard OP. MRI evaluation of lumbar spinal stenosis: is a rapid visual assessment as good as area measurement? Eur Spine J 2014;23:1320-4.
- Ruetten S, Komp M, Merk H, Godolias G. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. J Neurosurg Spine 2009;10:476-85.
- Wen B, Zhang X, Zhang L, Huang P, Zheng G. Percutaneous endoscopic transforaminal lumbar spinal canal decompression for lumbar spinal stenosis. Medicine (Baltimore) 2016;95:e5186.
- Ahn Y. Percutaneous endoscopic decompression for lumbar spinal stenosis. Expert Rev Med Devices 2014;11:605-16.
- Shin SH, Bae JS, Lee SH, Keum HJ, Kim HJ, Jang WS. Transforaminal endoscopic decompression for lumbar spinal stenosis: A novel surgical technique and clinical outcomes. World Neurosurg 2018;114:e873-82.
- Komp M, Hahn P, Merk H, Godolias G, Ruetten S. Bilateral operation of lumbar degenerative central spinal stenosis in full-endoscopic interlaminar technique with unilateral approach: prospective 2-year results of 74 patients. Clin Spine Surg 2011;24:281-7.
- Eum JH, Heo DH, Son SK, Park CK. Percutaneous biportal endoscopic decompression for lumbar spinal stenosis: a technical note and preliminary clinical results. J Neurosurg Spine 2016;24:602-7.
- Torudom Y, Dilokhuttakarn T. Two portal percutaneous endoscopic decompression for lumbar spinal stenosis: preliminary study. Asian Spine J 2016;10:335.
- Lee CW, Yoon KJ, Jun JH. Percutaneous endoscopic laminotomy with flavectomy by uniportal, unilateral approach for the lumbar canal or lateral recess stenosis. World Neurosurg 2018;113:e129-37.
- Ahn Y, Lee SH, Park WM, Lee HY. Posterolateral percutaneous endoscopic lumbar foraminotomy for L5-S1 foraminal or lateral exit zone stenosis. J Neurosurg Spine 2003;99:320-3.
- Kambin P, Casey K, O'Brien E, Zhou L. Transforaminal arthroscopic decompression of lateral recess stenosis. J Neurosurg 1996;84:462-7.
- Wang Y, Dou Q, Yang J, Zhang L, Yan Y, Peng Z, et al. Percutaneous endoscopic lumbar decompression for lumbar lateral spinal canal stenosis: classification of lateral region of lumbar spinal canal and surgical approaches. World Neurosurg 2018;119:e276-83.