- *Corresponding Author:
- W. Li
Department of Orthodontics, Peking University School and Hospital of Stomatology, China
E-mail: drliweiranbj@126.com
| This article was originally published in a special issue, "Clinical and Experimental Studies on Drug and Intervention Repurposing in China |
| Indian J Pharm Sci 2019:81(4)spl issue1;13-20 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
The purpose of this randomized controlled trial was to investigate the effects of direct and indirect mini-implant anchorage on tooth movement, skeletal and soft-tissue changes following sliding en masse retraction in adult patients with maxillary protrusion. A total of 30 patients (6 male, 24 female, mean age 23.5±6.29 years) were randomly assigned to group A with direct mini-implant anchorage or group B with indirect mini-implant anchorage. Lateral cephalograms taken before and after retraction were used to evaluate the changes during space closure. Independent sample t tests were performed to compare the baseline cephalometric data and treatment changes between the two groups. Paired sample t tests were performed to examine the changes within each group. The Results showed that no significant difference in anteroposterior skeletal changes was found between the two groups. The occlusal plane rotated clockwise 4.11° (p<0.001) in group A and remained stable in group B. Regarding dental changes, the maxillary molars mesialized by 0.83 mm in group B and showed non-significantly anteroposterior movement in group A. In group A the molars showed significant distal inclination (6.97°, p<0.001) and intrusion (2.74 mm, p<0.001) compared with group B (p<0.001). There was no significant difference in the anteroposterior or vertical movement of the incisors between the two groups. The soft-tissue parameters were significantly improved in both groups (p<0.001) while no differences were found between the groups. In conclusions, both directly and indirectly loaded mini-implants can provide successful anchorage. Indirect mini-implant anchorage enabled better sliding mechanics compared to direct anchorage.
Keywords
Mini-implant anchorage, direct anchorage, indirect anchorage, randomized clinical trial, maxillary protrusion
Anchorage control is essential for successful treatment of severe maxillary dentoalveolar protrusion patients. Treatment of this malocclusion usually involves premolars extraction and maximum anchorage to improve the facial profile[1]. It is well known that miniimplant anchorage is capable of providing maximum anchorage for anterior teeth retraction with sliding mechanics[2-7]. The benefits of mini-implant anchorage include independence from patients’ compliance, minimally invasive, less discomfort, shortened treatment time by en masse retraction of six anterior teeth, low cost, few anatomical limitations because of small dimensions[8]. Therefore, mini-implant anchorage has gained enormous popularity in the orthodontic community[9-13]. To retract anterior teeth, after the extraction of premolars, mini-implants can provide direct and indirect anchorage[14-20]. The force vectors and retraction forces are different for these two methods. The objectives of orthodontic treatment are not only optimal aesthetic appearances in harmony with maxillofacial hard and soft tissues but also functional and stable occlusions by properly positioning all teeth[21,22]. Therefore, high-quality treatment for maxillary protrusion should be guaranteed by not only to obtain soft-tissue profile changes but also to select the appropriate directions of force to move the teeth into the desired pattern.
Previous studies have been conducted on direct miniimplant anchorage in comparison with conventional anchorage, and found that direct anchorage provided maximum anchorage for anterior teeth retraction and led to intrusion of the maxillary incisors and molars[4,5,14]. The literature focused on indirect mini-implant anchorage is still rare. A recent study indicated that the anchorage loss with indirect anchorage is nearly equivalent to that with direct anchorage[19]. However, the differences of treatment changes between direct and indirect mini-implant anchorage were not described in the previous researches and require further exploration. The purpose of this randomized controlled trial (RCT) was to compare the skeletal, dental, and soft tissue changes following sliding en masse retraction of upper anterior teeth between direct and indirect mini-implant anchorage in maxillary protrusion patients.
Materials and Methods
Subjects:
This research was approved by the local ethics committee. The sample size was estimated by Power Analysis and Sample Size for Windows software (PASS 2000, NCSS, Kaysville, Utah), calculated on the base of simple comparison. Based on our preliminary study, group sizes of 13 achieved 80 % power to detect a difference of 1 mm in vertical displacement of upper first molar (standard deviation 0.9 mm) with a significance level (alpha) of 0.05. Allowing for 10 % drop out rate, the study was estimated to require 30 patients in total. This RCT was approved by the ethics committee of China-Japan Friendship Hospital, Beijing, China (approval number, 2013-40).
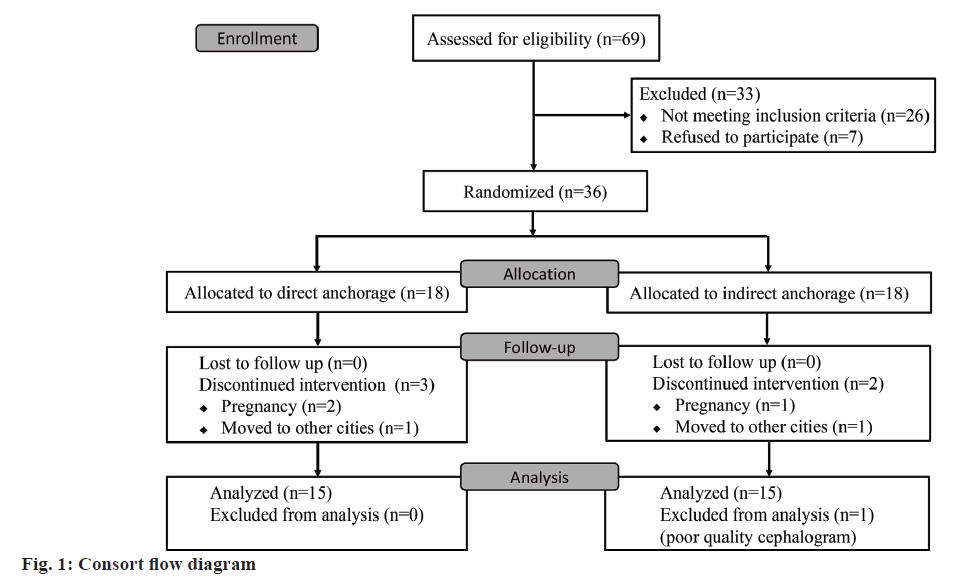
The inclusion criteria were as follows: (1) minimum age of 16 y for female patients and 18 y for male patients; (2) maxillary protrusion with angle class I or class II division I relationship, well aligned maxillary teeth with minimal crowding (less than 3 mm); (3) the treatment plan involved extraction of the bilateral maxillary first premolars (with first or second premolars extracted in the mandibular arch) and maximum anchorage was required in the upper arch; (4) agreed to use mini-implant anchorage during retraction of the upper anterior teeth to obtain good esthetics and correct the molar relationship; (5) full permanent dentition with no congenitally missing teeth (except for the third molars) or a malformed tooth; (6) no serious temporomandibular joint disorder or periodontal disease. The patients who met the inclusion criteria were randomly assigned to two equal groups: group A (direct anchorage) and group B (indirect anchorage). A random allocation sequence was generated using Microsoft Excel 2013 (Microsoft Corporation, Redmond, Washington, USA), and allocations were concealed in sequentially numbered, sealed opaque envelopes opened after written consent was obtained. The principal investigator was blinded to the allocation sequence during experiments and outcome assessment. A flow diagram of patients’ recruitment, assignment and follow-up is provided in fig. 1. Thirty patients were included in the final analyses and the patient details are shown in Table 1.
| Group A (n=15) | Group B (n=15) | P # | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Age at T0 (y) | 25.20 | 7.65 | 21.80 | 4.16 | 0.337 |
| Duration of retraction (mos) | 9.67 | 2.18 | 8.50 | 2.03 | <0.001* |
| Distance of space (mm) | 6.39 | 0.64 | 6.43 | 0.70 | 0.988 |
| Sex (male/female) | 3/12 | 3/12 | 0.217 | ||
| Angle classification (I/II) | 11/4 | 11/4 | 0.779 | ||
#Independent t test, *statistically significant difference
Table 1: Detailed information of 30 subjects and a comparison of the retraction duration between groups.
Appliances:
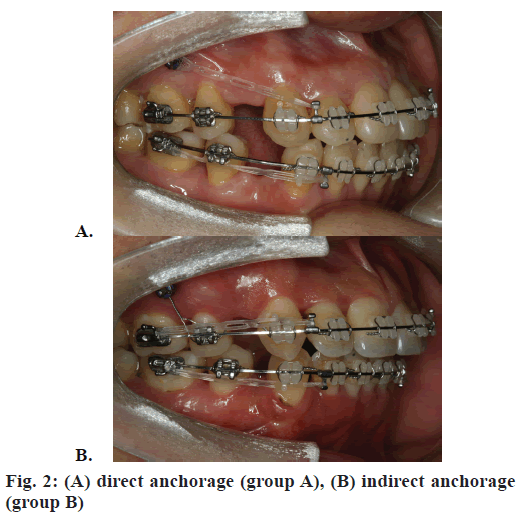
All patients were treated with MBT pre-adjusted appliances with slot size of 0.022×0.028-inch (3M Unitek, Monrovia, CA, USA). All first molars were bonded with molar tubes, and the second molars were not bonded to reduce sliding friction in the posterior segment. After initial leveling and alignment, handoperated self-drilling mini-implants (Ortho Easy, diameter 1.7 mm, length 8.0 mm, Forestadent, Pforzheim, Germany) were placed by the same operator in the buccal alveolar bone between the roots of the upper second premolars and first molars on both sides approximately 8 mm above the archwire. Three weeks after insertion of the mini-implants, en masse retraction of the anterior teeth by sliding mechanics was applied using 0.019×0.025-inch stainless steel archwires with crimpable hooks attached distal to the lateral incisors. In group A, the power chains (Ormco, Glendora, CA, USA) were stretched from each miniimplant head to a crimpable hook as direct anchorage (fig. 2A). In group B, the power chains were stretched from the first molar buccal tube to the crimpable hook, and then, the mini-implant was tightened to the second premolar bracket by a ligature wire of 0.25 mm in diameter as indirect anchorage (fig. 2B). The retraction force was approximately 150 g on each side, and the power chains were renewed every 4 w. During the space closure procedure, the archwires had no torque or curve of Spee, and intermaxillary elastics were avoided to eliminate possible side effects.
Cephalometric analysis:
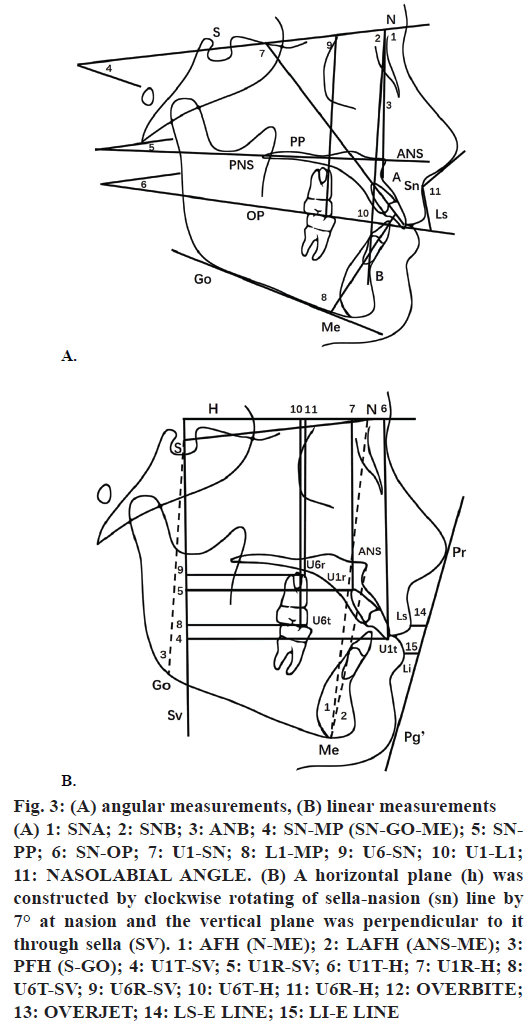
Standardized digital lateral cephalometric films (Promax, Planmeca, Helsinki, Finland) were taken before (T0) and after space closure (T1). To avoid assessment bias, archwires were removed before taking the cephalograms. Dolphin Imaging Software (version 11.7, Dolphin Imaging & Management Solutions, Chatsworth, CA, USA) was used to obtain the cephalometric measurements, and the data were exported to Microsoft Excel 2013 for further analysis. Digitization, tracing, and measurements of the cephalograms were performed by the same examiner who was blinded to the patient allocation of the study. The coordinate system, angular and linear measurements are shown in figs. 3A and B.
Figure 3: (A) angular measurements, (B) linear measurements
(A) 1: SNA; 2: SNB; 3: ANB; 4: SN-MP (SN-GO-ME); 5: SNPP; 6: SN-OP; 7: U1-SN; 8: L1-MP; 9: U6-SN; 10: U1-L1; 11: NASOLABIAL ANGLE. (B) A horizontal plane (h) was constructed by clockwise rotating of sella-nasion (sn) line by 7° at nasion and the vertical plane was perpendicular to it through sella (SV). 1: AFH (N-ME); 2: LAFH (ANS-ME); 3: PFH (S-GO); 4: U1T-SV; 5: U1R-SV; 6: U1T-H; 7: U1R-H; 8: U6T-SV; 9: U6R-SV; 10: U6T-H; 11: U6R-H; 12: OVERBITE; 13: OVERJET; 14: LS-E LINE; 15: LI-E LINE
Statistical analysis:
All statistical analyses were performed using SAS software (version 9.4; SAS Institute, Cary, NC, USA). Independent sample t tests were performed to compare the baseline cephalometric data and treatment changes between the two groups. Paired sample t tests were performed to examine the treatment changes between T0 and T1 in each group. The statistical significance was determined at the 5 % level of significance.
Measurement reliability:
To identify the measurement reliability, 10 randomly selected cases from each group were digitized and analysed 4 w apart by the same examiner. Intraexaminer reliability was evaluated using the intraclass correlation coefficient, with the highest r value of 0.998 for the SN-MP angle and lowest r value of 0.81 for the SN-PP angle.
Results and Discussion
Before treatment, no statistically significant differences were observed in patients’ age, sex distribution and angle's classification between the two groups (p>0.05, Table 1).
During the retraction period, 3 mini-implants became loosened in group A, but the 30 mini-implants in group B showed stability. Any loosened miniimplants were replaced by a new mini-implant in the same interradicular area neighboring the bone at the original site after bone healing for approximately 4 w. None of the replaced mini-implant subsequently failed. The descriptive statistics containing the means and standard deviations for the respective groups and treatment changes are given in Tables 2-4. There was no significant difference between the two groups in the pre-treatment cephalometric measurements except for LAFH/AFH % (p=0.008).
| Variable | Group A | Group B | P# | Group A | Group B | P# | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | P## | Mean | SD | P## | |||
| SNA (°) | 81.26 | 4.10 | 82.30 | 3.07 | 0.439 | -0.92 | 1.35 | 0.020* | -0.40 | 1.04 | 0.157 | 0.248 |
| SNB (°) | 76.97 | 3.42 | 78.91 | 2.73 | 0.099 | -0.16 | 1.58 | 0.701 | -0.21 | 0.81 | 0.326 | 0.909 |
| ANB (°) | 4.29 | 2.84 | 3.40 | 1.44 | 0.289 | -0.40 | 1.07 | 0.014* | -0.26 | 0.96 | 0.311 | 0.173 |
| SN-MP (°) | 37.64 | 5.93 | 36.39 | 6.21 | 0.578 | -0.21 | 2.63 | 0.758 | -0.32 | 2.03 | 0.551 | 0.901 |
| SN-PP (°) | 4.04 | 4.30 | 3.71 | 2.88 | 0.809 | 0.19 | 1.35 | 0.600 | -0.09 | 1.44 | 0.806 | 0.587 |
| SN-OP (°) | 17.97 | 3.66 | 19.05 | 3.62 | 0.424 | 4.11 | 2.27 | <0.001* | 0.25 | 1.45 | 0.521 | <0.001* |
| AFH (N-ANS) (mm) | 127.67 | 7.27 | 128.19 | 7.32 | 0.849 | -1.02 | 2.78 | 0.177 | -0.67 | 2.28 | 0.272 | 0.712 |
| LAFH (ANS-Me) (mm) | 67.41 | 5.37 | 66.21 | 4.53 | 0.514 | -0.79 | 3.05 | 0.331 | -0.09 | 1.30 | 0.785 | 0.424 |
| LAFH/AFH (%) | 56.80 | 2.17 | 54.46 | 2.29 | 0.008* | -0.29 | 1.35 | 0.425 | 0.22 | 1.17 | 0.480 | 0.282 |
| PFH (S-Go) (mm) | 81.15 | 4.06 | 81.09 | 5.73 | 0.977 | 0.39 | 2.96 | 0.621 | 1.32 | 1.82 | 0.014* | 0.309 |
#Independent t test, ##paired t test, *statistically significant difference
Table 2: Skeletal measurements before retraction (T0) and the changes during retraction (T1-T0) in groups A and B.
| Variable | T0 | T1-T0 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group A | Group B | P# | Group A | Group B | P# | |||||||||
| Mean | SD | Mean | SD | Mean | SD | P## | Mean | SD | P## | |||||
| U1t-Sv (mm) | 63.39 | 4.15 | 60.74 | 6.57 | 0.200 | -5.99 | 1.06 | <0.001* | -5.64 | 1.06 | <0.001* | 0.378 | ||
| U1r-Sv (mm) | 51.45 | 4.21 | 49.74 | 4.69 | 0.304 | -1.51 | 0.71 | <0.001* | -2.10 | 1.49 | <0.001* | 0.179 | ||
| U1t-H (mm) | 69.90 | 3.19 | 69.49 | 5.04 | 0.791 | 0.68 | 1.22 | 0.049* | 0.77 | 1.67 | 0.094 | 0.862 | ||
| U1r-H (mm) | 52.59 | 3.20 | 52.91 | 5.43 | 0.846 | 1.05 | 1.30 | 0.008* | 0.27 | 1.56 | 0.518 | 0.148 | ||
| U6t-Sv (mm) | 38.21 | 4.04 | 35.32 | 5.37 | 0.108 | -0.36 | 0.79 | 0.101 | 0.83 | 0.94 | 0.004* | 0.001* | ||
| U6r-Sv (mm) | 37.08 | 3.52 | 35.45 | 4.05 | 0.249 | 1.33 | 0.64 | 0.006* | -0.89 | 1.50 | 0.038* | 0.010* | ||
| U6t-H (mm) | 65.83 | 3.53 | 63.49 | 5.03 | 0.151 | -2.74 | 0.50 | <0.001* | 0.70 | 1.47 | 0.086 | <0.001* | ||
| U6r-H (mm) | 51.95 | 3.28 | 50.77 | 5.35 | 0.474 | -1.98 | 0.67 | <0.001* | 0.69 | 1.60 | 0.116 | <0.001* | ||
| U1-SN (°) | 110.55 | 2.92 | 113.89 | 4.52 | 0.024 | -9.58 | 3.50 | <0.001* | -9.77 | 2.68 | <0.001* | 0.871 | ||
| U6-SN (°) | 69.05 | 4.18 | 67.15 | 5.43 | 0.292 | -6.97 | 2.45 | <0.001* | 1.13 | 5.17 | 0.410 | <0.001* | ||
| Overbite (mm) | 1.35 | 1.95 | 1.47 | 2.11 | 0.866 | 0.80 | 1.30 | 0.032* | -0.07 | 2.05 | 0.892 | 0.177 | ||
| Overjet (mm) | 4.29 | 1.01 | 4.65 | 1.20 | 0.381 | -1.45 | 0.94 | <0.001* | -1.34 | 1.04 | <0.001* | 0.771 | ||
| U1-L1 (°) | 112.67 | 6.07 | 113.08 | 7.21 | 0.869 | 17.75 | 5.78 | <0.001* | 15.69 | 5.89 | <0.001* | 0.341 | ||
| IMPA (°) | 99.91 | 4.99 | 102.52 | 6.85 | 0.245 | -8.83 | 3.40 | <.001* | -9.56 | 6.83 | <0.001* | 0.716 | ||
#Independent t test, ##paired t test, *statistically significant difference
Table 3: Dental measurements before retraction (T0) and the changes during retraction (T1-T0) in groups A and B
| Variable | T0 | T1-T0 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group A | Group B | P# | Group A | Group B | P# | ||||||||
| Mean | SD | Mean | SD | Mean | SD | P## | Mean | SD | P## | ||||
| Nasolabial angle (°) | 94.96 | 7.99 | 95.39 | 7.86 | 0.882 | 7.30 | 3.55 | <0.001* | 6.63 | 3.83 | <0.001* | 0.625 | |
| Ls-E line (mm) | 2.80 | 1.69 | 2.17 | 0.79 | 0.210 | -2.84 | 1.05 | <0.001* | -2.36 | 0.96 | <0.001* | 0.200 | |
| Li-E line (mm) | 4.51 | 1.95 | 3.26 | 1.38 | 0.053 | -2.77 | 0.71 | <0.001* | -2.40 | 0.69 | <0.001* | 0.157 | |
#Independent t test, ##paired t test, *statistically significant difference
Table 4: Soft-tissue measurements before retraction (T0) and the changes during retraction (T1-T0) in groups A and B
As shown in Table 2, there was no significant difference in the anteroposterior changes between the two groups. Vertically, the changes in the SN-MP and SN-PP angles also were not significantly different between the groups. However, the SN-OP angle showed a significant increase (4.11°, p<0.001) in group A compared with that in group B (p<0.001).
As shown in Table 3, the incisor crown showed statistically significant distal movement in group A (−5.99 mm, p<0.001) and group B (−5.64 mm, p<0.001), and the amount of the root apex distal movement was 1.51 mm (p<0.001) in group A and 2.10 mm (p<0.001) in group B. Meanwhile, the maxillary incisor angle (U1-SN) was significantly decreased in both groups (−9.58°, −9.77°, p<0.001, respectively). The incisors (U1t-H) were significantly extruded 0.68 mm in group A and 0.77 mm in group B. There was no significant difference in the anteroposterior or vertical movement of the incisors between the two groups.
The anteroposterior movement of the molars crown in group A was non-significant (−0.36 mm). However, the maxillary molars crown showed mesial movement (0.83 mm) in group B. Meanwhile, the molars root showed mesial movement (1.33 mm) in group A and distal movement (−0.89 mm) in group B. The molars inclined distal (U6-SN) significantly (−6.97°, p<0.001) in group A and showed no significant changes in group B. The molars (U6t-H) were significantly intruded (−2.74 mm, p<0.001) in group A, but there was no significant vertical movement in group B.
As shown in Table 4, the soft-tissue parameter changes, including nasolabial angle increases, Ls-E line and Li-E line decreases, were statistically significant in both groups (p<0.001) but there was no significant difference between the two groups.
All subjects in this prospective RCT were adults to eliminate growth effect and that the molar's physiologic mesial movement could be ignored[23]. Patients were randomly assigned and cephalometric analysis was performed blindly to eliminate examiner bias. Therefore, this RCT was reliable for detecting the true differences in the cephalometric changes during space closure between direct and indirect mini-implant anchorage. We found remarkable anterior teeth retraction, lingual crown tipping, and significantly relatively extrusion in both groups. The crown tipping may have occurred because the retraction point was located lower than the center of the resistance of the upper anterior teeth when using direct or indirect anchorage, indicating that lingual root torque or increased the length of crimpable hooks are needed to ensure bodily movement of incisors when necessary[24-28]. However, the vertical change of upper incisors during retraction using direct anchorage, still remain controversial. Upadhyay et al.[4,5] stated that direct mini-implant anchorage led to intrusion of the maxillary incisors. Lee et al.[14] reported that the vertical position of the incisal edge did not change significantly during the retraction period, however results in present study showing the relative extrusion of maxillary incisors. Therefore, during sliding, to avoid extruding when distalize anterior teeth, it is better to incorporate a curve of Spee into the archwire[29].
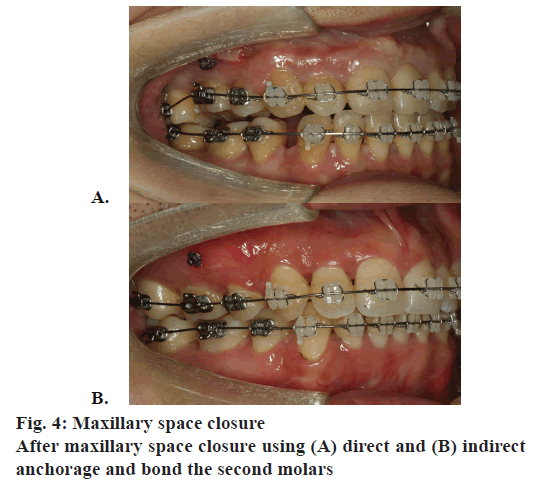
In the current study, the anchorage loss with indirect mini-implant anchorage was 0.83 mm, which was similar to Monga’s findings[19] and are nearly equivalent to those of direct anchorage. The molars were distally tipped significantly in the direct anchorage group. This result may be caused by the frictional force between archwire and appliance on the posterior teeth. But the frictional force was offset by the mesial elastic force loaded on molars in the indirect group. Forward movement and intrusion of the posterior teeth after premolar extraction leads to a reduction in the vertical dimension, which is known as the “wedge effect”[30]. Since the molars can be almost stable anteroposteriorly when using mini-implant anchorage, the vertical movement of posterior teeth is the main influencing factor in the vertical dimension. In group A, the first molar was intruded by 2.74 mm, this result may attribute to the vertical components of the retract force. However, the SN-MP angle showed no significant decrease after space closure. A reason for this outcome might be that only the first molars were intruded, while the second molars did not bond to the appliance and still had occlusion. This undesired localized open bite of the first molars needed to be corrected in subsequent phases via bonding the second molars or intermaxillary elastics in posterior segments and, in turn, may increase the duration of treatment or induce other unfavorable tooth displacement. Fig. 4A shows that after maxillary space closure using direct mini-implant anchorage, the first maxillary molar was intruded. Moreover, the extrusion of the anterior teeth limited the counter-clockwise rotation of the mandible. Therefore, intrusions of both posterior and anterior teeth are needed to improve the vertical dimension in hyperdivergent patients, and mini-implants placed in the maxillary anterior region are also necessary[12,14,28].
The occlusal plane was found to show a clockwise rotation in group A, which was attributed to the intrusion of molars and relative extrusion of anterior teeth and is in line with the results of Finite element method (FEM) studies[15-24]. Nevertheless, the occlusal plane was stable in group B, which resulted from few vertical changes in anterior and posterior teeth. Fig. 4B shows that after maxillary space closure using indirect mini-implant anchorage, the upper arch was stable. Therefore, standard sliding mechanics can be obtained with indirect anchorage to enable good biomechanical control of the teeth[19].
In this study, the mean duration of space closure in the upper arches due to direct mini-implant anchorage was longer than indirect anchorage, despite the distances of spaces being similar (Table 1). A possible explanation might be that the retraction force generated by direct mini-implant anchorage was upward and backward, thus producing both horizontal and vertical components of force, which may lead to deflection of the archwire[24,25], resulting in increased friction on the posterior segments. Another possible reason was that more mini-implants failures in the direct anchorage group, which may lead to an increase in treatment time.
During retraction, no mini-implants failure was observed in group B. Consistent with our results, Holberg[18] analysed the biomechanical differences between direct and indirect anchorage and their effects on the primary stability of the mini-implants and found that indirect mini-implant anchorage was reliable for reducing peri-implant loading of the bone and the risk of losing the mini-implants. Furthermore, better oral hygiene related to the power chain not directly attaching to mini-implant’s head might be another reason for the reduced plaque around the mini-implants, which in turn, lowered the risk of inflammation around the implant sites. However, a larger sample size and statistical analysis are needed to further investigate the stability of different loaded mini-implant anchorage.
Depending on the position of tooth which force apply to, buccolingual change of posterior segment will be different. The current study was conducted on twodimensional lateral cephalograms, and thus, transverse changes cannot be explored due to their inherent shortcomings. In future study, it is necessary to further investigate the ultimate clinical effect using conebeam computed tomography. In conclusions, both direct and indirect mini-implant anchorage can provide successful anchorage and induce favourable profile changes. In this study, indirect mini-implant anchorage which caused less archwire deformation and molars intrusion, enabled better sliding mechanics compared to direct anchorage.
Acknowledgements:
The present study was supported by the International Scientific and Technological Cooperation and Exchange (grant no. 2014DFA31520).
References
- Melsen B, Bosch C. Different approaches to anchorage: a survey and an evaluation. Angle Orthod 1997;67:23-30.
- Block MS, Hoffman DR. A new device for absolute anchorage for orthodontics. Am J Orthod Dentofacial Orthop 1995;107:251-8.
- Park HS. The skeletal cortical anchorage using titanium microscrew implants. Korean J Orthod 1999;29:699-706.
- Upadhyay M, Yadav S, Patil S. Mini-implant anchorage for en-masse retraction of maxillary anterior teeth: a clinical cephalometric study. Am J Orthod Dentofacial Orthop 2008;134:803-10.
- Upadhyay M, Yadav S, Nagaraj K, Patil S. Treatment effects of mini-implants for en-masse retraction of anterior teeth in bialveolar dental protrusion patients: A randomized controlled trial. Am J Orthod Dentofacial Orthop2008;134:18-29.
- Xu Y, Xie J. Comparison of the effects of mini-implant and traditional anchorage on patients with maxillary dentoalveolar protrusion. Angle Orthod 2017; 87:320-7.
- Antoszewska-Smith J, Sarul M, ?yczek J, Konopka T, Kawala B. Effectiveness of orthodontic miniscrew implants in anchorage reinforcement during en-masse retraction: A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop 2017;151:440-55.
- Lee J, Miyazawa K, Tabuchi M, Sato T, Kawaguchi M, Goto S. Effectiveness of en-masse retraction using midpalatal miniscrews and a modified transpalatal arch: Treatment duration and dentoskeletal changes. Korean J Orthod 2014;44:88-95.
- Antoszewska J, Trze?niewska P, Kawala B, Ludwig B, Park HS. Qualitative and quantitative evaluation of root injury risk potentially burdening insertion of miniscrew implants. Korean J Orthod 2011;41:112-20.
- Stanford N. Mini-screws success rates sufficient for orthodontic treatment. Evid Based Dent 2011;12:19.
- Park HS, Lee SK, Kwon OW. Group distal movement of teeth using microscrew implant anchorage. Angle Orthod 2005;75:602–9.
- Kim TW, Kim H, Lee SJ. Correction of deep overbite and gummy smile by using a mini implant with a segmented wire in a growing Class II Division 2 patient. Am J Orthod Dentofacial Orthop 2006;130:676-85.
- Lee SK, Abbas NH, Bayome M, Baik UB, Kook YA, Hong M, et al. A comparison of treatment effects of total arch distalization using modified C-palatal plate vs buccal miniscrews. Angle Orthod 2018;88:45-51.
- Lee KJ, Park YC, Hwang CJ, Kim YJ, Choi TH, Yoo HM, et al. Displacement pattern of the maxillary arch depending on miniscrew position in sliding mechanics. Am J Orthod Dentofacial Orthop 2011;140:224-32.
- Song JW, Lim JK, Lee KJ, Sung SJ, Chun YS, Mo SS. Finite element analysis of maxillary incisor displacement during en-masse retraction according to orthodontic mini-implant position. Korean J Orthod 2016;46:242-52.
- Singh S, Mogra S, Shetty VS, Shetty S, Philip P. Three-dimensional finite element analysis of strength, stability, and stress distribution in orthodontic anchorage: a conical, self-drilling miniscrew implant system. Am J Orthod Dentofacial Orthop 2012;141:327-36.
- Fritz U, Ehmer A, Diedrich P. Clinical suitability of titanium microscrews for orthodontic anchorage-preliminary experiences. J Orofac Orthop 2004;65:410-8.
- Holberg C, Winterhalder P, Holberg N, Rudzki-Janson I, Wichelhaus A. Direct versus indirect loading of orthodontic miniscrew implants-an FEM analysis. Clin Oral Investig 2013;17:1821-7.
- Monga N, Kharbanda OP, Samrit V. Quantitative and qualitative assessment of anchorage loss during en-masse retraction with indirectly loaded miniscrews in patients with bimaxillary protrusion. Am J Orthod Dentofacial Orthop 2016;150:274-82.
- Choi NC, Park YC, Lee HA, Lee KJ. Treatment of Class II protrusion with severe crowding using indirect miniscrew anchorage. Angle Orthod 2007;77:1109-18.
- Andrews LF. The six keys to normal occlusion. Am J Orthod 1972;62:296-309.
- Andrews LF. Straight Wire: the Concept and the Appliance. San Diego: LA Wells; 1989.
- Kuroda S, Yamada K, Deguchi T, Kyung HM, Takano-Yamamoto T. Class II malocclusion treated with miniscrew anchorage: comparison with traditional orthodontic mechanics outcomes.Am J Orthod Dentofacial Orthop 2009;135:302-9.
- Tominaga JY, Tanaka M, Koga Y, Gonzales C, Kobayashi M, Yoshida N. Optimal loading conditions for controlled movement of anterior teeth in sliding mechanics. Angle Orthod 2009;79:1102-7.
- Kojima Y, Kawamura J, Fukui H. Finite element analysis of the effect of force directions on tooth movement in extraction space closure with miniscrew sliding mechanics. Am J Orthod Dentofacial Orthop 2012;142:501-8.
- Lee D, Heo G, El-Bialy T, Carey JP, Major PW, Romanyk DL. Initial forces experienced by the anterior and posterior teeth during dental-anchored or skeletal-anchored en masse retraction in vitro. Angle Orthod 2017;87:549-55.
- Al-Sibaie S, Hajeer MY. Assessment of changes following en-masse retraction with mini-implants anchorage compared to two-step retraction with conventional anchorage in patients with class II division 1 malocclusion: a randomized controlled trial. Eur J Orthod 2014;36:275-83.
- Namburi M, Nagothu S, Kumar CS, Chakrapani N, Hanumantharao CH, Kumar SK. Evaluating the effects of consolidation on intrusion and retraction using temporary anchorage devices - a FEM study. Prog Ortho 2017;18:2-12.
- Song HS. Three-dimensional finite element analysis of tooth axis of maxillary anterior teeth during retraction with microimplant. MSD thesis. Daegu, Korea: Kyungpook National University; 2006.
- Isaacson JR, Isaacson RJ, Speidel TM, Worms FW. Extreme variation in vertical facial growth and associated variation in skeletal and dental relations. Angle Orthod 1971;41:219-29.