- *Corresponding Author:
- Jianhong Chen
Department of Anesthesiology
General Hospital of Medical Community
Keqiao District Hospital of Traditional Chinese Medicine
Shaoxing, Zhejiang 312060, China
E-mail: shu4233727@126.com
| This article was originally published in a special issue, “Trending Topics in Biomedical Research and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2022:84(1) Spl Issue “190-195” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To observe the effects of sufentanil/fentanyl combined with propofol on the stress response and hemodynamics in patients with hypertensive intracerebral hemorrhage. The control group received anesthesia with fentanyl plus propofol, while the observational group received sufentanil plus propofol. The hemodynamic measures, including diastolic blood pressure, systolic blood pressure, heart rate and stress response measures, including plasma angiotensin II, aldosterone and serum norepinephrine, in the two groups 5 min before induction of anesthesia (T0), at endotracheal intubation (T1), 5 min after endotracheal intubation (T2) and at postoperative extubation (T3) were compared, and the anesthesia recovery and adverse reactions in the two groups after surgery were also compared. At T0~T3, the DBP, SBP and HR in the observational group fluctuated less than the control group (p<0.05). At T1, T2 and T3, the plasma angiotensin II, aldosterone and serum norepinephrine in the observational group were lower than those in the control group (p<0.05). There were no significant differences between the groups in the extubation time, awakening time and spontaneous breathing recovery time after surgery (p>0.05). The incidence of adverse reactions in the observational group was 12.24 % (6/49), lower than that in the control group 29.17 % (14/48) (p<0.05). Sufentanil-propofol anesthesia for patients with hypertensive intracerebral hemorrhage can steady intraoperative hemodynamic status, relieve stress responses of the body, reduce the incidence of adverse reactions and does not affect postoperative anesthesia recovery.
Keywords
Hypertensive intracerebral hemorrhage, sufentanil, fentanyl, propofol, hemodynamics
Hypertensive Intracerebral Hemorrhage (HICH) is a kind of cardio-cerebrovascular disease with a high incidence and mostly diagnosed in middle-aged and old people. Data show that it accounts for about 10 %~40 % of acute cerebrovascular diseases and has a tendency of increase in recent years. HICH is characterized by sudden onset, rapid disease progression and high mortality. Some documents show that the mortality can reach 30 %~50 %, 1 mo after its onset, and ranking first among the causes of death caused by cerebrovascular diseases[1,2]. Hematoma removal surgery is currently the first choice for clinical treatment of HICH, which can effectively remove the hematoma, lower intracranial pressure, improve brain functions and reduce the rates of disability and cause fatality. However, due to the high risk of the procedure, some anesthesia intervention should be given to alleviate the pain degree of patients and reduce the risk of the surgery[3]. Therefore, in order to ensure patient’s perioperative safety, it becomes particularly important to choose an appropriate anesthesia plan which can suppress the body’s stress responses and maintain steady intraoperative hemodynamics. Propofol, as one of the ultra-short acting opioid anesthetics, has superior sedative and hypnotic effects and can lower intracranial pressure, protect the functional completeness of the mitochondrial sodium-potassium pump in cells, and reduce the incidence of cytotoxic cerebral edema. However, the analgesic effect is poor and the combination with opioid analgesics are often needed[4,5]. Sufentanil is an opioid analgesic with significantly superior analgesic intensity to fentanyl, high lipophilicity, less accumulation in the body and increased safety[6]. Therefore, this study attempted to apply sufentanil-propofol anesthesia to the surgical treatment of HICH patients and compared it with fentanyl-propofol anesthesia, with a view to analyzing the effects on patient’s stress responses and hemodynamics.
Materials and Methods
General data:
97 patients with HICH admitted to our hospital from March 2019 to March 2021 were selected and divided into a control group and an observational group according to the random number table method.
Control group include 48 cases, including 28 females and 30 males, aged 48 to 69 y, mean (57.60±7.90) y; cerebral hematoma volume 36~78 ml, mean (51.71±10.31) ml; hypertension stage include stage 1 (23 cases), stage 2 (14 cases) and stage 3 (11 cases); location of bleeding include lobar hemorrhage (11 cases), putaminal hemorrhage (24 cases) and thalamic hemorrhage (13 cases).
Observational group include 49 cases, including 26 females and 33 males, aged 49 to 68 y, mean (56.80±7.70) y; cerebral hematoma volume 35~77 ml, mean (51.81±10.11) ml; hypertension stage include stage 1 (24 cases), stage 2 (13 cases) and stage 3 (12 cases); location of bleeding include lobar hemorrhage (12 cases), putaminal hemorrhage (25 cases) and thalamic hemorrhage (12 cases). There were no statistically significant differences in the general data (sex, age, cerebral hematoma volume, hypertension stage and location of bleeding) between the groups (p>0.05).
Inclusion criteria:
Met the diagnostic criteria for HICH in Neurology (7th edition); underwent hematoma removal surgery; it was the first onset; the onset time did not exceed 24 h; knew this study and voluntarily signed the informed consent form.
Exclusion criteria:
Abnormal coagulation function; complicated with brain tumors or cerebral arteriovenous malformations; infectious diseases such as pulmonary tuberculosis; abnormal liver and kidney functions; long-term use of drugs affecting the neuropsychiatric functions; accompanied by serious cardiovascular disease; dilation of bilateral pupils or symptoms of brain herniation; intracerebral hemorrhage caused by traumatic brain injury among others; complicated with brain tumors; respiratory failure; accompanied by severe cognitive disorders.
Methods:
Anesthesia methods: After patients in both groups enter the operating room, routinely monitor their Electrocardiogram (ECG), Partial Pressure of Oxygen (PaO2), End Tidal Carbon Dioxide (ETCO2) and Heart Rate (HR), and establish venous access. Perform radial artery puncture and catheterization under local anesthesia and monitor Invasive Blood Pressure (IBP) in real time.
Control group: Anesthesia with fentanyl (Langfang Branch of China National Pharmaceutical Industry Corporation Ltd., SFDA Approval No. H20123297) plus propofol (Xi'an Libang Pharmaceutical Co., Ltd., SFDA Approval No. H20010368). Induction of anesthesia is done. Inject fentanyl at 3~4 μg/kg, cisatracurium (Jiangsu Hengrui Medicine Co., Ltd., State Food and Drug Administration’s (SFDA) approval No. H20060869) at 0.15~0.2 mg/kg, propofol 1.5~2 mg/kg and midazolam (Jiangsu Nhwa Pharmaceutical Co., Ltd., SFDA approval No. H10980025) at 0.05 mg/ kg; after completion of induction, perform endotracheal intubation and connect an anesthesia machine for mechanical ventilation. Maintenance of anesthesia is done through the Intravenous (IV) infusion pump of propofol at 5~6 mg/kg/h and fentanyl at 2 μg/kg/h, and inject 5 ml cisatracurium every 0.5 h.
Observational group: Anesthesia with sufentanil (Yichang Humanwell Pharmaceutical Co., Ltd., SFDA Approval No. H20054171) plus propofol. Induction of anesthesia-Inject sufentanil at 0.8 μg/kg, cisatracurium at 0.15~0.2 mg/kg, propofol 1.5~2 mg/kg, and midazolam at 0.05 mg/kg; after completion of induction, perform endotracheal intubation and connect an anesthesia machine for mechanical ventilation. Maintenance of anesthesia is done through the IV infusion pump of propofol at 0.3 mg/kg/h and sufentanil at 0.35 μg/kg/h, and inject 5 ml cisatracurium every 0.5 h.
Apply the Bispectral Index (BIS) in both groups to monitor the depth of anesthesia in real time during the operation and properly adjust the dose of anesthetics to maintain the BIS value at 45~60. Stop sufentanil/ fentanyl 0.5 h before the end of the operation and stop propofol 5 min before the end of the operation, when the patient has spontaneous breathing after surgery, use atropine plus neostigmine to go against residual muscle relaxation.
Determination of blood measures: Take 5 ml of sample early morning, fasting venous blood from the groups and take 2 ml for centrifugation for about 10 min (rotational speed: 3000 r/min); determine serum Norepinephrine (NE) levels by radioimmunoassay; centrifuge the remaining 3 ml to determine the levels of plasma Angiotensin II (Ang II) and Aldosterone (ALD); the kits were purchased from Shanghai Enzyme-linked Biotechnology Co., Ltd., and the operation was strictly carried out in accordance with the kit instructions.
Observation measures:
Hemodynamic measures (Diastolic Blood Pressure (DBP), Systolic Blood Pressure (SBP) and HR) in both groups 5 min before induction of anesthesia (T0), at endotracheal intubation (T1), 5 min after endotracheal intubation (T2) and at postoperative extubation (T3); stress response measures (plasma Ang II, ALD and serum NE) in the two groups at T0, T1, T2 and T3; postoperative anesthesia recovery in the two groups, including extubation time, awakening time and spontaneous breathing recovery time after surgery; occurrence of adverse reactions (such as hypotension, hypertension, bradycardia, tachycardia and respiratory depression) in the two groups.
Statistical analysis:
Statistical Package for the Social Sciences (SPSS) 21.0 was used for data processing. Measurement data were denoted by mean±standard deviation (x̄±s) and were compared with the independent samples t-test between groups and with the paired t-test within groups. Count data were expressed by n (%) and compared with the χ2 test between groups. Statistical significance could be attained when the p value was less than 0.05.
Results and Discussion
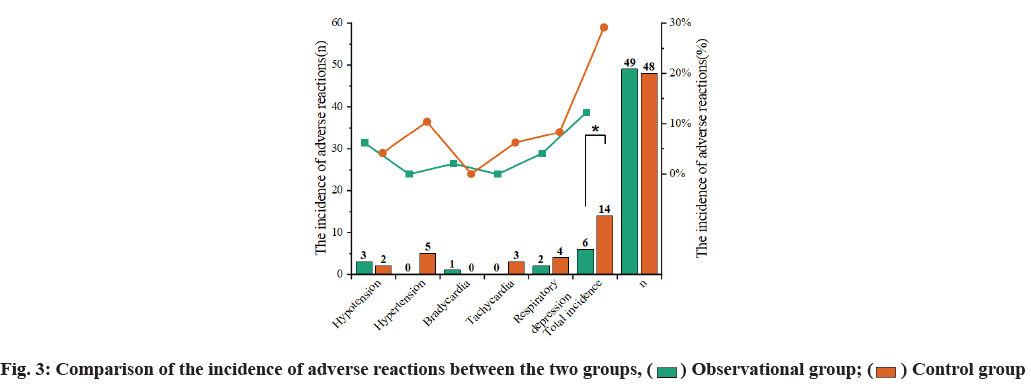
Hemodynamic measures at different time points were compared. At T0, there were no significant differences in DBP, SBP and HR between the two groups (p>0.05). At T1, T2 and T3, the DBP, SBP and HR in the two groups were all lower than those at T0 (p<0.05). At T0~T3, the DBP, SBP and HR in the observational group fluctuated less than the control group (p<0.05) (fig. 1).
Stress response measures at different time points were compared. At T0, the plasma Ang II, ALD and serum NE in the two groups had no statistically significant differences (p>0.05). At T1, T2 and T3, the plasma Ang II, ALD and serum NE in the observational group had no statistically significant differences with those at T0 (p>0.05). At T1, T2 and T3, the plasma Ang II, ALD and serum NE in the observational group were lower than those in the control group (p<0.05) (Table 1).
| Measure | Group | n | T0 | T1 | T2 | T3 |
|---|---|---|---|---|---|---|
| Ang II (μg/l) | Observational group | 49 | 33.20±5.62 | 34.44±5.90 | 35.19±6.27 | 35.58±6.73 |
| Control group | 48 | 33.46±5.28 | 38.72±5.93 | 40.87±6.31 | 42.10±7.25 | |
| t-value | 0.240 | 3.659 | 4.566 | 4.713 | ||
| p value | 0.811 | 0.000 | 0.000 | 0.000 | ||
| ALD (ng/l) | Observational group | 49 | 217.41±26.23 | 221.07±27.86 | 224.84±28.22 | 227.75±28.82 |
| Control group | 48 | 218.92±25.74 | 239.99±26.63a | 243.70±26.20a | 248.93±26.91a | |
| t-value | 0.293 | 3.634 | 3.498 | 3.836 | ||
| p value | 0.771 | 0.000 | 0.000 | 0.000 | ||
| NE (ng/l) | Observational group | 49 | 319.75±26.16 | 323.41±31.80 | 326.86±32.24 | 330.42±33.55 |
| Control group | 48 | 320.57±27.30 | 345.52±29.75a | 360.74±34.22a | 367.66±36.18a | |
| t-value | 0.156 | 3.626 | 5.147 | 5.391 | ||
| p value | 0.875 | 0.000 | 0.000 | 0.000 |
Note: Compared with those of the same group at T0, ap<0.05
Table 1: Comparison of Stress Response Measures between the Two Groups at Different Time Points
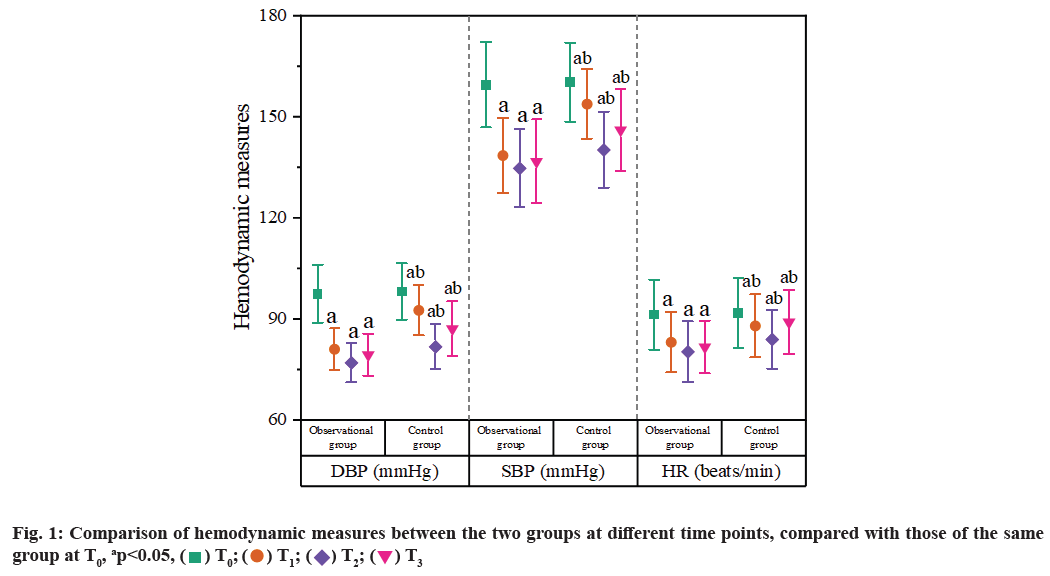
Postoperative anesthesia recovery between two groups was compared. There were no significant differences between the groups in the extubation time, awakening time and spontaneous breathing recovery time after surgery (p>0.05) (fig. 2).
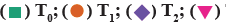
The incidence of adverse reactions in the observational group was 12.24 % (6/49), lower than that in the control group 29.17 % (14/48) (p<0.05) (fig. 3).
HICH can cause a series of damages such as brain tissue compression, intracranial hypertension, brain herniation, cerebral edema and dysfunction. The condition is extremely dangerous and has a high case fatality rate[7,8]. Surgery can effectively remove intracranial hematoma, lower intracranial pressure, relieve injuries secondary to hemorrhage and reduce the case fatality rate[9]. Clinical practice suggests that the surgery is relatively traumatic and has strong stimulation which may lead to strong stress responses, so there is a high risk in the surgery and anesthesia[10]. Therefore, in order to ensure the smooth operation and improve the prognosis of patients, it is of great significance to find a safe and effective anesthesia plan to maintain steady hemodynamics and reduce stress responses.
Propofol has a good sedative and hypnotic effect, a high clearance rate and a quick recovery after drug withdrawal[11]. Research also points out that propofol can effectively lower intracranial pressure, adjust the metabolism of brain cells, reduce the cerebral oxygen consumption and protect the functional completeness of the mitochondrial sodium-potassium pump in cells, avoid the water-sodium retention caused by mitochondrial swelling and disintegration, and reduce the risk of cytotoxic cerebral edema and has been widely used in anesthesia for intracerebral hemorrhage surgery[12]. However, due to the poor analgesic effect, propofol is often used in combination with opioid analgesics.
Sufentanil and fentanyl are opioid analgesics. The former is highly selective to mu (μ1) receptor and is the most powerful analgesic agent in the fentanyl family. The analgesic intensity of sufentanil is 5~10 times than that of fentanyl and the lipophilicity is about 2 times that of fentanyl. Furthermore, sufentanil can more easily go through the cell membrane and blood-brain barrier, and has a high binding rate with plasma proteins. Sufentanil is bio-transformed into metabolites in liver tissues and then metabolized in the kidney into some intermediates which still have certain activity and thus allow the drug to play a rapid and lasting analgesic effect. The low body accumulation also makes the drug safer. In addition, studies have shown that, compared with fentanyl, isodose sufentanil can more effectively reduce the distribution and clearance of propofol, improve plasma concentration, reduce baroreceptor sensitivity and maintain steady blood circulation. Jin et al. in their study pointed out that anesthesia with sufentanil plus propofol for brain surgery can effectively reduce cardiovascular stress responses and maintain steady hemodynamics[13]. This study showed that there were no significant differences between the groups in the extubation time, awakening time and spontaneous breathing recovery time after surgery (p>0.05). At T1, T2 and T3, the DBP, SBP and HR in the two groups were all lower than those at T0 (p<0.05), and at T0~T3, the DBP, SBP and HR in the observational group fluctuated less than the control group (p<0.05). These results showed that sufentanil-propofol anesthesia could steady the intraoperative hemodynamic status of patients without affecting the postoperative anesthesia recovery.
In addition, the concentration of catecholamine in the blood of patients undergoing surgery is one of the important measures reflecting the stress response of the body. The increase in the release of catecholamines such as NE and epinephrine can have a significant impact on the cardiovascular system, resulting in changes in metabolism and hemodynamics[14]. At the same time, the renin-angiotensin system can affect vascular functions and the metabolic regulation system and its regulatory effect on the body is closely related to the concentration of Ang II and ALD in plasma[15]. This study showed that at T1, T2 and T3, the plasma Ang II, ALD and serum NE in the observational group had no statistically significant differences with those at T0 (p>0.05). At T1, T2 and T3, the plasma Ang II, ALD and serum NE in the observational group were lower than those in the control group (p<0.05). These suggested that sufentanil-propofol anesthesia can significantly reduce the stress responses of the body. The possible reason is that sufentanil can reduce the levels of catecholamine, ADH and other measures in blood by down-regulating the excitability of the hypothalamic vasomotor center and sympathetic nerve. This study also found that the incidence of adverse reactions in the observational group was lower than that in the control group (p<0.05), suggesting that sufentanil-propofol anesthesia can reduce the incidence of adverse reactions.
In conclusion, sufentanil-propofol anesthesia for patients with HICH can steady intraoperative hemodynamic status, relieve stress responses of the body, reduce the incidence of adverse reactions and does not affect postoperative anesthesia recovery. Due to the small sample size of this study, whether the results are representative still needs further exploration by expanding the clinical sample size.
Conflict of interests:
The authors declared no conflict of interest.
References
- Xu X, Chen X, Li F, Zheng X, Wang Q, Sun G, et al. Effectiveness of endoscopic surgery for supratentorial hypertensive intracerebral hemorrhage: A comparison with craniotomy. J Neurosurg 2017;128(2):553-9.
[Crossref] [Google Scholar] [PubMed]
- Ye Z, Ai X, Hu X, Fang F, You C. Comparison of neuroendoscopic surgery and craniotomy for supratentorial hypertensive intracerebral hemorrhage: A meta-analysis. Medicine 2017;96(35): e7876.
[Crossref] [Google Scholar] [PubMed]
- Fontana J, Scharf J, Weiß C, Schmieder K, Barth M. The spontaneous arterial blood pressure rise after aneurysmal subarachnoid hemorrhage-A biphasic phenomenon. Clin Neurol Neurosurg 2015;137:22-7.
[Crossref] [Google Scholar] [PubMed]
- Kawamata T, Okada Y, Kawashima A, Yoneyama T, Yamaguchi K, Ono Y, et al. Postcarotid endarterectomy cerebral hyperperfusion can be prevented by minimizing intraoperative cerebral ischemia and strict postoperative blood pressure control under continuous sedation. Neurosurgery 2009;64(3):447-54.
[Crossref] [Google Scholar] [PubMed]
- Sun S, Li Y, Zhang H, Wang X, She L, Yan Z, et al. The effect of mannitol in the early stage of supratentorial hypertensive intracerebral hemorrhage: A systematic review and meta-analysis. World Neurosurg 2019;124:386-96.
[Crossref] [Google Scholar] [PubMed]
- Rasras S, Safari H, Zeinali M, Jahangiri M. Decompressive hemicraniectomy without clot evacuation in supratentorial deep-seated intracerebral hemorrhage. Clin Neurol Neurosurg 2018;174:1-6.
[Crossref] [Google Scholar] [PubMed]
- Xu X, Chen X, Li F, Zheng X, Wang Q, Sun G, et al. Erratum. Effectiveness of endoscopic surgery for supratentorial hypertensive intracerebral hemorrhage: A comparison with craniotomy. J Neurosurg 2017;128(2):649.
[Crossref] [Google Scholar] [PubMed]
- Lee KJ, Park C, Oh J, Lee B. Non-invasive detection of intracranial hypertension using a simplified intracranial hemo-and hydro-dynamics model. Biomed Eng Online 2015;14(1):1-2.
[Crossref] [Google Scholar] [PubMed]
- Samagh N, Bhagat H, Jangra K. Monitoring cerebral vasospasm: How much can we rely on transcranial doppler. J Anaesthesiol Clin Pharmacol 2019;35(1):12-8.
[Crossref] [Google Scholar] [PubMed]
- Gurney D. Are you using resuscitative endovascular balloon occlusion of the aorta (REBOA) for noncompressible hemorrhage? J Emerg Nurs 2019;45(3):329-31.
[Crossref] [Google Scholar] [PubMed]
- Millar K, Bowman AW, Burns D, McLaughlin P, Moores T, Morton NS, et al. Children's cognitive recovery after day‐case general anesthesia: A randomized trial of propofol or isoflurane for dental procedures. Pediatr Anesth 2014;24(2):201-7.
[Crossref] [Google Scholar] [PubMed]
- Yang LJ, Cui JL, Wu TM, Wu JL, Fan ZZ, Zhang GS. Sequential therapy for non-thalamus supratentorial hypertensive intracerebral hemorrhages. Eur Rev Med Pharmacol Sci 2014;18(23):3653-8.
[Google Scholar] [PubMed]
- Shimamura N, Munakata A, Naraoka M, Nakano T, Ohkuma H. Decompressive hemi-craniectomy is not necessary to rescue supratentorial hypertensive intracerebral hemorrhage patients: Consecutive single-center experience. Acta Neurochir Suppl 2011;111:415-9.
[Crossref] [Google Scholar] [PubMed]
- Maira G, Anile C, Colosimo C, Rossi GF. Surgical treatment of primary supratentorial intracerebral hemorrhage in stuporous and comatose patients. Neurol Res 2002;24(1):54-60.
[Crossref] [Google Scholar] [PubMed]
- Nakagawa Y, Fujimoto N, Ueda S, Matsumoto K. Some aspects of CT findings of the acute stage in hypertensive supratentorial intracerebral hemorrhages related to their prognosis quoad vitam-a retrospective study (author’s transl). No To Shinkei 1981;33(3):251-7.
[Google Scholar] [PubMed]
 T3
T3
 Control group
Control group