- *Corresponding Author:
- W. Du
Department of Ultrasound, the People's Hospital of Shizhu County, Shizhu Chongqing 409100, China
E-mail: duwenhua316@163.com
| This article was originally published in a special issue, "Clinical and Experimental Studies on Drug and Intervention Repurposing in China |
| Indian J Pharm Sci 2019:81(4)spl issue1;50-57 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
In order to study the differences in the sensitivity of various types of detection during the diagnosis of different pathological types of breast mass by ultrasound breast imaging reporting and data system classification, 3000 patients with breast disease treated in a hospital were selected for research in this study. The selected patient data had ultrasound effects and subsequent biopsy pathology reports, and the patient's basic data were also counted. The detection methods used for patients include ultrasound breast imaging reporting and data system classification and pathological tissue biopsy. The results of the study showed that the sensitivity of the ultrasound breast imaging reporting and data system classification was 87.75 %, the specificity was 90.89 %, the accuracy was 91.04 %, the positive predictive value was 79.24 %, the negative predictive value was 96.13 %, and through the receiver operating characteristic curve, the ultrasonic breast imaging reporting and data system classification test was verified to be an excellent detection method. Ultrasound breast imaging reporting and data system grading is generally more accurate for benign tumors, and the accuracy of detecting malignant tumors is slightly lower. This study demonstrated the differences in the detection sensitivity of different types of breast masses by ultrasound breast imaging reporting and data system grading. It provided a theoretical basis for the physician to judge whether the patient needs biopsy after receiving the ultrasound test, avoiding the unnecessary suffering of pain of biopsy in all patients, and reducing the pressure on both patients and physicians. The findings of this study is expected to enable breast imaging reporting and data system grading detection to exert a better effect.
Keywords
Breast mass, breast cancer, BI-RADS classification, difference Analysis
At present, breast cancer has become one of the most common malignant tumors in female worldwide, and it is also an important cause of female death[1-5]. The aetiology and pathogenesis of breast cancer is still unclear. Some research has shown that the 5-y survival rate of breast cancer is 97 % in stage I, 75.9 % in stage II, and only 45 % in stage III. Therefore, if breast cancer is detected early and treated regularly, the long-term cure rate is relatively high. At present, there are no effective breast cancer prevention measures. Only through early diagnosis and timely treatment of the disease can the patient's mortality be reduced and the quality of life of the patient improved. Early detection, rapid diagnosis, and early selection of the best treatment are the key to prolonging the lives of patients with breast cancer[6,7].
Early breast cancer has no obvious clinical symptoms, most of which are diagnosed by imaging examination. Molybdenum target filming, magnetic resonance imaging (MRI) and ultrasonography are the most commonly used imaging methods at present. Mammary gland X-ray can detect abnormal nodules in soft tissue and is sensitive to calcification lesion[8-12]. However, most Chinese women have higher breast density. There is a lack of effective contrast between the lesion and the surrounding tissue, resulting in unclear imaging of the lesion, and it is easy to miss or misdiagnose some lesions when reading the image. Due to the radiation damage of the molybdenum target X-ray to the human body, in the standardized diagnosis and treatment of breast cancer, in the cases that the patient is young women under the age of 40, the risk factors are not clear or no abnormalities are found during the physical examination, the molybdenum target X-ray can’t be used as the first choice. Although MRI has the advantages of no radiation damage and high diagnostic rate, it is not suitable for routine screening because of its high cost. Ultrasonic high-frequency probes have advantages in screening dense breasts, and it is safe, inexpensive, easy to operate, and can be repeatedly examined[13]. Especially in recent years, ultrasound equipment and technology are constantly updated, with the development of color Doppler flow ultrasound technology, elastography and the application of ultrasound contrast agents, breast ultrasound has been the first choice for imaging screening, diagnosis and monitoring of breast diseases.
The manifestations of benign breast lesions and malignant lesions are very diverse. There are some repetitions of the ultrasound image features of the two different lesions[14-16]. Many reports are not very clear on the description of the lesion, which makes the diagnosis of doctors very difficult. This study relied on the breast imaging reporting and data system (BIRADS) classification method to distinguish breast masses and explores the sensitivity of ultrasound detection for different types and different classes of breast masses.
Materials and Methods
Research subjects:
Three thousand breast lesion patients with 3860 lesions revealed by ultrasound examination and admitted to a hospital during the period of April 2008-October 2016 were selected as the research subjects of this study[17-20]. The patients underwent a needle biopsy or surgical resection after the examination. Pathological examination of the lesion was performed and pathological results were confirmed. Pathological results obtained before ultrasound diagnosis were not included in this study data. The patients were all female and the age range was 18-75 y. In addition to the results of ultrasound examination, other data of subjects were also obtained, including the age, menstrual status, weight, long-term oral contraceptives administration and breast gland density.
Inspection method:
Multiple color diasonograph instruments equipped with high-frequency linear array probes were used and the probe frequency was 8~14 MHz. The Doppler blood flow setting of the instrument included, low pulse repetition frequency, in the absence of color artifacts, the wall filtration and flow rate range were adjusted as low as possible, so that the low-speed blood flow in the mass was displayed as the best, the color flow gain was adjusted to just appear color artifacts and then slightly adjusted to suppress artifacts by about 50 %[21]. The patient was placed in the supine position, and the hands were lifted high on the head side. After fully exposing the breasts and armpits, routine ultrasound examination was performed to scan the lesions in multiple directions and multiple angles. Special position, local pressure or enlarge photography were given when it is necessary. Ultrasound images were acquired and recorded on the workstation, and a final grading diagnosis was made[22,23].
Image analysis:
Breast lesions were classified by 2 to 3 experienced diagnosticians in radiology department. When the diagnosis was inconsistent, the result was discussed and a consensus was reached. The image was analysed according to the BI-RADS classification diagnostic criteria: the final evaluation and classification of breast lesions was performed using the following characteristics of the lesion[24]. Background echouniform, uneven; mass- shape ellipse, circle, irregular; position- transverse diameter greater than longitudinal diameter, longitudinal diameter greater than transverse diameter; edge- complete, incomplete, fuzzy, sharpangled, tiny lobulated, Burr-like; surrounding of lesionsuneven, echoed; echo type- no echo, high echo, echo, low echo, mixed echo; rear echo characteristics- rear echo does not change, rear echo changes, enhancement, attenuation, or both; effects on surrounding tissuethe mass has no effect on surrounding tissue, and the identifiable effect of the mass on surrounding tissue, catheter changes, Cooper ligament changes, edema, structural disturbances, local or diffuse thickening of the skin, calcification- no calcifications are found, and calcifications are found, diameter >0.5 mm coarse calcification, microcalcification outside the mass, microcalcification in the mass; special circumstancesno special manifestations, masses on the surface or inside of the skin, complex cysts, clustered cysts, intraductal masses, foreign bodies, intramammary lymph nodes, axillary lymph nodes, scars after surgery; blood supply- incomplete blood flow assessment, no blood supply in the lesion, blood supply in the lesion, blood flow in the adjacent lesion area, and increased blood flow in the surrounding tissue.
BI-RADS classification:
Class 0- checking information is not satisfactory or incomplete. For further examinations (such as test in special position or ultrasound, MRI) or recall of old films for a limited time; if there is no old film for comparative analysis, there should be further examination[24]. In China, some women have less fat content in the breast and are rich in substance. The breast tissue lacks natural contrast. These cases also need to be further examined by other imaging methods such as ultrasound, MRI, or it can be evaluated as class 0.
Class 1- negative. The structure of the mammary gland is clear without obvious lesions; class 2- affirmative benign findings. Such as benign masses (fibrous adenomas, pleomorphic adenomas, lipomas, fibroid adenomas, simple cysts, breast cysts, hemangioma, leiomyoma), benign calcification (circular calcification, strip-like or rod-like calcification with clear boundaries, rough popcorn shape or spotted calcification, and rounded calcification of uniform size) most belong to this class.
Class 3- possible benign findings, recommended for regular follow-up. This class has a high benign likelihood, but it needs to be determined by a stable or gradual reduction in the extent and size of the lesion in the short-term (not more than one year, usually half a year) follow-up. The vicious rate in this class generally does not exceed 2 %. The three signs of non-calcified masses with clear border, focal asymmetry, clustered rounded, or/and punctate calcifications are considered to be likely to be benign.
Class 4- suspected abnormal changes, need to consider accepting biopsy. This class includes a number of changes that require clinical intervention. Although there are no characteristic malignant lesion morphological abnormalities, this type of lesion has a certain malignant possibility, and the malignant rate is about 20 to 35 %. This class continues to be subdivided into three sub-categories of 4A, 4B, and 4C, and the final decision can be made based on the degree of malignancy. Class 4A- it is used to describe lesions that require clinical intervention but have a lower degree of malignancy. The results of histopathological reports are not necessarily malignant. It is appropriate and necessary to follow up regularly for half a year after a benign test result. Class 4B- it is used to describe lesions that require clinical intervention but have a moderate degree of malignancy. In this case, the benign follow-up rate depends on the degree of consistency of the final diagnosis of the imaging and pathology departments. Class 4C- it is used to describe lesions that require clinical intervention and have a slightly milder degree of malignancy, but do not have typical malignant features like class 5.
Class 5- high suggestive of malignancy (almost certainly malignant), clinical interventions must be taken. This type of lesion has a high rate of malignancy and the malignant rate is approximately 80 to 90 %. Highdensity masses with irregular edge and burr, segmental or linear distributions of heterogeneous calcifications, and partially blurred pleomorphic calcifications with irregular edge may be classified in this class.
Class 6- known biopsy-proven malignant lesion, and measures must be taken in time. This classification is used in cases where the biopsy has been confirmed to be a malignant lesion but has not received any treatment. It is generally used to evaluate imaging changes before and after treatment, or to evaluate and analyse imaging changes in preoperative neoadjuvant chemotherapy.
According to the BI-RADS classification results, classes 1, 2, and 3 were used as negative evaluation results, and 4 and 5 categories were used as positive evaluation results. The subject decided whether to undergo biopsy or surgery based on the clinician's advice and her wishes[25]. The results of the subjects who had either biopsy or surgical treatment were compared with the BI-RADS classification of the pathological tissue as the gold standard. The accuracy of the BI-RADS classification evaluation results was calculated as shown in Eqn. 1, and the sensitivity was as in Eqn. 2, specificity as in Eqn. 3, positive predictive value (PPV) as shown in Eqn. 4, and negative predictive value (NPV) as shown in Eqn. 5. % accuracy= true positive+true negative/total number of cases×100; % sensitivity= true positive/ true positive+false negative×100; % specificity= true negative/true negative+false positive×100; % PPV = true positive/true positive+false positive×100; % NPV = true negative/true negative+false negative×100.
Breast biopsy method:
Transdermal perforation biopsy can be used to distinguish benign and malignant skin changes. Fine needle biopsy was performed using a 10 or 20 ml syringe and a 23 to 27 gauge needle. While maintaining the negative pressure on the syringe, the needle was twisted while rotating the wrist. The sample taken was then discharged into the specimen fixing solution for evaluation by the pathology department. Breast palpation fine needle aspiration has been used for many years to diagnose palpable breast lumps[26]. When the lesion is palpable, especially for large and obvious lesions, fine needle aspiration can be performed quickly as a non-imaging guide. Obtaining proper breast imaging prior to any biopsy procedure is essential to avoid the possibility that the tissue being taken is normal breast tissue. For lesions that are considered suspicious, whether by palpation or by imaging techniques, careful imaging studies are needed to determine the location of the mass. For inaccessible lesions or pathologically accessible lesions, ultrasound can be used to guide fine needle aspiration to improve the diagnostic rate. It is less invasive and can help to diagnose quickly and accurately.
Statistical analysis:
SPSS17.0 software was used for data analysis. The pathological results were used as the gold standard. The receiver operating characteristic (ROC) curve of BI-RADS ultrasound diagnosis was drawn to calculate the sensitivity, specificity, positive predictive value and negative predictive value. The measurement data were expressed by average±standard deviation (x±s), two independent sample t test was used to compare the age difference of patients in benign and malignant cases, p<0.05 was considered statistically significant.
Results and Discussion
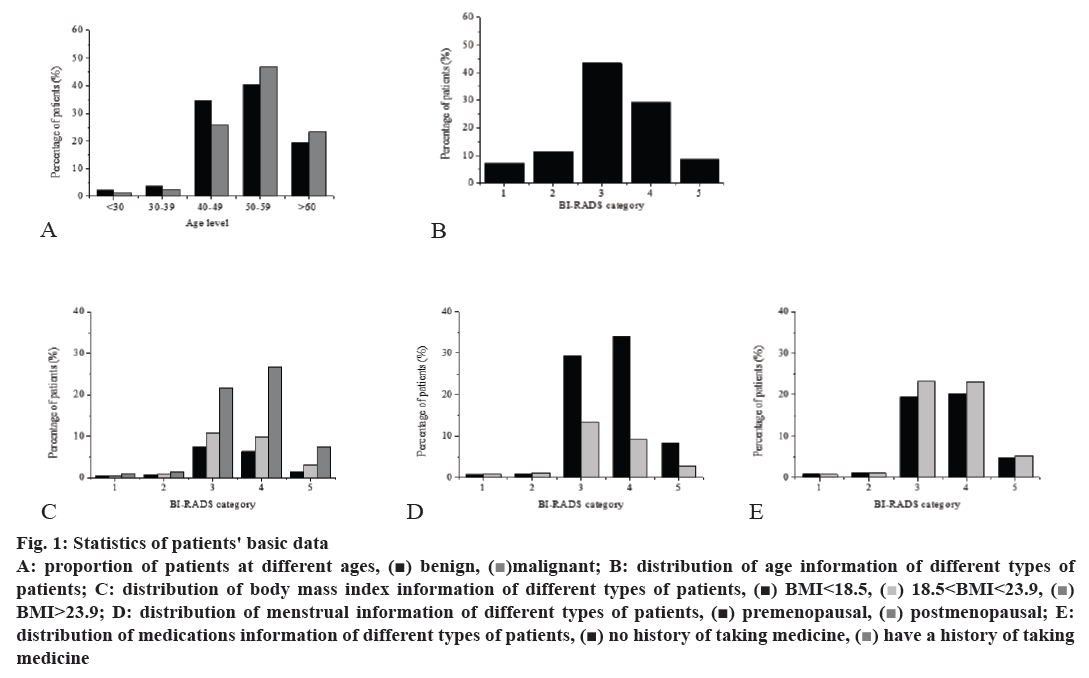
There were 3000 patients in the entire group, the final pathological results confirmed that 972 patients with malignant tumors, aged 22-75 y, mean age of 55.72±10.85 y, the remaining patients were all confirmed with benign tumors, aged 18 to 69 y, mean age of 43.66±11.71 y. The proportion of the age group of patients with different types of breast lumps is shown in fig. 1A. The distribution of age information of patients with different BI-RADS classifications is shown in fig. 1B, p<0.05, the difference was statistically significant. The distribution of body mass index information of patients with different BI-RADS classification is shown in fig. 1C, p<0.05, the difference was statistically significant. The distribution of menstrual status information of patients with different BI-RADS classification is shown in fig. 1D, p<0.05, the difference was statistically significant. The distribution of oral contraceptives administration in patients with different BI-RADS classification is shown in fig. 1E, p>0.05, the difference was not statistically significant.
Figure 1: Statistics of patients' basic data
A: proportion of patients at different ages, ( ) benign, (
) benign, ( )malignant; B: distribution of age information of different types of
patients; C: distribution of body mass index information of different types of patients, (
)malignant; B: distribution of age information of different types of
patients; C: distribution of body mass index information of different types of patients, ( ) BMI<18.5, (
) BMI<18.5, ( ) 18.5<BMI<23.9, (
) 18.5<BMI<23.9, ( )
BMI˃23.9; D: distribution of menstrual information of different types of patients, (
)
BMI˃23.9; D: distribution of menstrual information of different types of patients, ( ) premenopausal, (
) premenopausal, ( ) postmenopausal; E:
distribution of medications information of different types of patients, (
) postmenopausal; E:
distribution of medications information of different types of patients, ( ) no history of taking medicine, (
) no history of taking medicine, ( ) have a history of taking
medicine
) have a history of taking
medicine
As with most tumors, the incidence of breast tumors is linearly related to the age of female. Among them, there are more patients aged 40-49, and patients with BI-RADS Class 4 and 5 are also more in the 40-59 age group. However, patients with benign tumors (BI-RADS 1, 2, 3) are mostly in the 30-49 age group, which is slightly younger than BI-RADS 4 and 5 patients. Patients with a body mass index of less than 18.4 were underweight, with a body mass index of 18.5-23.9 was normal and a body mass index of over 24 being was overweight. In the study of the patient's body mass index, it was found that patients with a body mass index greater than 23.9 accounted for 58.5 %. The proportion of patients in overweight group was significantly greater than that of the normal group and the underweight group. It was speculated that the incidence of breast mass might be related to improper diet. In the menstrual status study of patients, it was found that the proportion of premenopausal and postmenopausal patients in BI-RADS class 1 and 2 was not very significant, and the proportion of premenopausal patients in BI-RADS class 3, 4, and 5 was significantly higher than the proportion of postmenopausal patients, it was speculated that the level of oestrogen in the body have a stimulating effect on breast masses. The effect of oral contraceptives on the occurrence of breast mass is still uncertain. After statistical calculations on the patient's oral contraceptives, it was found that there was no statistical difference in the information between the two groups with or without oral contraceptives administration.
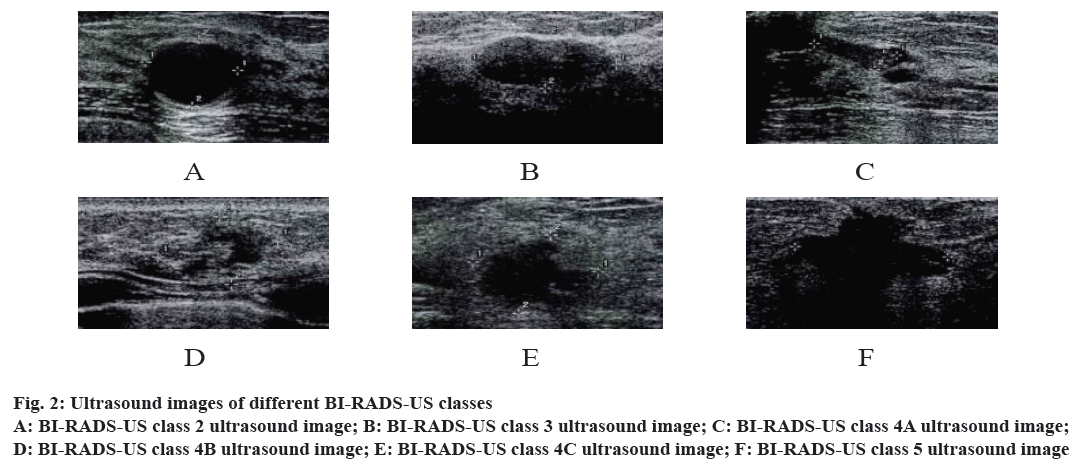
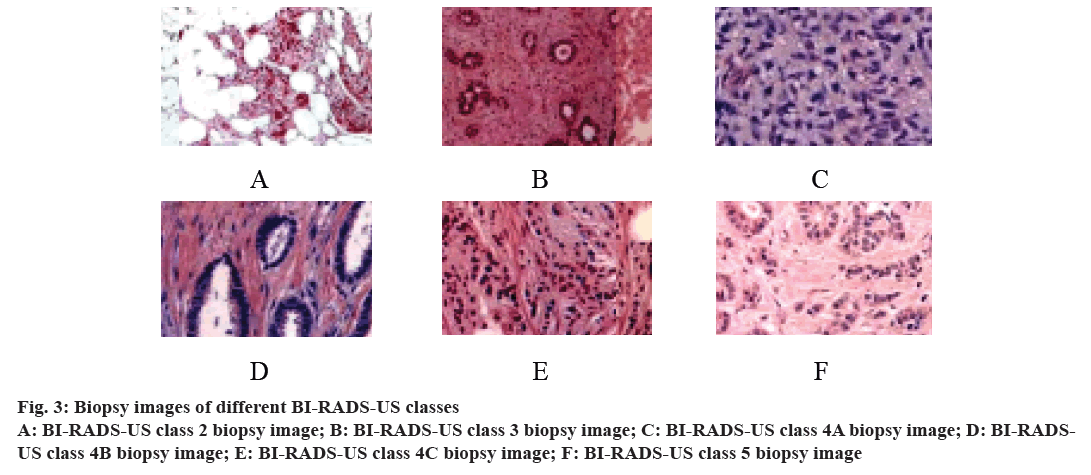
Among the 3860 lesions in the whole group, 40 of them had class 0 ultrasonographic (BI-RADSUS) lesions. Because the examination information was unsatisfactory or incomplete, the ultrasound evaluation was not completed, so they were excluded in the subsequent statistical analysis, and 3820 lesions remained. According to BI-RADS-US, they were divided into 1~5 classes. The class 1 is a normal ultrasound image, so it was no longer listed. The BI-RADS-US classes 2-4A were classified as a benign lesion for ultrasound examination, as shown in fig. 2A-C. The BI-RADS-US classes 4B-5 were classified as a malignant lesion for ultrasound examination, as shown in fig. 2D-F. 2780 benign lesions and 1040 malignant lesions were confirmed by surgery or biopsy pathology. BI-RADS-US Classes 1~5 biopsy is shown in (fig. 3). Class 1 was a normal biopsy image and was therefore not listed.
Figure 2: Ultrasound images of different BI-RADS-US classes
A: BI-RADS-US class 2 ultrasound image; B: BI-RADS-US class 3 ultrasound image; C: BI-RADS-US class 4A ultrasound image;
D: BI-RADS-US class 4B ultrasound image; E: BI-RADS-US class 4C ultrasound image; F: BI-RADS-US class 5 ultrasound image
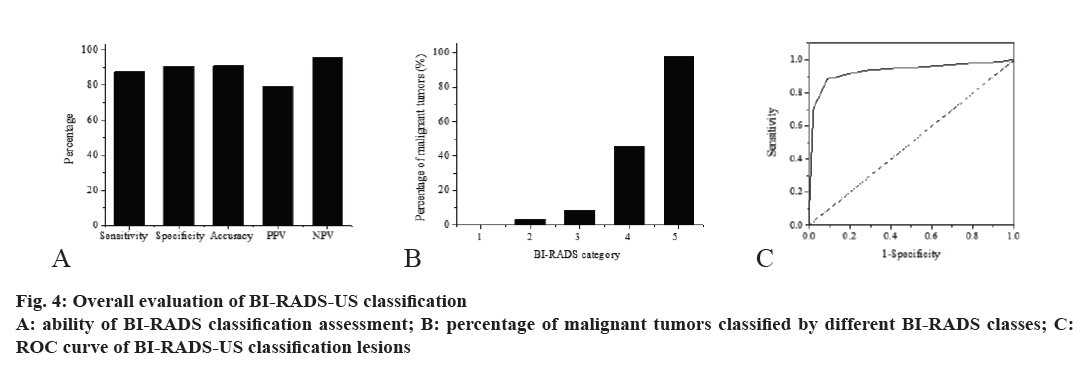
The overall sensitivity of the BI-RADS-US classification was 87.75 %, the specificity was 90.89 %, the accuracy was 91.04 %, the PPV was 79.24 %, and the NPV was 96.13 %, as shown in fig. 4A. The positive likelihood ratio and the negative likelihood ratio was respectively 9.78 and 0.21. BI-RADS-US class 1~5, in which BIRADS- US 4 was further divided into 3 subgroups, the percentages of malignant tumors were respectively 0, 3.26, 8.44, 45.29, and 97.96 %, as shown in fig. 4B. Taking the pathological result as the gold standard, the ROC curve was constructed according to the BIRADS- US classification as shown in fig. 4C, and the area under the curve (AUC) was calculated to be 0.928. At present, the ROC curve and the AUC have been used as the standard evaluation method for the accuracy evaluation of a certain diagnostic test. AUC comprehensively evaluates the sensitivity and specificity of the diagnostic test, and can select the best diagnosis plan through the AUC of multiple tests. It is generally considered that when the AUC is 0.5-0.7, the diagnostic value is lower, when the AUC is 0.7-0.9, the diagnostic value is medium, when the AUC is greater than 0.9, and the diagnostic value is higher. Based on the constructed ROC curve, the AUC was calculated to be 0.928, indicating that the diagnostic value of BIRADS- US is higher.
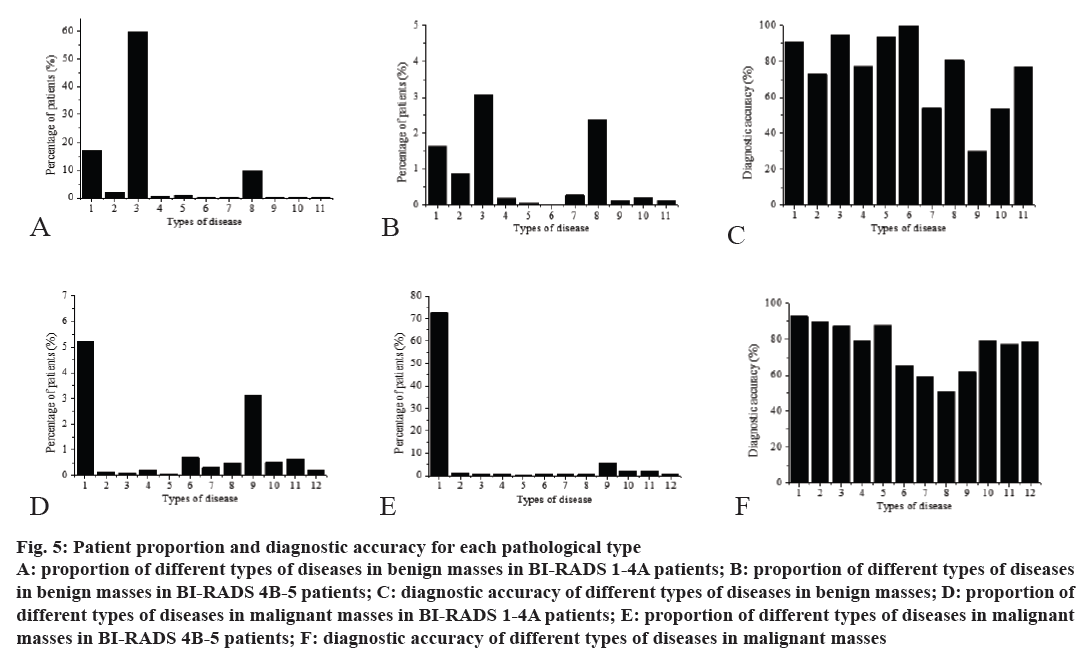
The diagnostic accuracy of each pathological type is shown in fig. 5. It can be observed from the figure that the ultrasound BI-RADS test was generally more accurate for benign tumors, and the accuracy of detecting malignant tumors was slightly lower. In the diagnosis of benign tumors, the diagnostic accuracy of lipomas has reached 100 %, but the correct rate of diagnosis of fat necrosis was only 30.2 %, and the diagnostic accuracy of benign phyllodes tumors and sclerosing breast diseases was also low, it only reached about 50 %, but the accuracy rate of diagnosis of other types of benign tumors can reach more than 70 %. In the diagnosis of malignant tumors, although the diagnostic accuracy of all types of malignant tumors listed has reached more than 50 %, the diagnostic accuracy rate for many malignant tumors was only about 60 %, and the diagnostic accuracy rate of most malignant tumors was 70-80 %, only the diagnostic accuracy rate for invasive cancer reached 92.8 %. This also shows that for different pathological types of tumors, it needs to rely on a variety of methods for detection. In the case that detection accuracy is not high, the physician needs to recommend patients to do biopsy or other examination to get more accurate results. However, when the accuracy of this method is high, biopsy or other tests can be avoided to reduce the pressure on the patient and the physician.
Figure 5: Patient proportion and diagnostic accuracy for each pathological type
A: proportion of different types of diseases in benign masses in BI-RADS 1-4A patients; B: proportion of different types of diseases
in benign masses in BI-RADS 4B-5 patients; C: diagnostic accuracy of different types of diseases in benign masses; D: proportion of
different types of diseases in malignant masses in BI-RADS 1-4A patients; E: proportion of different types of diseases in malignant
masses in BI-RADS 4B-5 patients; F: diagnostic accuracy of different types of diseases in malignant masses
The figures on abscissa of 5A-C in (fig. 5) represent respectively, 1. adenosis, 2. inflammation, 3. fibroadenomas, 4. catheter atypical hyperplasia, 5. cyst, 6. lipoma, 7. benign phyllodes, 8. intraductal papillary carcinoma, 9. fat necrosis, 10. sclerosing breast disease, 11. other types of diseases. The figures on abscissa of 5D-F in fig. 5 represent, 1. invasive carcinoma, 2. medullary carcinom,a 3. mixed cancer, 4. neuroendocrine carcinoma, 5. tubular carcinoma, 6. intraductal papillary carcinoma, 7. malignant phyllodes tumor, 8. borderline phyllodes tumor, 9. carcinoma in situ, 10. microinvasive cancer, 11. mucinous adenocarcinoma, and 12. other types of diseases, respectively.
In this study, after comparing the sensitivity of BIRADS classification and testing to different types of breast masses, it was found that the detection ability of different types of breast masses was different. It was concluded in the study that the sensitivity of the BIRADS- US classification was 87.75 %, the specificity was 90.89 %, the accuracy was 91.04 %, the PPV was 79.24 %, the NPV was 96.13 %, and through the ROC curve, the ultrasonic BI-RADS classification test was verified to be an excellent detection method. The ultrasound BI-RADS test was generally more accurate for benign tumors, and the accuracy of detecting malignant tumors was slightly lower. In the diagnosis of benign tumors, the diagnostic accuracy of lipomas has reached 100 %, but the correct rate of diagnosis of fat necrosis was only 30.2 %, and the diagnostic accuracy of benign phyllodes tumors and sclerosing breast diseases was also low, it only reached about 50 %, but the accuracy rate of diagnosis of other types of benign tumors can reach more than 70 %. In the diagnosis of malignant tumors, although the diagnostic accuracy of all types of malignant tumors listed has reached more than 50 %, the diagnostic accuracy rate for many malignant tumors was only about 60 %, and the diagnostic accuracy rate of most malignant tumors was 70-80 %. And through the statistical study of the patient's basic data, it was found that the patient's disease was linearly related to age, and was also related to body mass index, menstrual conditions and so on. The study confirmed that ultrasound BI-RADS classification is an excellent detection method, but the sensitivity of detection of different types of breast lumps is also different. The research in this study provided a theoretical basis for physicians to determine whether patients need biopsy or other examination, it is expected to enable BI-RADS grading detection to exert a better effect.
References
- Hu Y, Qiao M, Guo Y, Wang Y, Yu J, Li J, et al. Reproducibility of quantitative high‐throughput BI‐RADS features extracted from ultrasound images of breast cancer. Med Phys 2017;44(7):3676-85.
- Sirous M, Shahnani PS, Sirous A. Investigation of Frequency Distribution of Breast Imaging Reporting and Data System (BIRADS) Classification and Epidemiological Factors Related to Breast Cancer in Iran: A 7-year Study (2010–2016). Adv Biomed Res 2018;7(1):56.
- Uzunhisarcikli E, Goreke V. A novel classifier model for mass classification using BI-RADS category in ultrasound images based on Type-2 fuzzy inference system. Sādhanā 2018;43(9):138.
- Kim SM, Kim Y, Jeong K, Jeong H, Kim J. Logistic LASSO regression for the diagnosis of breast cancer using clinical demographic data and the BI-RADS lexicon for ultrasonography. Ultrasonography 2018;37(1):36-42.
- Grimm LJ, Johnson DY, Johnson KS, Baker JA Soo MS, Hwang ES, et al. Suspicious breast calcifications undergoing stereotactic biopsy in women ages 70 and over: Breast cancer incidence by BI-RADS descriptors. Eur Radiol 2017;27(6):2275-81.
- Gweon HM, Cho N, Kim SY, Koo HR, Seo M, Chu A, et al. Management for BI-RADS category 3 lesions detected in preoperative breast MR imaging of breast cancer patients. Eur Radiol 2017;27(8):1-6.
- Cen D, Xu L, Zhang S, Zhou S, Huang Y, Chen Z. BI-RADS 3–5 microcalcifications: prediction of lymph node metastasis of breast cancer. Oncotarget 2017;8(18):30190-8.
- Hoti A, Kraja F, Gashi E. Correlation between BI-RADS classification and histopathological findings of breast lesions in Albanian women. Eur J Cancer 2017;72:S13-S4.
- Woodard GA, Ray KM, Joe BN, Price ER. Qualitative Radiogenomics: Association between Oncotype DX Test Recurrence Score and BI-RADS Mammographic and Breast MR Imaging Features. Radiology 2017;286(1):162333.
- Iyengar NM, Brown KA, Zhou XK, Gucalp A, Subbaramaiah K, Giri DD. Metabolic Obesity, Adipose Inflammation and Elevated Breast Aromatase in Women with Normal Body Mass Index. Cancer Prev Res 2017;10(4):235.
- Niehoff N, White AJ, McCullough LE, Steck SE, Beyea J, Mordukhovich I, et al. Polycyclic aromatic hydrocarbons and postmenopausal breast cancer: An evaluation of effect measure modification by body mass index and weight change. Environ Res 2017;152:17-25.
- Ma H, Ursin G, Xu X, Lee E, Togawa K, Malone KE, et al. Body mass index at age 18 years and recent body mass index in relation to risk of breast cancer overall and ER/PR/HER2-defined subtypes in white women and African American women: a pooled analysis. Breast Cancer Res 2018;20(1):5.
- Hadi NI, Jamal Q, Iqbal A, Shaikh F, Somroo S, Musharraf SG. Serum Metabolomic Profiles for Breast Cancer Diagnosis, Grading and Staging by Gas Chromatography-Mass Spectrometry. Sci Rep 2017;7(1):1715.
- Qiu Y, Yan S, Gundreddy RR, Wang Y, Cheng S, Liu H. A New Approach to Develop Computer-Aided Diagnosis Scheme of Breast Mass Classification Using Deep Learning Technology. J Xray Sci Technol 2017;25(5):751.
- Park SY, Choi JS, Han BK, Ko EY, Ko ES. Shear wave elastography in the diagnosis of breast non-mass lesions: factors associated with false negative and false positive results. Eur Radiol 2017;27(9):3788-98.
- Martin N, Buykx P, Shevills C, Sullivan C, Clark L, Newbury-Birch D. Population Level Effects of a Mass Media Alcohol and Breast Cancer Campaign: A Cross-Sectional Pre-Intervention and Post-Intervention Evaluation. Alcohol 2017;53(1):1-8.
- Pai T, Nair N, Pantvaidya G, Deodhar K, Shet T. Metastatic nasopharyngeal carcinoma presenting as an isolated breast mass: A diagnostic pitfall and a review of literature. Indian J Pathol Microbiol 2017;60(1):119-21.
- Dai L, Shi C, Xinbo LU. Difference analysis on physical characteristics and chemical components of reconstituted tobacco used in traditional cigarettes and heat not burn tobacco products. Acta Tabacaria Sin 2017;23(1):20-6.
- Pastorian K, Hawel L 3rd, Byus CV. Optimization of cDNA representational difference analysis for the identification of differentially expressed mRNAs. Anal Biochem 2000;283(1):89-98.
- Ringling C, Rychlik M. Origins of the difference between food folate analysis results obtained by LC–MS/MS and microbiological assays. Anal Bioanal Chem 2017;409(7):1815-25.
- Moritz F, Kaling M, Schnitzler JP, Schmitt-Kopplin P. Characterization of poplar metabotypes via mass difference enrichment analysis. Plant Cell Environ 2017;40(7):1057-73.
- Zhan F, Tao Y, Zhao H. Alternative difference analysis scheme combining R-space EXAFS fit with global optimization XANES fit for X-ray transient absorption spectroscopy. J Synchrotron Radiat 2017;24(Pt 4):818.
- Lewerenz M, Warnecke A, Sauer DU. Introduction of capacity difference analysis (CDA) for analyzing lateral lithium-ion flow to determine the state of covering layer evolution. J Power Sources 2017;354:157-66.
- Liu S, Zou JL, Zhou FL, Fang YM. Efficacy of ultrasound-guided vacuum-assisted Mammotome excision for management of benign breast diseases: analysis of 1267 cases. Nan Fang Yi Ke Da Xue Xue Bao 2017;37(8):1121-5.
- Wan P, Wu C, Lin Y. On-road experimental study on driving anger identification model based on physiological features by ROC curve analysis. IET Intel Transport Syst 2017;11(5):290-8.
- Zhu BP, Guo ZQ, Lin L, Liu Q. Serum BSP, PSADT, and Spondin-2 levels in prostate cancer and the diagnostic significance of their ROC curves in bone metastasis. Eur Rev Med Pharmacol Sci 2017;21(1):61.